Published online Mar 21, 2013. doi: 10.3748/wjg.v19.i11.1845
Revised: January 8, 2013
Accepted: January 23, 2013
Published online: March 21, 2013
Processing time: 195 Days and 23.2 Hours
We present three cases of gastrointestinal muco-submucosal elongated polyps, two located in the duodenum and one in the descending colon. All three cases had a characteristic, “worm-like” endoscopic appearance and were lined by unremarkable mucosa. The vascular component was located in the submucosa and was composed of a mixture of variably dilated blood vessels (capillaries and veins) and lymphatics. The duodenal polyps displayed lipomatous metaplasia of the submucosal stroma. The dual vascular phenotype of the vascular component was confirmed by immunohistochemistry with D2-40 and CD31.
- Citation: Tan CL, Tan SH, So JB, Petersson F. Muco-submucosal elongated polyps of the gastrointestinal tract: A case series and a review of the literature. World J Gastroenterol 2013; 19(11): 1845-1849
- URL: https://www.wjgnet.com/1007-9327/full/v19/i11/1845.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i11.1845
Benign gastrointestinal polyps composed of mucosa and submucosa, the latter with a prominent vascular component are relatively unusual non-neoplastic lesions with uncertain etiopathogenesis. Such polyps have mainly been studied by Japanese investigators, but are increasingly being recognized by western investigators[1,2]. The nomenclature pertaining to these polyps has varied. In the seminal paper on this entity, Matake et al[3] chose the term “colonic muco-submucosal elongated polyp”. Most of the reported cases have been located in the large bowel[4-7], but three polyps with identical endoscopic and histological features have also been documented in the small bowel, including the duodenum[8-10].
Irrespective of site, muco-submucosal elongated polyps display characteristic endoscopic features, with a “worm-like” appearance which are lined by unremarkable mucosa. Histologic examination confirms the presence of a normal mucosa and reveals a submucosal component with a variably prominent mixture of blood vessels and lymphatics and absence of significant inflammation. In this paper we present the clinicopathologic features of three additional cases of this entity and review the literature on these characteristic benign gastrointestinal polyps.
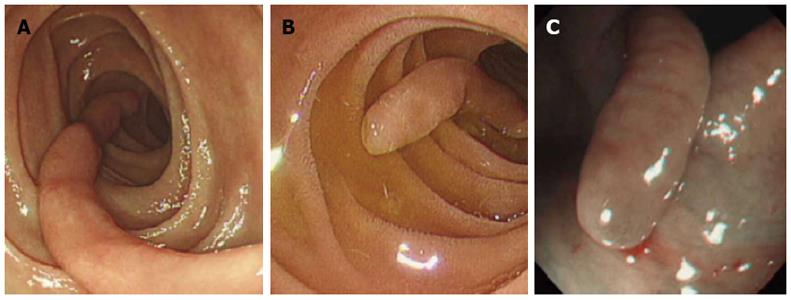
A 55 year-old previously healthy female presented with postprandial abdominal discomfort of 3 mo duration. There were no signs or symptoms of gastrointestinal bleeding or malabsorption. Gastroduodenoscopy revealed a 4 cm long, slender, “worm-like” polyp in the second part of the duodenum (Figure 1A). The polyp was removed endoscopically. The patient was well on follow up at 3 mo.
A 70 year-old previously healthy man presented with reflux symptoms of unknown duration. Gastroduodenoscopy showed a 2.2 cm long, slender polyp in the duodenum (Figure 1B). The polyp was removed endoscopically.
A 74 year-old female with a history of hypertension and iron deficiency anemia secondary to peptic ulcer disease presented with epigastric pain associated with constipation of 1 mo duration. Colonoscopy showed a 1.4 cm long, slender polyp in the descending colon (Figure 1C) and a distal rectal ulcer near the anal verge. The polyp was removed endoscopically. There was no evidence of diverticular disease. In addition, gastroduodenoscopy showed several benign gastric and duodenal ulcers (biopsies from the gastric ulcers showed mild chronic gastritis with reactive changes and no activity; no Helicobacter pylori were identified; the rectal biopsy showed features consistent with a solitary rectal ulcer).
The tissues were fixed in neutral formalin and both polyps were completely embedded in paraffin. 4 μm thick sections were cut and stained with hematoxylin and eosin (HE). An immunohistochemical study with commercially available antibodies (D2-40-podoplanin, CD31) using protocols according to the manufacturers’ recommendations were employed in Case 1 and 3. Immunohisto-chemistry with WT-1 were performed in all three cases.
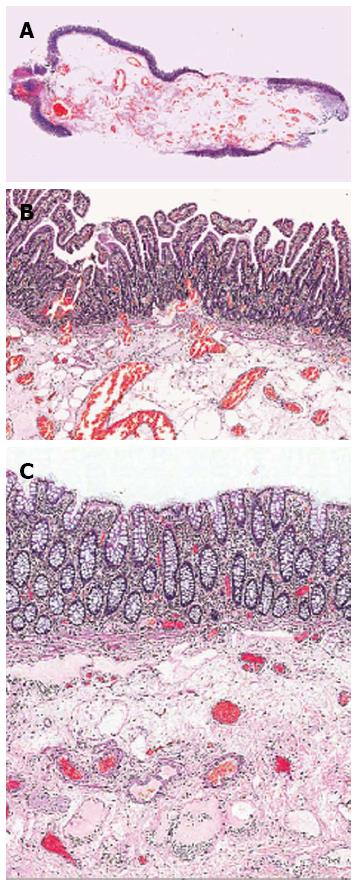
All three polyps were thin and elongated corresponding to the “worm-like” endoscopic appearance (Figure 2A). All polyps were lined by unremarkable mucosa. The submucosal components contained prominent vasculature including dilated, variably sized veins and lymphatic vessels running parallel to the long axis of the polyps and surrounded by loose collagenous stroma (Figure 2B and C). In addition, there was also focal lipomatous metaplasia in both duodenal polyps. No arterial vascular component was identified. No vascular abnormalities were present in the mucosa. No significant inflammation was identified.
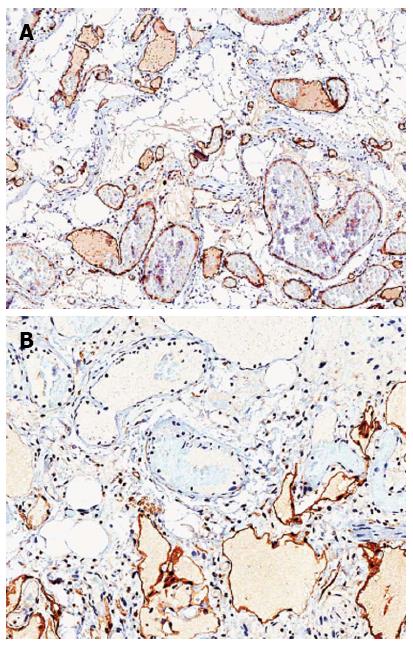
The endothelial cells of both vascular components in the polyps displayed immunoreactivity for CD31 throughout the lesion (Figure 3A). D2-40-podoplanin was selectively expressed by the endothelial cells of the lymphatic component (Figure 3B). In Case 1 and 2, the endothelial cells of both vascular components displayed patchy cytoplasmic positivity for WT-1 whereas Case 3 was completely negative (data not shown).
We herein report three cases of muco-submucosal elongated polyps, two in the duodenum and the other one in descending colon. This characteristic, albeit unusual entity, is not well covered in most standard textbooks in gastrointestinal pathology. Initially described by Japanese investigators, Matake et al[3,11] published two series of these polyps comprising 19 cases in toto. The polyps ranged in size from 1.2-16 cm (mean 2.9 cm) and displayed a characteristic appearance (elongated, slender, drumstick shaped). Histological examination revealed normal mucosa and a loose to dense submucosal layer containing a variably prominent vascular component composed of dilated blood vessels (veins and capillaries) and lymphatics. Subsequently, these polyps have been increasingly recognized and mostly documented in the large bowel (all parts) including rectum[1,5,6,12,13]. In all 23 reported polyps from the large bowel, the size has ranged from 0.7 to 15 cm (mean 2.8 cm).
Two polyps with endoscopic and morphologic features conforming to a muco-submucosal elongated polyp have also been described in the small bowel[9,10].
In addition, in 2009, Kim et al[8] reported a case of a 5 cm long duodenal polyp with a “wormlike/drumstick” endoscopic appearance which they labelled as “polypoid vascular and lymphatic malformation of the duodenum”. The histologic features as described by the authors and the provided photomicrographs show, in our opinion, a muco-submucosal elongated polyp.
Our Case 1 and 2 were of duodenal origin, which is a rare site and thus represents the third and fourth published cases of muco-submucosal elongated polyps of the small bowel.
A lesion resembling muco-submucosal elongated polyps has been described by Kelly[14]. In this paper, the author characterized eight cases of swollen mucosal folds and broad based, ‘leaf-like’ polyps with mucosal and submucosal vascular congestion, thrombi, edema, hemorrhage and hemosiderin deposits in the sigmoid colon associated with diverticular disease in resection specimens. In addition to the submucosal component, these polypoidal lesions showed mucosal prolapse-type changes. The author adequately labelled these lesions “polypoid prolapsing mucosal folds in diverticular disease” (PPMF). Interestingly, cases of muco-submucosal elongated polyps associated with diverticular disease have also been documented[1,7]. In contrast to muco-submucosal elongated polyps, PPMFs do not display the “wormlike”, slender gross appearance with narrow attachment to the bowel mucosa. In addition, on histological examination, the mucosal component in PPMFs shows prolapse-type changes, which reportedly are absent in muco-submucosal elongated polyps, including the three cases presented herein.
