Published online Feb 6, 2019. doi: 10.12998/wjcc.v7.i3.366
Peer-review started: November 1, 2018
First decision: November 27, 2018
Revised: December 20, 2018
Accepted: December 29, 2018
Article in press: December 30, 2018
Published online: February 6, 2019
Processing time: 89 Days and 11.7 Hours
Papillary cystadenoma is a rare benign epithelial tumor of the salivary gland, which is characterized by papillary structures and oncocytic cells with rich eosinophilic cytoplasm. We found only one case of papillary cystadenoma in nearly 700 cases of salivary gland tumors. Our case was initially mistaken for a tumor of the right temporomandibular joint (TMJ) capsule rather than of parotid gland origin. Preoperative magnetic resonance imaging (MRI) and computed tomography (CT) should be carefully studied, which allows for appropriate preoperative counseling and operative planning.
Here, we report an unusual case of a 54-year-old woman with a parotid gland papillary cystadenoma (PGPC) that was misdiagnosed as a tumor of the right TMJ capsule. She was initially admitted to our hospital due to a mass anterior to her right ear inadvertently found 5 d ago. Preoperative CT and MRI revealed a well circumscribed tumor that was attached to the right TMJ capsule. The patient underwent a resection through an incision for TMJ, but evaluation of an intraoperative frozen section revealed a benign tumor of the parotid gland. Then we removed part of the parotid gland above the temporal facial trunk. The facial nerve was preserved. Postoperative histopathological findings revealed that the tumor was PGPC. No additional treatment was performed. There was no recurrence during a 20-mo follow-up period.
The integrity of the interstitial space around the condyle in MRI or CT should be carefully evaluated for parotid gland or TMJ tumors.
Core tip: We present an unusual parotid gland papillary cystadenoma that was mistaken for a temporomandibular joint (TMJ) tumor. Surgeons should pay particular attention to the integrity of the interstitial space around the condyle in preoperative magnetic resonance imaging and computed tomography. If the space is intact, the mass may come from the parotid gland, otherwise, it is of TMJ origin. The tumor‘s origin determines operative planning and process.
- Citation: Wang L, Zhang SK, Ma Y, Ha PK, Wang ZM. Papillary cystadenoma of the parotid gland: A case report. World J Clin Cases 2019; 7(3): 366-372
- URL: https://www.wjgnet.com/2307-8960/full/v7/i3/366.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v7.i3.366
Cystadenoma is a rare benign epithelial tumor of the salivary gland. It can be divided into mucinous and papillary subtypes[1]. It is mainly characterized by polycystic growth, with the epithelial component showing adenomatous hyperplasia[2]. It can occur in all the salivary glands, and is most commonly seen in the parotid and palatal glands[3]. For many years, the classification of cystadenoma and knowledge about its properties were unclear. Cystadenoma was once known as a cystic duct adenoma or oncocytic cystadenoma. This tumor was described in 1990 by the World Health Organization as a separate entity, which was classified as a subtype of salivary gland tumor[4]. However, in 2005, it was defined as a specific type of salivary gland epithelial tumor[5]. Papillary cystadenoma is easily confused with papillary cystadenoma lymphomatosum (Warthin tumor), due to their histologic similarity: papillary structures and oncocytic cells with rich eosinophilic cytoplasm. However, Warthin tumors are rich in lymphoid stroma. Here, we report a case of papillary cystadenoma of the right parotid gland, which was preoperatively misdiagnosed as a tumor of the temporomandibular joint (TMJ). The main treatment in this case included removal of the entire tumor and locally extended excision of the parotid gland. The histopathological diagnosis was papillary cystadenoma of the parotid gland.
A 54-year-old female patient was initially admitted to our department due to a mass anterior to her right ear inadvertently found for 5 d.
There were no significant changes in size since she found the mass. The patient complained of dull pain when she opened her mouth, but did not take any medicine for it.
At admission, her medical history was otherwise unremarkable.
The patient was a nonsmoker, without personal or family history of other diseases.
On physical examination a palpable mass, about 2.5 cm × 2.0 cm, was found to be located near the right parotid region immediately anterior to the tragus. The mass had unclear boundaries, was fairly immobile, and was not tender.
Laboratory results including complete blood count, electrolytes, and coagulation panels were within normal limits, with a white blood count of 4.21 K/μL, red blood cell count of 4.5 × 1012/L, and hemoglobin of 138 G/L.
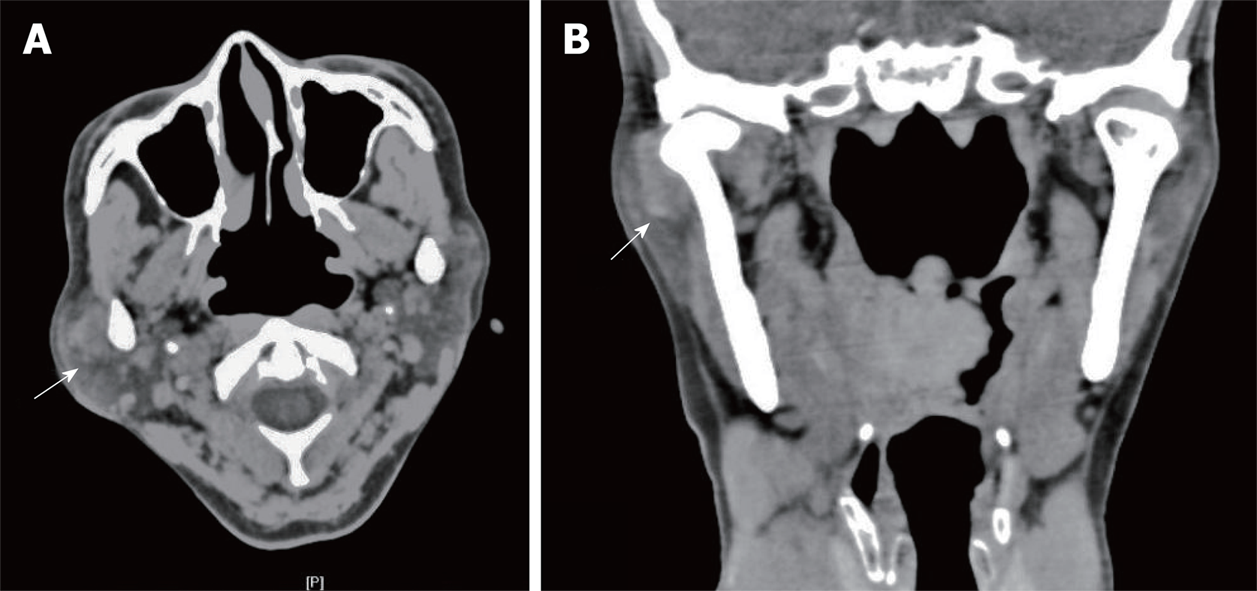
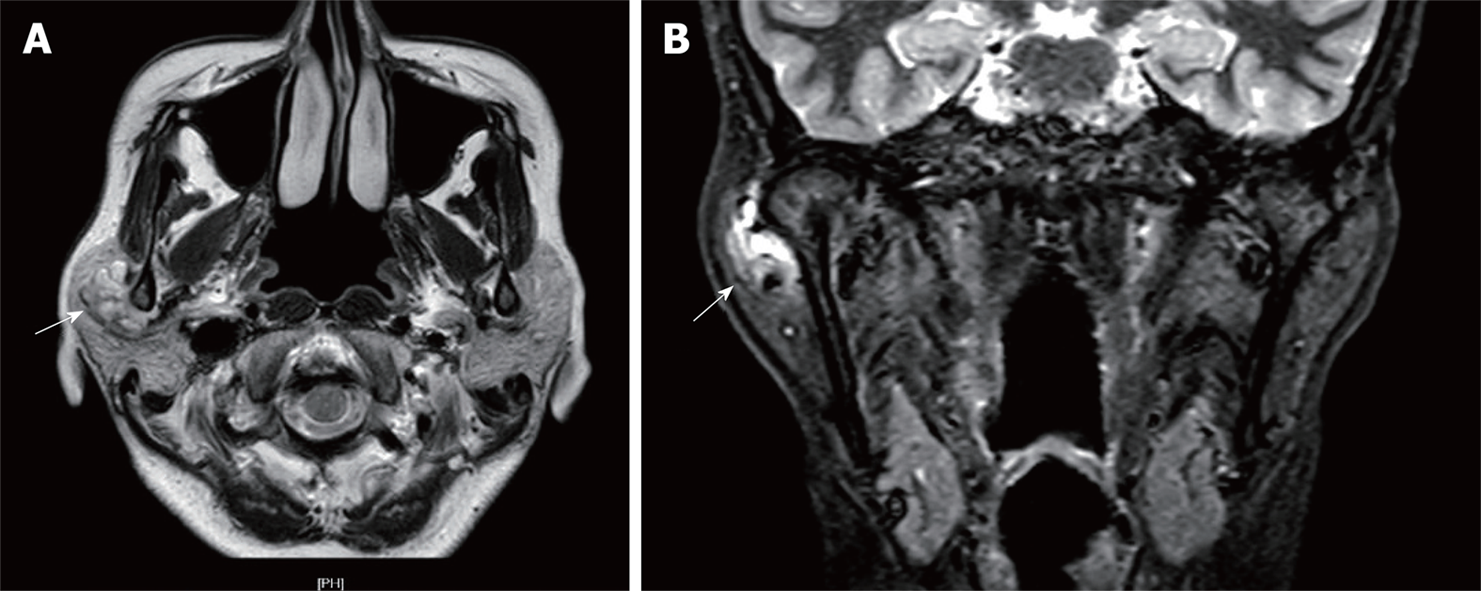
Computed tomography (CT) revealed an occupying lesion just outside the right TMJ capsule. A clear capsule surrounded the mass, which contained cystic structures. The right mandibular condyle showed no evidence of bone destruction (Figure 1). Closed-position magnetic resonance imaging (MRI) revealed symmetrical bilateral TMJs without evidence of bone destruction. T2-weighted scanning showed a mixed polycystic lesion in the lateral right condyle. The mass measured approximately 2.0 cm × 1.6 cm. Open-position MRI showed stripe-like high-signal images in the right TMJ (Figure 2).
The preoperative diagnosis was a tumor in the right TMJ capsule. Although we strongly recommended a fine needle aspiration biopsy before surgery, the patient refused our suggestion due to her deep worry about the tumor spread.
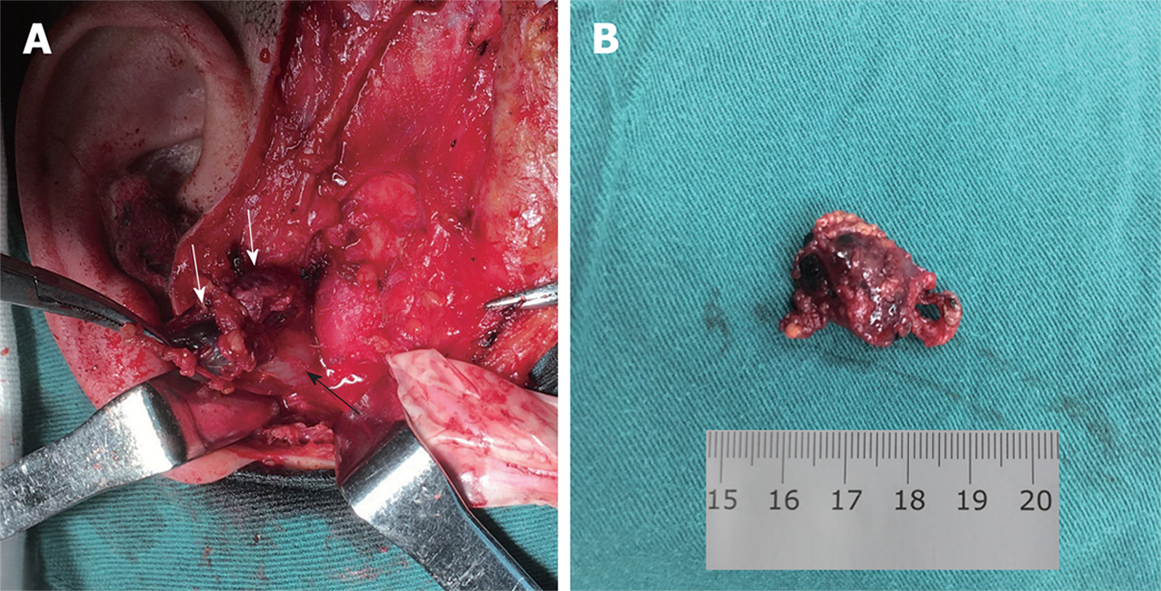
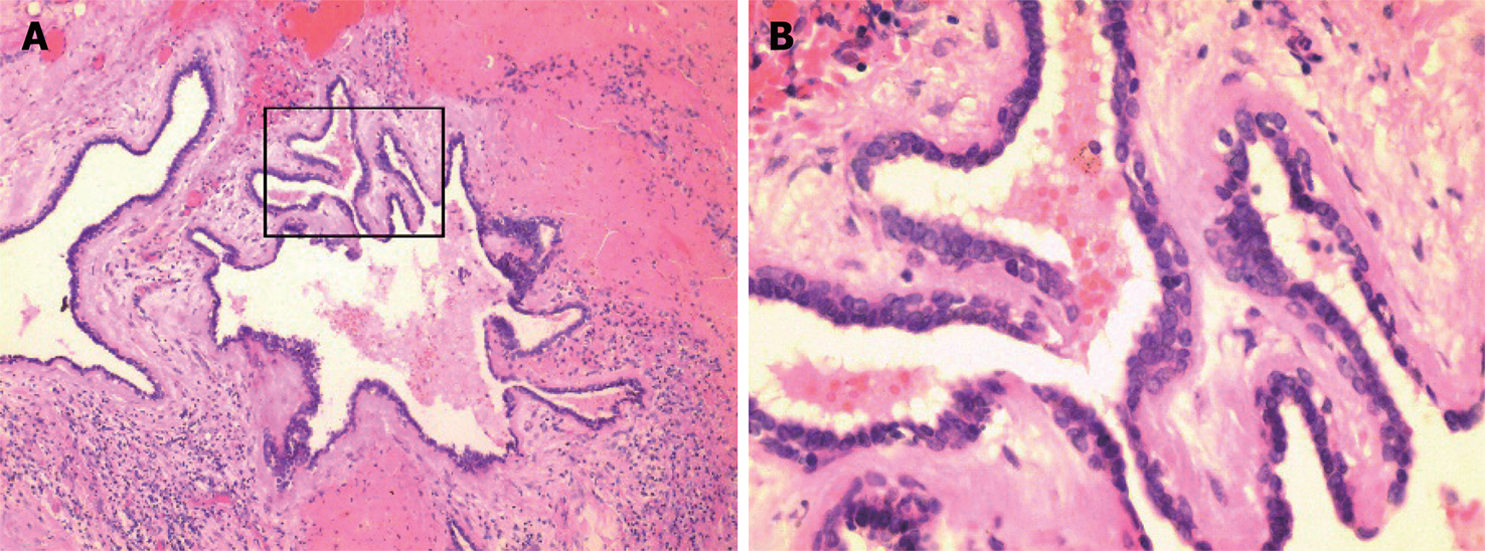
At surgery, we designed and performed an incision for TMJ, that was a 3 cm preauricular vertical incision and a 3 cm temporal incision in the hair line with an angle of 135° to the preauricular incision as described in the literature[6]. After further dissecting procedures, a cystic mass was found, which was loosely attached to the TMJ capsule. The mass was resected completely without opening the TMJ capsule. It measured approximately 2.0 cm × 1.5 cm (Figure 3). Evaluation of an intraoperative frozen section revealed a benign tumor of the parotid gland. Because the tumor was located within the upper part of the parotid gland, we decided to remove the part of the parotid gland above the temporal facial trunk. Thus, we extended the vertical incision down to the earlobe and then around it as an S-shaped incision for the parotid gland. After dissection anterior to the surface of the sternocleidomastoid muscle, the main trunk of the facial nerve was exposed. Dissection was performed along the temporal facial trunk, and the upper part of the parotid gland was resected. The facial nerve was preserved. This operation took 105 min and estimated blood loss was 60 mL. The patient’s postoperative course was uneventful. Postoperative histopathological examination found cystic regions that were lined by one to three layers of cuboidal or columnar cells. Multiple papillary projections extended into cyst lumens. The lumens contained eosinophilic material with inflammatory, scattered epithelial and foamy cells. Based on these findings, the patient was diagnosed with parotid gland papillary cystadenoma (PGPC) (Figure 4).
There was no recurrence during a 20-mo follow-up period according to postoperative CT.
Cystadenoma has also been reported to occur in intrahepatic bile ducts, the pancreas, ovary, epididymis, and kidney[7-11]. The prevalence of salivary gland papillary cystadenoma is low. In a study of 360 cases of salivary gland tumors, three patients (all female) were found to have cystadenoma of the parotid gland, which accounted for about 0.83% of all study tumors and about 1.0% of the benign study tumors[12]. A review of 30 cases of papillary cystadenoma of the minor salivary glands reported 17 male and 13 female patients[13]. Our study of 700 patients with salivary gland tumors during 2010 to 2016 found only one patient (female) with PGPC, which accounted for about 0.14% of all study tumors and about 0.15% of benign study tumors. We listed the reported cases of PGPC with comparatively complete data between 2009 and 2018 in Table 1[3,14-17], while solely retrospective studies without detailed data were excluded. Because of the rarity of cystadenoma of the salivary glands, the gender ratio of patients remains unclear and the etiopathogenesis of this disease has not been well discussed in textbooks and other published articles.
| Case | Authors | Year | Age | Sex | Location | Symptom duration | Size (cm) | Treatment | Recurrence | Follow-up |
| 1 | Zhang et al[3] | 2009 | 26 | F | Right parotid gland | 4 mo | 2.4 | Excision | n/r | n/r |
| 2 | Zhang et al[3] | 2009 | 52 | M | Left parotid gland | Few | 1.5 | Excision | n/r | n/r |
| 3 | Gupta et al[14] | 2011 | 75 | M | Right parotid gland | 12 mo | 2.5 | Excision | n/r | n/r |
| 4 | Chin et al[15] | 2014 | 38 | M | Right parotid gland | 1 mo | 2.5 | Excision | n/r | n/r |
| 5 | Chin et al[15] | 2014 | 84 | M | Left parotid gland | 12 mo | 3.1 × 2.7 | Excision | n/r | n/r |
| 6 | Chin et al[15] | 2014 | 57 | M | Right submandibular Gland | 12 mo | 2.4 | Excision | n/r | n/r |
| 7 | Alexiev et al[16] | 2017 | 64 | M | Left parotid gland | 3 mo | 3.0 × 2.5 | Excision | No | 2 mo |
| 8 | Bajpai et al[17] | 2018 | 54 | M | Right parotid gland | 3 mo | 3.5 | Excision | n/r | n/r |
| 9 | Wang ZM* | 2018 | 54 | F | Right parotid gland | 5 d | 2.0 × 1.6 | Excision | No | 20 mo |
The preoperative imaging examinations of our case showed a well circumscribed mass. MRI of the parotid gland revealed a polycystic mass tightly surrounding the lateral and upper sides of the right TMJ capsule, which was misdiagnosed as a tumor of the TMJ capsule. However, during surgery the mass appeared to be a vascular malformation. The frozen section examination showed a benign tumor of the parotid gland that was diagnosed by postoperative histopathology as a papillary cystadenoma of the parotid gland. Therefore, the clinical manifestations and imaging examinations were not adequate for the correct definitive diagnosis. More notably, if the interstitial space around the condyle does not change and margin of the space is smooth in MRI, this indicates that the condyle is not damaged, and the mass is probably free of TMJ origin. Our case reminds surgeons of the utility of preoperative imaging, and surgeons should pay particular attention to the integrity of the interstitial space around the condyle in MRI, which stands for the condyle cortical plate. If the space is intact, the mass may come from the parotid gland, otherwise, it is of TMJ origin. Consequently, preoperative evaluation would potentially lead to a different incision design and an operative plan.
Surgical excision remains the main treatment of choice, despite the benign characteristics of this tumor; and the prognosis is good. Recurrence is seldom seen, with more tumors recurring in major salivary glands than in minor ones. Inadequate removal due to an incomplete capsule or tumor cell infiltration of the parotid gland is probably responsible for recurrence[13,18]. Although cystadenoma of the salivary gland is a benign tumor, postoperative malignant transformation has been reported[19]. A long-standing mass in the parotid gland may compress the facial nerve, causing hemifacial spasms[20].
The definitive diagnosis is made mainly on the basis of histopathological findings. Histologically, papillary cystadenoma is composed of well-defined unilocular or multilocular cysts, with intraluminal papillary projections[21]. The epithelial cells lining the cystic spaces are cuboidal or columnar, and the cystic structures are separated by a limited amount of interstitial tissue[13]. The differential diagnosis of papillary cystadenoma includes a variety of malignant and benign lesions, including Warthin tumor, intraductal papilloma, cystadenocarcinoma, and oncocytoma[13]. Warthin tumors are rich in lymphoid stroma. Sections of the lesion reveal multiple small cystic regions or a single large cyst surrounded by salivary gland lobules or connective tissue[22]. Intraductal papilloma is composed of dilated cystic ducts with papillary epithelial projections[23]. Oncocytoma is characterized by polyhedral oncocytic cells and absence of papillary projections[15]. Cystadenocarcinomas have structures similar to those of papillary cystadenomas, but cystadenocarcinomas have more cells invading the surrounding connective tissue[21,24].
We present an unusual case of PGPC that was mistaken for a TMJ tumor. Preoperative MRI and CT should be carefully studied for all tumors near this area in order to evaluate the integrity of the interstitial space around the condyle. This allows for appropriate preoperative counseling and operative planning. If possible, preoperative fine needle aspiration should be strongly recommended so as to distinguish the tumor’s nature and origin. In the future, more cases are helpful to learn about this disease.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Sridharan G S- Editor: Dou Y L- Editor: Wang TQ E- Editor: Song H
| 1. | Mahler V, Schell H. Papillary cystadenoma: a rare tumor of the minor salivary glands. Eur J Dermatol. 1999;9:387-389. [PubMed] [Cited in This Article: ] |
| 2. | Lim CS, Ngu I, Collins AP, McKellar GM. Papillary cystadenoma of a minor salivary gland: report of a case involving cytological analysis and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105:e28-e33. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Zhang S, Bao R, Abreo F. Papillary oncocytic cystadenoma of the parotid glands: a report of 2 cases with varied cytologic features. Acta Cytol. 2009;53:445-448. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Seifert G, Brocheriou C, Cardesa A, Eveson JW. WHO International Histological Classification of Tumours. Tentative Histological Classification of Salivary Gland Tumours. Pathol Res Pract. 1990;186:555-581. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 202] [Cited by in F6Publishing: 209] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 5. | Barnes L, Eveson JW, Reichart P, Sidransky D. World Health Organization classification of tumours. Pathology and genetics of head and neck tumours. Lyon: IARC Press 2005; 232-233. [Cited in This Article: ] |
| 6. | Qiu YT, Yang C, Chen MJ, Qiu WL. Can a Novel Surgical Approach to the Temporomandibular Joint Improve Access and Reduce Complications? J Oral Maxillofac Surg. 2016;74:1336-1342. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Li H, Peng B. Laparoscopic Anatomical Left Hepatectomy for Intrahepatic Bile Duct Papillary Mucinous Cystadenoma With Intraoperative Vascular Repair: A Case Report. Medicine (Baltimore). 2016;95:e2802. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Pravisani R, Intini SG, Girometti R, Avellini C, Leo CA, Bugiantella W, Risaliti A. Macrocystic serous cystadenoma of the pancreas: Report of 4 cases. Int J Surg. 2015;21 Suppl 1:S98-S101. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Singh AK, Singh M. Collision tumours of ovary: a very rare case series. J Clin Diagn Res. 2014;8:FD14-FD16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Kano H, Adachi Y, Nagahama K, Maeda M, Ishida T. A case of papillary cystadenoma of the epididymis mimicking a testicular tumor. Hinyokika Kiyo. 2012;58:39-43. [PubMed] [Cited in This Article: ] |
| 11. | Davidov MI, Ponomareva TB, Liadov AA. [Multiple bilateral papillary cystadenoma of the kidney]. Urologiia. 2003;60-61. [PubMed] [Cited in This Article: ] |
| 12. | Mejía-Velázquez CP, Durán-Padilla MA, Gómez-Apo E, Quezada-Rivera D, Gaitán-Cepeda LA. Tumors of the salivary gland in Mexicans. A retrospective study of 360 cases. Med Oral Patol Oral Cir Bucal. 2012;17:e183-e189. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Tjioe KC, de Lima HG, Thompson LD, Lara VS, Damante JH, de Oliveira-Santos C. Papillary Cystadenoma of Minor Salivary Glands: Report of 11 Cases and Review of the English Literature. Head Neck Pathol. 2015;9:354-359. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Gupta S, Sodhani P, Jain S, Khurana N, Agarwal PN. Oncocytic papillary cystadenoma of parotid gland: a diagnostic challenge on fine-needle aspiration cytology. Diagn Cytopathol. 2011;39:627-630. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Chin S, Kim HK, Kwak JJ. Oncocytic papillary cystadenoma of major salivary glands: Three rare cases with diverse cytologic features. J Cytol. 2014;31:221-223. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Alexiev BA, Jennings LJ, Samant S, Rao S. Oncocytic papillary cystadenoma with prominent mucinous differentiation of parotid gland: A case report. Pathol Res Pract. 2017;213:1310-1314. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Bajpai M, Pardhe N, Kumar M. Oncocytic Papillary Cystadenoma of Parotid Gland. J Coll Physicians Surg Pak. 2018;28:814. [PubMed] [Cited in This Article: ] |
| 18. | Girotra C, Padhye MN, Mahajan P, Nair A. A rare case report of mucinous cystadenoma with immunohistochemical analysis and review of literature. J Maxillofac Oral Surg. 2015;14:426-434. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Telugu RB, Job AJ, Manipadam MT. Papillary Cystadenocarcinoma of the Parotid Gland: A Rare Case Report. J Clin Diagn Res. 2016;10:ED01-ED03. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Erol O, Aydın E. A Rare Cause of Hemifacial Spasm: Papillary Oncocytic Cystadenoma. Balkan Med J. 2016;33:569-572. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Gallego L, Junquera L, Fresno MF, de Vicente JC. Papillary cystadenoma and cystadenocarcinoma of salivary glands: two unusual entities. Med Oral Patol Oral Cir Bucal. 2008;13:E460-E463. [PubMed] [Cited in This Article: ] |
| 22. | Goto M, Ohnishi Y, Shoju Y, Wato M, Kakudo K. Papillary oncocytic cystadenoma of a palatal minor salivary gland: A case report. Oncol Lett. 2016;11:1220-1222. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 23. | Brannon RB, Sciubba JJ, Giulani M. Ductal papillomas of salivary gland origin: A report of 19 cases and a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92:68-77. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 87] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 24. | Foss RD, Ellis GL, Auclair PL. Salivary gland cystadenocarcinomas. A clinicopathologic study of 57 cases. Am J Surg Pathol. 1996;20:1440-1447. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 119] [Cited by in F6Publishing: 123] [Article Influence: 4.4] [Reference Citation Analysis (0)] |