Copyright
©2014 Baishideng Publishing Group Inc.
World J Gastroenterol. May 28, 2014; 20(20): 6180-6200
Published online May 28, 2014. doi: 10.3748/wjg.v20.i20.6180
Published online May 28, 2014. doi: 10.3748/wjg.v20.i20.6180
Figure 1 Suggested workflow for the assessment and management of post-transplant complications.
US: Ultrasound; MDCT: Multidetector computed tomography; ERC: Endoscopic retrograde cholangiography; PTC: Percutaneous transhepatic cholangiography; MDCTA: Multidetector computed tomography angiography; PHC: Primary hepatic complications.
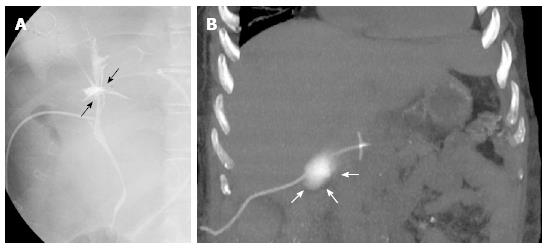
Figure 2 T-tube cholangiography.
A: The examination performed few days after liver transplant in a 28-year-old female with primary sclerosing cholangitis shows bile leakage at the anastomotic site (black arrows); B: Fifty-six year-old male recipient. Coronal maximum intensity projection reconstruction from unenhanced multidetector computed tomography scan shows contrast medium extravasation in the right subhepatic space, suggesting T-tube rupture (white arrows).
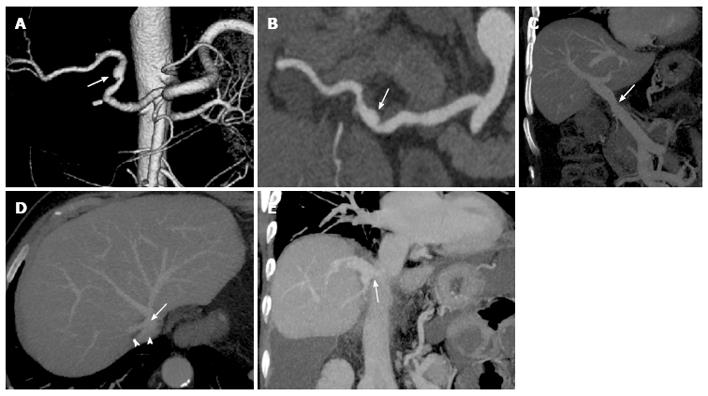
Figure 3 Common vascular anatomy after liver transplant on multidetector computed tomography images.
Volume rendering reconstruction (A) and curved-maximum intensity projection (MIP) reconstruction (B) show conventional “fish-mouth” end-to-end anastomosis (arrow) between donor and recipient arterial vessels. Portal vein (C) is usually reconstructed with an end-to-end anastomosis (arrow) between donor and recipient portal veins, as shown in the coronal MIP reconstruction. “Piggyback” reconstruction (D) of the inferior vena cava (IVC), in which an end-to-side anastomosis is performed between the donor IVC (arrow) and the common stump of recipient hepatic veins (arrowheads). The anastomotic site is indicated by the arrow in the coronal MIP reconstruction (E).
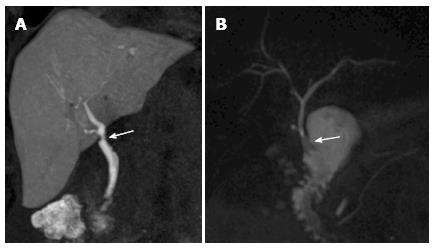
Figure 4 Biliary anatomy after liver transplant on magnetic resonance cholangiography images.
A: End-to-end anastomosis (arrow) between the donor common bile duct and the recipient common hepatic duct, as shown in this coronal T1-weighted magnetic resonance cholangiography (MRC) obtained after iv administration of an hepatobiliary contrast agent (gadoxetic acid); B: In the case of technical challenge, re-transplantation or primary sclerosing cholangitis as the cause of the transplant, choledochojejunostomy using a Roux-en-Y anastomosis (arrow) is performed, as shown in this maximum intensity projection reconstruction from a T2-weighted, 3D MRC examination.
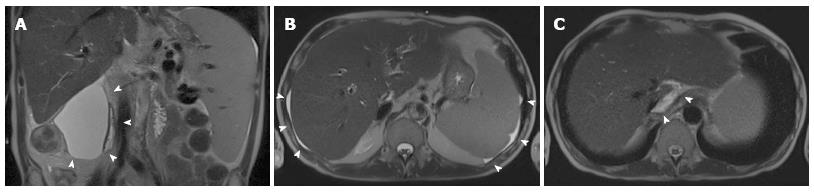
Figure 5 Normal postoperative fluid after liver transplant.
Coronal (A) and axial (B, C) T2-weighted single-shot turbo-spin echo magnetic resonance images acquired in a 48 year-old male few days after the intervention show a large fluid collection in the right subhepatic space (arrowheads in A) and a small amount of free fluid in the perihepatic and perisplenic space (arrowheads in B). It is not infrequent to observe a small fluid collection in the retrohepatic space, around the cavo-caval anastomosis (arrowheads in C).
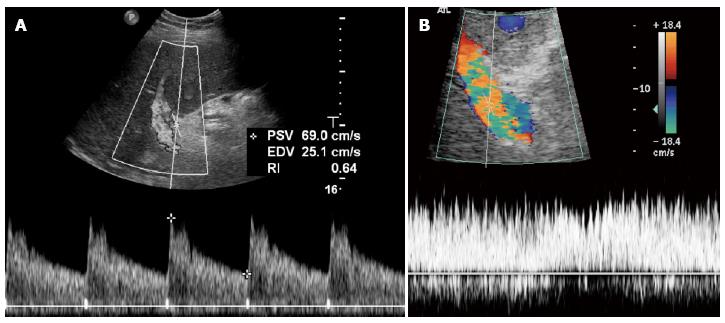
Figure 6 Normal findings doppler ultrasound after the transplant.
A: Normal hepatic artery waveform shows a rapid systolic upstroke followed by continuous diastolic flow; B: Portal flow is continuous, hepatopetal and monophasic, with mild respiratory variations that may be masked by increased velocity and flow turbulence, sometimes persisting even in the late post-operative period. PSV: Peak systolic velocity; EDV: End diastolic velocity; RI: Resistance index.
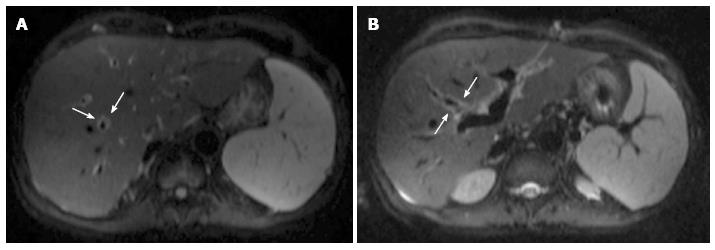
Figure 7 Periportal edema on magnetic resonance diffusion-weighted imaging.
Axial b = 500 s/mm2 diffusion-weighted images acquired on a 54-year-old male patient show a thin rim of hyperintense signal surrounding intrahepatic portal branches (arrows in A and B).
Figure 8 Sequels of hepatic artery thrombosis in a 28-year-old female patient transplanted for primary sclerosing cholangitis.
Coronal maximum intensity projection reconstruction (A) from multidetector computed tomography (MDCT) arterial angiographic phase shows abrupt interruption of the hepatic artery at the anastomotic site (arrow). The venous phase from the same MDCT examination (B) shows subhepatic and intrahepatic hypoattenuating fluid collections that were shown to be bilomas at T-tube cholangiography (arrows in C). Magnetic resonance imaging shows rapid evolution to massive liver infarction on axial T2-weighted single-shot turbo-spin-echo imaging (D), with multiple intra- and extrahepatic biliary strictures on magnetic resonance cholangiography (arrows in E). Patient required urgent re-transplantation.
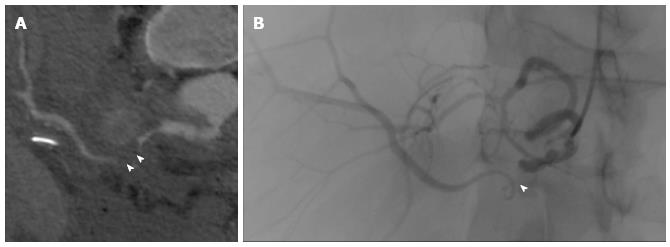
Figure 9 Hepatic artery stenosis.
Stenosis is visible (arrowheads) on curved thick-multiplanar reformation from multidetector computed tomography angiography (A) and digital subtraction angiography (B) performed to place a stent.
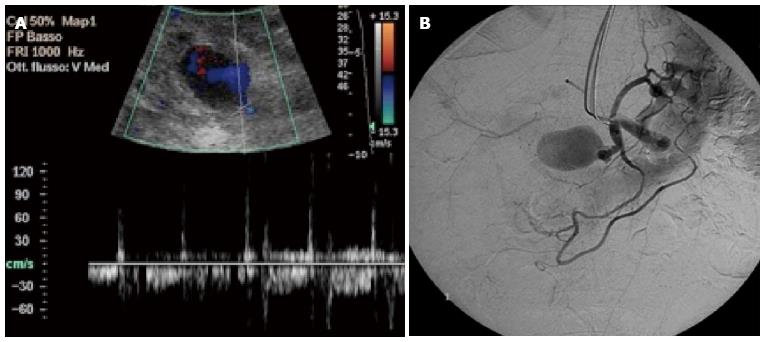
Figure 10 Pseudoaneurysm of the hepatic artery following angioplasty in a 63-year-old male transplanted patient.
A: Color Doppler examination shows a cystic formation near the hepatic artery, with a complex flow waveform related to partial thrombosis: high velocity peaks (blood inflow) are followed by diastolic reversal flow (outflow); B: Pseudoaneurysm has been confirmed by digital subtraction angiography by showing contrast filling.
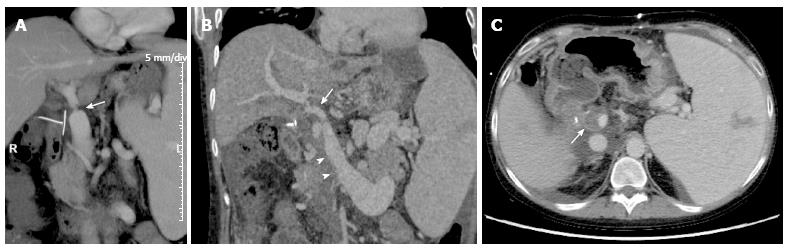
Figure 11 Portal vein complications on multidetector computed tomography images of the same patient of Figure 8.
A: Coronal maximum intensity projection (MIP) reconstruction shows a significant portal stenosis at the site of end-to-end anastomosis (arrow). Signs of portal hypertension such as splenomegaly and venous collaterals coexist; B: As shown in the coronal MIP reconstruction, thrombosis occurred after a few days, appearing as a filling defect extending from the superior mesenteric vein (arrowheads) to the portal trunk and portal bifurcation (arrow); C: Axial multidetector computed tomography image shows the partial filling defect in the portal lumen (arrow). R: Right.
Figure 12 Caval stenosis in a 54-year-old patient.
Sagittal maximum intensity projection reconstruction from multidetector computed tomography (A) shows a supranastomotic stenosis of the inferior vena cava (arrow) that is confirmed in the angiogram before (B) and after (C) stenting. A: Anterior; P: Posterior.
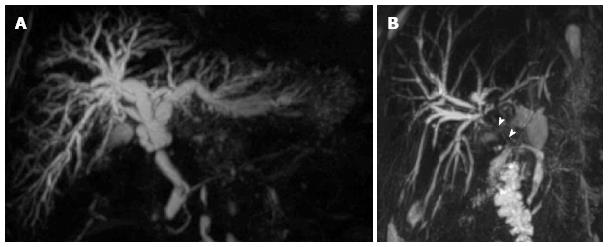
Figure 13 Biliary strictures on coronal maximum intensity projection reconstructions from volumetric magnetic resonance cholangiography.
A: Anastomotic stricture at the middle third of the extrahepatic bile duct in a 53-year-old female patient, with biliary dilation upstream; B: Anastomotic stricture extended to the proximal hepatic duct (arrowheads) in a 62 year-old patient with patent hepatic artery.
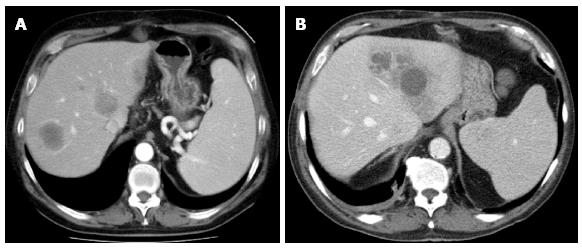
Figure 14 Multiple liver abscesses arising from infected bilomas in a 48-year-old recipient with hepatic artery stenosis.
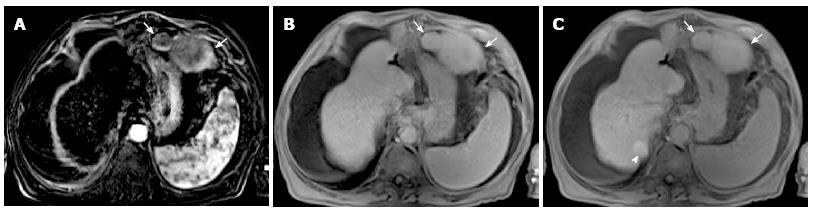
Figure 15 Recurrence of hepatocarcinoma in a 65-year-old human B virus infected male transplanted patient.
On the subtracted arterial phase magnetic resonance imaging (A) two mildly hypervascular lesions are visible in the extrahepatic region, between the stomach and left diaphragm (arrows). Lesions, that were histologically confirmed to be hepatocellular carcinoma, show absence of contrast wash-out on the venous phase (arrows in B) and hepatocellular contrast uptake in the hepatospecific phase (arrows in C). A regenerative nodule with intense contrast uptake is visible in the hepatospecific phase only (arrowhead in C).
- Citation: Girometti R, Como G, Bazzocchi M, Zuiani C. Post-operative imaging in liver transplantation: State-of-the-art and future perspectives. World J Gastroenterol 2014; 20(20): 6180-6200
- URL: https://www.wjgnet.com/1007-9327/full/v20/i20/6180.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i20.6180