Published online Dec 21, 2012. doi: 10.3748/wjg.v18.i47.7118
Revised: October 13, 2012
Accepted: October 30, 2012
Published online: December 21, 2012
Esophageal granular cell tumors (GCTs) are rare tumors of the esophagus. We evaluated the clinical and pathologic features of 9 esophageal GCT patients (5 men and 4 women) from our institute and reviewed the related disease literature. Patient age ranged from 25 to 53 years (mean: 41 years). All the patients were asymptomatic or presented with non-specific symptoms. Most GCTs occurred in the distal esophagus and were less than 6 mm in diameter. Computational analysis showed that the average gray-scale endoscopic ultrasound images of esophageal GCTs were greater than that of esophageal leiomyomas. Eight patients were treated by endoscopic resection, and 1 patient underwent surgical excision. No post-therapy recurrence or metastasis developed during follow-up (mean: 36.4 mo, range: 1-72 mo).
- Citation: Xu GQ, Chen HT, Xu CF, Teng XD. Esophageal granular cell tumors: Report of 9 cases and a literature review. World J Gastroenterol 2012; 18(47): 7118-7121
- URL: https://www.wjgnet.com/1007-9327/full/v18/i47/7118.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i47.7118
Granular cell tumors (GCTs) are nerve sheath tumors composed of Schwann cells with granular cytoplasm[1]. GCTs were first described in the 1920s by Abrikossoff in a series of 5 cases with benign tumors removed from the tongue. These tumors were once regarded as specific to skeletal muscle. However, subsequent studies identified GCTs in various other tissues, including skin, breast, respiratory tract, and biliary system[1].
GCTs are relatively rare in the gastrointestinal tract, accounting for approximately 8% of all GCTs[2,3]. Of these, only about 2% occur in the esophagus[3]. Abrikossoff described the first case of an esophageal GCT in the early 1930s. To date, about 200 cases of esophageal GCTs have been described in the literature, mostly representing single case reports or small case series. Several aspects of esophageal GCTs remain to be elucidated, such as whether endoscopic ultrasound (EUS) can effectively diagnose the disease, what the appropriate management is, and whether GCTs undergo malignant degeneration. Therefore, we studied the clinical and pathologic features of esophageal GCTs by retrospectively analyzing all esophageal GCT cases treated at our institution to address these unresolved issues.
All the patients evaluated in this study were in- or outpatients treated at the First Affiliated Hospital, College of Medicine, Zhejiang University, between January 2001 and December 2011. All the patients were initially diagnosed with suspected esophageal submucosal protruding lesions (as revealed by conventional endoscopy), and were subsequently confirmed as GCT by histology. The study was approved by the hospital’s ethics committee, and all the patients agreed to study participation.
Patient preparation for EUS examinations was the same as those for conventional gastroscopy. The EUS equipment was composed of double cavity mirrors (Olympus GIF-2T 240), a mini-ultrasound probe with 12 mHz frequency, and the ultrasound device (Olympus EU M2000). Endoscopic specialists performed all operations, diagnoses, and therapeutic interventions.
Esophageal GCTs may be easily misdiagnosed as leiomyomas using EUS examination. To explore whether EUS can distinguish the two diseases by computer-aided image analysis, we compared the average gray-scale and gray-scale standard deviation of the EUS images for the two diseases. We selected the lesions with a range of interest for each of the cases, then determined the average gray-scale and gray standard deviation of the range of interest and compared the results for the two disease groups. The image analysis software was Photoshop CS2 9.0. The parameter indices of average gray-scale and gray standard deviation referred to the nature of echo and echogenicity, respectively.
Eight cases underwent endoscopic resection, and the remaining case underwent surgical excision. The procedures for endoscopic resection of GCTs were the same as those used for other mucosal-based and submucosal esophageal lesions. In a case with esophageal GCT originating from the submucosa and having a diameter larger than 10 mm, the trans-thoracic operation was performed.
The tissue specimens obtained by endoscopic resection or surgical excision were fixed in 10% formalin and processed for paraffin embedding using standard methods. Sections of 4 mm thickness were stained with hematoxylin and eosin, and observed by light microscopy. Subsequently, specimens from all cases were stained for CD68, CD34, Ki-67, smooth muscle actin (SMA), S-100, GFAP, and p53 using standard immunohistochemistry techniques.
