Published online Oct 16, 2022. doi: 10.12998/wjcc.v10.i29.10399
Peer-review started: April 17, 2022
First decision: May 12, 2022
Revised: May 13, 2022
Accepted: September 1, 2022
Article in press: Sepyember 1, 2022
Published online: October 16, 2022
Gallstones are a common public health problem, especially in developed countries. There are an increasing number of patients who are diagnosed with gallstones due to increasing awareness and liberal use of imaging, with 22.6%-80% of gallstone patients being asymptomatic at the time of diagnosis. Despite being asymptomatic, this group of patients are still at life-long risk of developing symptoms and complications such as acute cholangitis and acute biliary pancreatitis. Hence, while early prophylactic cholecystectomy may have some benefits in selected groups of patients, the current standard practice is to recommend cholecystectomy only after symptoms or complications occur. After reviewing the current evidence about the natural course of asymptomatic gallstones, complications of cholecystectomy, quality of life outcomes, and economic outcomes, we recommend that the option of cholecystectomy should be discussed with all asymptomatic gallstone patients. Disclosure of material information is essential for patients to make an informed choice for prophylactic cholecystectomy. It is for the patient to decide on watchful waiting or prophylactic cholecystectomy, and not for the medical community to make a blanket policy of watchful waiting for asymptomatic gallstone patients. For patients with high-risk profiles, it is clinically justifiable to advocate cholecystectomy to minimize the likelihood of morbidity due to complications.
Core Tip: We recommend that an option of cholecystectomy should be discussed with all asymptomatic gallstone patients. Disclosure of material information is essential for patients to make an informed choice for prophylactic cholecystectomy. It is for the patient to decide on watchful waiting or prophylactic cholecystectomy, and not for the medical community to make a blanket policy of watchful waiting for asymptomatic gallstone patients. For patients with high-risk profiles, it is clinically justifiable to advocate cholecystectomy to minimize the likelihood of morbidity due to complications.
- Citation: Lee BJH, Yap QV, Low JK, Chan YH, Shelat VG. Cholecystectomy for asymptomatic gallstones: Markov decision tree analysis. World J Clin Cases 2022; 10(29): 10399-10412
- URL: https://www.wjgnet.com/2307-8960/full/v10/i29/10399.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i29.10399
Gallstones, or cholelithiasis, is a common public health problem, especially in developed countries[1-3]. In the United States, an estimated 20-25 million people have gallstones, and over 700000 cholecystectomies are performed annually, costing a median of $11584 per discharge and $6.2-6.5 billion[2,4-6]. There are three main types of gallstones - cholesterol stones, brown pigment stones, and black pigment stones, with cholesterol stones accounting for 80%-90% of all gallstones[1]. Many risk factors predispose an individual to develop gallstones, broadly classified into modifiable and nonmodifiable factors. Modifiable risk factors include rapid weight loss, diet, drugs such as hormone replacement therapy and fibrates, and metabolic syndromes such as type two diabetes mellitus and nonalcoholic fatty liver disease[7,8]. Examples of nonmodifiable risk factors are female gender, race and hemoglobinopathies like sickle cell disease and spherocytosis[7-11]. Additionally, chronic Salmonella typhi gallbladder infection also predisposes to gallstones.
Ultrasonography (US) is the gold standard for gallstone diagnosis due to its noninvasive nature and high sensitivity and specificity[12]. Universal accessibility and affordability of US scans have bolstered epidemiological studies on gallstone prevalence. The gallstone burden varies across different populations. For example, western populations report gallstone prevalence of 0.1%-61.5%[1,13] compared to 3%-15.6% in Asian populations[2,12,14]. Overall, many patients are diagnosed with asymptomatic gallstones due to increasing awareness and liberal use of imaging[15]. An estimated 22.6%-80% of gallstone patients are asymptomatic at the time of diagnosis[16-18]. However, asym
One of the earliest and most common presenting complaints in patients with symptomatic gallstones is biliary colic[18,23]. Sometimes, biliary colic can be confused with dyspepsia or atypical chest pain, resulting in a delayed diagnosis of gallstone disease. This subsequently increases the risk of complications like acute cholecystitis, acute cholangitis and acute biliary pancreatitis. If timely intervention is not done, severe complications like Mirrizzi’s syndrome, cholecystoenteric fistula, pyogenic liver abscess, and gallstone ileus can develop[24]. Clinical outcomes of patients with complicated gallstone disease are inferior to those of elective laparoscopic cholecystectomy for symptomatic biliary colic patients[25,26].
Since 1985, laparoscopic cholecystectomy has replaced traditional open cholecystectomy as the gold standard for managing gallstones and related complications[27,28]. Therefore, it is intuitive to ask ourselves, can elective laparoscopic cholecystectomy in asymptomatic gallstone patients reduce the overall morbidity and mortality from gallstone disease? We need to review the current evidence about the natural course of asymptomatic gallstones, complications of cholecystectomy, quality of life outcomes, emerging concerns of gut microbiome alteration following cholecystectomy, and ethical and economic considerations. As bile duct injury (BDI) is an Achilles heel of cholecystectomy, it is integral that we include BDI in our discussion.
William Mayo stated, “There is no innocent gallstone”. The progression from asymptomatic to symptomatic gallstone disease was variable, ranging from 11.7% to 23.7% over 9-20 years[29-32]. The cumulative incidence of developing complications for asymptomatic gallstone patients was about 3%-8% over the same period[29-31,33]. In contrast, prior population studies have reported that the rate of recurrent symptoms in already symptomatic patients was significantly higher, ranging from 18.6% to 37.1% over 1-14 years[13,34-38]. Similarly, this group of patients was also at a higher risk of developing complications, ranging from 4% to 30.3% over the same period[36-38]. Overall, the cumulative incidences of cholecystectomy due to recurrent symptoms or complications was 22.3%-50.7% in symptomatic gallstone patients[34,36-38], which were substantially greater compared to the 8.3%-25.8% of those who were asymptomatic and eventually underwent cholecystectomy[29,30,32,33].
The blanket policy for asymptomatic gallstone patients is currently watchful management, except in selected scenarios. Cholecystectomy is not routinely offered due to the inherent risks of surgery. These include risks of anesthesia, potential vascular and bowel injuries, retained stone, bile leak, BDI (estimated incidence of 0.2%-0.8%), and postcholecystectomy syndrome (PCS)[39,40], which are discussed below.
PCS encompasses symptoms and signs due to biliary and nonbiliary sequelae of surgery[41,42]. These heterogeneous complexes of symptoms include abdominal pain, dyspepsia, and jaundice. The prevalence of PCS has been reported to range from very low to 47%[41-44]. In a study by Shirah et al[41] of 272 patients with PCS, recurrent or retained common bile duct (CBD) stone, cystic duct stump syndrome, CBD stricture, bile leakage, and stenosis of the sphincter of Oddi accounted for 34.9% of PCS. Thus, with the increasing number of cholecystectomies, the number of patients suffering from PCS and related morbidity is likely to rise[45]. Hence, routine cholecystectomy is not recommended for most patients with asymptomatic gallstones[15]. However, we argue that some of the PCS complications are a result of technical difficulty following a chronic gallbladder pathology, thus early cholecystectomy could at least in part, reduce the PCS morbidity. Furthermore, the term PCS is loosely interpreted in the literature; and patients with obvious diagnoses of bile leak, CBD stone, etc. should not be classified as having PCS.
Removal of the gallbladder is associated with two times increased enterohepatic circulation, with increased bile acid exposure of the intestinal mucosa. This physiological change leads to an altered gut microbiome. The intestinal microbiome is implicated in gallstone diseases and has relevance both as a causative and end effect. Frost et al[46] studied the fecal microbiota profile of 404 gallstone carriers, 580 individuals post-cholecystectomy, and 984 healthy controls using the 16S rRNA gene sequencing technique. The participants were matched for age, sex, body mass index, smoking habits, and food-frequency score. They did not observe significant differences in microbiota composition of gallstone carriers and controls. However, cholecystectomy patients exhibited reduced microbiota diversity, reduced potentially beneficial genus Faecalibacterium, and increased opportunistic pathogen Escherichia/Shigella. A decrease of Faecalibacterium reduces short-chain fatty acid production. Thus, colonocytes are deprived of energy, and the colon is subjected to a proinflammatory intestinal state. In a meta-analysis including 10 cohort studies and 524649 patients, Zhang et al[47] reported that cholecystectomy patients had an increased risk of colorectal cancer. The opportunistic pathogens may induce DNA damage, increase gene mutagenicity, and increase lipopolysaccharide synthesis. Lipopolysaccharide promotes liver metastases in colorectal cancer patients by stimulating toll-like receptor 4 signaling[48]. More data are necessary to establish if cholecystectomy increases colorectal cancer risk. If a causal link is established, information disclosure during informed consenting would be material from a reasonable patient perspective.
Aside from the risks of surgery, multiple studies have documented the decrease in quality of life (QoL) post-cholecystectomy for asymptomatic gallstone patients[49-51]. Quintana et al[52] also reported a poorer health-related QoL risk to benefit ratio for patients with asymptomatic gallstones post cholecystectomy. For example, in the Short Form 36 (SF-36), patients with symptomatic gallstones and low surgical risks reported an increase in their SF-36 scores and hence improvement in their QoL post-cholecystectomy under the social function (+9.88), bodily pain (+13.76), and mental health (+0.51) domains. In contrast, patients with asymptomatic gallstones and low surgical risk had minimal improvements in their social function (+0.57) and bodily pain (+2.62) scores post-cholecystectomy, while there was a decrease in their mental health scores (-4.16). In another study on prophylactic chole
Prophylactic cholecystectomy on asymptomatic gallstone patients also has its ethical implications. An example of an ethically justified prophylactic surgery is prophylactic mastectomy, commonly performed for patients at risk of breast cancer. These include patients with BRCA1 mutations, strong family history of breast cancer with no demonstratable mutations, and tumors with histological risk factors such as unilateral ductal carcinoma in situ[54-57]. This is because female patients with BRCA1 mutations have an 80%-90% lifetime risk of developing breast cancer compared to the 5.7%-12.6% risk in the general population[58-60]. Similarly, Zendejas et al[61] reported that prophylactic mastectomy, costing $36594, provided 21.22 mean quality-adjusted life-years (QALY) compared to the 20.93 QALY for surveillance, which cost $35182. This gave an incremental cost-effectiveness ratio (CER) of $4869 per QALY gained for prophylactic mastectomy. Therefore, it is ethical and beneficial to perform prophylactic mastectomy in asymptomatic high-risk female patients to reduce the likelihood of developing breast cancer[62,63].
In contrast, although 85% of gallbladder cancers were associated with the presence of gallstones, the actual incidence of gallbladder cancer was low, ranging from 0.3% to 3%, with the highest incidence seen in patients of Indian descent[64-67]. The 20-year cumulative risk of gallbladder cancer in patients with gallstones was also reported to be low at 0.13%-1.5%[68]. Additionally, in a study by Wanjura et al[69], while there was QoL improvement, the Gastrointestinal Quality-of-Life Index scores were lower in the patients post-cholecystectomy (115.2) compared to the background population (116.7). In this aspect, the benefits of prophylactic cholecystectomy for all gallstone patients may not be comparable to those of prophylactic mastectomy. However, prophylactic cholecystectomy for asymptomatic gallstone patients may be considered in countries with a high prevalence of gallbladder cancer[70,71].
Offering prophylactic cholecystectomy for asymptomatic gallstone patients also has financial consequences on the healthcare system. An increasing number of individuals with health insurance coverage may lead to overservicing with strains on healthcare infrastructure and resources. For example, a study done by Ellimoottil et al[72] found that insurance expansion in Massachusetts, United States led to a 9.3% increase in elective surgery. On a similar note, Barros et al[73] reported that private health insurance played a key factor in the overwhelming healthcare expenditure in Brazil. Thus, offering prophylactic cholecystectomy may encourage individuals with full coverage under health insurance to exploit their health benefits. However, when the therapeutic benefits do not justify the costs, this eventually leads to overutilization and wastage of healthcare resources.
Conversely, the financial benefits of performing early cholecystectomy may outweigh that of delayed cholecystectomy in the setting of complications. For example, Tan et al[74] previously described the median total inpatient costs to be lower in patients who underwent early cholecystectomy (€4400) compared to those who had interval cholecystectomy (€5500). Similarly, the median cost of chole
Routine treatment of asymptomatic gallstones is not recommended in current guidelines, mainly due to reasons of low annual incidence of developing symptoms and complications, as well as the costs and risks of surgery[75,76]. It is acknowledged that only a minority of asymptomatic gallstone patients eventually develop symptomatic gallstone disease or related complications, with an incidence of 1%-4% per year[13,16,77]. Patients who are < 55 years old or with > 20 years’ life expectancy, female gender, smoking history, higher body mass index, presence of three or more stones, floating gallstones, gallstone > 2 cm in diameter, gallstone < 3 mm size with patent cystic duct, and nonfunctioning gallbladder are associated with a higher likelihood of having symptoms[15,78,79]. It remains unproven if patients who fall within these criteria would benefit from elective prophylactic cholecystectomy. Routine cholecystectomy in all patients with asymptomatic gallstones may result in anecdotal BDI, anesthesia-related morbidity, the increased overall cost of care and burden on healthcare resources. Thus, selective policy for prophylactic cholecystectomy may be justified and could be considered. There are certain health situations where prophylactic cholecystectomy is beneficial, and these are discussed below.
Cholecystectomy can be recommended as a prophylactic option in selected asymptomatic patients. For example, patients with red blood cell abnormalities such as sickle cell anemia and hereditary spherocytosis are predisposed to higher risks of cholelithiasis, with prevalence of 30%-70%[80-84]. Studies have also shown that gallstones complicated the clinical course of sickle cell anemia in 40% of adolescents and 70% of adults[9]. Rutledge et al[85] described that 75% of sickle cell anemia patients with asymptomatic gallstones eventually turned symptomatic. More recently, Muroni et al[86] reported that postoperative complications related to sickle cell anemia were less frequent for asymptomatic gallstone patients (11.5%) who received prophylactic laparoscopic cholecystectomy compared to symptomatic gallstone patients (25.5%). In addition, the same group of patients had shorter hospital admissions and potentially avoided complications such as acute cholecystitis and cholangitis[86]. Hence, prophylactic cholecystectomy is recommended for sickle cell anemia or hereditary spherocytosis patients with concurrent asymptomatic gallstones, along with splenectomy[87-90].
Similarly, cholecystectomy is also recommended in asymptomatic gallstone patients who are organ transplant recipients. Studies have shown that organ transplant patients with gallstones have a higher incidence of developing symptoms and complications than the general population[91-94]. For example, Graham et al[94] reported that patients who underwent cholecystectomy prior to transplant had no morbidity and mortality and 4% graft loss compared to patients who underwent cholecystectomy post-transplant who had 19% morbidity, 6% mortality and 25% graft loss. Similarly, Kao et al[95] reported that for heart transplant patients with asymptomatic gallstones, prophylactic cholecystectomy could result in cost savings of $17799 per QALY. Likewise, patients with neuroendocrine tumors on somatostatin analog treatment like octreotide are at risk of up to 65% of developing gallstones and associated biliary complications[96]. Hence prophylactic cholecystectomy can also be recommended for asymptomatic gallstone patients with neuroendocrine tumors on somatostatin analogs or prior to organ transplant[97,98].
Other possible considerations for cholecystectomy for asymptomatic gallstone patients include gallstones > 3 cm, concurrent gallbladder polyps, concomitant cholecystectomy during bariatric surgery, and existing comorbidities such as diabetes[99-103], albeit some of these indications are controversial[104].
Performing cholecystectomy on gallstone patients when still asymptomatic puts them at a lower overall risk of surgical complications. For example, waiting for patients to turn symptomatic already puts them at higher perioperative risk, including age-dependent risk factors[105]. Studies have also demonstrated that early cholecystectomy reduces the risk of developing gallbladder and bile duct malignancies in the presence of polyps, large gallstones, and porcelain gallbladders[106,107].
In terms of mortality rates, Zheng et al[21] found a significantly lower number of all-cause deaths in patients who received cholecystectomy versus those who did not across two large prospective cohorts. For example, the rate of all-cause death for individuals with gallstone disease in the National Healthcare Service between 1980 and 2012 was 1347 per 100000 each year compared to individuals without gallstone disease, which was 739 per 100000 each year[21]. Similarly, in the Health Professionals Follow-Up Study from 1986 to 2012, the all-cause death rate for individuals with gallstone disease was 2917 per 100000 each year against the 1315 per 100000 each year for individuals without gallstone disease[21].
Waiting for symptoms and complications to arise inevitably leads to higher risks of performing emergency cholecystectomy instead of elective cholecystectomy, associated with higher mortality rates, morbidity, and conversion to open conversion[108,109]. Steiner et al[110] reported that laparoscopic cholecystectomy led to a 33% relative risk reduction in operative mortality than open cholecystectomy did. Similarly, the rate of open conversion was found to be low in asymptomatic patients (1.5%)[111], compared to that for patients with symptomatic gallstones (5.9%-9.2%) and in acute cholecystitis (7.5%-26%)[112,113]. In a study by Amirthalingam et al[114] on 149 patients who underwent emergency cholecystectomy, the rate of open conversion was also found to be 5.2% in moderate (Tokyo grade II) and severe (Tokyo grade III) acute cholecystitis compared to 0% in mild acute cholecystitis (Tokyo grade I). Open conversion involves inherent risks such as incisional hernias and postoperative abdominal adhesions, which carry their own set of complications like abdominal colic or even intestinal obstruction necessitating surgical intervention[115]. Multiple studies reported higher rates of abdominal adhesions in patients who underwent open cholecystectomy (45.5%-75%) in contrast to laparoscopic cholecystectomy (0-35%)[116]. Hence, prophylactic cholecystectomy in asymptomatic gallstone patients can potentially avert these complications.
In the setting of fibrosis or severe inflammation, cholecystectomy is more technically challenging and leads to a higher risk of surgical complications[117,118]. For instance, Törnqvist et al[119] reported that the adjusted risk of BDI was doubled among patients with acute cholecystitis. In patients with moderate acute cholecystitis (Tokyo grade II), the risk of BDI was more than doubled and increased almost eightfold for severe (Tokyo grade III) acute cholecystitis. Other studies have also reported a positive correlation between the severity of acute cholecystitis and morbidity[120,121]. The increased BDI risk, especially in complicated cholecystitis, can also precipitate nonsurgical issues such as detrimental socioeconomic and QoL impacts on patients[51,122-124]. Given its severe outcomes, iatrogenic BDI may also result in litigations, adversely impacting the surgeon and the healthcare institution.
Furthermore, once complications occur, or if cholecystectomy is deemed unfeasible, surgeons may resort to bail-out techniques such as subtotal cholecystectomy, which is more technically challenging. Subtotal cholecystectomy leads to added complications such as retained stone, bile leak, and the need for secondary bail-out procedures like ERCP[125]. For example, the risk of bile duct leaks from subtotal cholecystectomy ranged from 0.6% to 18%[126-128]. Similarly, the risk of recurrent stones ranged from 1.1% to 4.6%[125,127,128]. Hence, performing cholecystectomy while asymptomatic may be ideal in avoiding complications.
Based on the above-mentioned inherent risks of waiting, we suggest that those who are asymptomatic but have multiple small gallbladder stones (< 1 cm), solitary large gallstone (> 1 cm), and gallbladder sludge occupying > 50% of the gallbladder volume should have discussions for considering prophylactic cholecystectomy[129]. Given that gallstones do not dissolve or disappear with time[130], the stone burden in young patients would either be the same or increase with age. This could result in a further increase in gallstone-related complications. In the same way, fit older patients with a high stone burden could be considered for prophylactic cholecystectomy to avoid age-related general anesthetic risks should complications arise as they age further and become frailer. Besides surgery, there is the option of percutaneous cholecystostomy in this group of older frail patients with cholecystitis. However, there are problems related to a permanent or semipermanent cholecystostomy tubes such as tube occlusion, dislodgement, skin excoriation at the exit site because of bile leakage, constant change of dressings or base plate, and the ensuing hospital or clinic visits[121]. In practice, many patients have found it uncomfortable to have a permanent tube in situ. Some of our older patients have even reconsidered the decision to undergo laparoscopic cholecystectomy after medical optimization, to improve their QoL.
The National Institutes of Health report in 1993 advised against expanding the indications of cholecystectomy, just because the laparoscopy technology was widely expanding[131]. The main concern for not routinely offering cholecystectomy to asymptomatic gallstone patients is the inherent risks of surgery, of which the most common and feared complication is BDI. This is frequently attributed to surgical inexperience and poor training[132-134]. However, these earlier data that reported surgical risks for cholecystectomy are no more valid with widespread training, especially with laparoscopic cholecystectomy. These include the SAGES safe cholecystectomy program and advocating the “Critical View of Safety” approach, which is strategized to minimize BDI[135,136]. In difficult cholecystectomy situations, bail-out strategies aid in reducing BDI risk.
Multiple studies have improved cholecystectomy outcomes over the years due to improved training standards and technological advancements[137]. Newer surgical pedagogy has been incorporating simulation and virtual reality training to enhance training and transfer skills into real-life practice[138]. Guidelines and recommendations such as indocyanine green dye fluorescent cholangiography and intraoperative cholangiography have also been set up to decrease the risk of operative complications[39]. Thus, the risks of performing elective cholecystectomy can be minimized dramatically due to the factors above. However, it would not be prudent to argue for universal prophylactic cholecystectomy, as despite refinements in technique and standardization of surgical training, BDI continues to be reported. Injuries continue to be reported even after the learning curve[139] or despite resorting to bail-out strategies[128]. In our opinion, most BDI happens due to difficulty from chronically neglected pathology, and it is possible that prophylactic cholecystectomy could reduce BDI risk.
Although BDI is considered the main outcome metric, retained bile duct stones and bile leak are increasingly important key performance indicators. These complications also warrant additional interventions like radiology-guided abdominal cavity drainage or ERCP and biliary drainage. Therefore, we can argue that a prophylactic cholecystectomy could also reduce such risks.
Imaging technology is becoming sophisticated with improved diagnostic and prognostic accuracy. In addition, the integration of artificial intelligence and machine learning algorithms aid pattern recognition and enhance diagnostics by reducing interobserver variability. Recently, an international multidisciplinary committee comprising expert radiologists, gastroenterologists, gastrointestinal surgeons, surgical oncologists, medical oncologists, and pathologists reported the Gallbladder Reporting and Data System (GB-RADS) ultrasound risk stratification to improve consistency in American interpretations, reporting, and assessment of the risk of malignancy in gallbladder wall thickening[140]. The GB-RADS system recommends six categories (GB-RADS 0-5) of gallbladder wall thickening based on gallbladder wall features, including symmetry and extent (focal vs circumferential) of involvement, layered appearance, intramural features (including intramural cysts and echogenic foci), and interface with the liver, with increased probability of malignancy. However, the utility of clinical application of the GB-RADS system for justifying prophylactic cholecystectomy in asymptomatic patients remains to be validated.
