Published online Jun 16, 2022. doi: 10.12998/wjcc.v10.i17.5789
Peer-review started: November 16, 2021
First decision: February 14, 2022
Revised: February 26, 2022
Accepted: April 3, 2022
Article in press: April 3, 2022
Published online: June 16, 2022
Processing time: 204 Days and 21.9 Hours
Continuous severe horizontal bone defect is common in the aesthetic maxillary anterior area, and presents a major challenge in implant dentistry and requires predictable bone augmentation to increase the width of the alveolar bone.
A 24-year-old man, with a history of well-controlled IgA nephropathy, presented to the Dentistry Department of our hospital complaining of missing his right maxillary anterior teeth 1 mo ago. Severe horizontal alveolar bone defects at sites of teeth 12, 13 and 14 were diagnosed. A modified guided bone regeneration surgical approach stabilizing the absorbable collagen membrane and particulate graft materials by periosteal diagonal mattress suture (PDMS) combined with four corner pins was used for this severe continuous horizontal bone defect. The outcome revealed that the newly formed alveolar ridge dimension increased from 0.72 mm to 11.55 mm horizontally 10 mo postoperatively, with no adverse events. The implant surgery was successfully performed.
This case highlights that PDMS combined with four corner pins is feasible to maintain the space and stabilize the graft and membranes in severe continuous horizontal bone defect.
Core Tip: We report a 24-year-old man with severe horizontal alveolar bone defects in the maxillary anterior teeth area. A modified guided bone regeneration surgical approach stabilizing the absorbable collagen membrane and particulate graft materials by periosteal diagonal mattress sutures (PDMS) combined with four corner pins was used for this severe continuous horizontal bone defect. The outcome revealed that the newly formed alveolar ridge dimension increased approximately 10 mm horizontally at 10 mo postoperatively. The technique PDMS combined with four corner pins may provide an alternative to traditional methods to obtain better bone regeneration.
- Citation: Wang LH, Ruan Y, Zhao WY, Chen JP, Yang F. Modified membrane fixation technique in a severe continuous horizontal bone defect: A case report. World J Clin Cases 2022; 10(17): 5789-5797
- URL: https://www.wjgnet.com/2307-8960/full/v10/i17/5789.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i17.5789
Horizontal bone defect is common in the aesthetic maxillary anterior area, and presents a major challenge in implant dentistry and often requires bone augmentation to increase the width of the alveolar bone[1,2]. Various horizontal ridge reconstruction methods have been developed[3], including guided bone regeneration (GBR), onlay bone block graft, ridge splitting and expansion, distraction osteogenesis, and sandwich osteoplasty[4]. According to the decision tree of horizontal bone augmentation[5], when the ridge width is less than 3.5 mm, onlay bone grafting with the use of an autogenic or allogenic block is the first choice for horizontal bone augmentation[6]. However, this treatment also has some complications, such as extended surgical time, cost, discomfort to patients, nerve damage or morbidity, and unavoidable bone resorption[7]. An average resorption rate is 35%-51%, and 10 years of follow-up showed the range was between 20% and 92%[8].
GBR for alveolar bone reconstruction is effective and less invasive than block grafting. Advances in biomaterials and clinical techniques have led to the incorporation of GBR as a potential alternative in these challenging cases[9]. GBR with particulate graft materials and absorbable collagen membranes is an effective technique for horizontal alveolar ridge augmentation, and additional techniques like membrane fixation and decortication may be beneficial[10]. However, GBR for large horizontal and vertical ridge defects is still a technically sensitive procedure. External pressure from the flap or the occlusal forces may displace the graft and membrane laterally and apically, resulting in deficient bone. The “PASS” principle of GBR requires the use of absorbable or nonabsorbable membranes for the creation of a stable space for the particulate graft above the bone defect and under the periosteum[11].
Membrane fixation may have beneficial implications for GBR[12,13]. Several membrane fixation techniques have been reported despite them having several clinical challenges[13-18]. Application of titanium minipins for fixation of the nonabsorbable barrier membranes could limit movement of the membrane, surrounding bone and soft tissue flap[16]. The sausage technique using a membrane fixed with titanium pins has been developed to stabilize the particle grafts and membrane[18]. However, several potential risks have been documented: Damage of the adjacent roots and underlying anatomical vital structures, and the need for an extensive reopening procedure to retrieve the nonresorbable pins[19,20]. Therefore, a technique utilizing periosteal vertical mattress suture (PVMS) for the fixation of grafts and membranes has been proposed for single implant sites, and this technique can avoid potential complications of using fixation pins[13]. Similar to PVMS, continuous periosteal strapping sutures (CPSS) have been used to fix the grafts and absorbable membranes for buccal ridge augmentation and minimize the risks and comorbidities[17]. However, all this suture techniques are all limited by the tensile strength and the resorption rate of the sutures, the time of fixation is also limited by the biodegradation period of the absorbable suture material. Another limitation is that the linear-guided suture may result in possible migration of the particulate graft material in an apicocoronal direction. Moreover, the PVMS technique may not provide enough stability for grafts in large defects, and for large ridge defects the use of pins is still recommended. In the case of large bone defects with continuous multi-tooth positions, it is still recommended to use a large number of pins to fix the membrane and grafts, which is still the first choice currently, even if it has high technical sensitivity and costly.
So far, there are still no literatures about the combination use of suture technique and titanium pins to fix the membrane and grafts. Here, we present a case using a modified membrane fixation technique for stabilizing the absorbable membrane and underlying particulate grafts in a continuous severe horizontal bone defect with an average width of only approximately 1 mm. We used GBR with the graft composed of a 1:1 mixture of autogenous bone and anorganic bovine bone mineral (ABBM), covered by bilayer absorbable membranes, fixed by periosteal diagonal mattress suture (PDMS) and four corner titanium pins.
A 24-year-old male patient was referred to the Dentistry Department of Zhejiang Provincial People’s Hospital complaining of spontaneous loss of his right maxillary anterior tooth 1 mo previously.
The patient lost his right maxillary anterior tooth 1 mo prior to referral due to excessive loosening, and now he felt that it affected his appearance and required repair.
The patient had IgA nephropathy and hypertension, which were well controlled after treatment, and the conditions have been stable for > 5 years.
The patient had no other personal or family history.
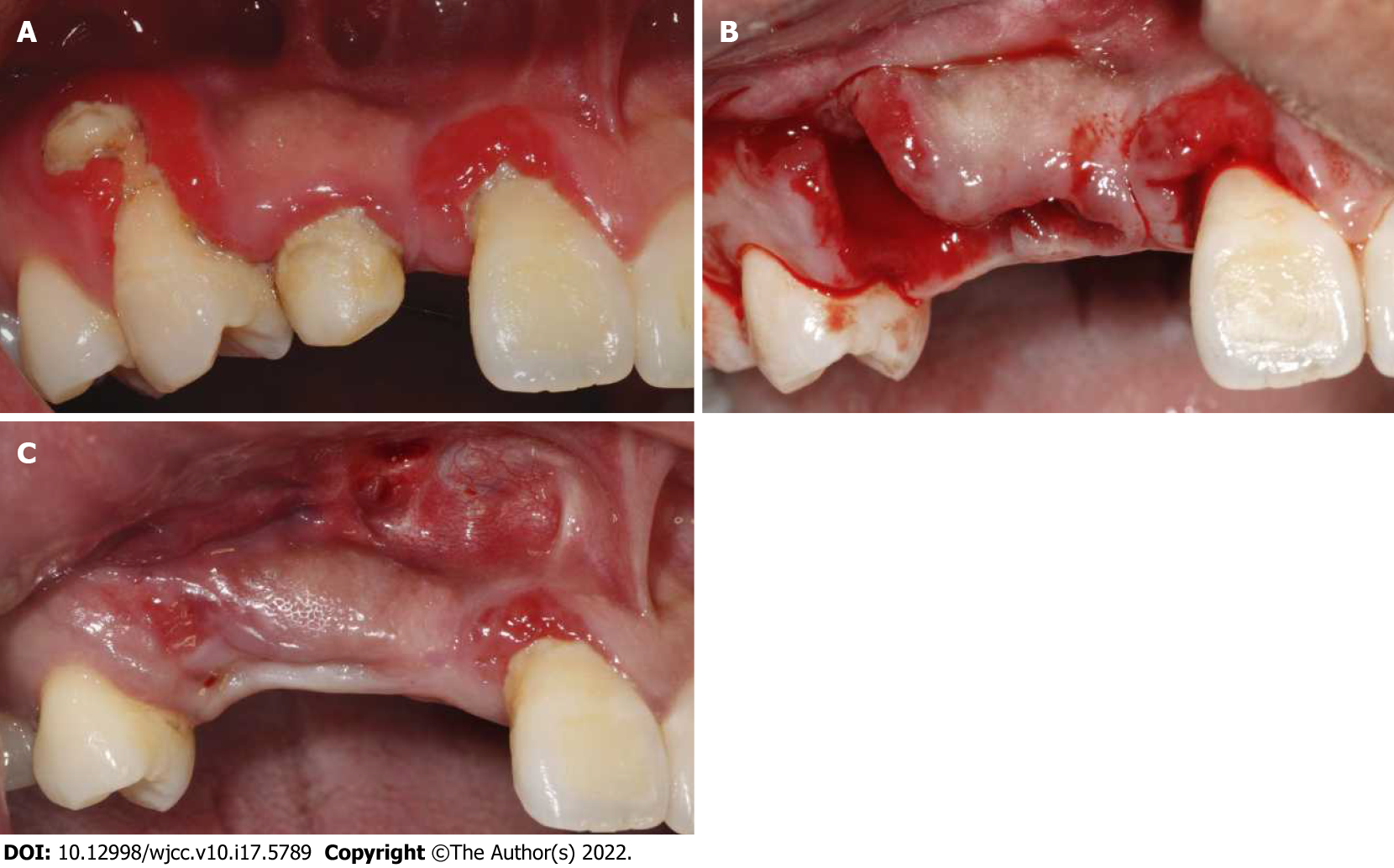
His vital sign was stable, with blood pressure of 120/82 mmHg, heart rate of 75 beats per minute and body temperature of 36.7°C. Oral examination showed tooth 12 deficiency, and deciduous tooth 53 retention with a mobility degree of II, the root of tooth 14 was exposed and the buccal alveolar bone completely absorbed, poor oral hygiene with dental calculus and bleeding on probing (Figure 1A).
Blood analysis and other laboratory findings were normal.
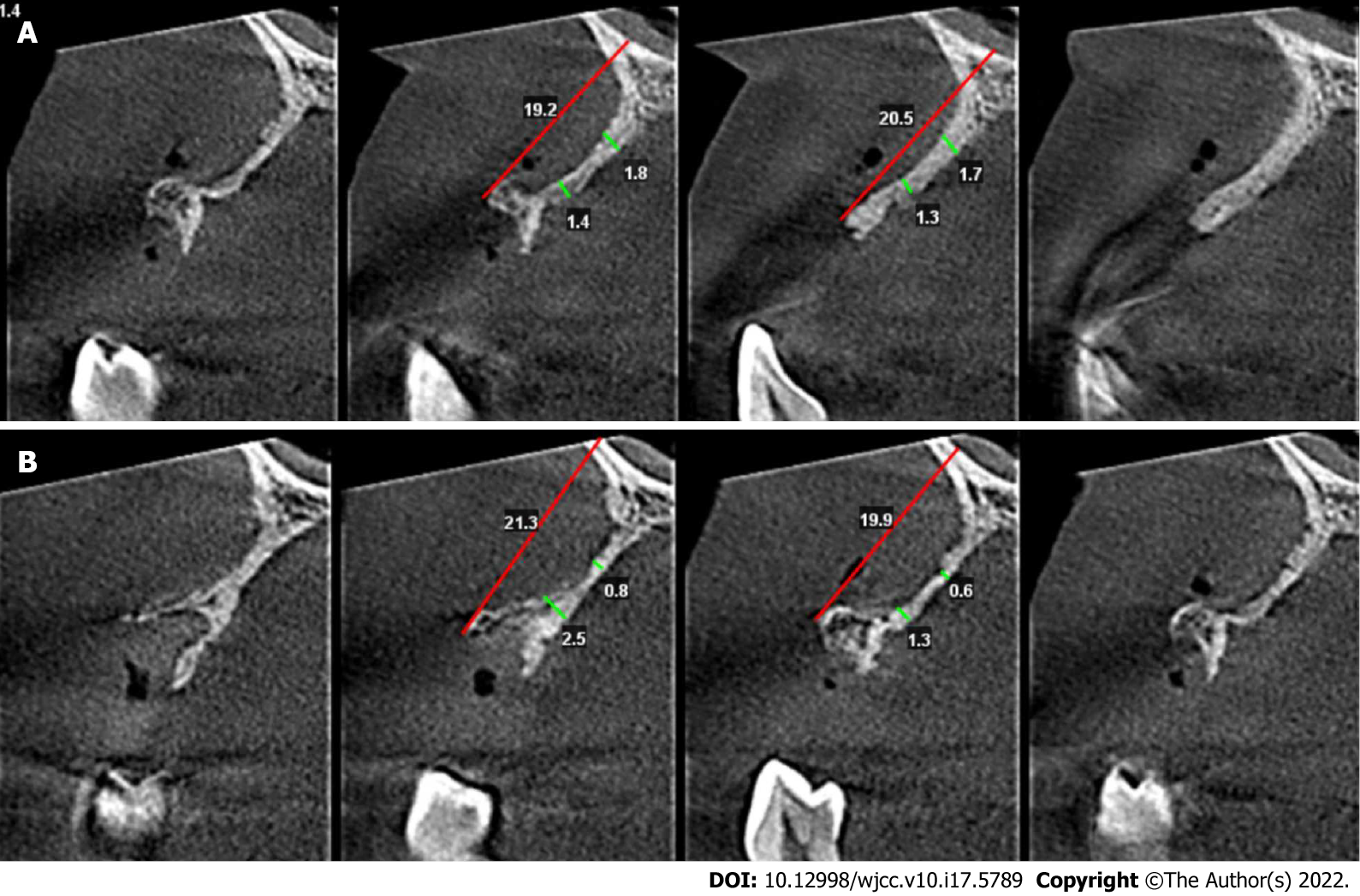
Cone beam computed tomography (CBCT) scanning revealed the vertical height of alveolar bone was sufficient (19.2-21.3 mm) but the horizontal width of alveolar crest was merely 0.6-2.5 mm.
The final diagnosis of the presented case was deficiency of tooth 12, and deciduous tooth 53 retention, severe periodontitis of tooth 14, severe continuous horizontal alveolar bone defects at sites of teeth 12, 13 and 14, and chronic gingivitis.
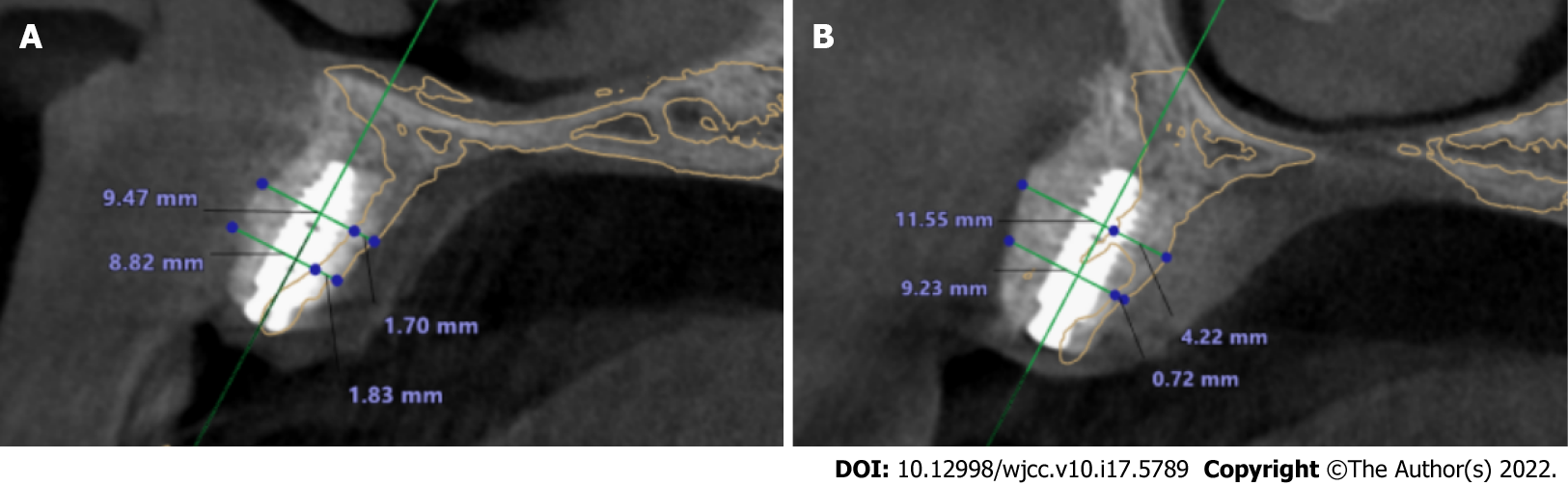
The initial treatment was extraction of teeth 53 and 14 (Figure 1B), periodontal scaling and oral hygiene maintenance. Three weeks after teeth extraction and soft tissue healing (Figure 1C), clinical examination indicated that the bone quantity of right maxillary regions was insufficient for implant placement. CBCT scanning revealed the vertical height of alveolar bone was sufficient (19.2-21.3 mm) but the horizontal width of alveolar bone was merely 0.6-2.5 mm at the site 5 mm and 10 mm below the alveolar crest at sites 12 (Figure 2A) and 14 (Figure 2B). Horizontal bone augmentation and postponed implant placement was planned for this continuous severe horizontal bone defect. Bone augmentation was treated by GBR, with the graft composed of a 1:1 mixture of autogenous bone and ABBM, covered by bilayer absorbable membranes. The graft and membranes were fixed by PDMS combined with four corner pins. This study was approved by the Zhejiang Provincial People’s Hospital Institutional Review Board (No. 2021QT267) and the participant gave signed informed consent.
Autogenous bone harvest: a vestibular incision followed by two divergent vertical incisions were made below the mucogingival border in the mandibular intercanine region under local anesthesia, and a full-thickness mucoperiostal flap was elevated to expose the bone. Autogenous bone fragments were harvested using an autogenous bone drill (Osstem, Korea) within the safety margin to the tooth apex and the mental foramen, then mixed with particle bone graft (Bio-Oss, Geistlich, Switzerland) at a ratio of 1:1. Prior to soft tissue closure of the donor site, sharp edges were removed and a gelatin sponge was applied to the remaining defect as a hemostatic dressing. The wounds were closed with 4-0 resorbable suture (Coated VICRYL, Ethicon, United States). To minimize postoperative swelling and hematoma, an extraoral pressure dressing was applied to the donor sites and maintained for 3 d.
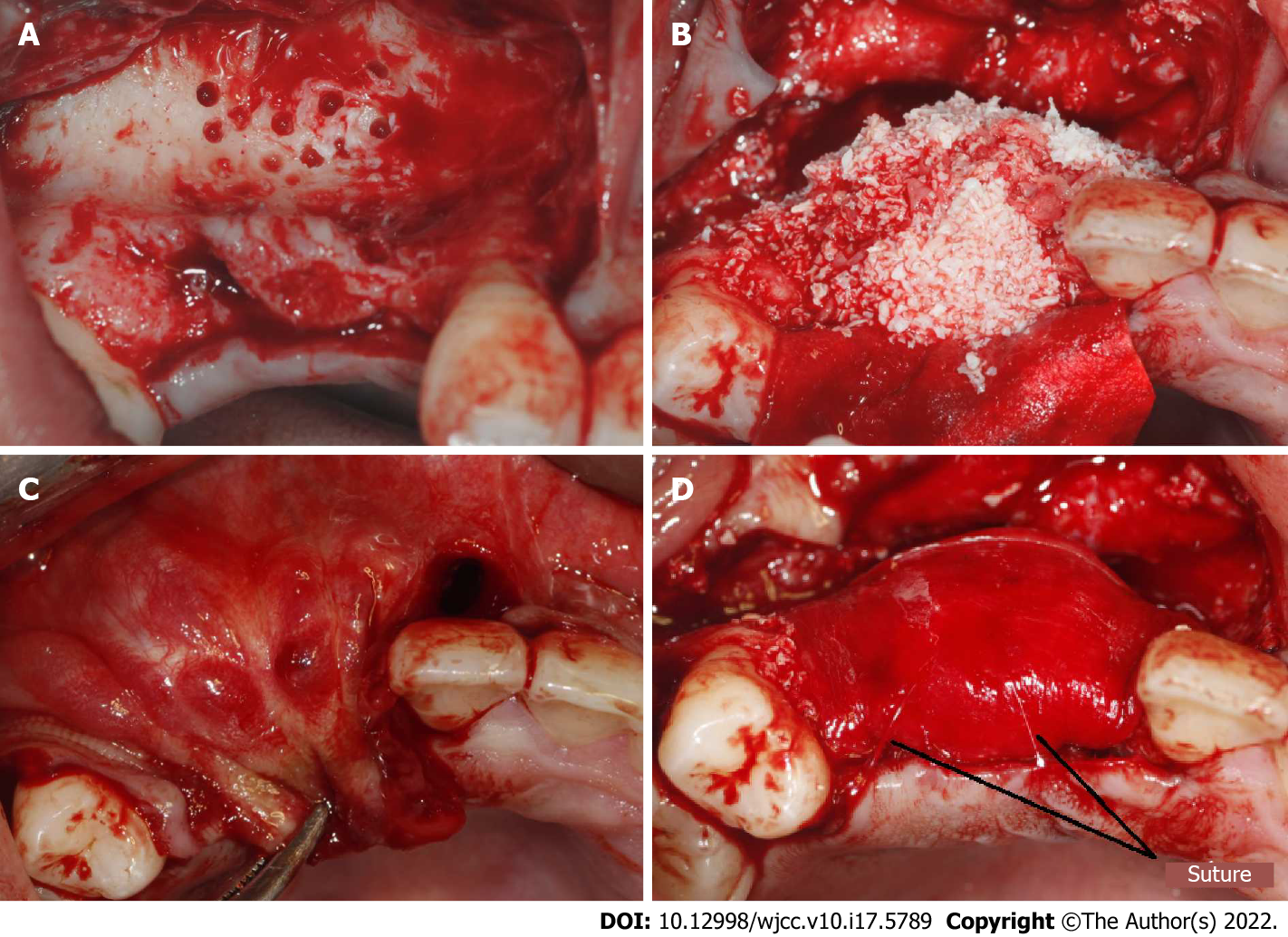
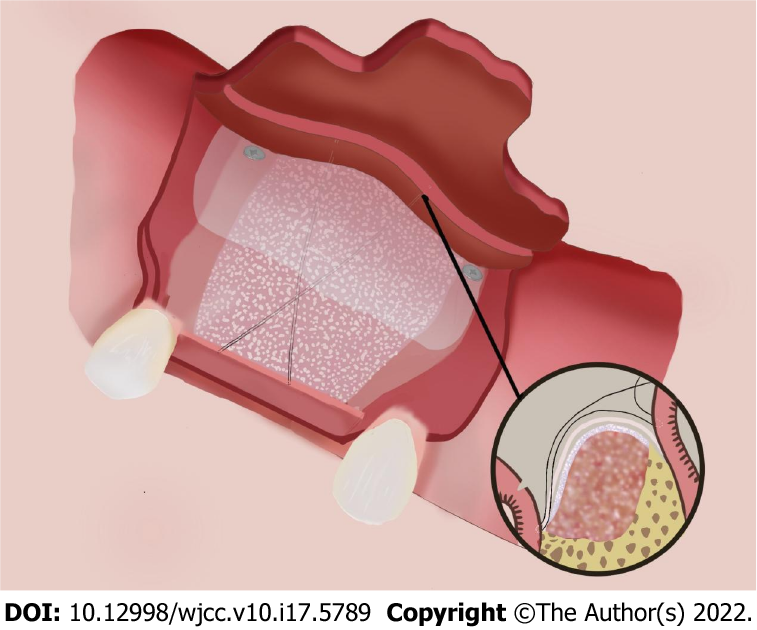
Recipient site preparation: after disinfection and local anesthesia, a mid-crestal incision along with an intrasulcus incision of the adjacent tooth were performed, extending into the distal of teeth 11 and 15, with two divergent vertical incisions made one tooth away from teeth 11 and 15 and a full-thickness flap was reflected. Decortication holes were prepared on the surface of the recipient region (Figure 3A). The mixed particle bone graft was adapted to the recipient sites, with the width more than 10 mm, then entirely covered by bilayer absorbable collagen membrane (Bio-Gide, Geistlich, Switzerland) (Figure 3B). Four titanium pins (Trausim, China) were used to fix the four marginal angles of the collagen membrane; two of which were located on the buccal side and two on the palatal side, avoiding the anatomical structures such as root and maxillary sinus. A periosteal release incision was made 2-3 mm beneath the planned apical position of the graft material and membrane. Incremental incisions of 1 to 3 mm into the periosteum and submucosa were made perpendicular to the base of the inner surface of the flap[21]. The flap on the palatal side was partially reflected and the buccal flap advancement was evaluated to determine if deeper incisions into the submucosa were needed to attain more advancement to make sure the soft tissue could be closed without any tension (Figure 3C)[22]. A 6-0 absorbable suture (Coated VICRYL, Ethicon, United States) was used to fix the absorbable membranes and bone graft material using PDMS (Figure 3D).
PDMS and titanium pins fixation technique: after accurate placement of the four titanium pins, the suture needle was introduced through the palatine mucosa at a point one third distal to the mesial corner pin at the palatal site. The needle was carried over the membrane and stitched through the periosteum 2-3 mm apical to the periosteal release incision at a point one third mesial to the distal buccal pin. The needle was looped back at the exterior surface of the grafts and passed through the palatine mucosa, tightening the suture, and then a knot was tied at the exterior of the palatine mucosa to stabilize the suture. The same procedure was repeated at a point one third mesial to the distal corner pin at the palatal site to a point one third distal to the mesial buccal corner pin and then knotted. The two sutures formed a figure of eight cross at the midpoint of the graft material on the buccal side (Figure 4). After tightening the suture, we checked if the bone graft and the membrane were completely immobilized and positioned correctly. Two PDMS prevented potential movement and migration of the bone graft and membranes. Finally, the mucoperiosteal flap was released to ensure a tension-free closure and the flaps were sutured by two layers, combining horizontal mattress sutures with single interrupted sutures. Vertical incisions were closed using single interrupted sutures, which were removed 7 d after surgery, while the mattress suture remained in place until 2 wk. The patient was instructed to use antibiotics and 0.2% chlorhexidine mouth rinse twice a day for 7 d to prevent infection. Two implants (Ankylos A11; Friadent, Germany) were placed after 10 mo’s healing without any bone augmentation surgery, and the final prostheses were finished at 3 mo after implant placement.
The cross-sections of the grafted area were measured to evaluate the width of the reconstructed alveolar ridge. CBCT imaging was performed preoperatively, immediately after bone augmentation surgery, and before and after implant placement. The CBCT images were superimposed before bone grafting and after implantation using a software system (3Shape, Denmark); the yellow line represented the alveolar ridge before bone grafting. The result showed that an average augmentation of approximately 10 mm in the alveolar ridge width was achieved at the surgical site after 10 mo’ of healing. Two sites were selected to analyze the volume of bone augmentation, 5 and 10 mm below the alveolar crest. Significant bone width increment was achieved by this modified GBR technique. CBCT images showed that at the tooth 12 site, the bone width was increased from 1.83 to 8.83 mm at a point 5 mm below the crest, and from 1.70 to 9.47 mm at a point 10 mm below the crest (Figure 5A). At the tooth 14 site, the bone width was increased from 0.72 to 9.23 mm and from 4.22 to 11.55 mm at points 5 and 10 mm below the crest, respectively (Figure 5B).
Various techniques and materials have been used for bone augmentation procedures. It is difficult to choose GBR or Onlay bone blocks in cases of continuous severe horizontal alveolar bone defects. In this case, the remaining alveolar ridge width was < 2 mm at most sites and it seemed that onlay bone graft was the first choice for horizontal bone augmentation according to the decision tree of horizontal bone augmentation[5]. Moreover, bone block is reported to be more effective than GBR in maintaining the volume at the initial stages of healing, and GBR experiences more changes compared with block grafts[2]. However, in the present case, it was difficult to use bone blocks. Firstly, the residual bone of most sites was only 1 mm or less and it was too thin to be used for retention and stabilization of the graft bone bock by titanium screws. Secondly, it was difficult to obtain bone blocks of sufficient size and thickness in the mandibular intercanine region and the external oblique line due to the large area of bone defect, and the patient refused additional surgery outside the oral cavity, such as the fibula or the ilium, and he refused to use any allogenic bone. Finally, GBR might have been a good alternative choice, and an average of approximately 10 mm horizontal bone was gained by GBR to fix the absorbable collagen membranes and particulate grafts with PDMS and four corner pins after 10 mo of healing.
Bone augmentation surgery was performed 3 wk after tooth extraction and the soft tissue was healing at that time. More recently, clinicians have preferred to use non-form-stable collagen membranes to reconstruct severely thin ridges instead of titanium mesh or Poly Tetra Fluoro Ethylene membrane which is a more sensitive technique, with poor angiogenesis, higher rate of soft tissue dehiscence and difficulty in secondary removal[10,23]. Moreover, significant scar tissue was found in the area of the bone defect and the soft tissue was a thin gingival biological type, therefore absorbable collagen membrane was selected for GBR.
For severe horizontal bone defect, the key factor for successful GBR is to fix the graft material and membranes at the desired position, reduce the movement, and maintain the spatial shape[24]. The stability of the bone substitute and collagen membrane can be enhanced by the application of fixation pins or by the use of block bone substitute instead of particulate bone substitute[25]. The sausage technique using a membrane fixed with titanium pins to stabilize the particle grafts has been reported[18]; however, several potential risks have been documented such as damage to the adjacent roots and underlying anatomical vital structures, and the need for an extensive reopening procedure to retrieve the nonabsorbable pins[20]. The PVMS technique may be preferable to fix the absorbable collagen membrane and particulate graft materials for single implant sites. However, a limitation to this technique is the tensile strength of the absorbable suture material, and possible migration of the particulate graft material in an apicocoronal direction[13], it is only possible to fix the membrane by means of a linear-guided suture, resulting in possible migration of the particulate graft material in an apicocoronal direction. Thus, for continuous severe horizontal bone defect, the use of pins is still recommended because PVMS may not provide sufficient graft stabilization. So far, the relationship between the new bone regeneration and the various fixation methods used is still unknown, and future research is needed to establish the optimal fixation method for adequate bone regeneration[26].
In the present case, the stability of the graft and membrane seemed unable to be provided only by the PDMS technique, thus, the use of four corner pins was still mandatory. Firstly, the four corner pins can limit the possible movement of the membrane and the particulate graft material in the apicocoronal direction. Secondly, the four corner pins might compensate the gradually decreasing strength of the suture due to degradation and absorption. According to the manufacturer, the tensile strength of the VICRYL suture is approximately 75% of its original strength after 14 d and approximately 25% after 28 d in vivo. All of the original tensile strength is lost by 5 wk after implantation. Absorption of the suture is essentially complete between 56 and 70 d. In contrast, the Bio-Gide membrane showed obvious tissue integration at 2 wk postimplantation, and almost complete degradation at week 4[27]. Membrane thickness decreased significantly at week 4, and at week 12, the Bio-Gide was almost absorbed and there was a significant increase in mean bone formation[28]. However, it should be kept in mind that the membrane absorption time might not be the most important, and angiogenesis of the membrane plays a crucial role in GBR[29]. The prolonged biodegradation of the membranes might be associated with decreased tissue integration, vascularization and foreign body reactions[27]. The stability of the graft and membrane, as well as vascularization of the membrane, are crucial to the success of GBR, especially in the early stage of bone regeneration. So far there is no evidence for the time required for membrane fixation, and whether the biodegradation period of the absorbable suture material affects the result of GBR is still unknown.
Titanium pins and sutures can be combined effectively and flexibly. Compared with the sausage technique using pins only, multiple pins are required, which is costly, and it is difficult to operate the pins on the lingual or palatal side, and sometimes it is also difficult to avoid hazardous sites and damage to adjacent roots during insertion. Reducing the number of titanium pins can reduce the risk of complications and the difficulty of surgery. This combined technique is flexible and is very useful in clinical practice.
For continuous severe horizontal bone defect, PDMS combined with four corner pins may provide an alternative to traditional methods to obtain better bone regeneration, and is a feasible technique to maintain the space and stabilize the graft and membranes in severe horizontal bone defect. Nevertheless, well-designed future clinical studies are needed to verify that the technique described here generates comparable and reproducible results.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Zhejiang Stomatological Association, vice-chairman; Chinese Stomatological Association, Standing Committee member.
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Agrawal AA, India; Oji C, Nigeria; Rakhshan V, Iran S-Editor: Wu YXJ L-Editor: A P-Editor: Wu YXJ
| 1. | Benic GI, Hämmerle CH. Horizontal bone augmentation by means of guided bone regeneration. Periodontol 2000. 2014;66:13-40. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 205] [Cited by in F6Publishing: 214] [Article Influence: 21.4] [Reference Citation Analysis (0)] |
| 2. | Elnayef B, Porta C, Suárez-López Del Amo F, Mordini L, Gargallo-Albiol J, Hernández-Alfaro F. The Fate of Lateral Ridge Augmentation: A Systematic Review and Meta-Analysis. Int J Oral Maxillofac Implants. 2018;33:622-635. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 56] [Article Influence: 9.3] [Reference Citation Analysis (1)] |
| 3. | Chiapasco M, Casentini P. Horizontal bone-augmentation procedures in implant dentistry: prosthetically guided regeneration. Periodontol 2000. 2018;77:213-240. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 46] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 4. | Aghaloo TL, Moy PK. Which hard tissue augmentation techniques are the most successful in furnishing bony support for implant placement? Int J Oral Maxillofac Implants. 2007;22 Suppl:49-70. [PubMed] [Cited in This Article: ] |
| 5. | Fu JH, Wang HL. Horizontal bone augmentation: the decision tree. Int J Periodontics Restorative Dent. 2011;31:429-436. [PubMed] [Cited in This Article: ] |
| 6. | Lehmijoki M, Holming H, Thorén H, Stoor P. Rehabilitation of the severely atrophied dentoalveolar ridge in the aesthetic region with corticocancellous grafts from the iliac crest and dental implants. Med Oral Patol Oral Cir Bucal. 2016;21:e614-e620. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Scheerlinck LM, Muradin MS, van der Bilt A, Meijer GJ, Koole R, Van Cann EM. Donor site complications in bone grafting: comparison of iliac crest, calvarial, and mandibular ramus bone. Int J Oral Maxillofac Implants. 2013;28:222-227. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 60] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 8. | Sbordone C, Toti P, Guidetti F, Califano L, Santoro A, Sbordone L. Volume changes of iliac crest autogenous bone grafts after vertical and horizontal alveolar ridge augmentation of atrophic maxillas and mandibles: a 6-year computerized tomographic follow-up. J Oral Maxillofac Surg. 2012;70:2559-2565. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 70] [Cited by in F6Publishing: 70] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 9. | Urban IA, Monje A. Guided Bone Regeneration in Alveolar Bone Reconstruction. Oral Maxillofac Surg Clin North Am. 2019;31:331-338. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 10. | Wessing B, Lettner S, Zechner W. Guided Bone Regeneration with Collagen Membranes and Particulate Graft Materials: A Systematic Review and Meta-Analysis. Int J Oral Maxillofac Implants. 2018;33:87-100. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 93] [Cited by in F6Publishing: 134] [Article Influence: 19.1] [Reference Citation Analysis (0)] |
| 11. | Wang HL, Boyapati L. "PASS" principles for predictable bone regeneration. Implant Dent. 2006;15:8-17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 262] [Cited by in F6Publishing: 317] [Article Influence: 17.6] [Reference Citation Analysis (0)] |
| 12. | An YZ, Strauss FJ, Park JY, Shen YQ, Thoma DS, Lee JS. Membrane fixation enhances guided bone regeneration in standardized calvarial defects: A pre-clinical study. J Clin Periodontol. 2022;49:177-187. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 13. | Urban IA, Lozada JL, Wessing B, Suárez-López del Amo F, Wang HL. Vertical Bone Grafting and Periosteal Vertical Mattress Suture for the Fixation of Resorbable Membranes and Stabilization of Particulate Grafts in Horizontal Guided Bone Regeneration to Achieve More Predictable Results: A Technical Report. Int J Periodontics Restorative Dent. 2016;36:153-159. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 14. | Johnson TM, Vargas SM, Wagner JC, Lincicum AR, Stancoven BW, Lancaster DD. The Triangle Suture for Membrane Fixation in Guided Bone Regeneration Procedures: A Report of two Cases. Clin Adv Periodontics. 2022;. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Kamat SM, Khandeparker RV, Akkara F, Dhupar V, Mysore A. SauFRa Technique for the Fixation of Resorbable Membranes in Horizontal Guided Bone Regeneration: A Technical Report. J Oral Implantol. 2020;46:609-613. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Kirsch A, Ackermann KL, Hurzeler MB, Durr W, Hutmacher D. Development and clinical application of titanium minipins for fixation of nonresorbable barrier membranes. Quintessence Int. 1998;29:368-381. [PubMed] [Cited in This Article: ] |
| 17. | Shalev TH, Kurtzman GM, Shalev AH, Johnson DK, Kersten MEM. Continuous Periosteal Strapping Sutures for Stabilization of Osseous Grafts With Resorbable Membranes for Buccal Ridge Augmentation: A Technique Report. J Oral Implantol. 2017;43:283-290. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Wang HL, Misch C, Neiva RF. "Sandwich" bone augmentation technique: rationale and report of pilot cases. Int J Periodontics Restorative Dent. 2004;24:232-245. [PubMed] [Cited in This Article: ] |
| 19. | Siar CH, Toh CG, Romanos G, Ng KH. Subcutaneous reactions and degradation characteristics of collagenous and noncollagenous membranes in a macaque model. Clin Oral Implants Res. 2011;22:113-120. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Lorenzoni M, Pertl C, Polansky RA, Jakse N, Wegscheider WA. Evaluation of implants placed with barrier membranes. A restrospective follow-up study up to five years. Clin Oral Implants Res. 2002;13:274-280. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 41] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Zazou N, Diab N, Bahaa S, El Arab AE, Aziz OA, El Nahass H. Clinical comparison of different flap advancement techniques to periosteal releasing incision in guided bone regeneration: A randomized controlled trial. Clin Implant Dent Relat Res. 2021;23:107-116. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Romanos GE. Periosteal releasing incision for successful coverage of augmented sites. A technical note. J Oral Implantol. 2010;36:25-30. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 23. | Atef M, Tarek A, Shaheen M, Alarawi RM, Askar N. Horizontal ridge augmentation using native collagen membrane vs titanium mesh in atrophic maxillary ridges: Randomized clinical trial. Clin Implant Dent Relat Res. 2020;22:156-166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 24. | Carpio L, Loza J, Lynch S, Genco R. Guided bone regeneration around endosseous implants with anorganic bovine bone mineral. A randomized controlled trial comparing bioabsorbable versus non-resorbable barriers. J Periodontol. 2000;71:1743-1749. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 91] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 25. | Mir-Mari J, Wui H, Jung RE, Hämmerle CH, Benic GI. Influence of blinded wound closure on the volume stability of different GBR materials: an in vitro cone-beam computed tomographic examination. Clin Oral Implants Res. 2016;27:258-265. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 69] [Cited by in F6Publishing: 72] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 26. | Cucchi A, Chierico A, Fontana F, Mazzocco F, Cinquegrana C, Belleggia F, Rossetti P, Soardi CM, Todisco M, Luongo R, Signorini L, Ronda M, Pistilli R. Statements and Recommendations for Guided Bone Regeneration: Consensus Report of the Guided Bone Regeneration Symposium Held in Bologna, October 15 to 16, 2016. Implant Dent. 2019;28:388-399. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 27. | Rothamel D, Schwarz F, Sager M, Herten M, Sculean A, Becker J. Biodegradation of differently cross-linked collagen membranes: an experimental study in the rat. Clin Oral Implants Res. 2005;16:369-378. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 224] [Cited by in F6Publishing: 238] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 28. | Hämmerle CH, Jung RE, Yaman D, Lang NP. Ridge augmentation by applying bioresorbable membranes and deproteinized bovine bone mineral: a report of twelve consecutive cases. Clin Oral Implants Res. 2008;19:19-25. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 56] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 29. | Schwarz F, Rothamel D, Herten M, Wüstefeld M, Sager M, Ferrari D, Becker J. Immunohistochemical characterization of guided bone regeneration at a dehiscence-type defect using different barrier membranes: an experimental study in dogs. Clin Oral Implants Res. 2008;19:402-415. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 98] [Cited by in F6Publishing: 102] [Article Influence: 6.4] [Reference Citation Analysis (0)] |