The criteria for histological diagnoses of GCT were: the tumor being mainly composed of larger tumor cells with cytoplasm rich in eosinophilic granules; the tumor cell morphology showing densely nested or stringy structure; the granules in the cytoplasm showing positive periodic acid-Schiff (PAS) staining; the tumor cells expressing S-100.
To study the progression of GCTs, all the patients were followed-up with periodic endoscopic examination. Statistical analyses were performed using the SPSS 13.0 software for Windows. P values less than 0.05 (by a 2-tailed test) were considered statistically significant.
The clinical characteristics of the patients are listed in Table 1. Our case series included 9 histologically confirmed esophageal GCT patients (5 men and 4 women). Patient age ranged from 25 to 53 years, with a mean age of 41 years. Of the 9 patients, 7 complained of nonspecific symptoms, including upper abdominal distension, poor appetite, belching, and acid reflux.
| Case | Gender | Age | Symptoms | Location | Size (mm × mm) | Originating layer |
| 1 | Female | 45 | Upper abdominal distension | Distal | 5 × 4 | Undetermined |
| 2 | Female | 25 | Upper abdominal distension | Distal | 5 × 4 | Submucosa |
| 3 | Male | 41 | No | Distal | 4 × 3 | Muscularis mucosa |
| 4 | Female | 41 | Recurrent belching and acid reflux | Distal | 5 × 4 | Mucosa |
| 5 | Male | 47 | No | Distal | 4 × 2 | Muscularis mucosa |
| 6 | Male | 50 | Upper abdominal distension, poor appetite | Distal | 6 × 4 | Mucosa |
| 7 | Female | 44 | Abdominal distension and belching | Middle | 5 × 3 | Muscularis mucosa |
| 8 | Male | 53 | Substernal distension | Distal | 11 × 10 | Submucosa |
| 9 | Male | 32 | Upper abdominal distension | Middle | 4 × 3 | Mucosa |
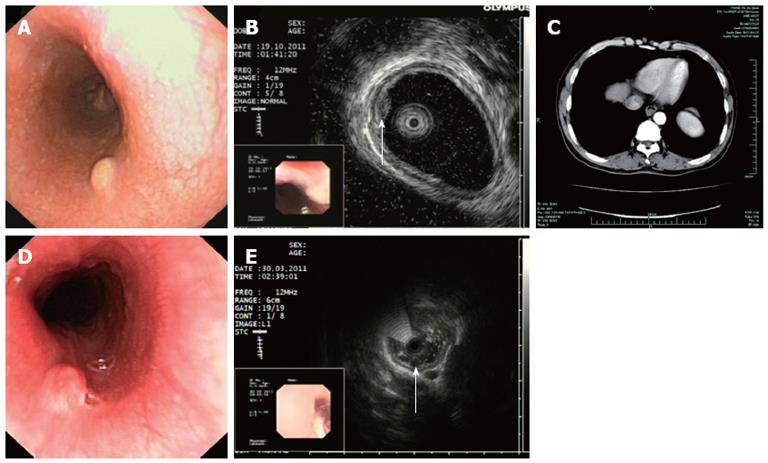
All 9 cases were initially diagnosed with suspected esophageal submucosal protruding lesions, as indicated by conventional endoscopy. The typical endoscopic appearance was isolated, tawny or grayish white submucosal nodules with the overlying mucosa being normal or slightly granular, without ulceration or mucosal depression (Figure 1). Seven cases involved the distal esophagus, and 2 cases involved the middle esophagus. Eight cases received computed tomography chest examination; all of which revealed a soft-tissue mass in the esophagus and partial narrowing of the esophageal lumen. The enhanced scan technique showed that all masses were moderately enhanced.
EUS was performed in 8 patients and showed that the tumors were slightly low echo and were circular or quasi-circular in shape. The surrounding esophageal structure appeared normal for all the lesions. Three cases originated from the mucosa, 2 from the submucosa, and 3 from the muscularis mucosa. The size of the tumors ranged from 4 to 11 mm in diameter. In comparison to esophageal leiomyomas, the esophageal GCTs showed slightly stronger echo. Quantitative gray-scale analysis confirmed this observation. Photoshop CS2 9.0 analysis of the EUS images of esophageal GCTs, compared to age-, sex-, size- and location-matched esophageal leiomyomas, indicated that the average gray-scale EUS images of esophageal GCTs were slightly and significantly greater than that of esophageal leiomyomas. Accordingly, we propose that the echo of GCTs may be stronger than that of esophageal leiomyomas.
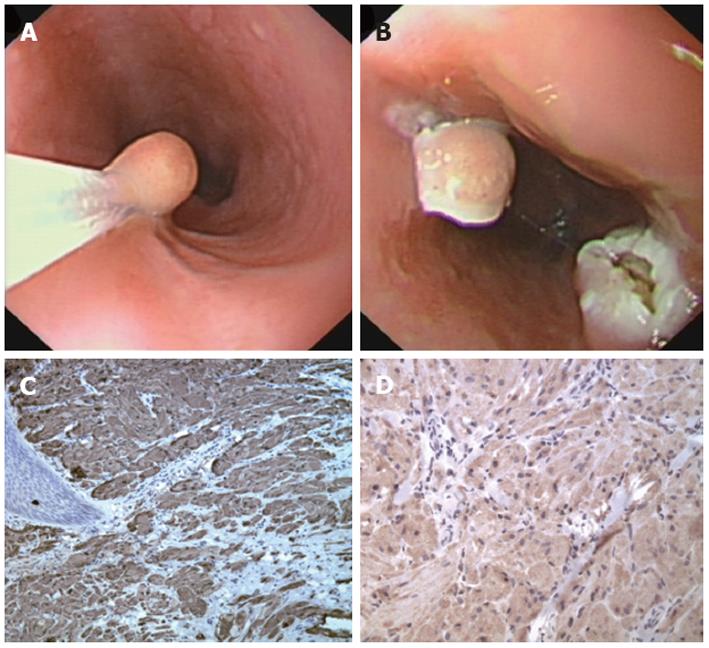
Histological analysis showed that all tumors were composed of proliferating cells of slightly ovoid shape and with abundant eosinophilic granular cytoplasm. The tumors were PAS-positive. Diastase-resistant granules, representing lysosomes, were present within the cytoplasm of some cells. Immunohistological study showed that all the tumors were positive for S-100 and CD68, but negative for SMA, CD34, p53, GFAP, Ki-67, and CD117 (Figure 2).
No recurrence was observed after endoscopic or surgical resection or during the follow-up period (mean: 36.4 mo, range: 1-72 mo).
GCT is a rare type of esophageal submucosal tumor. Its character of dormant onset lends to the disease being overlooked or misdiagnosed. GCTs are female predominant[4], and mainly occur in middle-age[5,6]. In the current series of esophageal GCTs patients, the mean age was 41 years, but the sex distribution was more equal than in the collected literature. Since ethnicity may play a role in the development of GCTs[7], the observed difference in sex distribution may reflect our patients’ Chinese background. According to the collected literature, esophageal GCTs primarily occur in the distal esophagus. Orlowska et al[6] reported that two-thirds of esophageal GCTs were found in the distal esophagus, with only 20% and 15% in the middle and proximal esophagus, respectively. Another case series reported by Goldblum et al[5] showed that 12 of 13 patients had distal esophageal GCT. Similarly, our case series included 7 cases with GCTs in the distal esophagus, and only 2 cases of GCT in the middle esophagus.
In general, esophageal GCTs are initially observed by conventional gastroscopy and confirmed by histological analysis. The ability of EUS to show the size, origin, borders, and echo structure of the submucosal lesion, has dramatically improved the diagnostic accuracy for submucosal disorders[8]. However, EUS may still misdiagnose some lesions with similar imaging features, such as esophageal GCTs and leiomyomas. In the current study, we applied computer-aided analysis techniques to comparatively analyze the ultrasound images of GCTs and leiomyomas. Our results showed that the gray value of esophageal GCTs was slightly, but significantly, greater than that of esophageal leiomyomas. This suggests that the EUS echo of esophageal GCTs is higher than that of leiomyomas, which possibly represents a discriminating feature of esophageal GCTs and leiomyomas. This feature may aid in the differential analysis of gray values on EUS images and help to improve the preoperative diagnostic accuracy of esophageal GCTs and possibly stimulate ideas for new strategies for earlier diagnosis and more effective treatment.
GCTs are potential malignant tumors. Fanburg-Smith et al[9] proposed the first histological criteria for prospectively diagnosing malignancy in GCTs, which include tumor cell necrosis, tumor cell spindling, increased nuclear size, large nucleoli, mitotic activity, and nuclear pleomorphism. Due to the potential for malignancy, endoscopic resection or surgical excision is recommended for patients with esophageal GCTs. In the current study, 8 cases were treated by endoscopic resection and one case was treated by surgical excision. All the patients were followed-up with periodic endoscopic examinations, during which no recurrence was detected. Our experience, as well as that of other treating physicians reported in the literature, defines endoscopic resection as a safe and effective therapeutic choice for esophageal GCTs[10-12].
In conclusion, GCTs are uncommon esophageal tumors, which are mainly asymptomatic and located in the distal esophagus of middle-age subjects. Histology remains the gold standard for diagnosis of esophageal GCTs, while EUS may also provide important diagnostic information. Endoscopic resection or surgical excision should be performed due to the potential for malignancy.
Peer reviewers: Matthew James Schuchert, MD, FACS, Assistant Professor of Surgery, Heart, Lung and Esophageal Surgery Institute, University of Pittsburgh Medical Center, Shadyside Medical Building, 5200 Centre Avenue, Suite 715, Pittsburgh, PA 15232, United States; Vincenzo Villanacci, MD, 2nd Department of Pathology, Spedali Civili Piazzale Spedali Civili 1, 25100 Brescia, Italy
S- Editor Gou SX L- Editor Webster JR E- Editor Zhang DN
| 1. | Ordóñez NG. Granular cell tumor: a review and update. Adv Anat Pathol. 1999;6:186-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 124] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Parfitt JR, McLean CA, Joseph MG, Streutker CJ, Al-Haddad S, Driman DK. Granular cell tumours of the gastrointestinal tract: expression of nestin and clinicopathological evaluation of 11 patients. Histopathology. 2006;48:424-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 56] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Johnston J, Helwig EB. Granular cell tumors of the gastrointestinal tract and perianal region: a study of 74 cases. Dig Dis Sci. 1981;26:807-816. [PubMed] |
| 4. | Lack EE, Worsham GF, Callihan MD, Crawford BE, Klappenbach S, Rowden G, Chun B. Granular cell tumor: a clinicopathologic study of 110 patients. J Surg Oncol. 1980;13:301-316. [PubMed] |
| 5. | Goldblum JR, Rice TW, Zuccaro G, Richter JE. Granular cell tumors of the esophagus: a clinical and pathologic study of 13 cases. Ann Thorac Surg. 1996;62:860-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 65] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Orlowska J, Pachlewski J, Gugulski A, Butruk E. A conservative approach to granular cell tumors of the esophagus: four case reports and literature review. Am J Gastroenterol. 1993;88:311-315. [PubMed] |
| 7. | Subramanyam K, Shannon CR, Patterson M, Davis M, Gourley WK. Granular cell myoblastoma of the esophagus. J Clin Gastroenterol. 1984;6:113-118. [PubMed] |
| 8. | Kim DU, Kim GH, Ryu DY, Lee DG, Cheong JH, Lee BE, Song GA, Park do Y, Shin NR, I H. Endosonographic features of esophageal granular cell tumors using a high-frequency catheter probe. Scand J Gastroenterol. 2011;46:142-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Fanburg-Smith JC, Meis-Kindblom JM, Fante R, Kindblom LG. Malignant granular cell tumor of soft tissue: diagnostic criteria and clinicopathologic correlation. Am J Surg Pathol. 1998;22:779-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 505] [Cited by in RCA: 458] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 10. | De Ceglie A, Gatteschi B, Blanchi S, Scotto F, Pellecchia A, Conio M. Esophageal granular cell tumor treated by endoscopic mucosal resection. A case report and review of the literature. Dig Dis Sci. 2005;50:1875-1879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Sakamoto Y, Inamori M, Iida H, Hosono K, Endo H, Takahashi H, Koide T, Tokoro C, Abe Y, Kawana K. Esophageal granular cell tumor treated by endoscopic mucosal resection. Digestion. 2009;80:258-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Zhong N, Katzka DA, Smyrk TC, Wang KK, Topazian M. Endoscopic diagnosis and resection of esophageal granular cell tumors. Dis Esophagus. 2011;24:538-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |