Copyright
©The Author(s) 2023.
World J Clin Cases. Mar 26, 2023; 11(9): 2029-2035
Published online Mar 26, 2023. doi: 10.12998/wjcc.v11.i9.2029
Published online Mar 26, 2023. doi: 10.12998/wjcc.v11.i9.2029
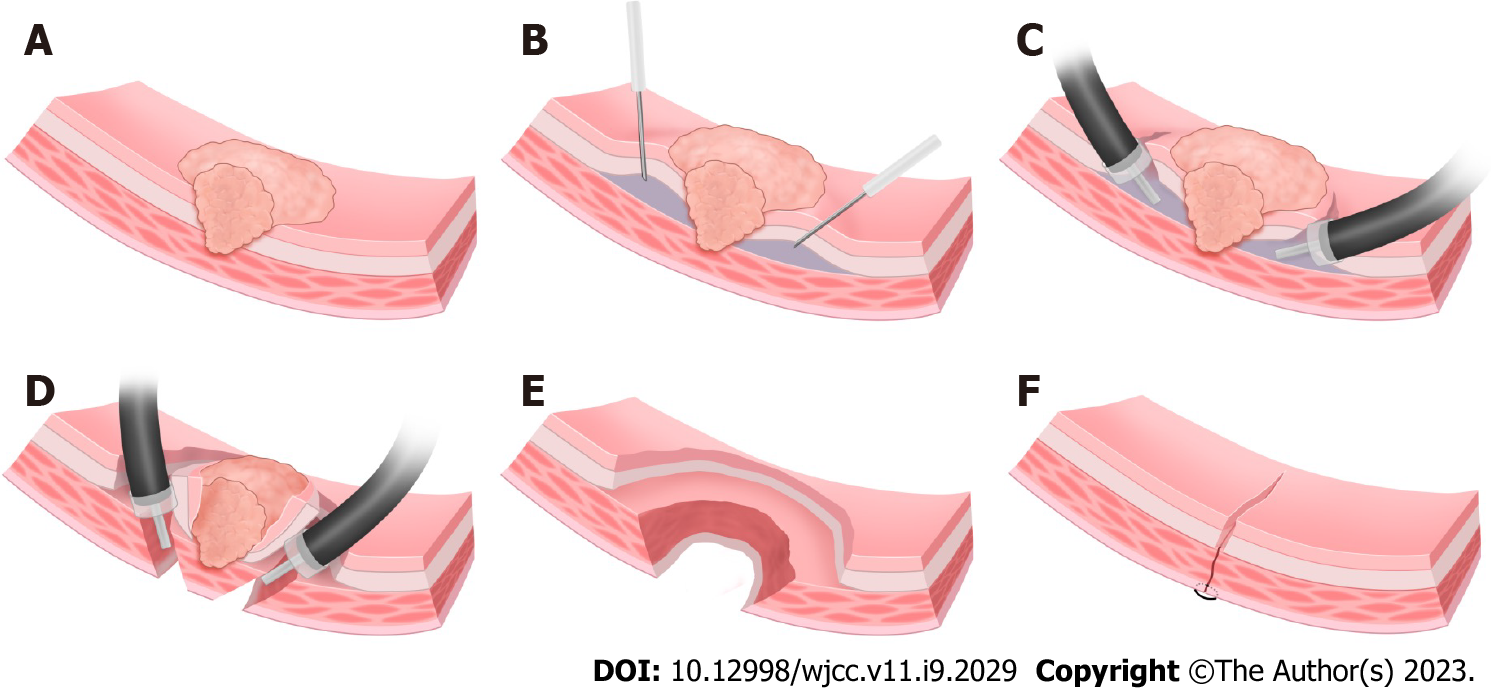
Figure 1 Endoscopic submucosal dissection and full-thickness resection.
A: T2 gastric cancer lesion; B: Submucosal injection on the lateral side of the lesion; C: Endoscopic submucosal dissection; D: The circumferential full-thickness resection is performed at 0.5-1.0 cm lateral to the deep infiltration, and the resected lesion is removed; E: Gastric wall wound after endoscopic submucosal dissection and full-thickness resection. The serosal defect is smaller than the mucosal defect; F: The gastric wall wound is sutured by endoscope or laparoscope.
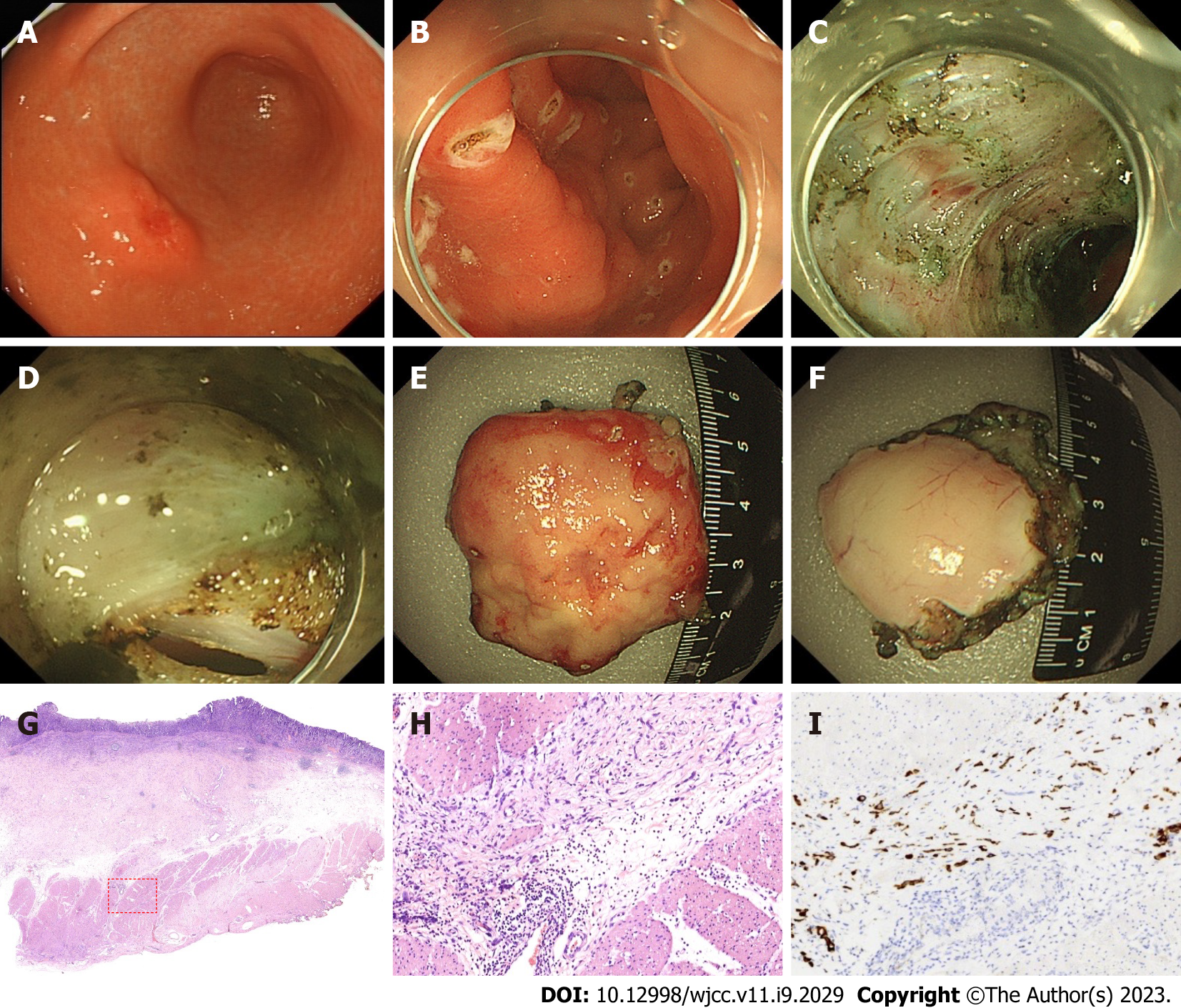
Figure 2 Case 1, minimally invasive endoscopic resection of T2 gastric cancer (endoscopic submucosal dissection and full-thickness resection) and pathology.
A and B: Protuberant lesion on the greater curvature of the anterior wall of the gastric antrum, about 2.0 cm × 2.0 cm. The resection area was marked 1.5 cm outside the edge of the lesion, then endoscopic submucosal dissection (ESD) was performed along the outside of the marked point; C and D: ESD circumferentially peeled to the submucosa, which was thinned and unclear, indicating that the lesion was deeply infiltrated (SM3 or T2). At 0.5-1.0 cm outside the unclear portion of submucosa, the lesion was resected by ESD and full-thickness resection; E: Mucosal surface of resected lesion (3.2 cm × 3.5 cm); F: The serosa of the resected lesion revealed that the area of the resected mucosa (normal mucosa and the mucosa with shallow infiltration) was significantly larger than that of the serosa (location of deep infiltration); G and H: Poorly differentiated adenocarcinoma, infiltrating into the superficial layer of the muscularis propria (red box); scale bar, 500 μm; I: Immunohistochemical staining of cytokeratin expression at location of poorly differentiated adenocarcinoma.
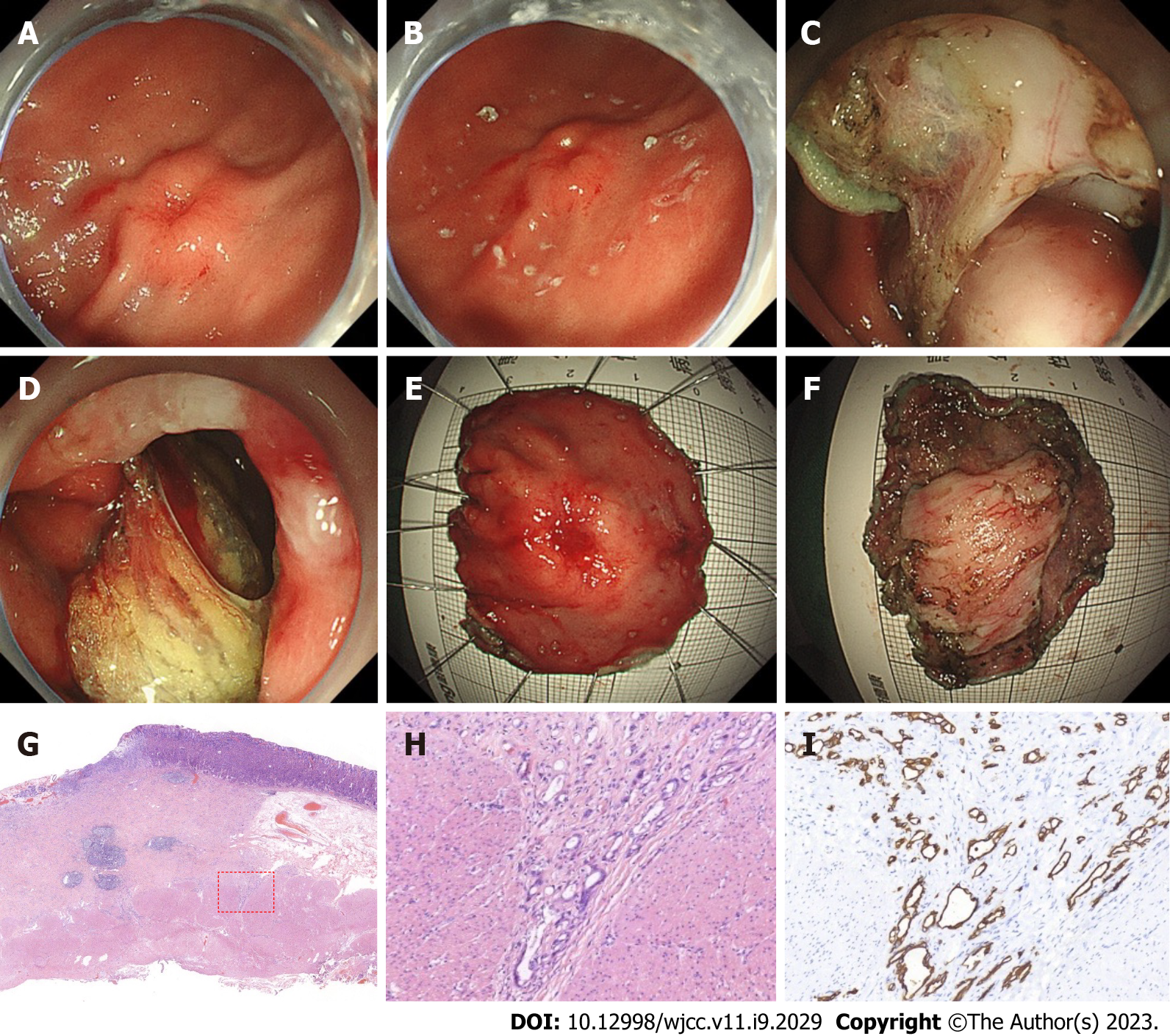
Figure 3 Case 2, minimally invasive endoscopic resection of T2 gastric cancer (endoscopic submucosal dissection and full-thickness resection) and pathology.
A and B: Lesion on the greater curvature of the lower gastric body, central ulcer, marginal eminence, about 2.0 cm × 2.5 cm. The resection area was marked 1.5 cm outside the edge of the lesion, and endoscopic submucosal dissection (ESD) was performed along the outside of the marked point. ESD circumferentially peeled to the submucosa, which was thinned and unclear, indicating that the lesion was deeply infiltrated (SM3 or T2); C and D: At 0.5-1.0 cm outside the unclear portion of submucosa, the lesion was resected by ESD and full-thickness resection; E: Mucosal surface of resected lesion (3.8 cm × 4.0 cm); F: The serosa of the resected lesion showed that the area of the resected mucosa (normal mucosa and the mucosa with shallow infiltration) was significantly larger than that of the serosa (location with deep infiltration); G and H: Poorly differentiated adenocarcinoma, containing signet ring cells, infiltrating into the superficial layer of muscularis propria (red box); scale bar, 500 μm; I: Immunohistochemical staining of cytokeratin expression at location of poorly differentiated adenocarcinoma.
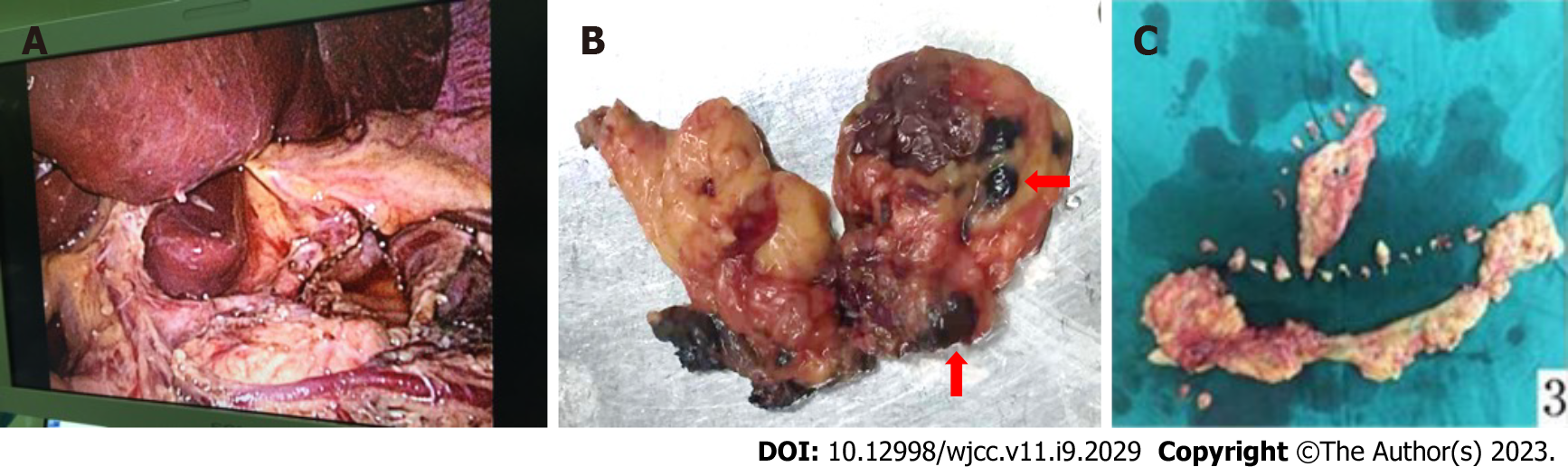
Figure 4 Novel combined endoscopic and laparoscopic surgery.
A: Laparoscopic D2 lymphadenectomy can achieve skeletonization of common hepatic artery, proper hepatic artery and splenic artery; B and C: Dissection of lymph nodes (red arrow) and omentum.
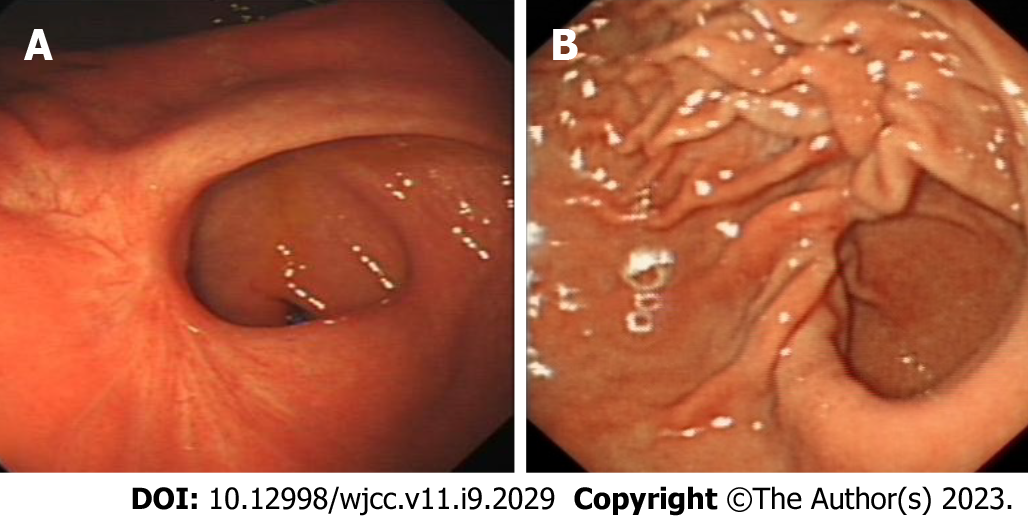
Figure 5 Endoscopy images after endoscopic submucosal dissection and full-thickness resection.
A: Case 1 endoscopy image after endoscopic submucosal dissection and full-thickness resection (ESDFTR); B: Case 2 endoscopy image after ESDFTR.
- Citation: Dai JH, Qian F, Chen L, Xu SL, Feng XF, Wu HB, Chen Y, Peng ZH, Yu PW, Peng GY. Novel combined endoscopic and laparoscopic surgery for advanced T2 gastric cancer: Two case reports. World J Clin Cases 2023; 11(9): 2029-2035
- URL: https://www.wjgnet.com/2307-8960/full/v11/i9/2029.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i9.2029