Copyright
©The Author(s) 2019.
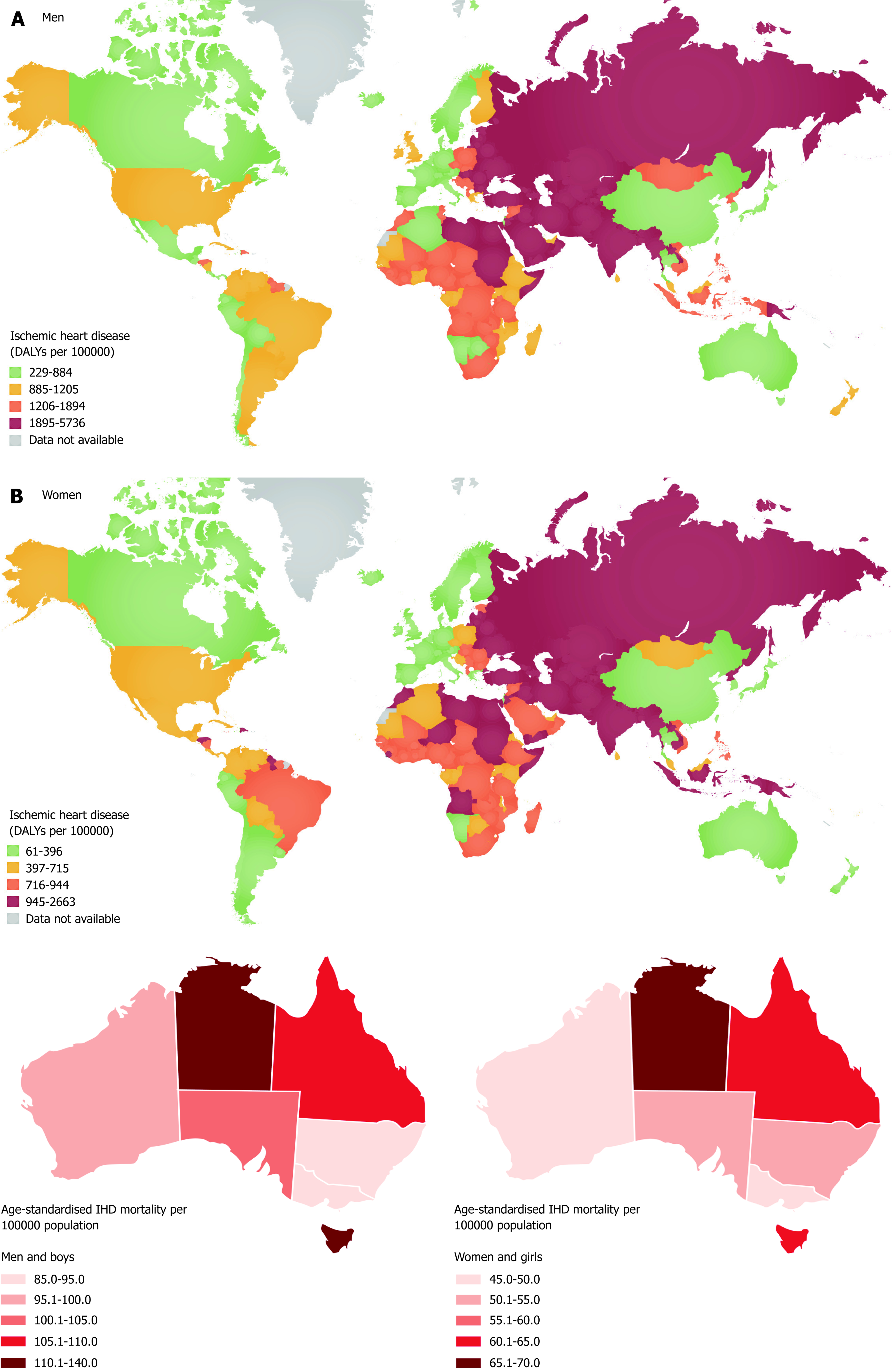
Figure 1 Ethnicity, epidemiological transition and coronary artery disease.
A: The global distribution of CAD deaths. B: Mean national data may underrepresent variations within health system clusters of CAD risk, prevalence and incidences. Within developing nations, traditional and non-traditional factors contribute to risk and may alter baseline risks associated with ethnicity and gender. When such groups’ transition to developed nations such has Australia, excellent mean health care outcomes data could mask greater heterogeneity of outcomes data. These variations in epidemiological transition areas are also seen in some remote and Aboriginal populations. As demographic variations are represented variably within various health clusters this has to be factored in risk stratification. Centralized fixed guidelines and health funding models could thus be suboptimal for optimal health efficacy. (Geographical map from reference 6 and 17).
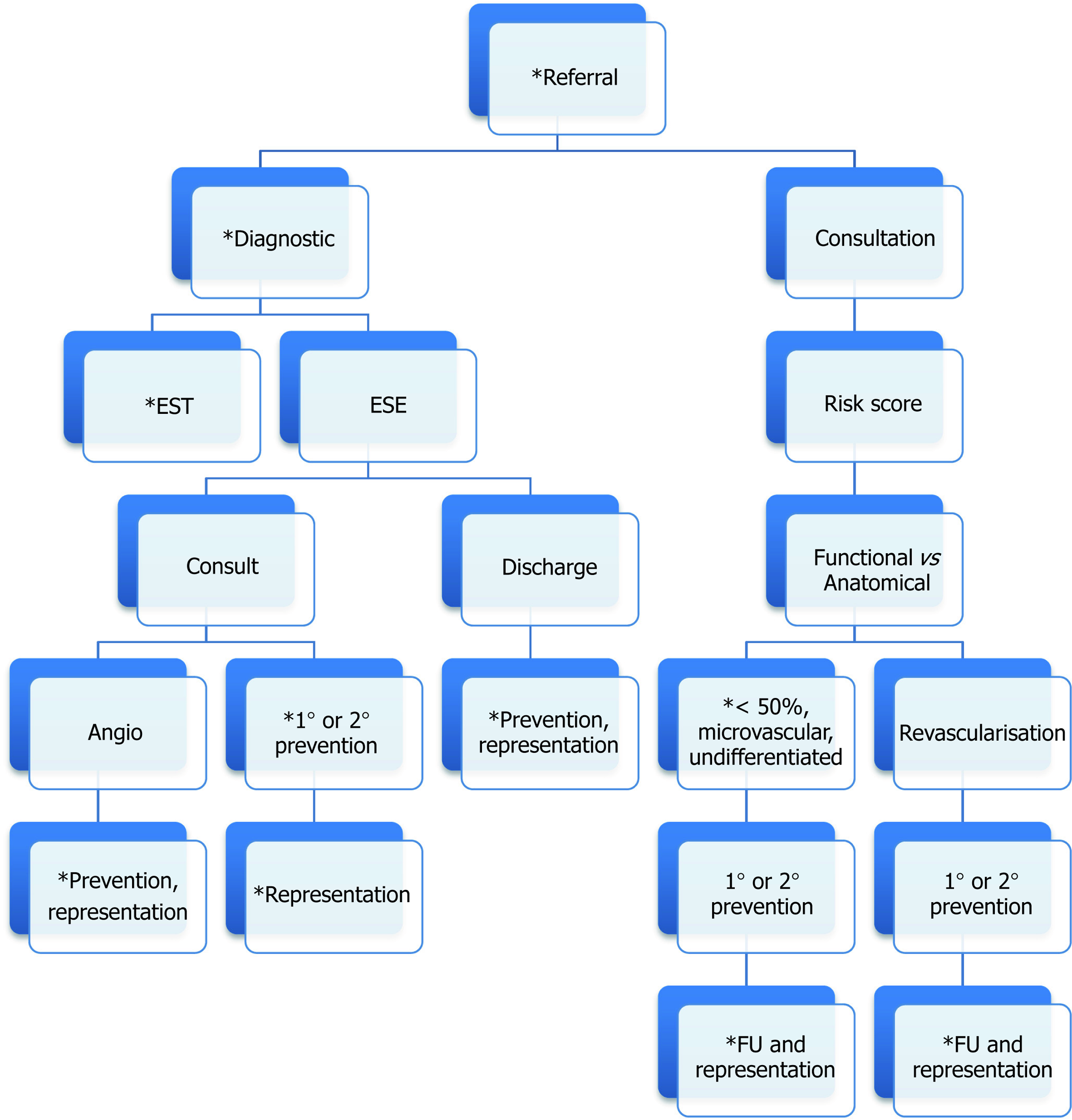
Figure 2 Triage and subsequent evaluation of suspected coronary artery disease referrals.
CAD presentations to specialist are predominately referrals from general practitioners or following triage from emergency departments. Referrers either request a specialized test or a cardiac consultation. The choice between EST and ESE are not always clear. Direct specialist consultation may precipitate a more risk score guided approach. Moving down the pathway following complaints of typical symptom or positive stress test, following ascertaining anatomical information, gaps still exist for future health encounters subsequent from inconsistent classification of CAD burden probable vasospastic angina or undifferentiated cases. Direct diagnostic referrals run the highest risk of duplication for future representations. *Highlights points in the pathways where models of cost-efficacy and risk stratification can be examined further. EST: Exercise stress test; ESE: Exercise stress echocardiography; FU: Follow-up.
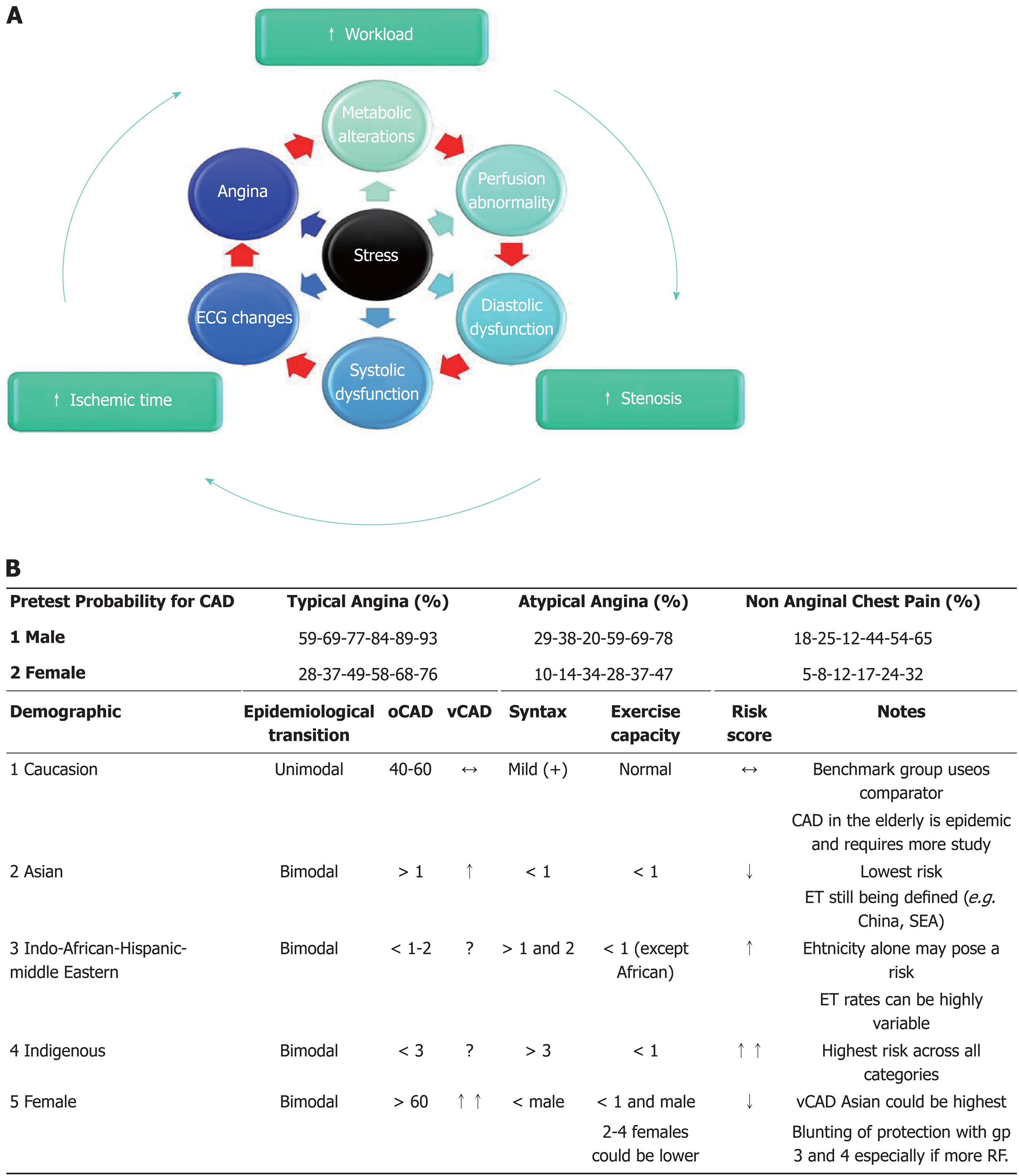
Figure 3 Ischemic Cascade and Constellation in clinical context.
A: Stress creates myocardial energy imbalance leading to any of six manifestations in the ichemic cascade (red arrow) in a forward linear direction. Individual variations and combinations of workload, stenosis severity and ischemia duration (outer green arrows) that inlfuences the order for components in the cascde, creates more reaslistically an ischemic constellation’ of events, where any order for observable events is possilbe (multicolour arrows); B: PTP guides diagnostic workup. The probability is never 0 or 100%. With < 15 and > 85% guiding low or high risk. The actual number are for age range 30-39 years, increasing by decades, to > 80 years. Variations from the mean are determined by demography. No 1-4 represent males. Females across all groups represent the same CAD risk as the males except are relatively protected during middle ages, delaying mean onset of significant CAD. Etiological variations exist in: (1) vasospasm, being more likely in women, especially Asian. The actual rates among other non-caucasion female races are nor well defined; (2) gender protection: from premature CAD in women may also be blunted in higher risk groups 2; (3) ethnicity - Aboriginal populations suffer from the greatest risk and severity of CAD, followed by 3, 1 and 2. Asians have the lowest risks; (4) developmental status - of any group also lowers mean age of onset of any ethnicity. Defining the coronary anatomy early could be one way of risk stratifying subgroups within braod ethnic based categories. oCAD: Obstructive coronary artery disease; ET: Epidemiological transition; PTP: Pre-test probablity; RF: Risk factors; SEA: South East Asia; vCAD: Vasospastic coronary artery disease. (Concepts modified from ref 38, 39, 82-101).
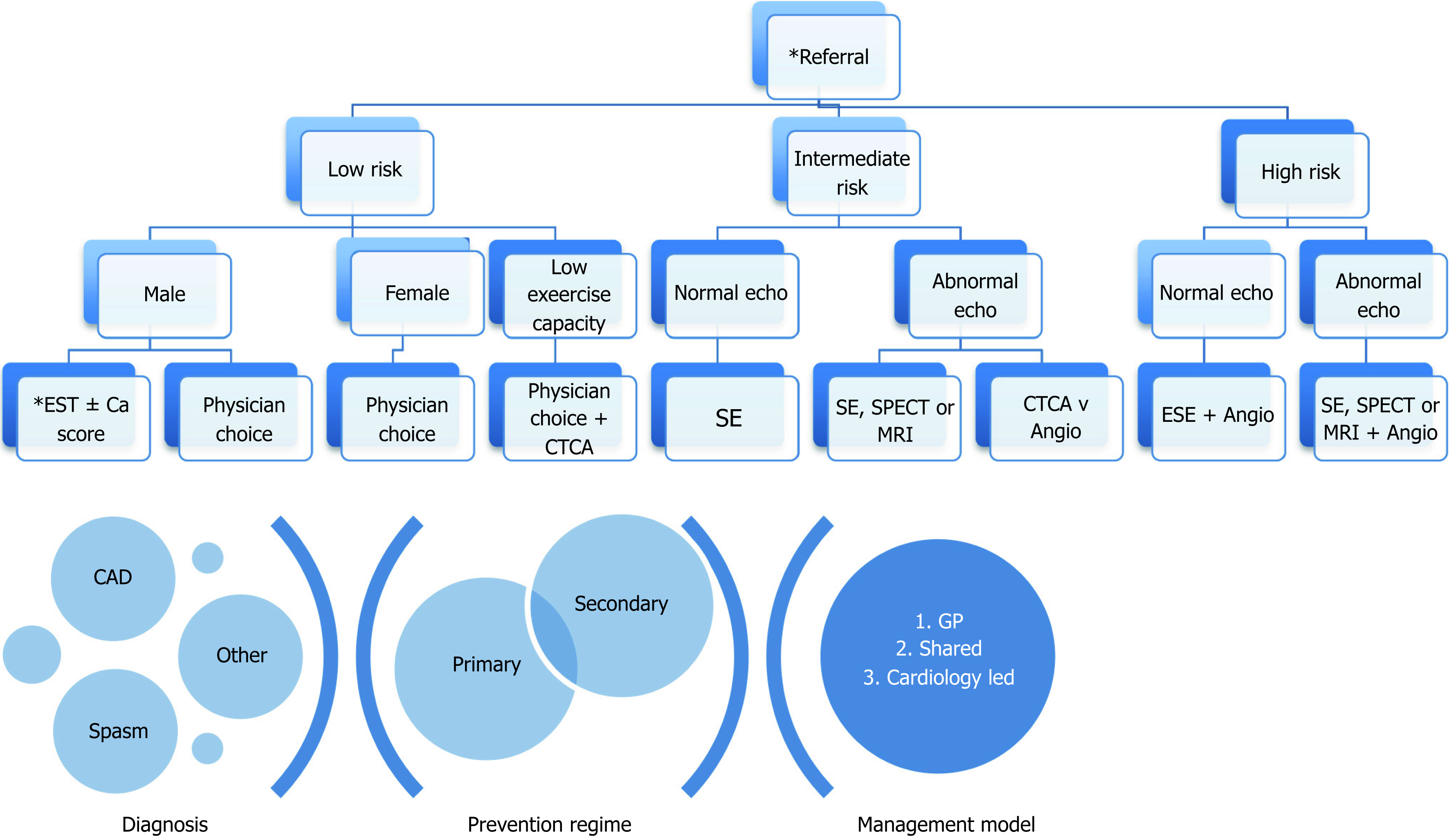
Figure 4 Theoretical Considerations for Future Cost-Efficiency.
Three avenues for cost-efficacy analysis within a health cluster are identified. (1) Referral: the PTP gives a rough guide as to first choice of diagnostic test. High demand for evaluation raises an argument for observational studies for the best point of initial PTP work-up e.g. with GP supported education or early cardiology review; (2) Diagnostics: the combination of patient factors, cost and availability dictates stress echocardiography be the first choice of imaging modality, however more understanding of other modalities should also be encouraged; (3) Clinical Evaluation: this area is most likely to influence lifetime CAD cost-efficiency. Avenues to explore are: (a) patients and primary care preventive education after findings of minor CAD and/or with intermediate and high risk criteria factors; (b) patients at increased risk of recurrent chest pains and readmission e.g. vasospastic angina; (c) risk models for screening and follow-up of various ethnicities and demographies at different stages of epidemiological transition; (d) combinations of primary, specialist and tertiary care management models: the long term patient specific and health system goals once the work-up for CAD is initiated, aside from actual diagnosis of definite CAD, is prevention of disease progression or risk of future disease and preventing cost-ineffective utility of health resources especially unnecessary diagnostics and hospital beds. Physician Choice: includes any combination of investigation based on additional characteristics deemed to alter risk of accuracy of EST. Ca: Calcium; CAD: Coronary artery disease; CTCA: Computerized tomography coronary angiography; ESE/SE: Exercise stress echocardiography; PTP: Pretest probability; SPECT: Single photon emission computerized tomography.
- Citation: Iyngkaran P, Chan W, Liew D, Zamani J, Horowitz JD, Jelinek M, Hare DL, Shaw JA. Risk stratification for coronary artery disease in multi-ethnic populations: Are there broader considerations for cost efficiency? World J Methodol 2019; 9(1): 1-19
- URL: https://www.wjgnet.com/2222-0682/full/v9/i1/1.htm
- DOI: https://dx.doi.org/10.5662/wjm.v9.i1.1