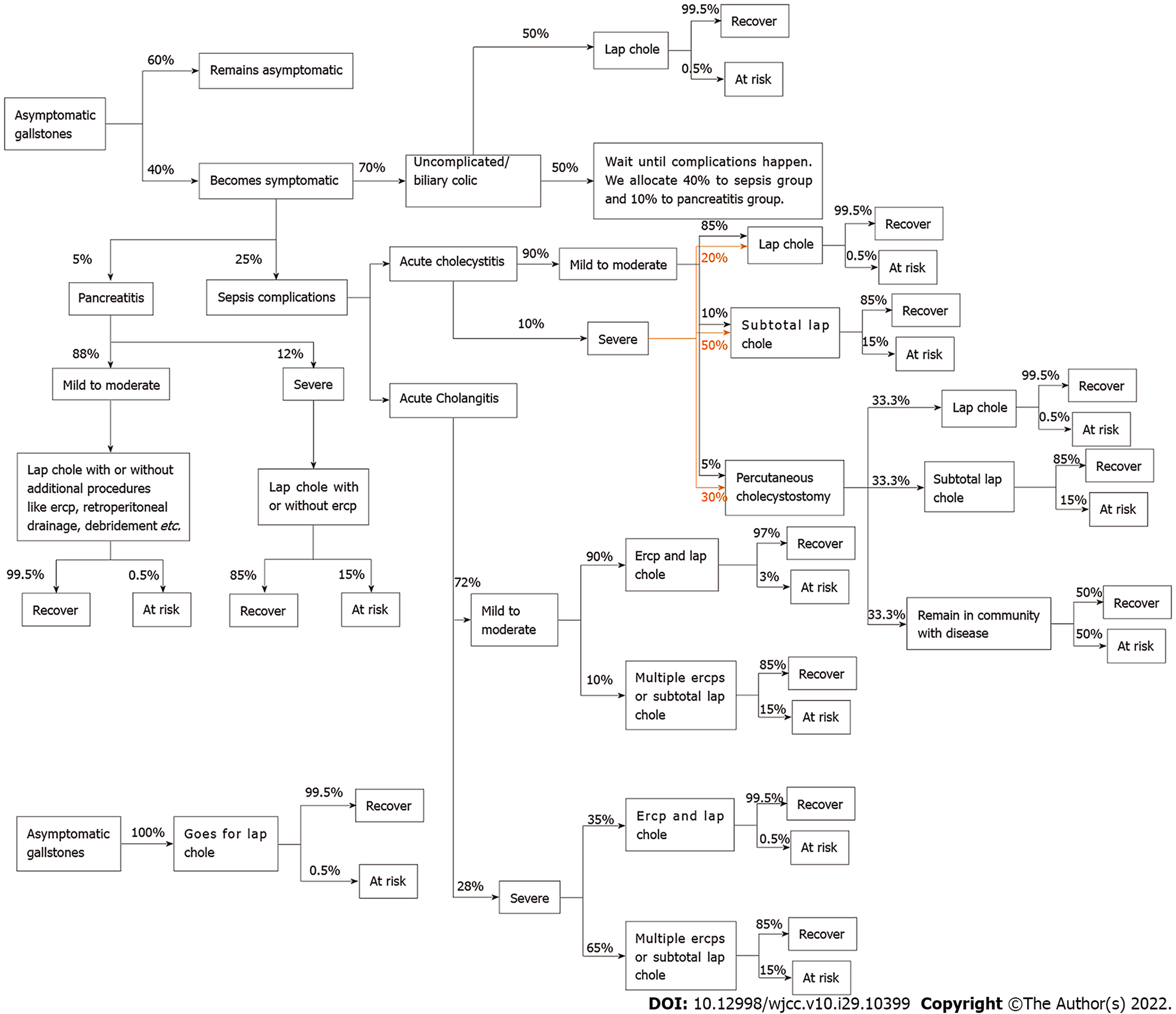
Markov decision tree analysis was performed to quantify the benefits of cholecystectomy for asym
We recommend that an option of cholecystectomy should be discussed with all asymptomatic gallstone patients. Our justifications for this stance address the main considerations of the current guidelines such as the low annual incidence of developing symptoms and complications, as well as the costs and risks of surgery. Disclosure of material information is essential for a reasonable patient to make an informed choice for prophylactic cholecystectomy. Ultimately, patients have the autonomy to choose their preferred intervention, although it may not be the best therapeutic decision in the eyes of the medical community or based on scientific evidence and numbers. The medical community should not make a blanket policy of watchful waiting for asymptomatic gallstone patients. For patients with high-risk profiles, it is clinically justifiable to advocate cholecystectomy to minimize the likelihood of morbidity due to complications.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Singapore
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Fan Y, China; Vahedi M, Iran S-Editor: Wang DM L-Editor: Kerr C P-Editor: Wang DM
| 1. | Marschall HU, Einarsson C. Gallstone disease. J Intern Med. 2007;261:529-542. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 100] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 2. | Shaffer EA. Epidemiology and risk factors for gallstone disease: has the paradigm changed in the 21st century? Curr Gastroenterol Rep. 2005;7:132-140. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 261] [Cited by in F6Publishing: 278] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 3. | Stinton LM, Myers RP, Shaffer EA. Epidemiology of gallstones. Gastroenterol Clin North Am. 2010;39:157-169, vii. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 200] [Cited by in F6Publishing: 186] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 4. | Schirmer BD, Winters KL, Edlich RF. Cholelithiasis and cholecystitis. J Long Term Eff Med Implants. 2005;15:329-338. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 170] [Cited by in F6Publishing: 163] [Article Influence: 8.6] [Reference Citation Analysis (1)] |
| 5. | Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut Liver. 2012;6:172-187. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 556] [Cited by in F6Publishing: 582] [Article Influence: 48.5] [Reference Citation Analysis (0)] |
| 6. | Tazuma S. Gallstone disease: Epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic). Best Pract Res Clin Gastroenterol. 2006;20:1075-1083. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 262] [Cited by in F6Publishing: 252] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 7. | Lammert F, Gurusamy K, Ko CW, Miquel JF, Méndez-Sánchez N, Portincasa P, van Erpecum KJ, van Laarhoven CJ, Wang DQ. Gallstones. Nat Rev Dis Primers. 2016;2:16024. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 286] [Cited by in F6Publishing: 335] [Article Influence: 41.9] [Reference Citation Analysis (0)] |
| 8. | Stokes CS, Krawczyk M, Lammert F. Gallstones: environment, lifestyle and genes. Dig Dis. 2011;29:191-201. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 65] [Article Influence: 5.0] [Reference Citation Analysis (1)] |
| 9. | Malone BS, Werlin SL. Cholecystectomy and cholelithiasis in sickle cell anemia. Am J Dis Child. 1988;142:799-800. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Marchetti M, Quaglini S, Barosi G. Prophylactic splenectomy and cholecystectomy in mild hereditary spherocytosis: analyzing the decision in different clinical scenarios. J Intern Med. 1998;244:217-226. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Gonzalez-Escobedo G, Marshall JM, Gunn JS. Chronic and acute infection of the gall bladder by Salmonella Typhi: understanding the carrier state. Nat Rev Microbiol. 2011;9:9-14. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 188] [Cited by in F6Publishing: 196] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 12. | Kratzer W, Mason RA, Kächele V. Prevalence of gallstones in sonographic surveys worldwide. J Clin Ultrasound. 1999;27:1-7. [PubMed] [DOI] [Cited in This Article: ] |
| 13. | Barbara L, Sama C, Morselli Labate AM, Taroni F, Rusticali AG, Festi D, Sapio C, Roda E, Banterle C, Puci A. A population study on the prevalence of gallstone disease: the Sirmione Study. Hepatology. 1987;7:913-917. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 353] [Cited by in F6Publishing: 315] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 14. | Chen CH, Huang MH, Yang JC, Nien CK, Etheredge GD, Yang CC, Yeh YH, Wu HS, Chou DA, Yueh SK. Prevalence and risk factors of gallstone disease in an adult population of Taiwan: an epidemiological survey. J Gastroenterol Hepatol. 2006;21:1737-1743. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 107] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 15. | Sakorafas GH, Milingos D, Peros G. Asymptomatic cholelithiasis: is cholecystectomy really needed? Dig Dis Sci. 2007;52:1313-1325. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 128] [Cited by in F6Publishing: 120] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 16. | Portincasa P, Di Ciaula A, de Bari O, Garruti G, Palmieri VO, Wang DQ. Management of gallstones and its related complications. Expert Rev Gastroenterol Hepatol. 2016;10:93-112. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 17. | Wada K, Wada K, Imamura T. [Natural course of asymptomatic gallstone disease]. Nihon Rinsho. 1993;51:1737-1743. [PubMed] [Cited in This Article: ] |
| 18. | Portincasa P, Moschetta A, Palasciano G. Cholesterol gallstone disease. Lancet. 2006;368:230-239. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 441] [Cited by in F6Publishing: 428] [Article Influence: 23.8] [Reference Citation Analysis (1)] |
| 19. | Grimaldi CH, Nelson RG, Pettitt DJ, Sampliner RE, Bennett PH, Knowler WC. Increased mortality with gallstone disease: results of a 20-year population-based survey in Pima Indians. Ann Intern Med. 1993;118:185-190. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 37] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Ruhl CE, Everhart JE. Gallstone disease is associated with increased mortality in the United States. Gastroenterology. 2011;140:508-516. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 135] [Cited by in F6Publishing: 114] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 21. | Zheng Y, Xu M, Heianza Y, Ma W, Wang T, Sun D, Albert CM, Hu FB, Rexrode KM, Manson JE, Qi L. Gallstone disease and increased risk of mortality: Two large prospective studies in US men and women. J Gastroenterol Hepatol. 2018;33:1925-1931. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 15] [Article Influence: 2.5] [Reference Citation Analysis (1)] |
| 22. | Shabanzadeh DM, Sørensen LT, Jørgensen T. Gallstone disease and mortality: a cohort study. Int J Public Health. 2017;62:353-360. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 17] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 23. | Gutt C, Schläfer S, Lammert F. The Treatment of Gallstone Disease. Dtsch Arztebl Int. 2020;117:148-158. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 24. | Yamashita Y, Takada T, Kawarada Y, Nimura Y, Hirota M, Miura F, Mayumi T, Yoshida M, Strasberg S, Pitt HA, de Santibanes E, Belghiti J, Büchler MW, Gouma DJ, Fan ST, Hilvano SC, Lau JW, Kim SW, Belli G, Windsor JA, Liau KH, Sachakul V. Surgical treatment of patients with acute cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007;14:91-97. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 138] [Cited by in F6Publishing: 111] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 25. | Argiriov Y, Dani M, Tsironis C, Koizia LJ. Cholecystectomy for Complicated Gallbladder and Common Biliary Duct Stones: Current Surgical Management. Front Surg. 2020;7:42. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Glasgow RE, Cho M, Hutter MM, Mulvihill SJ. The spectrum and cost of complicated gallstone disease in California. Arch Surg. 2000;135:1021-5; discussion 1025. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 54] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 27. | Schwesinger WH, Diehl AK. Changing indications for laparoscopic cholecystectomy. Stones without symptoms and symptoms without stones. Surg Clin North Am. 1996;76:493-504. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 51] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 28. | Reynolds W Jr. The first laparoscopic cholecystectomy. JSLS. 2001;5:89-94. [PubMed] [Cited in This Article: ] |
| 29. | Festi D, Reggiani ML, Attili AF, Loria P, Pazzi P, Scaioli E, Capodicasa S, Romano F, Roda E, Colecchia A. Natural history of gallstone disease: Expectant management or active treatment? J Gastroenterol Hepatol. 2010;25:719-724. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 106] [Cited by in F6Publishing: 91] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 30. | Attili AF, De Santis A, Capri R, Repice AM, Maselli S. The natural history of gallstones: the GREPCO experience. The GREPCO Group. Hepatology. 1995;21:655-660. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 177] [Cited by in F6Publishing: 144] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 31. | Shabanzadeh DM, Sørensen LT, Jørgensen T. A Prediction Rule for Risk Stratification of Incidentally Discovered Gallstones: Results From a Large Cohort Study. Gastroenterology. 2016;150:156-167.e1. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 64] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 32. | Angelico F, Del Ben M, Barbato A, Conti R, Urbinati G. Ten-year incidence and natural history of gallstone disease in a rural population of women in central Italy. The Rome Group for the Epidemiology and Prevention of Cholelithiasis (GREPCO). Ital J Gastroenterol Hepatol. 1997;29:249-254. [PubMed] [Cited in This Article: ] |
| 33. | Halldestam I, Enell EL, Kullman E, Borch K. Development of symptoms and complications in individuals with asymptomatic gallstones. Br J Surg. 2004;91:734-738. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 228] [Cited by in F6Publishing: 204] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 34. | Riall TS, Adhikari D, Parmar AD, Linder SK, Dimou FM, Crowell W, Tamirisa NP, Townsend CM Jr, Goodwin JS. The risk paradox: use of elective cholecystectomy in older patients is independent of their risk of developing complications. J Am Coll Surg. 2015;220:682-690. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 35. | Riall TS, Zhang D, Townsend CM Jr, Kuo YF, Goodwin JS. Failure to perform cholecystectomy for acute cholecystitis in elderly patients is associated with increased morbidity, mortality, and cost. J Am Coll Surg. 2010;210:668-677, 677. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 145] [Cited by in F6Publishing: 145] [Article Influence: 10.4] [Reference Citation Analysis (1)] |
| 36. | Schmidt M, Søndenaa K, Vetrhus M, Berhane T, Eide GE. A randomized controlled study of uncomplicated gallstone disease with a 14-year follow-up showed that operation was the preferred treatment. Dig Surg. 2011;28:270-276. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 37. | Schmidt M, Søndenaa K, Vetrhus M, Berhane T, Eide GE. Long-term follow-up of a randomized controlled trial of observation versus surgery for acute cholecystitis: non-operative management is an option in some patients. Scand J Gastroenterol. 2011;46:1257-1262. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 44] [Cited by in F6Publishing: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 38. | Williams TP, Dimou FM, Adhikari D, Kimbrough TD, Riall TS. Hospital readmission after emergency room visit for cholelithiasis. J Surg Res. 2015;197:318-323. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 39. | Flum DR, Dellinger EP, Cheadle A, Chan L, Koepsell T. Intraoperative cholangiography and risk of common bile duct injury during cholecystectomy. JAMA. 2003;289:1639-1644. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 334] [Cited by in F6Publishing: 298] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 40. | Shamiyeh A, Wayand W. Laparoscopic cholecystectomy: early and late complications and their treatment. Langenbecks Arch Surg. 2004;389:164-171. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 66] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 41. | Shirah BH, Shirah HA, Zafar SH, Albeladi KB. Clinical patterns of postcholecystectomy syndrome. Ann Hepatobiliary Pancreat Surg. 2018;22:52-57. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 42. | Girometti R, Brondani G, Cereser L, Como G, Del Pin M, Bazzocchi M, Zuiani C. Post-cholecystectomy syndrome: spectrum of biliary findings at magnetic resonance cholangiopancreatography. Br J Radiol. 2010;83:351-361. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 43. | Schofer JM. Biliary causes of postcholecystectomy syndrome. J Emerg Med. 2010;39:406-410. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 38] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 44. | Terhaar OA, Abbas S, Thornton FJ, Duke D, O'Kelly P, Abdullah K, Varghese JC, Lee MJ. Imaging patients with "post-cholecystectomy syndrome": an algorithmic approach. Clin Radiol. 2005;60:78-84. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 25] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 45. | Jaunoo SS, Mohandas S, Almond LM. Postcholecystectomy syndrome (PCS). Int J Surg. 2010;8:15-17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 83] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 46. | Frost F, Kacprowski T, Rühlemann M, Weiss S, Bang C, Franke A, Pietzner M, Aghdassi AA, Sendler M, Völker U, Völzke H, Mayerle J, Weiss FU, Homuth G, Lerch MM. Carrying asymptomatic gallstones is not associated with changes in intestinal microbiota composition and diversity but cholecystectomy with significant dysbiosis. Sci Rep. 2021;11:6677. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 47. | Zhang Y, Liu H, Li L, Ai M, Gong Z, He Y, Dong Y, Xu S, Wang J, Jin B, Liu J, Teng Z. Cholecystectomy can increase the risk of colorectal cancer: A meta-analysis of 10 cohort studies. PLoS One. 2017;12:e0181852. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 48. | Hsu RY, Chan CH, Spicer JD, Rousseau MC, Giannias B, Rousseau S, Ferri LE. LPS-induced TLR4 signaling in human colorectal cancer cells increases beta1 integrin-mediated cell adhesion and liver metastasis. Cancer Res. 2011;71:1989-1998. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 184] [Cited by in F6Publishing: 203] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 49. | Gach T, Bogacki P, Markowska B, Szura M. Quality of Life after Laparoscopic Cholecystectomy: Single-Center Experience. J Am Coll Surg. 2020;231:e135-e136. [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (3)] |
| 50. | Boerma D, Rauws EA, Keulemans YC, Bergman JJ, Obertop H, Huibregtse K, Gouma DJ. Impaired quality of life 5 years after bile duct injury during laparoscopic cholecystectomy: a prospective analysis. Ann Surg. 2001;234:750-757. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 160] [Cited by in F6Publishing: 148] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 51. | de Reuver PR, Sprangers MA, Rauws EA, Lameris JS, Busch OR, van Gulik TM, Gouma DJ. Impact of bile duct injury after laparoscopic cholecystectomy on quality of life: a longitudinal study after multidisciplinary treatment. Endoscopy. 2008;40:637-643. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 71] [Cited by in F6Publishing: 71] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 52. | Quintana JM, Aróstegui I, Cabriada J, López de Tejada I, Perdigo L. Predictors of improvement in health-related quality of life in patients undergoing cholecystectomy. Br J Surg. 2003;90:1549-1555. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 53. | Huang-Fu L, Qian YH, Qian MJ. The correlation between postoperative complications of ERCP and quality of life after discharge in patients with choledocholithiasis. Ann Palliat Med. 2021;10:7794-7801. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 54. | Giuliano AE, Boolbol S, Degnim A, Kuerer H, Leitch AM, Morrow M. Society of Surgical Oncology: position statement on prophylactic mastectomy. Approved by the Society of Surgical Oncology Executive Council, March 2007. Ann Surg Oncol. 2007;14:2425-2427. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 91] [Cited by in F6Publishing: 96] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 55. | Hawley ST, Jagsi R, Morrow M, Janz NK, Hamilton A, Graff JJ, Katz SJ. Social and Clinical Determinants of Contralateral Prophylactic Mastectomy. JAMA Surg. 2014;149:582-589. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 129] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 56. | Spear SL, Carter ME, Schwarz K. Prophylactic mastectomy: indications, options, and reconstructive alternatives. Plast Reconstr Surg. 2005;115:891-909. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 69] [Cited by in F6Publishing: 70] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 57. | Tuttle TM, Jarosek S, Habermann EB, Arrington A, Abraham A, Morris TJ, Virnig BA. Increasing rates of contralateral prophylactic mastectomy among patients with ductal carcinoma in situ. J Clin Oncol. 2009;27:1362-1367. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 267] [Cited by in F6Publishing: 274] [Article Influence: 18.3] [Reference Citation Analysis (0)] |
| 58. | Feuer EJ, Wun LM, Boring CC, Flanders WD, Timmel MJ, Tong T. The lifetime risk of developing breast cancer. J Natl Cancer Inst. 1993;85:892-897. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 324] [Cited by in F6Publishing: 342] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 59. | Pharoah P, Mackay J. Absolute risk of breast cancer in women at increased risk: a more useful clinical measure than relative risk? The Breast. 1998;7:255-259. [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 60. | Struewing JP, Abeliovich D, Peretz T, Avishai N, Kaback MM, Collins FS, Brody LC. The carrier frequency of the BRCA1 185delAG mutation is approximately 1 percent in Ashkenazi Jewish individuals. Nat Genet. 1995;11:198-200. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 421] [Cited by in F6Publishing: 417] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 61. | Zendejas B, Moriarty JP, O'Byrne J, Degnim AC, Farley DR, Boughey JC. Cost-effectiveness of contralateral prophylactic mastectomy versus routine surveillance in patients with unilateral breast cancer. J Clin Oncol. 2011;29:2993-3000. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 65] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 62. | Lostumbo L, Carbine NE, Wallace J. Prophylactic mastectomy for the prevention of breast cancer. Cochrane Database Syst Rev. 2010;CD002748. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 100] [Cited by in F6Publishing: 156] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 63. | Tuttle TM, Abbott A, Arrington A, Rueth N. The increasing use of prophylactic mastectomy in the prevention of breast cancer. Curr Oncol Rep. 2010;12:16-21. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 64] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 64. | Diehl AK. Gallstone size and the risk of gallbladder cancer. JAMA. 1983;250:2323-2326. [PubMed] [Cited in This Article: ] |
| 65. | Hamdani NH, Qadri SK, Aggarwalla R, Bhartia VK, Chaudhuri S, Debakshi S, Baig SJ, Pal NK. Clinicopathological study of gall bladder carcinoma with special reference to gallstones: our 8-year experience from eastern India. Asian Pac J Cancer Prev. 2012;13:5613-5617. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 66. | Hsing AW, Gao YT, Han TQ, Rashid A, Sakoda LC, Wang BS, Shen MC, Zhang BH, Niwa S, Chen J, Fraumeni JF Jr. Gallstones and the risk of biliary tract cancer: a population-based study in China. Br J Cancer. 2007;97:1577-1582. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 161] [Cited by in F6Publishing: 172] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 67. | Perpetuo MD, Valdivieso M, Heilbrun LK, Nelson RS, Connor T, Bodey GP. Natural history study of gallbladder cancer: a review of 36 years experience at M. D. Anderson Hospital and Tumor Institute. Cancer. 1978;42:330-335. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 68. | Lowenfels AB, Lindström CG, Conway MJ, Hastings PR. Gallstones and risk of gallbladder cancer. J Natl Cancer Inst. 1985;75:77-80. [PubMed] [Cited in This Article: ] |
| 69. | Wanjura V, Sandblom G. How Do Quality-of-Life and Gastrointestinal Symptoms Differ Between Post-cholecystectomy Patients and the Background Population? World J Surg. 2016;40:81-88. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 70. | Behari A, Kapoor VK. Asymptomatic Gallstones (AsGS) - To Treat or Not to? Indian J Surg. 2012;74:4-12. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 71. | Meshikhes AW. Asymptomatic gallstones in the laparoscopic era. J R Coll Surg Edinb. 2002;47:742-748. [PubMed] [Cited in This Article: ] |
| 72. | Ellimoottil C, Miller S, Ayanian JZ, Miller DC. Effect of insurance expansion on utilization of inpatient surgery. JAMA Surg. 2014;149:829-836. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 73. | Barros AJ, Bastos JL, Dâmaso AH. Catastrophic spending on health care in Brazil: private health insurance does not seem to be the solution. Cad Saude Publica. 2011;27 Suppl 2:S254-S262. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 74. | Tan CH, Pang TC, Woon WW, Low JK, Junnarkar SP. Analysis of actual healthcare costs of early versus interval cholecystectomy in acute cholecystitis. J Hepatobiliary Pancreat Sci. 2015;22:237-243. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 75. | European Association for the Study of the Liver (EASL). EASL Clinical Practice Guidelines on the prevention, diagnosis and treatment of gallstones. J Hepatol. 2016;65:146-181. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 268] [Cited by in F6Publishing: 255] [Article Influence: 31.9] [Reference Citation Analysis (1)] |
| 76. | Abraham S, Rivero HG, Erlikh IV, Griffith LF, Kondamudi VK. Surgical and nonsurgical management of gallstones. Am Fam Physician. 2014;89:795-802. [PubMed] [Cited in This Article: ] |
| 77. | Gracie WA, Ransohoff DF. The natural history of silent gallstones: the innocent gallstone is not a myth. N Engl J Med. 1982;307:798-800. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 430] [Cited by in F6Publishing: 430] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 78. | Friedman LS, Roberts MS, Brett AS, Marton KI. Management of asymptomatic gallstones in the diabetic patient. A decision analysis. Ann Intern Med. 1988;109:913-919. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 24] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 79. | Thistle JL, Cleary PA, Lachin JM, Tyor MP, Hersh T. The natural history of cholelithiasis: the National Cooperative Gallstone Study. Ann Intern Med. 1984;101:171-175. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 182] [Cited by in F6Publishing: 138] [Article Influence: 3.5] [Reference Citation Analysis (2)] |
| 80. | Lachman BS, Lazerson J, Starshak RJ, Vaughters FM, Werlin SL. The prevalence of cholelithiasis in sickle cell disease as diagnosed by ultrasound and cholecystography. Pediatrics. 1979;64:601-603. [PubMed] [Cited in This Article: ] |
| 81. | Rennels MB, Dunne MG, Grossman NJ, Schwartz AD. Cholelithiasis in patients with major sickle hemoglobinopathies. Am J Dis Child. 1984;138:66-67. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 18] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 82. | Sarnaik S, Slovis TL, Corbett DP, Emami A, Whitten CF. Incidence of cholelithiasis in sickle cell anemia using the ultrasonic gray-scale technique. J Pediatr. 1980;96:1005-1008. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 91] [Cited by in F6Publishing: 97] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 83. | Barrett-Connor E. Cholelithiasis in sickle cell anemia. Am J Med. 1968;45:889-898. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 46] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 84. | Bond LR, Hatty SR, Horn ME, Dick M, Meire HB, Bellingham AJ. Gall stones in sickle cell disease in the United Kingdom. Br Med J (Clin Res Ed). 1987;295:234-236. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 60] [Cited by in F6Publishing: 69] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 85. | Rutledge R, Croom RD 3rd, Davis JW Jr, Berkowitz LR, Orringer EP. Cholelithiasis in sickle cell anemia: surgical considerations. South Med J. 1986;79:28-30. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 25] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 86. | Muroni M, Loi V, Lionnet F, Girot R, Houry S. Prophylactic laparoscopic cholecystectomy in adult sickle cell disease patients with cholelithiasis: A prospective cohort study. Int J Surg. 2015;22:62-66. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 87. | Al-Salem AH. Should cholecystectomy be performed concomitantly with splenectomy in children with sickle-cell disease? Pediatr Surg Int. 2003;19:71-74. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 88. | Patton ML, Moss BE, Haith LR Jr, Shotwell BA, Milliner DH, Simeone MR, Kraut JD, Patton JN. Concomitant laparoscopic cholecystectomy and splenectomy for surgical management of hereditary spherocytosis. Am Surg. 1997;63:536-539. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 89. | Sasaki A, Nitta H, Otuska K, Kimura Y, Obuchi T, Wakabayashi G. Concomitant laparoscopic splenectomy and cholecystectomy. Surg Laparosc Endosc Percutan Tech. 2010;20:66-68. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 90. | Vecchio R, Intagliata E, Marchese S, La Corte F, Cacciola RR, Cacciola E. Laparoscopic splenectomy coupled with laparoscopic cholecystectomy. JSLS. 2014;18:252-257. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 91. | Lord RV, Ho S, Coleman MJ, Spratt PM. Cholecystectomy in cardiothoracic organ transplant recipients. Arch Surg. 1998;133:73-79. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 92. | Milas M, Ricketts RR, Amerson JR, Kanter K. Management of biliary tract stones in heart transplant patients. Ann Surg. 1996;223:747-53; discussion 753. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 27] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 93. | Peterseim DS, Pappas TN, Meyers CH, Shaeffer GS, Meyers WC, Van Trigt P. Management of biliary complications after heart transplantation. J Heart Lung Transplant. 1995;14:623-631. [PubMed] [Cited in This Article: ] |
| 94. | Graham SM, Flowers JL, Schweitzer E, Bartlett ST, Imbembo AL. The utility of prophylactic laparoscopic cholecystectomy in transplant candidates. Am J Surg. 1995;169:44-8; discussion 48. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 46] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 95. | Kao LS, Flowers C, Flum DR. Prophylactic cholecystectomy in transplant patients: a decision analysis. J Gastrointest Surg. 2005;9:965-972. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 37] [Cited by in F6Publishing: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 96. | Paisley AN, Roberts ME, Trainer PJ. Withdrawal of somatostatin analogue therapy in patients with acromegaly is associated with an increased risk of acute biliary problems. Clin Endocrinol (Oxf). 2007;66:723-726. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 97. | Brighi N, Lamberti G, Maggio I, Manuzzi L, Ricci C, Casadei R, Santini D, Mosconi C, Lisotti A, Ambrosini V, Pantaleo MA, Campana D. Biliary stone disease in patients receiving somatostatin analogs for neuroendocrine neoplasms. A retrospective observational study. Dig Liver Dis. 2019;51:689-694. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 98. | Sinnamon AJ, Neuwirth MG, Vining CC, Sharoky CE, Yang YX, Kelz RR, Fraker DL, Roses RE, Karakousis GC. Prophylactic Cholecystectomy at Time of Surgery for Small Bowel Neuroendocrine Tumor Does Not Increase Postoperative Morbidity. Ann Surg Oncol. 2018;25:239-245. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 99. | Aucott JN, Cooper GS, Bloom AD, Aron DC. Management of gallstones in diabetic patients. Arch Intern Med. 1993;153:1053-1058. [PubMed] [Cited in This Article: ] |
| 100. | Elmasry M, Lindop D, Dunne DF, Malik H, Poston GJ, Fenwick SW. The risk of malignancy in ultrasound detected gallbladder polyps: A systematic review. Int J Surg. 2016;33 Pt A:28-35. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 101. | Lowenfels AB, Walker AM, Althaus DP, Townsend G, Domellöf L. Gallstone growth, size, and risk of gallbladder cancer: an interracial study. Int J Epidemiol. 1989;18:50-54. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 108] [Cited by in F6Publishing: 92] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 102. | Plecka Östlund M, Wenger U, Mattsson F, Ebrahim F, Botha A, Lagergren J. Population-based study of the need for cholecystectomy after obesity surgery. Br J Surg. 2012;99:864-869. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 103. | Patiño JF, Quintero GA. Asymptomatic cholelithiasis revisited. World J Surg. 1998;22:1119-1124. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 38] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 104. | Warschkow R, Tarantino I, Ukegjini K, Beutner U, Güller U, Schmied BM, Müller SA, Schultes B, Thurnheer M. Concomitant cholecystectomy during laparoscopic Roux-en-Y gastric bypass in obese patients is not justified: a meta-analysis. Obes Surg. 2013;23:397-407. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 111] [Cited by in F6Publishing: 117] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 105. | McSherry CK, Ferstenberg H, Calhoun WF, Lahman E, Virshup M. The natural history of diagnosed gallstone disease in symptomatic and asymptomatic patients. Ann Surg. 1985;202:59-63. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 239] [Cited by in F6Publishing: 212] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 106. | Ponte E, Panebianco A, Morena S. [Diabetic enteropathy]. Minerva Med. 1990;81:335-340. [PubMed] [Cited in This Article: ] |
| 107. | Ekbom A, Hsieh CC, Yuen J, Trichopoulos D, McLaughlin JK, Lan SJ, Adami HO. Risk of extrahepatic bileduct cancer after cholecystectomy. Lancet. 1993;342:1262-1265. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 47] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 108. | Scollay JM, Mullen R, McPhillips G, Thompson AM. Mortality associated with the treatment of gallstone disease: a 10-year contemporary national experience. World J Surg. 2011;35:643-647. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 109. | To KB, Cherry-Bukowiec JR, Englesbe MJ, Terjimanian MN, Shijie C, Campbell DA Jr, Napolitano LM. Emergent versus elective cholecystectomy: conversion rates and outcomes. Surg Infect (Larchmt). 2013;14:512-519. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 110. | Steiner CA, Bass EB, Talamini MA, Pitt HA, Steinberg EP. Surgical rates and operative mortality for open and laparoscopic cholecystectomy in Maryland. N Engl J Med. 1994;330:403-408. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 241] [Cited by in F6Publishing: 292] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 111. | Yano H, Kinuta M, Iwazawa T, Kanoh T, Monden T. Laparoscopic cholecystectomy for asymptomatic cholelithiasis. Digest Endos. 15:190-195. [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 112. | Kama NA, Kologlu M, Doganay M, Reis E, Atli M, Dolapci M. A risk score for conversion from laparoscopic to open cholecystectomy. Am J Surg. 2001;181:520-525. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 102] [Cited by in F6Publishing: 109] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 113. | Licciardello A, Arena M, Nicosia A, Di Stefano B, Calì G, Arena G, Minutolo V. Preoperative risk factors for conversion from laparoscopic to open cholecystectomy. Eur Rev Med Pharmacol Sci. 2014;18:60-68. [PubMed] [Cited in This Article: ] |
| 114. | Amirthalingam V, Low JK, Woon W, Shelat V. Tokyo Guidelines 2013 may be too restrictive and patients with moderate and severe acute cholecystitis can be managed by early cholecystectomy too. Surg Endosc. 2017;31:2892-2900. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 48] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 115. | Milingos S, Kallipolitis G, Loutradis D, Liapi A, Mavrommatis K, Drakakis P, Tourikis J, Creatsas G, Michalas S. Adhesions: laparoscopic surgery versus laparotomy. Ann N Y Acad Sci. 2000;900:272-285. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 45] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 116. | Lo CM, Fan ST, Liu CL, Lai EC, Wong J. Early decision for conversion of laparoscopic to open cholecystectomy for treatment of acute cholecystitis. Am J Surg. 1997;173:513-517. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 77] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 117. | Iwashita Y, Ohyama T, Honda G, Hibi T, Yoshida M, Miura F, Takada T, Han HS, Hwang TL, Shinya S, Suzuki K, Umezawa A, Yoon YS, Choi IS, Huang WS, Chen KH, Watanabe M, Abe Y, Misawa T, Nagakawa Y, Yoon DS, Jang JY, Yu HC, Ahn KS, Kim SC, Song IS, Kim JH, Yun SS, Choi SH, Jan YY, Sheen-Chen SM, Shan YS, Ker CG, Chan DC, Lee KT, Toyota N, Higuchi R, Nakamura Y, Mizuguchi Y, Takeda Y, Ito M, Norimizu S, Yamada S, Matsumura N, Shindoh J, Sunagawa H, Hasegawa H, Rikiyama T, Sata N, Kano N, Kitano S, Tokumura H, Yamashita Y, Watanabe G, Nakagawa K, Kimura T, Yamakawa T, Wakabayashi G, Endo I, Miyazaki M, Yamamoto M. What are the appropriate indicators of surgical difficulty during laparoscopic cholecystectomy? J Hepatobiliary Pancreat Sci. 2016;23:533-547. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 41] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 118. | Kuldip S, Ashish O. Difficult laparoscopic cholecystectomy: A large series from north India. Indian J Surg. 2006;68:205-208. [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 119. | Törnqvist B, Waage A, Zheng Z, Ye W, Nilsson M. Severity of Acute Cholecystitis and Risk of Iatrogenic Bile Duct Injury During Cholecystectomy, a Population-Based Case-Control Study. World J Surg. 2016;40:1060-1067. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 57] [Cited by in F6Publishing: 47] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 120. | Rice CP, Vaishnavi KB, Chao C, Jupiter D, Schaeffer AB, Jenson WR, Griffin LW, Mileski WJ. Operative complications and economic outcomes of cholecystectomy for acute cholecystitis. World J Gastroenterol. 2019;25:6916-6927. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 28] [Cited by in F6Publishing: 32] [Article Influence: 6.4] [Reference Citation Analysis (2)] |
| 121. | Yeo CS, Tay VW, Low JK, Woon WW, Punamiya SJ, Shelat VG. Outcomes of percutaneous cholecystostomy and predictors of eventual cholecystectomy. J Hepatobiliary Pancreat Sci. 2016;23:65-73. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 58] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 122. | Moore DE, Feurer ID, Holzman MD, Wudel LJ, Strickland C, Gorden DL, Chari R, Wright JK, Pinson CW. Long-term detrimental effect of bile duct injury on health-related quality of life. Arch Surg. 2004;139:476-81; discussion 481. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 85] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 123. | Andersson R, Eriksson K, Blind PJ, Tingstedt B. Iatrogenic bile duct injury--a cost analysis. HPB (Oxford). 2008;10:416-419. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 31] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 124. | Halle-Smith JM, Hodson J, Stevens LG, Dasari B, Marudanayagam R, Perera T, Sutcliffe RP, Muiesan P, Isaac J, Mirza DF, Roberts KJ. A comprehensive evaluation of the long-term clinical and economic impact of minor bile duct injury. Surgery. 2020;167:942-949. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 125. | Palanivelu C, Rajan PS, Jani K, Shetty AR, Sendhilkumar K, Senthilnathan P, Parthasarthi R. Laparoscopic cholecystectomy in cirrhotic patients: the role of subtotal cholecystectomy and its variants. J Am Coll Surg. 2006;203:145-151. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 80] [Cited by in F6Publishing: 80] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 126. | Elshaer M, Gravante G, Thomas K, Sorge R, Al-Hamali S, Ebdewi H. Subtotal cholecystectomy for "difficult gallbladders": systematic review and meta-analysis. JAMA Surg. 2015;150:159-168. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 172] [Cited by in F6Publishing: 188] [Article Influence: 20.9] [Reference Citation Analysis (0)] |
| 127. | Harilingam MR, Shrestha AK, Basu S. Laparoscopic modified subtotal cholecystectomy for difficult gall bladders: A single-centre experience. J Minim Access Surg. 2016;12:325-329. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 128. | Koo JGA, Chan YH, Shelat VG. Laparoscopic subtotal cholecystectomy: comparison of reconstituting and fenestrating techniques. Surg Endosc. 2021;35:1014-1024. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 28] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 129. | LUND J. Surgical indications in cholelithiasis: prophylactic choleithiasis: prophylactic cholecystectomy elucidated on the basis of long-term follow up on 526 nonoperated cases. Ann Surg. 1960;151:153-162. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 147] [Cited by in F6Publishing: 161] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 130. | Gurusamy KS, Davidson BR. Gallstones. BMJ. 2014;348:g2669. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 61] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 131. | National Institutes of Health Consensus Development Conference Statement on Gallstones and Laparoscopic Cholecystectomy. Am J Surg. 1993;165:390-398. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 162] [Cited by in F6Publishing: 168] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 132. | Cagir B, Rangraj M, Maffuci L, Herz BL. The learning curve for laparoscopic cholecystectomy. J Laparoendosc Surg. 1994;4:419-427. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 74] [Cited by in F6Publishing: 70] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 133. | Lee VS, Chari RS, Cucchiaro G, Meyers WC. Complications of laparoscopic cholecystectomy. Am J Surg. 1993;165:527-532. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 95] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 134. | Parmeggiani D, Cimmino G, Cerbone D, Avenia N, Ruggero R, Gubitosi A, Docimo G, Mordente S, Misso C, Parmeggiani U. Biliary tract injuries during laparoscopic cholecystectomy: three case reports and literature review. G Chir. 2010;31:16-19. [PubMed] [Cited in This Article: ] |
| 135. | Pucher PH, Brunt LM, Fanelli RD, Asbun HJ, Aggarwal R. SAGES expert Delphi consensus: critical factors for safe surgical practice in laparoscopic cholecystectomy. Surg Endosc. 2015;29:3074-3085. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 100] [Cited by in F6Publishing: 98] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 136. | Vettoretto N, Saronni C, Harbi A, Balestra L, Taglietti L, Giovanetti M. Critical view of safety during laparoscopic cholecystectomy. JSLS. 2011;15:322-325. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 49] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 137. | Osborne DA, Alexander G, Boe B, Zervos EE. Laparoscopic cholecystectomy: past, present, and future. Surg Technol Int. 2006;15:81-85. [PubMed] [Cited in This Article: ] |
| 138. | Haque S, Srinivasan S. A meta-analysis of the training effectiveness of virtual reality surgical simulators. IEEE Trans Inf Technol Biomed. 2006;10:51-58. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 124] [Cited by in F6Publishing: 130] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 139. | Archer SB, Brown DW, Smith CD, Branum GD, Hunter JG. Bile duct injury during laparoscopic cholecystectomy: results of a national survey. Ann Surg. 2001;234:549-58; discussion 558. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 242] [Cited by in F6Publishing: 260] [Article Influence: 11.3] [Reference Citation Analysis (0)] |
| 140. | Gupta P, Dutta U, Rana P, Singhal M, Gulati A, Kalra N, Soundararajan R, Kalage D, Chhabra M, Sharma V, Gupta V, Yadav TD, Kaman L, Irrinki S, Singh H, Sakaray Y, Das CK, Saikia U, Nada R, Srinivasan R, Sandhu MS, Sharma R, Shetty N, Eapen A, Kaur H, Kambadakone A, de Haas R, Kapoor VK, Barreto SG, Sharma AK, Patel A, Garg P, Pal SK, Goel M, Patkar S, Behari A, Agarwal AK, Sirohi B, Javle M, Garcea G, Nervi F, Adsay V, Roa JC, Han HS. Gallbladder reporting and data system (GB-RADS) for risk stratification of gallbladder wall thickening on ultrasonography: an international expert consensus. Abdom Radiol (NY). 2022;47:554-565. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 16] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 141. | Mohan R, Wei Lynn Goh S, Tan GW, Tan YP, Junnarkar SP, Huey CWT, Low JK, Shelat VG. Validation of Tokyo Guidelines 2007 and Tokyo Guidelines 2013/2018 Criteria for Acute Cholangitis and Predictors of In-Hospital Mortality. Visc Med. 2021;37:434-442. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 142. | Teng TZJ, Tan JKT, Baey S, Gunasekaran SK, Junnarkar SP, Low JK, Huey CWT, Shelat VG. Sequential organ failure assessment score is superior to other prognostic indices in acute pancreatitis. World J Crit Care Med. 2021;10:355-368. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 10] [Cited by in F6Publishing: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |