Published online Jun 28, 2020. doi: 10.35713/aic.v1.i1.8
Peer-review started: May 20, 2020
First decision: June 12, 2020
Revised: June 22, 2020
Accepted: June 28, 2020
Article in press: June 28, 2020
Published online: June 28, 2020
Processing time: 47 Days and 18.4 Hours
The novel 2019 corona virus disease also called severe acute respiratory syndrome coronavirus 2 has caused a global pandemic and more than 2.5 million people have been affected globally with over 100000 deaths. The disease has caused an escalation in hospitalization with growing need for hospital beds and intensive care unit for severe cases. Recent evidence has shown that a significant proportion of cancer patients affected by the corona virus present with severe respiratory pneumonia-like illness with need for subsequent intensive care unit ventilation and higher mortality risk. This susceptibility may be due to the immunosuppressive state of patients with malignancy confounded by chemotherapy, immunotherapy and targeted therapy. Many solid tumors (lung cancer, pancreatic cancer) as well as hematological malignancies (leukemias) may require prompt diagnosis and treatment based on the disease aggression and progression. Many centers lack clear guideline on the management of cancer during the pandemic. The objective of this review is to synthesize the available literature and provide recommendations on the management of various soft tissue and hematological malignancies. The review will also assess the management guidelines for hospitalized cancer patients; cancer patients in the outpatient setting as well as available modalities for follow-up.
Core tip: Management of cancer patients during the novel 2019 corona virus disease pandemic is challenging. The need of surgery, chemotherapy or radiation therapy places the patients at risk of nosocomial transmission. The myelosuppressive effect of chemotherapy and radiation may increase the morbidity and mortality associated with the coronavirus. Therefore, cancer treatment should be stratified based on the benefits and risk of intervention. Avoiding unnecessary procedures, social distancing, hand hygiene and mask wear could reduce the associated disease burden.
- Citation: Cassell III AK, Cassell LT, Bague AH. Management of cancer patients during the COVID-19 pandemic: A comprehensive review. Artif Intell Cancer 2020; 1(1): 8-18
- URL: https://www.wjgnet.com/2644-3228/full/v1/i1/8.htm
- DOI: https://dx.doi.org/10.35713/aic.v1.i1.8
The novel 2019 corona virus disease (COVID-19) also called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has caused a global pandemic and more than 2.5 million people have been affected globally with over 100000 deaths[1]. The corona virus is highly contagious and transmitted from person to person through direct contact of respiratory secretions from coughing or sneezing[2]. The disease has caused an escalation in hospitalization with growing need for hospital beds and intensive care unit for severe cases. During this period, the oncological practice has faced enormous challenges.
Recent evidence has shown that a significant proportion of cancer patients affected by the corona virus present with severe respiratory pneumonia-like illness with need for subsequent intensive care unit (ICU) ventilation along with higher mortality risk[3]. Study by Liang et al[4] revealed that cancer patients with corona virus progress more rapidly to severe disease than non-cancer patients. This susceptibility may be due to the immunosuppressive state of patients with malignancy confounded by chemotherapy, immunotherapy and targeted therapy[1]. Most cancers centers are now weighing the benefit of cancer treatment and risk of exposure to the corona virus.
Many solid tumors (lung cancer, pancreatic cancer) as well as hematological malignancies (leukemias) may require prompt diagnosis and treatment based on the disease aggression and progression[5]. However, low risk early-stage breast cancer, prostate cancer and cervical cancer may be amenable to some delay in treatment. The major risks to cancer patients remain the availability of hospital beds, changes of resource allocation and the lack of an appropriate guideline for cancer care during a pandemic[6]. Even if cancer treatment is to continue, the risk of nosocomial infection remains a concern during the pandemic.
Currently, many oncological societies and cancer networks have assessed the risk of COVID-19 infection for cancer patients and formulated practice recommendation for oncological care including neoadjuvant therapy, surgery, adjuvant therapy, immunotherapy, targeted therapy and palliative care. Several soft tissue malignancies have now been stratified according to priority or risk level predicting the need for either urgent intervention, delayed intervention or deferment of intervention after the pandemic.
The objective of this review is to synthesize the available literature and provide recommendations on the management of various soft tissue and hematological malignancies. The review will also assess the management guidelines for hospitalized cancer patients; cancer patients in the outpatient setting as well as available modalities for follow-up.
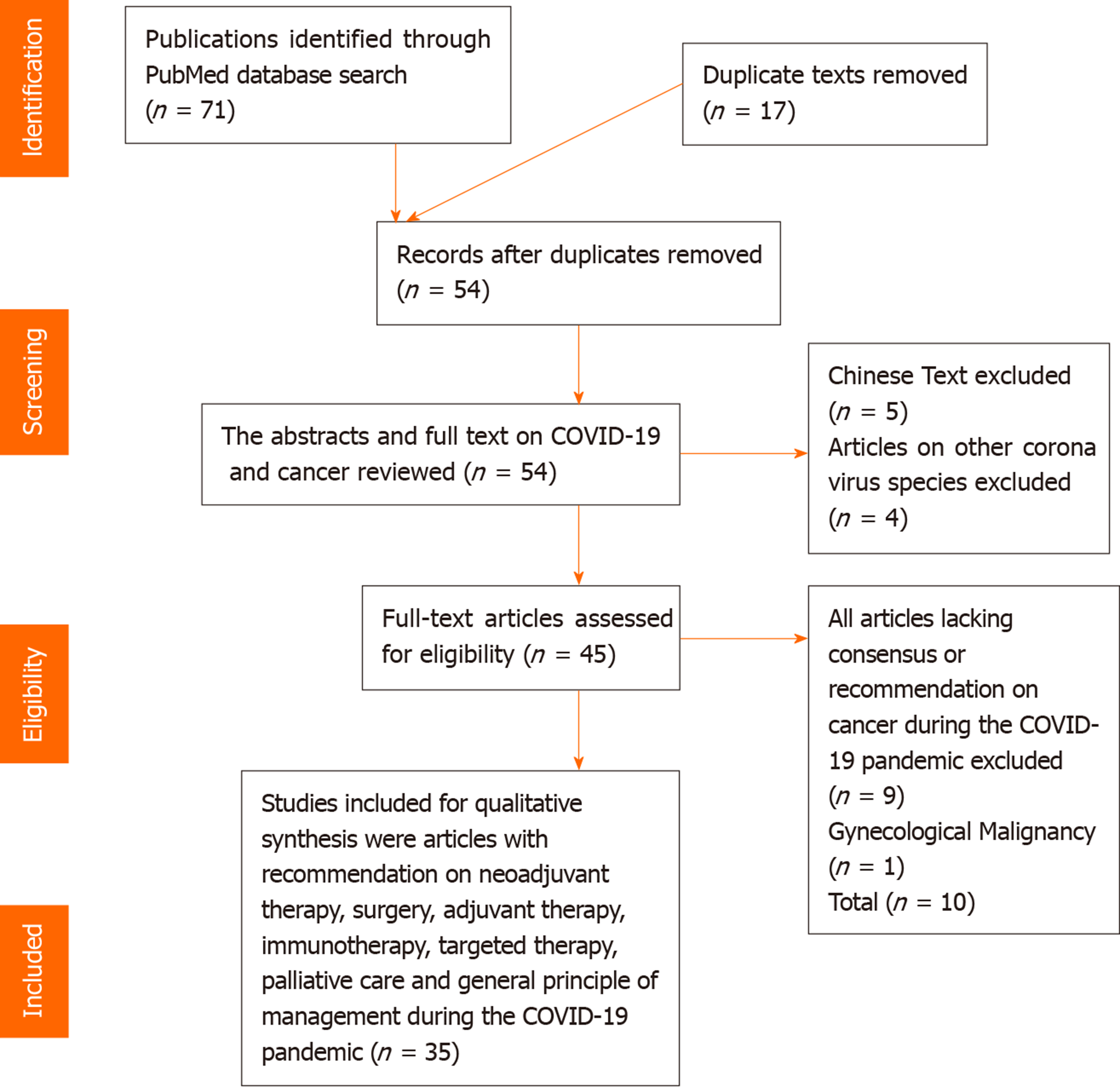
A comprehensive literature search of COVID-19 was conducted using the PubMed database from December 2019 until the May 11, 2020. The keyword used was “managing cancer patients during the COVID-19 pandemic”. A total of 71 articles were retrieved after using free full-text filter in the PubMed database. Both the English and French literatures were included for analysis. Duplicated articles on COVID-19 during the search were also excluded. All articles published in the Chinese language were also excluded from the study. The title, abstract and full text of the retrieved publication were screened for eligibility. A snapshot of the search in PubMed data was presented in Figure 1.
About 37 texts met the desired objective and were included in the review for analysis. All soft tissue malignancies with proposed management recommendation on neoadjuvant therapy, surgery, adjuvant therapy, immunotherapy, targeted therapy and palliative care were included in the study. All commentaries, editorials, reviews, group consensus and original article with recommendation on cancer management during the COVID-19 pandemic were considered for inclusion. All accepted articles, with published online proof reviewing recommendation of cancer management were included for analysis. A PRISMA flow chart was used to summarize the selection process (Figure 2).
Out of the 35 papers retrieved, 34 articles were published in the English language with only one in French. The result included review recommendations and guidelines, commentaries, editorials, letters and correspondence. The selected articles provided various recommendations for cancer care during this current corona virus crisis assessing the benefit of treatment against the risk of contracting the virus.
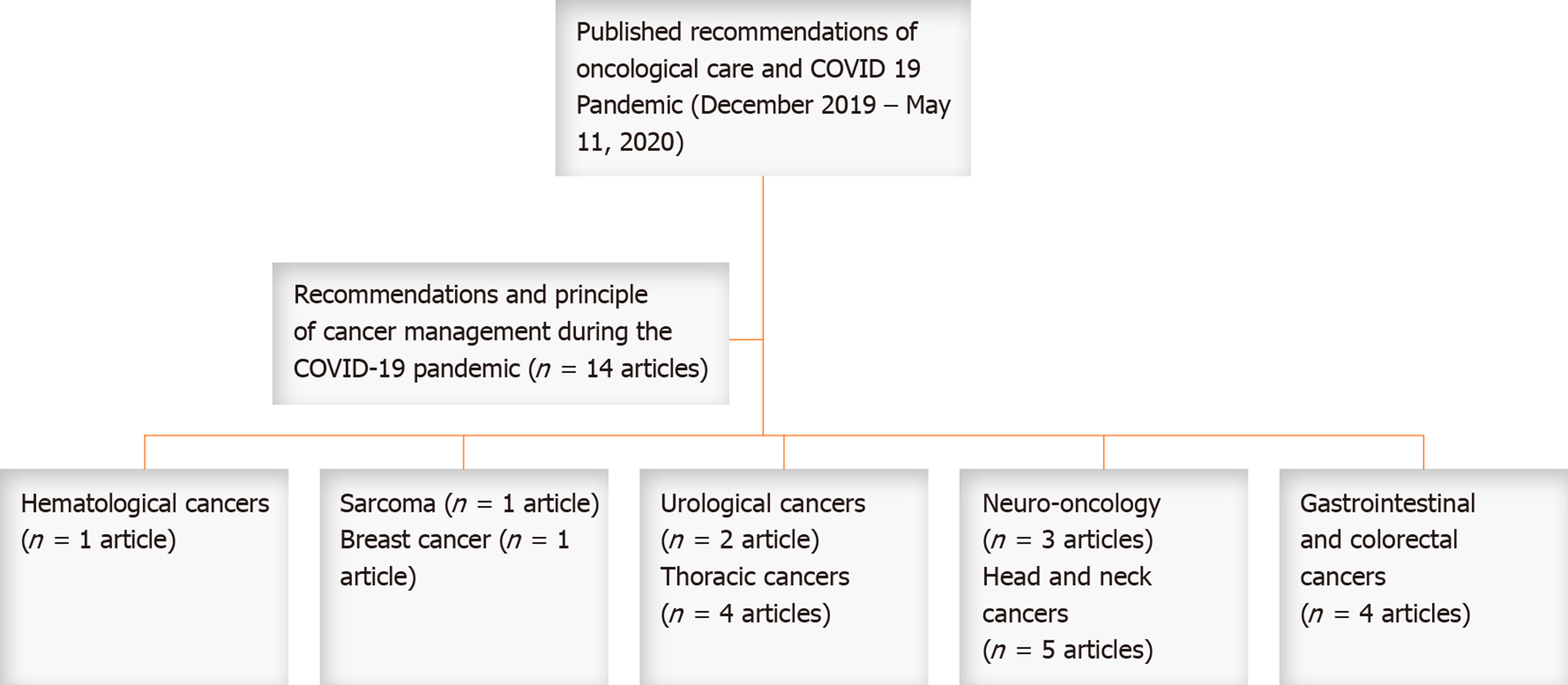
The qualitative analysis included articles with data on COVID-19 epidemiology, recommendations for hospitalized cancer patients, outpatient settings and oncological follow-up during the COVID-19 pandemic. There was also specific recommendation for specific types of malignancy during the pandemic including hematological cancers, sarcoma, breast cancer, urological cancers, thoracic cancers, neuro-oncology, head and neck cancers, gastrointestinal cancers and colorectal cancer (Figure 3). A qualitative analysis of the various ‘malignancies is synthesized below.
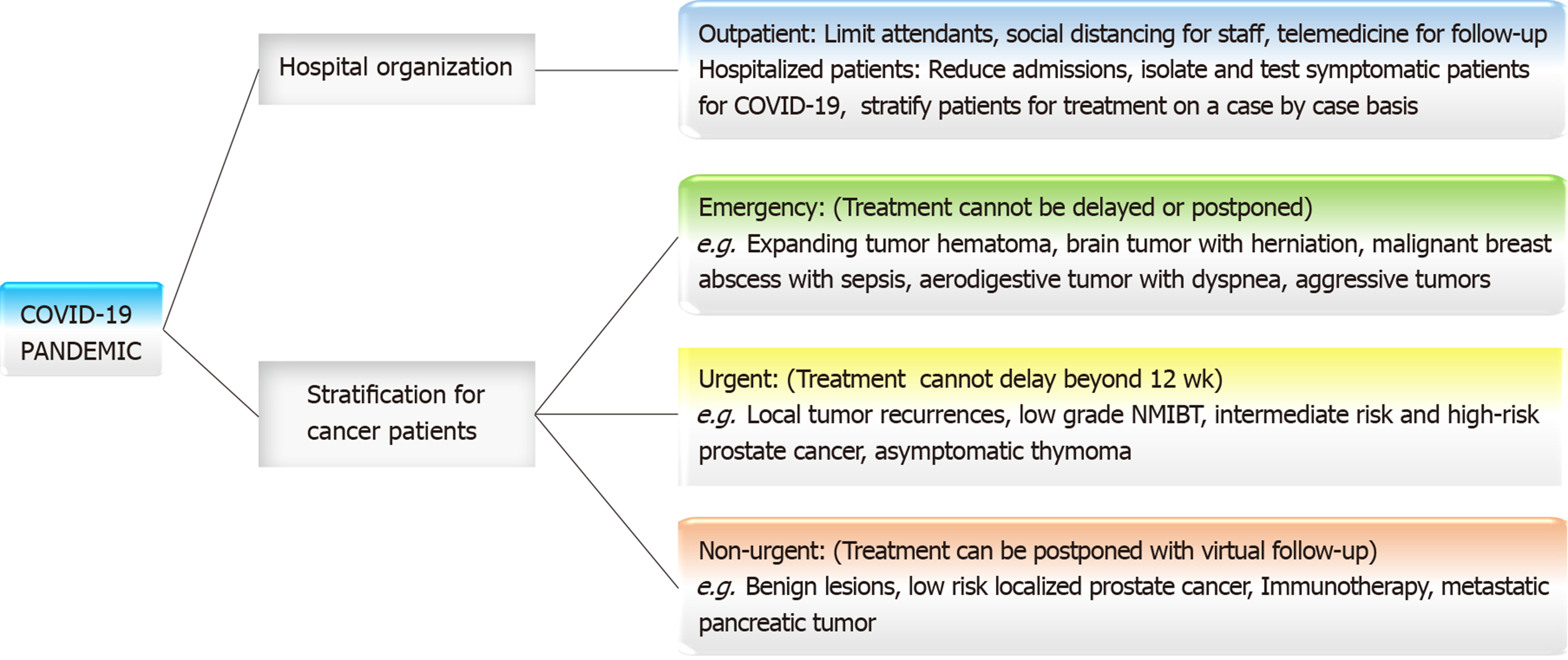
Due to the immunosuppressive state of cancer patients most oncological practices are now informing all cancer patients about signs and symptoms of COVID-19 (fever, cough, dyspnea, fatigue)[7] and advocating strong adherence to social distancing principle[1,5]. Report from a Collaborative Cancer Network in the United States by Ueda et al[8] have demanded that all cancer patients are triaged for respiratory symptoms as part of a mandatory practice for this current outbreak. A systematic review by Moujaess et al[9] found that cancer patients may present with atypical clinical and radiological features that could be confused for SARS-CoV-2 infection causing a diagnostic dilemma.
Management in outpatient settings: An International Collaborative Group involving several cancer centers around the world have proposed that clinic visits should be restricted, and universal precaution is taken[6]. According to Al-Shamsi et al[6], clinic attendants should be limited as much as possible because the coronavirus could be asymptomatic in up to 33.3% of patients. To minimize occupational hazard, health care workers wear personal protection equipment (PPE) and maintain health protocols to ensure infection control and avoid nosocomial transmission[1]. Shankar et al[1] and Motlagh et al[2] recommended that patients with cancer could be selectively treated provided there is a guideline for risk stratification to prevent unnecessary infection from COVID-19 in hospital settings[5]. According to Al-Shamsi et al[6] and Gosain et al[7], patients on intravenous chemotherapy can be switched to appropriate oral chemotherapy if feasible. Decision should be considered on a case by case basis. Home drawn blood service is now being recommended to monitor side effect from chemotherapy[6]. For symptom management and chemotherapy supervision, telemedicine is being strongly advocated. The Gustave Roussy cancer center in France is now utilizing telemedicine for monitoring and organizing referrals for cancer patients with COVID-19[10]. According to Scotté et al[10] telemedicine is also being used by other institution in France to monitor cancer patients on oral therapy. Mei et al[11] reported that the Cancer Center of Wuhan in China have now attended to more than 80000 cancer patients using the telemedicine platform. Nonetheless, the limitation of telemedicine remains the inability to perform a physical examination. Patients receiving curative radiation therapy are encouraged to continue[3]. Patients who have a known contact can continue treatment in a separate compartment.
Hospitalized patients with cancer: The management of hospitalized patients during the pandemic is complicated. Strict safety measures should be ensured by all health care provider to avoid nosocomial transmission[11]. The number of ward staff should be reduced as much as possible[12]. Patients that are symptomatic should be isolated and tested. If results are positive for SARS-CoV-2 infection, the patient should be moved to the COVID-19 disease treatment unit according to the safety protocols. According to Motlagh et al[2] cancer patients are at higher risk vascular thrombosis therefore, mobilizing the patients is crucial during these isolations. Delaying surgery and chemotherapy in these setting is reasonable due to the high demand of ICU beds and ventilation[3,4]. Conversely, an editorial by Peng et al[13] stated that the cessation or continuation of chemotherapy in the setting of COVID-19 infection remains debatable. This was based on reports that cancer patients coinfected with human immunodeficiency virus and hepatitis B did not experience viral reactivation during chemotherapy. A multi-center study by Tan et al[12] recommended risk stratification for cancer patients requiring surgery as either emergency or selective operation. Rapidly progressing and compressive tumors with imminent risk of rupture and hemorrhage should be operated as an emergency[12]. According to Gosain et al[7] patient who have received neoadjuvant therapy awaiting tumor resection can be addressed on a selective basis considering the hospital capacity, cancer stage and the burden of the prevailing coronavirus pandemic. Intervention for cancer can be avoided for patients that are clinically stable or those requiring palliative care during the peak of the virus epidemic.
Cancer in older patients: Data have shown that older cancer patients have higher risk of respiratory complications and death following a viral infection therefore increase barrier methods, mask wearing, and hand hygiene should be provided for this population[3,4,14]. The report by Falandry et al[14] from France was inconclusive whether older cancer with COVID-19 infection should be offer resuscitation when needed considering the high demand of ICU beds and ventilation. This calls into question ethical issues that differs across center based on the disease burden and available resources for treatment. However, it is being advocated that older cancer patients should not become systemically excluded from oncological care with the theory of their impending risk of severe disease when infected with the coronavirus[3,14].
Specific recommendation for hematological malignancies: A multi-center review in Brazil by Perini et al[15] provided recommended management algorithm for patients with lymphoid malignancies during the coronavirus outbreak. All lymphoid malignancies in remission are advised to be postponed with virtual follow-up and counseling. Patients with aggressive non-Hodgkin lymphoma like Burkitt’s lymphoma, plasmoblastic lymphoma, lymphoblastic lymphoma, mantle cell lymphoma and peripheral T-cell lymphoma are recommended immediate treatment using the appropriate regimen[15]. Granulocyte stimulating agents (G-CSF) should be considered strongly to avoid febrile neutropenia during the COVID-19 pandemic. Nonetheless, patients with indolent lymphoma like chronic lymphocytic lymphoma and follicular lymphoma can benefit from watchful waiting or a less intense regimen including oral chemotherapies can be considered. Patients with relapse and refractory diseases can be managed on an outpatient basis. Treatment should not be delayed for patients with Hodgkin lymphoma, but less intensive chemotherapeutic regimen should be initiated.
Specific recommendation for sarcoma: The French Sarcoma in collaboration with the European Society for Medical Oncology (ESMO) by Penel et al[16] proposed several management recommendations for sarcoma patients during the COVID-19 crisis. Operable patients with soft tissue sarcoma, visceral sarcoma and bone sarcoma without symptoms of coronavirus infection should not have their surgery delayed[16]. Patients with Ewing’s sarcoma, osteosarcoma, alveolar sarcoma and embryonal rhabdomyosarcoma without symptoms of COVID-19 infection should proceed with standard treatment including neoadjuvant chemotherapy, surgery and adjuvant chemotherapy[16]. Patients with advanced soft tissue sarcoma should receive standard chemotherapy along with G-CSF to avoid neutropenia.
Specific recommendation for breast cancer: Based on the challenges of cancer care during the recent coronavirus outbreak, the Commission on Cancer, the National Accreditation Program for Breast Centers, American Society of Breast Surgeons, the National Comprehensive Care Net-work, and the American College of Radiology have stratified patients with breast cancer into priority categories[17]. These recommenda-tions were based on individual patient’s disease, comorbidities and treatment benefits.
Priority A category are patients that are clinically unstable with life threatening disease like breast abscess and sepsis or expanding breast hematoma. Immediate operative drainage is warranted for breast abscess; breast tumor hematoma should be evacuated with control of the bleeder.
Patients priority B category do not have life threatening conditions, but their surgery should not be deferred after the pandemic. A short delay of 6-12 wk may not adversely affect treatment outcome in this group. Patients in this group include hormone receptor positive patients, mastectomy flap ischemia, patients completing neoadjuvant therapy and suspected local recurrences[17].
Individuals in priority C category are patients whose intervention can be deferred indefinitely till after the epidemic without adversely affecting treatment outcome. These include hormone receptor +/- ductal carcinoma in situ, clinical stage I breast cancers, benign breast lesions, prophylactic mastectomies and discordant benign biopsies[17].
Specific recommendation for urological cancers: The Cancer Committee of the French Association of Urology (CCFAU) published a report by Méjean et al[18] with formulated guidelines for the management of urological malignancies during the COVID-19 pandemic.
Localized renal cancer along with renal cyst Bosniak I and II should be postponed and undergo quarterly surveillance. Patients with locally advanced renal cancer or symptomatic tumor with pain and hematuria should have their surgery prioritized. Good prognosis metastatic renal cancer can benefit from immunotherapy with virtual follow-up from home. Poor prognosis metastatic renal cancer can receive immunotherapy, but the benefit should be balanced against the risk of toxicity[18]. Otherwise, palliative care is a reasonable alternative.
According the CCFAU guideline, transurethral resection for low-grade, low volume, non-muscle invasive bladder tumor without out evidence of carcinoma in situ from urine cytology can be delayed for 3 mo. Patients with muscle invasive bladder cancer or non-muscle invasive disease refractory to bacille Calmette-Guerin therapy should have radical cystectomy within 3 mo following diagnosis[18]. Neoadjuvant chemotherapy is discouraged in this setting.
According to Méjean et al[18] low risk localized prostate cancer should preferably undergo surveillance during the outbreak. A systematic review by radio-oncology groups in the United Kingdom (UK) and the United States of America (USA) by Zaorsky et al[19] recommended that radiotherapy for low risk prostate cancer can be delayed until safe. The CCFAU recommended that patients with intermediate risk localized prostate cancer, treatment can be delayed within 2 mo. These include radical prostatectomy, extremal beam radiotherapy and brachytherapy. For patients with high risk and localized advanced prostate cancer, surgery cannot be delayed more than 2 mo and hormonotherapy should not be delayed. The radio-oncology group in UK and USA[19] recommended a delay of 1-3 mo for intermediate risk prostate cancer, high risk prostate cancer, postprostatectomy and nodal cancer requiring radiation therapy. The initiation of androgen deprivation therapy (ADT) for high risk prostate cancer can help in the delay of intervention. However, if delay is not feasible, external beam radiotherapy is preferred with the shortest fractionation schedule. Nevertheless, the benefit of treatment, the toxicity of treatment as well as the risk of contracting COVID-19 infection are important parameters to assess to limit morbidity and mortality.
Patients with hormone sensitive metastatic prostate cancer can continue ADT and newer generation hormonotherapy (apalutamide or enzalutamide)[18]. Patients with castrate resistant metastatic prostate cancer treated who did not receive second generation hormonotherapy can continue ADT with enzalutamide. Chemotherapy and steroid should be avoided to prevent unwanted toxicity. For patients with castrate resistant metastatic prostate cancer who received second generation hormonotherapy, the risk and benefits of initiating chemotherapy can be discussed (docetaxel, carbazitaxel)[18]. G-CSF should be considered to avoid neutropenia in patient on chemotherapy. According to Zaorsky et al[19] radiotherapy for low volume metastatic cancer and oligometastases can be delayed up to 6 mo for patients on ADT.
Specific recommendation for thoracic cancers: A consensus statement from the Thoracic Surgery Outcomes Research Network formulated several recommendations for thoracic cancers based on the high usage of ICU beds, ventilators and PPE during the COVID-19 pandemic. Lung cancer ≥ 2-cm, node positive lung cancer, high risk chest wall tumors, symptomatic mediastinal tumors and invasive esophageal cancer should have surgery prioritized in the soonest possible time[20]. Yet, lung cancer less than 2-cm, indolent histology, asymptomatic thymoma, pulmonary oligometastases, bronchoscopy, upper endoscopy and tracheostomy can be deferred for up to 3 mo[20].
An ESMO publication by Banna et al[21] also stratified non-small cell lung cancer and small cell lung cancer for treatment intervention. For locally advanced resectable non-small cell lung cell, neoadjuvant chemotherapy, chemotherapy + radiotherapy and immunotherapy should not delay treatment when possible[21]. Nonetheless, Chemotherapy should be withheld in patients at significant risk of COVID-19 infection. Patients with locally advanced to advanced small cell lung cancer should continue with standard treatment. Treatment should be delayed in patients at risk of COVID-19 infection or those requiring long period of immunotherapy. According to Zhao et al[22], immunotherapy is associated with significant pulmonary toxicity as such should be suspended or postponed in patients with stable disease.
Study by Mazzone et al[23] also provided a consensus statement on the management of lung nodule during the epidemic. There was almost a unanimous agreement that evaluation should be delayed for pulmonary nodule discovered incidentally or during screening that are likely indolent[23]. The expert group from this study generally agreed that surgery for localized non-small cell lung cancer can be postponed if there no evidence of an aggressive disease or progression.
Specific recommendation for brain cancers: A correspondence by Zacharia et al[24] stratified patients with brain tumor needing surgery into emergent, urgent and semi-urgent. In the setting of a brain tumor with impending herniation or hydrocephalus, surgery should be performed as soon as possible[24]. All patients should be considered COVID-19 positive until otherwise. Enhanced PPE is required for all operating staff and health care providers. High grade malignancies or tumor presenting with progressive neurological deficits should be operated urgently between 2 to 7 d. Attempt COVID-19 testing preoperatively if possible.
Patients with asymptomatic or benign brain lesions can have their surgery delayed up to 4 wk. Patient should be properly screened, and every health precaution should be maintained including self-quarantine for 14 d before surgery. Studies by Mohile et al[25] and Bernhardt et al[26] also formulated guidelines for patients with gliomas during the COVID-19 pandemic. According to Mohile et al[25] newly diagnosed glioma should continue with their standard of care but with precaution to avoid nosocomial transmission. Therapy for recurrent glioma should be delayed and certain chemotherapeutic agents avoided[25,26].
Specific recommendation for head and neck cancers: The French consensus on the standard of care of head and neck surgery by Fakhry et al[27] stratified patients into 3 groups. Cancer patients with life-threatening emergencies (dyspnea, hemorrhage) where classified as Group A and required immediate treatment. The SARS-COV-2 swab test along with a chest CT-san in 24 h is advisable before surgery.
Aggressive cancer of the salivary gland and aerodigestive tract for whom treatment postponement for a month will adversely affect outcome of the disease were considered as Group B. If tracheostomy is not required, the surgery should be delayed, and all necessary investigation done[27].
Well differentiated thyroid cancer, non-progressive skin cancer and slow growing salivary gland tumor were considered as Group C for which treatment can be postponed for 6 to 8 wk without adversely affecting outcome.
A review by a head and neck oncology group Day et al[28] proposed that hospitals should provide preoperative, intraoperative and postoperative management algorithm to ensure patient and staff safety. They proposed several reasons for strict precautions by head and neck surgeons. The coronavirus replicates in the nasal cavities, nasopharynx and oropharynx which are sites for routine head and neck surgery[28]. The coronavirus is aerosolized for at least three hours. Most head and neck surgeries require general anesthesia which entail aerosol generating procedures like bag-valve mask ventilation and intubation. The team recommended that most high-risk procedures should be performed with an N95 mask or a powered air-purifying respirator. The disadvantage is that these masks are uncomfortable to surgeons for long standing procedures.
A guideline consensus from the European Society for Radiotherapy and Oncology and the American Society of Radiation Oncology agreed that patients with locally advanced squamous cell carcinoma of the oropharynx and larynx scan continue radiation therapy with concurrent chemotherapy[29].
According to Sharma et al[30] the management of head and neck cancer in elderly patient during the COVID-19 pandemic is very challenging. About 70% of death from head and neck cancer occur in patients over 70 years. Moreover, 95% of COVID-19 death occur in patients over 60 years and about 50% in patients over 80 years alone[30]. Therefore, treatment decision for this group should be individualized considering disease severity, comorbidity and risk of coronavirus infection (Figure 4).
Report by Salari et al[31] conveyed that multidisciplinary meeting for head and neck cancer in Iran have now been moved to a virtual platform, since the COVID-19 pandemic. During these virtual meetings, cancer surgeons, head and neck surgeons, maxillofacial surgeons, medical oncologists, radiologist, radiotherapist and nuclear medicine specialist discuss the benefit and risk of treatment and patient are prioritized for the appropriate treatment[31].
Specific recommendation for gastrointestinal and colorectal cancers: An editorial by Patel et al[32] recently outlined three groups prioritizing the treatment of cancer patient during the COVID-19 pandemic. This stratification had been previously released by the American Society of Clinical Oncology. Group 1 were patients who completed treatment or patients with controlled disease. Clinics visits were recommended to be delayed and telemedicine platform are to be used for follow-up. Group 2 were patients undergoing active neoadjuvant or adjuvant treatment with curative intent. Patients were encouraged to continue treatment while minimizing the risk of nosocomial transmission with hand hygiene, PPE for staff and social distancing[32]. Patients undergoing treatment for metastatic disease were considered as Group 3. Delaying treatment in this group was considered reasonable if it did not adversely affect the disease outcome. Another multi-center radio-oncology report by Tchelebi et al[33] classified the provision of radiotherapy during the pandemic for several gastrointestinal cancers including esophageal cancer, gastric cancer, hepatocellular cancer, cholangiocarcinoma, pancreatic cancer, rectal cancer and anal cancer. The group recommended that operable esophageal cancer, advanced gastric cancer, locally advanced operable rectal cancer and hepatocellular cancer can receive radiation therapy reducing the period of fractionation. Radiotherapy was not recommended in operable or resected gastric cancer, operable cholangiocarcinoma and resectable pancreatic tumor[33]. These recommendations were made to guide treatment decision; to either reduce disease progression or avoid unnecessary exposure to the COVID-19 infection. A report by Romesser et al[34] from the Memorial Sloan Kettering Cancer Center suggested that short course radiation therapy (SCRT) can provide quality and efficient oncological care for patients while reducing the risk of exposure to the COVID-19 infection. A report from a multinational colorectal cancer group in Europe by Di Saverio et al[35] proposed that surgery during the COVID-19 pandemic should be aligned by clear perioperative protocols. The group advocated safe transfer of patients between the ward and the operating theater with the proper use of PPE by staffs and coordinated transport system between the theater staff and ward staff[35].
Management of cancer patients during the COVID-19 pandemic is challenging. The need of surgery, chemotherapy or radiation therapy places the patients at risk of nosocomial transmission. The myelosuppressive effect of chemotherapy and radiation may increase the morbidity and mortality associated with the coronavirus. Therefore, cancer treatment should be stratified based on the benefits and risk of intervention. Avoiding unnecessary procedures, social distancing, hand hygiene and mask wear could reduce the associated disease burden.
Special thanks to Department of Surgery, Liberia College of Physicians and Surgeons.
Manuscript source: Invited manuscript
Corresponding Author's Membership in Professional Societies: American College of Surgeon (Associate Fellow); American Urological Association (Member); Faculty of Surgical Trainer; Royal College of Edinburgh (Member); and International College of Surgeons (Fellow).
Specialty type: Oncology
Country/Territory of origin: Senegal
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Fusaroli P, Li J, Yang JS S-Editor: Wang JL L-Editor: A E-Editor: Liu JH
| 1. | Shankar A, Saini D, Roy S, Mosavi Jarrahi A, Chakraborty A, Bharti SJ, Taghizadeh-Hesary F. Cancer Care Delivery Challenges Amidst Coronavirus Disease - 19 (COVID-19) Outbreak: Specific Precautions for Cancer Patients and Cancer Care Providers to Prevent Spread. Asian Pac J Cancer Prev. 2020;21:569-573. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 105] [Cited by in RCA: 96] [Article Influence: 19.2] [Reference Citation Analysis (0)] |
| 2. | Motlagh A, Yamrali M, Azghandi S, Azadeh P, Vaezi M, Ashrafi F, Zendehdel K, Mirzaei H, Basi A, Rakhsha A, Seifi S, Tabatabaeefar M, Elahi A, Pirjani P, Moadab Shoar L, Nadarkhani F, Khoshabi M, Bahar M, Esfahani F, Fudazi H, Samiei F, Farazmand B, Ahmari A, Vand Rajabpour M, Janbabaei G, Raisi A, Ostovar A, Malekzadeh R. COVID19 Prevention & Care; A Cancer Specific Guideline. Arch Iran Med. 2020;23:255-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 3. | Al-Quteimat OM, Amer AM. The Impact of the COVID-19 Pandemic on Cancer Patients. Am J Clin Oncol. 2020;43:452-455. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 178] [Cited by in RCA: 233] [Article Influence: 46.6] [Reference Citation Analysis (1)] |
| 4. | Liang W, Guan W, Chen R, Wang W, Li J, Xu K, Li C, Ai Q, Lu W, Liang H, Li S, He J. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335-337. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3332] [Cited by in RCA: 3125] [Article Influence: 625.0] [Reference Citation Analysis (0)] |
| 5. | Kutikov A, Weinberg DS, Edelman MJ, Horwitz EM, Uzzo RG, Fisher RI. A War on Two Fronts: Cancer Care in the Time of COVID-19. Ann Intern Med. 2020;172:756-758. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 252] [Cited by in RCA: 302] [Article Influence: 60.4] [Reference Citation Analysis (0)] |
| 6. | Al-Shamsi HO, Alhazzani W, Alhuraiji A, Coomes EA, Chemaly RF, Almuhanna M, Wolff RA, Ibrahim NK, Chua MLK, Hotte SJ, Meyers BM, Elfiki T, Curigliano G, Eng C, Grothey A, Xie C. A Practical Approach to the Management of Cancer Patients During the Novel Coronavirus Disease 2019 (COVID-19) Pandemic: An International Collaborative Group. Oncologist. 2020;25:e936-e945. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 443] [Cited by in RCA: 458] [Article Influence: 91.6] [Reference Citation Analysis (0)] |
| 7. | Gosain R, Abdou Y, Singh A, Rana N, Puzanov I, Ernstoff MS. COVID-19 and Cancer: a Comprehensive Review. Curr Oncol Rep. 2020;22:53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 162] [Cited by in RCA: 196] [Article Influence: 39.2] [Reference Citation Analysis (0)] |
| 8. | Ueda M, Martins R, Hendrie PC, McDonnell T, Crews JR, Wong TL, McCreery B, Jagels B, Crane A, Byrd DR, Pergam SA, Davidson NE, Liu C, Stewart FM. Managing Cancer Care During the COVID-19 Pandemic: Agility and Collaboration Toward a Common Goal. J Natl Compr Canc Netw. 2020;1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 325] [Article Influence: 65.0] [Reference Citation Analysis (0)] |
| 9. | Moujaess E, Kourie HR, Ghosn M. Cancer patients and research during COVID-19 pandemic: A systematic review of current evidence. Crit Rev Oncol Hematol. 2020;150:102972. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 154] [Cited by in RCA: 146] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 10. | Scotté F, Minvielle E, Mir O, André F, Barlesi F, Soria JC. A patient reported outcome platform, a useful tool to improve monitoring and effective management of Covid-19-positive patients with cancer. Eur J Cancer. 2020;132:1-4. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 11. | Mei H, Dong X, Wang Y, Tang L, Hu Y. Managing patients with cancer during the COVID-19 pandemic: frontline experience from Wuhan. Lancet Oncol. 2020;21:634-636. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 12. | Tan J, Yang C. Prevention and control strategies for the diagnosis and treatment of cancer patients during the COVID-19 pandemic. Br J Cancer. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 13. | Peng L, Zagorac S, Stebbing J. Managing patients with cancer in the COVID-19 era. Eur J Cancer. 2020;132:5-7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Falandry C, Filteau C, Ravot C, Le Saux O. Challenges with the management of older patients with cancer during the COVID-19 pandemic. J Geriatr Oncol. 2020;11:747-749. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Perini GF, Fischer T, Gaiolla RD, Rocha TB, Bellesso M, Teixeira LLC, Delamain MT, Scheliga AAS, Ribeiro GN, Neto JV, Baiocchi OCCG, Abdo ANR, Arrais-Rodrigues C, Fogliatto LM, Bigni RS, Schaffel R, Biasoli I, Pereira J, Nabhan SK, Souza CA, Chiattone CS; Associação Brasileira de Hematologia, Hemoterapia e Terapia Celular (ABHH). How to manage lymphoid malignancies during novel 2019 coronavirus (CoVid-19) outbreak: a Brazilian task force recommendation. Hematol Transfus Cell Ther. 2020;42:103-110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 16. | Penel N, Bonvalot S, Minard V, Orbach D, Gouin F, Corradini N, Brahmi M, Marec-Bérard P, Briand S, Gaspar N, Llacer C, Carrère S, Dufresne A, Le Cesne A, Blay JY. French Sarcoma Group proposals for management of sarcoma patients during the COVID-19 outbreak. Ann Oncol. 2020;31:965-966. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 17. | Dietz JR, Moran MS, Isakoff SJ, Kurtzman SH, Willey SC, Burstein HJ, Bleicher RJ, Lyons JA, Sarantou T, Baron PL, Stevens RE, Boolbol SK, Anderson BO, Shulman LN, Gradishar WJ, Monticciolo DL, Plecha DM, Nelson H, Yao KA. Recommendations for prioritization, treatment, and triage of breast cancer patients during the COVID-19 pandemic. the COVID-19 pandemic breast cancer consortium. Breast Cancer Res Treat. 2020;181:487-497. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 190] [Cited by in RCA: 274] [Article Influence: 54.8] [Reference Citation Analysis (0)] |
| 18. | Méjean A, Rouprêt M, Rozet F, Bensalah K, Murez T, Game X, Rebillard X, Mallet R, Faix A, Mongiat-Artus P, Fournier G, Neuzillet Y; le comité de cancérologie de l’Association française d’urologie (CCAFU). [Recommendations CCAFU on the management of cancers of the urogenital system during an epidemic with Coronavirus COVID-19]. Prog Urol. 2020;30:221-231. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Zaorsky NG, Yu JB, McBride SM, Dess RT, Jackson WC, Mahal BA, Chen R, Choudhury A, Henry A, Syndikus I, Mitin T, Tree A, Kishan AU, Spratt DE. Prostate Cancer Radiotherapy Recommendations in Response to COVID-19. Adv Radiat Oncol. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 121] [Cited by in RCA: 139] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 20. | Thoracic Surgery Outcomes Research Network, Inc. COVID-19 Guidance for Triage of Operations for Thoracic Malignancies: A Consensus Statement from Thoracic Surgery Outcomes Research Network. Ann Thorac Surg. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 51] [Cited by in RCA: 69] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 21. | Banna G, Curioni-Fontecedro A, Friedlaender A, Addeo A. How we treat patients with lung cancer during the SARS-CoV-2 pandemic: primum non nocere. ESMO Open. 2020;5:e000765. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 61] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 22. | Zhao Z, Bai H, Duan J, Wang J. Recommendations of individualized medical treatment and common adverse events management for lung cancer patients during the outbreak of COVID-19 epidemic. Thorac Cancer. 2020;11:1752-1757. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 23. | Mazzone PJ, Gould MK, Arenberg DA, Chen AC, Choi HK, Detterbeck FC, Farjah F, Fong KM, Iaccarino JM, Janes SM, Kanne JP, Kazerooni EA, MacMahon H, Naidich DP, Powell CA, Raoof S, Rivera MP, Tanner NT, Tanoue LK, Tremblay A, Vachani A, White CS, Wiener RS, Silvestri GA. Management of Lung Nodules and Lung Cancer Screening During the COVID-19 Pandemic: CHEST Expert Panel Report. Chest. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 80] [Cited by in RCA: 81] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 24. | Zacharia BE, Eichberg DG, Ivan ME, Hanft S, Boockvar JA, Isildak H, Mansouri A, Komotar RJ, D'Amico RS. Letter: Surgical Management of Brain Tumor Patients in the COVID-19 Era. Neurosurgery. 2020;nyaa162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 25. | Mohile NA, Blakeley JO, Gatson NTN, Hottinger AF, Lassman AB, Ney DE, Olar A, Schiff D, Shih HA, Strowd R, van den Bent MJ, Ziu M. Urgent Considerations for the Neuro-oncologic Treatment of Patients with Gliomas During the COVID-19 Pandemic. Neuro Oncol. 2020;noaa090. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 56] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 26. | Bernhardt D, Wick W, Weiss SE, Sahgal A, Lo SS, Suh JH, Chang EL, Foote M, Perry J, Meyer B, Vajkoczy P, Wen PY, Straube C, Pigorsch S, Wilkens JJ, Combs SE. Neuro-oncology Management During the COVID-19 Pandemic With a Focus on WHO Grade III and IV Gliomas. Neuro Oncol. 2020;noaa113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 60] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 27. | Fakhry N, Schultz P, Morinière S, Breuskin I, Bozec A, Vergez S, de Garbory L, Hartl D, Temam S, Lescanne E, Couloigner V, Barry B; French Society of Otorhinolaryngology, Head and Neck Surgery (SFORL); French Society of Head and Neck Carcinology (SFCCF). French consensus on management of head and neck cancer surgery during COVID-19 pandemic. Eur Ann Otorhinolaryngol Head Neck Dis. 2020;137:159-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 53] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 28. | Day AT, Sher DJ, Lee RC, Truelson JM, Myers LL, Sumer BD, Stankova L, Tillman BN, Hughes RS, Khan SA, Gordin EA. Head and neck oncology during the COVID-19 pandemic: Reconsidering traditional treatment paradigms in light of new surgical and other multilevel risks. Oral Oncol. 2020;105:104684. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 92] [Cited by in RCA: 90] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 29. | Thomson DJ, Palma D, Guckenberger M, Balermpas P, Beitler JJ, Blanchard P, Brizel D, Budach W, Caudell J, Corry J, Corvo R, Evans M, Garden AS, Giralt J, Gregoire V, Harari PM, Harrington K, Hitchcock YJ, Johansen J, Kaanders J, Koyfman S, Langendijk JA, Le QT, Lee N, Margalit D, Mierzwa M, Porceddu S, Soong YL, Sun Y, Thariat J, Waldron J, Yom SS. Practice Recommendations for Risk-Adapted Head and Neck Cancer Radiation Therapy During the COVID-19 Pandemic: An ASTRO-ESTRO Consensus Statement. Int J Radiat Oncol Biol Phys. 2020;107:618-627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 121] [Cited by in RCA: 143] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 30. | Sharma A, Crosby DL. Special considerations for elderly patients with head and neck cancer during the COVID-19 pandemic. Head Neck. 2020;42:1147-1149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 31. | Salari A, Shirkhoda M. COVID-19 pandemic & head and neck cancer patients management: The role of virtual multidisciplinary team meetings. Oral Oncol. 2020;105:104693. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 32. | Patel R, Saif MW. Management of Pancreatic Cancer During COVID-19 Pandemic: To Treat or Not to Treat? JOP. 2020;21:27-28. [PubMed] |
| 33. | Tchelebi LT, Haustermans K, Scorsetti M, Hosni A, Huguet F, Hawkins MA, Dawson LA, Goodman KA. Recommendations for the use of radiation therapy in managing patients with gastrointestinal malignancies in the era of COVID-19. Radiother Oncol. 2020;148:194-200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 34. | Romesser PB, Wu AJ, Cercek A, Smith JJ, Weiser M, Saltz L, Garcia-Aguilar J, Crane CH. Management of Locally Advanced Rectal Cancer During The COVID-19 Pandemic: A Necessary Paradigm Change at Memorial Sloan Kettering Cancer Center. Adv Radiat Oncol. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 35. | Di Saverio S, Pata F, Gallo G, Carrano F, Scorza A, Sileri P, Smart N, Spinelli A, Pellino G. Coronavirus pandemic and colorectal surgery: practical advice based on the Italian experience. Colorectal Dis. 2020;22:625-634. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 146] [Article Influence: 29.2] [Reference Citation Analysis (0)] |