Absence of significant inflammation in muco-submucosal elongated polyps also differentiate this entity from other mucosal prolapse associated polyps such as inflammatory “cap” polyps, inflammatory cloacogenic polyps and inflammatory myoglandular polyps[15].
Filiform polyps (a subtype of inflammatory polyps) characterized by finger like projection covered by normal colonic mucosa with central core containing vessels and smooth muscle fibers can also mimic muco-submucosal elongated polyps. However, these polyps are usually multiple (“filiform polyposis”) and are associated with inflammatory bowel disease. Of note is that cases without apparent history of inflammatory bowel disease appear to exist[16].
An inverted colonic diverticulum is a clinically important differential diagnosis. When these are large in size, they may resemble a pedunculated polyp and an endoscopic polypectomy may be performed which is associated with risk of perforation[17]. A high index of clinical suspicion is important for these lesions and the key to its recognition is the endoscopic association with conventional diverticuli in the segment where the polyp is located. A small biopsy from an inverted diverticulum shows non-specific features including normal to mildly inflamed mucosa and congested submucosa with variable degrees of chronic inflammation.
The residual stalk after a previously excised pedunculated adenoma or after autoamputation of any pedunculated polyp may also come into the endoscopic and histological differential diagnosis. Distinguishing, albeit non-specific features, are procedure related changes (granulation tissue and hemosiderin) and obviously, a history of previous polypectomy.
The etiology of muco-submucosal elongated polyps is unknown. It has been suggested that the gastrointestinal peristaltic movement may serve as mechanical traction for redundant mucosa, thereby making such areas of mucosa a nidus for polyp formation[3,18]. In line with this, Alizart et al[1] hypothesized that focal areas with prominent submucosal venous plexus may elevate the mucosa and serve as the leading point/nidus for the traction and hence polyp formation. A similar explanation has also been put forward by Kelly[14] to explain the formation of PPMFs associated with diverticular disease.
We have immunohistochemically confirmed that the submucosal vascular component is composed of both blood vessels and lymphatics. Thus, we suggest that in addition to the criteria for the diagnosis of muco-submucosal elongated polyp as suggested by Alizart et al[1]: (1) elongated, cylindrical shape with narrow base; (2) presence of submucosa; (3) absence of marked architectural disturbance of the overlying mucosa; and (4) absence of inflammatory infiltrate in both the mucosa and submucosa; the presence of a significant vascular submucosal component with a dual phenotype could be added to these criteria.
The endoscopic ultrasonographic features of muco-submucosal elongated polyps have been reported by Takahashi et al[12] and Akahoshi et al[13]. The ultrasonographic findings appear characteristic for this entity and in all lesions, elongated polypoid structures with both mucosal and submucosal layers were visualized. The “microcystic components” that the authors reported in the submucosal layer, most likely corresponds to the ectatic vascular component that is characteristically present in these lesions. The authors conclude that the distinctive ultrasonographic features allow for the diagnosis to be made and hence differentiate muco-submucosal elongated polyps from other submucosal lesions such as leiomyoma, lipoma and lymphangioma[13]. Successful endoscopic removal of muco-submucosal elongated polyp (as in our cases) have previously been reported[5,6,9,13].
Recently it has been suggested that endothelial cytoplasmic immunohistochemical expression of WT-1 is helpful in discriminating between cutaneous vascular neoplasms and vascular malformations. Trindade et al[19] studied 117 cutaneous vascular neoplasms and 50 vascular malformations and found that all vascular neoplasms showed diffuse endothelial expression of WT-1 whereas all vascular malformations except for the arteriovenous type were negative. The expression of WT-1 in a random manner in our first and second case and complete negativity in our third case lend support to the reactive nature of the vascular components in muco-submucosal elongated polyps. However, it is important to bear in mind that all the cases in Trindade et al[19] study were of cutaneous origin and the underlying molecular mechanisms behind the development of cutaneous and intestinal vascular lesions may differ. Further studies are warranted to clarify this.
In conclusion, we report three cases of gastrointestinal muco-submucosal elongated polyps with prominent submucosal vascular components. One of these was located in the large bowel and the other two were of duodenal origin. We have determined by immunohistochemistry that the vascular component is a mixture of blood vessels and lymphatics. The endoscopic ultrasonographic appearance of these polyps appears to be characteristic allowing for a high degree of certainty in making this diagnosis by the endoscopists.
We would like to thank Department of Pathology, Singapore General Hospital for performing immunohistochemistry D2-40-podoplanin on Case 1 and 3.
P- Reviewers Capasso R S- Editor Gou SX L- Editor A E- Editor Zhang DN
| 1. | Alizart MM, Rosty C, Brown IS. Colonic mucosubmucosal elongated polyp: a clinicopathologic study of 13 cases and review of the literature. Am J Surg Pathol. 2011;35:1818-1822. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Ambrosio MR, Rocca BJ, Ginori A, Barone A, Onorati M, Lazzi S. Long pedunculated colonic polyp with diverticulosis: case report and review of the literature. Pathologica. 2011;103:8-10. [PubMed] |
| 3. | Matake H, Matsui T, Yao T, Iwashita A, Hoashi T, Yao K, Tsuda S, Takenaka K, Sakurai T, Yamada Y. Long pedunculated colonic polyp composed of mucosa and submucosa: proposal of a new entity, colonic muco-submucosal elongated polyp. Dis Colon Rectum. 1998;41:1557-1561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Lee HS, Choi BK, Seo WS, Kim MK, Lee JK, Yang SY, Park ET, Jang YS, Lee SH, Seol SY. Colonic Muco-Submucosal Elongated Polyp. Korean J Gastrointest Endosc. 2003;26:103-105. |
| 5. | Kume K, Sakata H, Yoshikawa I, Watanabe T, Harada M. Polypectomy of a colonic muco-submucosal elongated polyp. Endoscopy. 2009;41 Suppl 2:E265-E266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Hirasaki S, Koide N, Fukazawa M, Fujiwara K. Small muco-submucosal elongated polyp of the sigmoid colon. Intern Med. 2011;50:1855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Ogata T, Itagaki S, Ishiguro S, Koseki T, Adachi T, Arai S. [A case of colonic muco-submucosal elongated polyp (CMSEP) with colonic diverticulosis]. Nihon Shokakibyo Gakkai Zasshi. 2000;97:44-47. [PubMed] |
| 8. | Kim JW, Oh HC, Kim MK, Kim JG. Polypoid vascular and lymphatic malformation of the duodenum: a case report. J Gastrointestin Liver Dis. 2010;19:85-88. [PubMed] |
| 9. | Sugimori S, Watanabe K, Fujiwara Y, Oshitani N, Arakawa T. [Enteric muco-submucosal elongated polyp]. Nihon Rinsho. 2008;66:1359-1363. [PubMed] |
| 10. | Nishimura J, Nishikawa J, Tanabe R, Hashimoto S, Matsunaga T, Nakamura M, Goto A, Hamabe K, Okamoto T, Sakaida I. A case of enteric muco-submucosal elongated polyp. Nihon Shokakibyo Gakkai Zasshi. 2012;109:1940-1945. [PubMed] |
| 11. | Matake H, Seo M, Oh K. Long pedunculated colonic polyps composed of mucosa and submucosa: a report of four cases. Stomach Intest. 1994;29:1330-1334. |
| 12. | Takahashi M, Kubokawa M, Tanaka M, Sadamoto Y, Ito K, Yoshimura R, Harada N, Nawata H. Endoscopic ultrasonography features of colonic muco-submucosal elongated polyp. Endoscopy. 2002;34:515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Akahoshi K, Matsumoto M, Kimura M, Murata A, Murao H, Sumida Y, Kubokawa M, Ito K, Oya M. Colonic muco-submucosal elongated polyp: diagnosis with endoscopic ultrasound. Br J Radiol. 2005;78:419-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Kelly JK. Polypoid prolapsing mucosal folds in diverticular disease. Am J Surg Pathol. 1991;15:871-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 117] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 15. | Williams G, Bussey . H, Morson. B. Inflammatory cap polyps of the large intestine. Br J Surg. 1985;72:133. |
| 16. | Lee CG, Lim YJ, Choi JS, Lee JH. Filiform polyposis in the sigmoid colon: a case series. World J Gastroenterol. 2010;16:2443-2447. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Paoluzi OA, Tosti C, Andrei F, Stroppa I, Pallone F. Look out before polypectomy in patients with diverticular disease--a case of a large, inverted diverticulum of the colon resembling a pedunculated polyp. Can J Gastroenterol. 2010;24:61-63. [PubMed] |
| 18. | Kanazawa N, Kawahara Y, Kasahara I, Higuchi Y, Arai T, Kuroiwa K. Polypoid prolapsing mucosal folds with diverticulosis and colonic muco-submucosal elongated polyps. Geriatr Gerontol Int. 2006;6:65-68. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Trindade F, Tellechea O, Torrelo A, Requena L, Colmenero I. Wilms tumor 1 expression in vascular neoplasms and vascular malformations. Am J Dermatopathol. 2011;33:569-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 69] [Article Influence: 4.9] [Reference Citation Analysis (0)] |