Published online Jan 31, 2019. doi: 10.5528/wjtm.v8.i1.1
Peer-review started: August 6, 2018
First decision: October 10, 2018
Revised: January 9, 2019
Accepted: January 28, 2019
Article in press: January 28, 2019
Published online: January 31, 2019
Processing time: 179 Days and 10.4 Hours
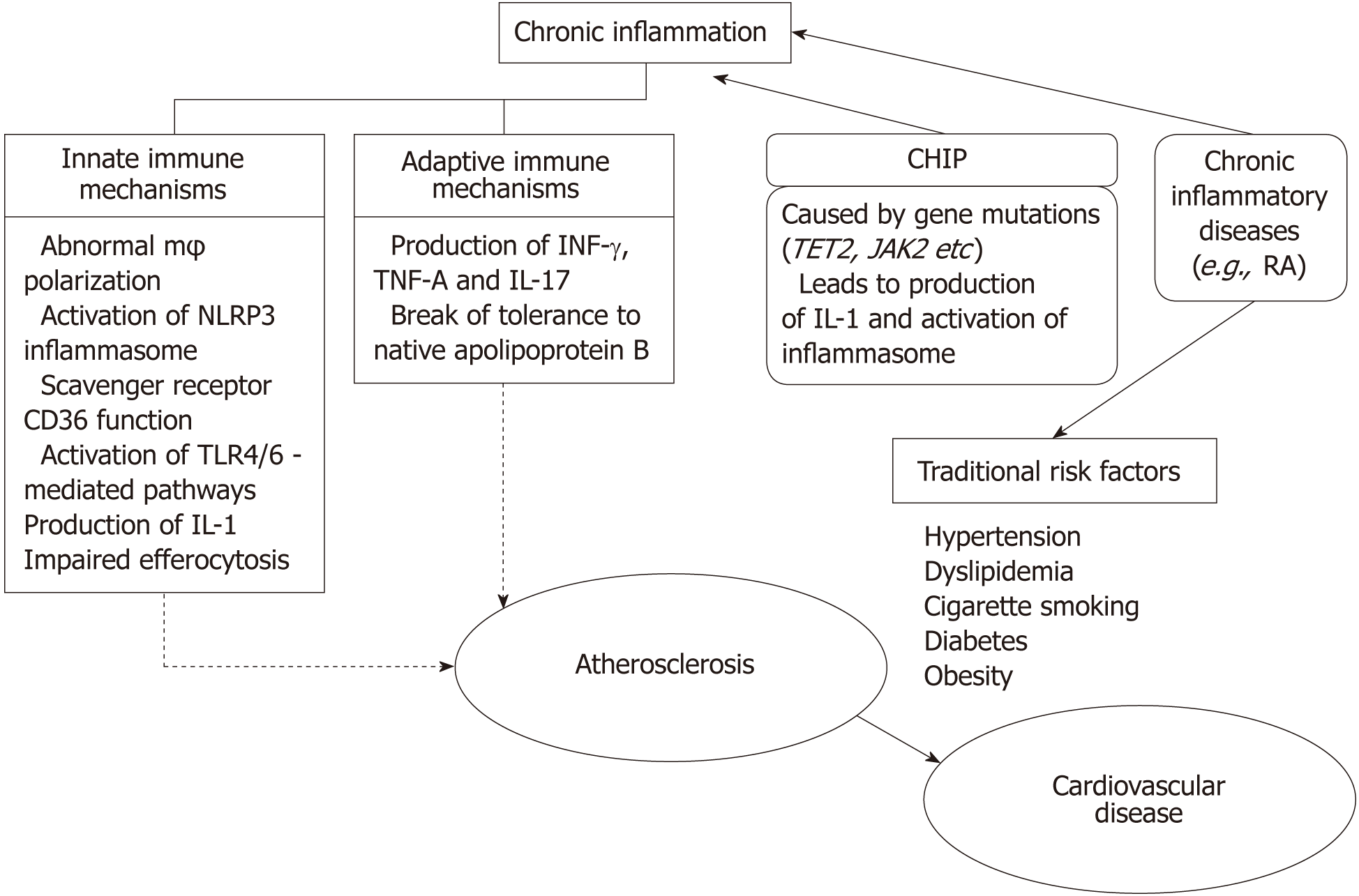
Cardiovascular disease (CVD) has been associated with the so-called traditional risk factors, such as hypertension, hypercholesterolemia and cigarette smoking. Chronic inflammation, exemplified by elevated high sensitivity C-reactive protein, has been added to these risk factors for CVD as non-traditional risk factor. There are two aspects in this association. The first is whether inflammation plays a pathogenic role in traditional risk factors-mediated CVD or it is just an epiphenomenon. The second is whether chronic inflammation caused by an inflammatory disease has any impact on CVD. Accumulated data have shown that inflammation has a central and inciting role in the development of atherosclerosis leading to increased CVD risk. How inflammation contributes to CVD is a topic of continuous research where mechanisms involving both innate and adaptive immune pathways are involved. Endothelial dysfunction, oxidative stress in vascular endothelial cells, macrophage accumulation, formation of inflammasome, production of tumor necrosis factor (TNF)-a, IL-1 and IL-6 characterize the inflammatory process leading to atherogenesis. Recently clonal hematopoiesis of indeterminate potential represents a surprising and novel mechanism underlying atherogenesis. Data from chronic rheumatic inflammatory diseases exemplify the complexity of mechanisms leading to increased CVD, while they also provide evidence that anti-inflammatory biologic drugs, such as anti-TNF and anti-IL6 agents, could control atherogenesis and ameliorate CVD risk. Recent groundbreaking work using biologic anti-IL-1b therapy to treat men and women who have had a prior heart attack provides the best proof of the pathogenic contribution of inflammation in the development of CVD.
Core tip: The association of inflammation with cardiovascular disease (CVD) has two aspects. The first is whether inflammation plays a pathogenic role in traditional risk factors-mediated CVD or it is just an epiphenomenon. The second is whether chronic inflammation caused by an inflammatory disease has any impact on CVD. Chronic inflammation exemplified by elevated high sensitivity C-reactive protein has been added for risk factors for CVD. How inflammation contributes to CVD is a topic of continuous research. A trial showing that anti-IL1b monoclonal-antibody reduced cardiovascular events is the best proof of the pathogenic contribution of inflammation in atherosclerosis and CVD.
- Citation: Katsiari CG, Bogdanos DP, Sakkas LI. Inflammation and cardiovascular disease. World J Transl Med 2019; 8(1): 1-8
- URL: https://www.wjgnet.com/2220-6132/full/v8/i1/1.htm
- DOI: https://dx.doi.org/10.5528/wjtm.v8.i1.1
Cardiovascular diseases (CVD) encompass several entities such as coronary artery disease, cerebrovascular events, peripheral arterial disease, renal artery stenosis and aortic aneurysm. CVD are globally the leading cause of death[1]. Coronary artery disease and stroke are the cause of 80% of CVD deaths in males and 75% in females[1]. One major event underlying the development of a CVD is the presence of atheromatosis where cholesterol is indisputably recognized as an environmental and genetic driver of the disease[2]. In contrast however to the notion that atherosclerosis represents a consequence of lipid accumulation as an ageing and degenerative process, the concept of inflammation is now in the center of current research addressing questions regarding which inflammatory mechanisms are involved as well as ways to intervene therapeutically[3].
Inflammation as an important factor in atherogenesis seemed to be a rather new concept when few years ago intense research interest appeared in the literature. If we search PubMed using both “inflammation” and “atherosclerosis” as key words, we can see an expediential increase of the number of articles on the subject: from around 80 articles found over an entire 20-years period between 1970 and 1990 to more than 12000 new publications since 2010. However, work by researchers and scholars have taught us that “arteriosclerosis”, inflammation and their in-between link had emerged over 200 years ago, as a long standing scientific discussion that actually evolved in active debate with legendary physician Rudolph Virchow as a strong advocate in favor of the significant role of the inflammatory process[4]. Considering the almost complete absence of any discussion during the 20th century, it is incredible to realize that the argument around the topic had begun long before Virchow himself. Lobstein[5,6] is credited as the first to use the term arteriosclerosis. Lobstein[5,6] having observed inflammation in the internal layer of the aorta, attributed an earlier recognition of this disease to Aretaeus of Cappadocia, a Greek physician from the 1st century, although “it had been all forgotten over the last 18 centuries”. Undoubtedly, a connection between inflammation and atherosclerosis was explicitly made in the beginning of the 19th century as we can read in the writings of the English physician Joseph Hodgson: “…Thus the coats of arteries inflame and pass all the stages of adhesion, suppuration, or gangrene, in the same manner as the skin, a gland or a muscle”[7].
During the last decades, the emergence of new imaging methods to assess sub-clinical atherosclerosis in epidemiologic and clinical studies[8-10], combined with advances in molecular biology, prompted the re-emergence of the original theories of atherogenesis and a renewed interest in the putative role of inflammation.
Atherosclerosis begins with the accumulation of LDL in the subendothelial space of the vessel wall in places where endothelium displays abnormal permeability. A recently recognized mechanism enabling active transportation of LDL through the endothelial cells involve activin receptor-like kinase 1 (Alk-1)[11] and scavenger receptor class B type I (SR-BI)[12]. Accumulated LDL can form bulky complexes and undergo protein modification through the action of lipoxygenases, myeloperoxidases and reactive oxygen species, which induces immune cell mediated phagocytosis[13] initially by tissue macrophages and dendritic cells residing inside the arterial intima[14]. Interestingly, it has been recently shown that before the development of atherosclerosis, circulating non-classical monocytes engulf oxidized LDL via scavenger receptor CD36 in an effort to protect the vasculature[15]. Bone marrow derived monocytes on the other hand infiltrate the vascular wall where they differentiate to macrophages, which in turn uptake modified LDL. The formation of lipid droplets inside macrophages through the esterification of cholesterol results in the characteristic foam-like appearance of these cells. Although foamy macrophages were initially considered as the waste bin of lipids, it is now clear that they actively participate in the pathogenesis of atherosclerosis through several inflammatory interactions[16,17]. It has been shown that the modification of cholesterol inside macrophages activates scavenger receptor CD36, which in turn trigger an array of immune responses downstream Toll-like-receptor (TLR) 4 and 6[18]. At the same time our understanding of the molecular mechanisms underlying the inflammatory process in atherogenesis was broadened when it was shown that cholesterol crystals inside macrophages, activates caspase-1-activating NACHT, LRR and PYD domains-containing protein 3 (or cryopyrin) (NLRP3) inflammasome leading to the production and secretion of IL-1 and IL-18[19]. Of note, detailed study using confocal reflection microscopy revealed the presence of cholesterol crystals in the atheromatic plaques inside macrophages as well as in the extracellular spaces found during the very early stages of atheromatosis, pointing towards the fact that the formation of cholesterol crystals drives inflammation rather than follows it[19]. Moreover, it was later shown that activation of NLRP3 inflammasome is orchestrated by the function of scavenger receptor CD36, where macrophages lacking this receptor were unable to stimulate the production of IL-1[20].
Along with the autoinflammatory nature of atherosclerosis exemplified by abnormal macrophage polarization[17], activation of TLRs-mediated pathways and aberrant inflammasome activation and IL-1 production, adaptive immune responses have also a role in the regulation of atherogenesis. Pro-inflammatory T cell subsets (Th1 and Th17) facilitate the progression of atheromatosis through the secretion of interferon-γ, tumor necrosis factor (TNF) and IL-17. On the other hand T regulatory cells (Tregs) have a protective effect through cytokines such as IL-10 and TGFb[21,22]. Recently, an interesting hypothesis has been proposed placing atheromatosis inside the broad spectrum of “autoimmune diseases”. In particular, although modified oxidized LDL is usually suggested as the responsible antigen provoking T cell polyclonal activation, several data derived from animal studies support the idea that a break of tolerance to native, unaltered apolipoprotein B may represent the trigger for lymphocyte abnormal responses[22].
Destabilization of the atheromatic plaque constitutes a critical step regarding the risk of acute cardiovascular events[23]. Although a lot is to be learned about the mechanisms underlying the transformation of an atheromatic plaque from stable to unstable, the development of the necrotic core represents a key event. The necrotic core is created from dead macrophages within the plaque which were not cleared[24]. During the early stages of plaque formation, macrophage apoptosis represents a protective mechanism leading to reduced cellularity and cholesterol burden within the lesion assuming that efferocytosis (phagocytosis of the dead cells) is intact. In case efferocytosis is impaired or overwhelmed, apoptotic debris starts to accumulate, which can lead to secondary necrosis[25]. Impaired efferocytosis appear to stem from different abnormalities including aberrant expression of CD47, which leads to reduced recognition of apoptotic cells, as well as impaired expression of crucial surface receptors such as MerTK[26]. Impaired efferocytosis will lead to secondary necrosis. In situ necrotic material is furthermore added through necroptosis of macrophages. Necroptosis which represents a programmed form of inflammatory cell death is thought to be driven by unrelenting cell exposure to lipoproteins and mediated by mixed lineage kinase domain-like pseudokinase (MLKL) and receptor-interacting serine/threonine-protein kinases (RIPK)[27,28].
Analogous to monoclonal gammopathy of undetermined significance, representing a potential precursor of multiple myeloma, clonal hematopoiesis of indeterminate potential (CHIP) has been recently described as a condition subsequent to somatic mutations within bone marrow cells that could lead to hematologic neoplasia[29]. Apart from increased risk for developing hematologic cancer, the presence of CHIP has been recently and surprisingly associated with increased risk of CVD: risk of myocardial infarction and stroke increased by 2 fold and risk of premature atherosclerosis in patients younger than 50 years old increased by 4-fold compared to control subjects without CHIP[30]. Mutations in each of TET2, DNMT3A, ASXL1, and JAK2 genes were found to be associated with CVD. The effect and underlying mechanisms of TET2 mutations, which represent one of the most frequently mutated genes linked to CHIP, was further tested in a murine model of atherosclerosis. It was found that loss of Tet2 function accelerated athrerosclerosis while in parallel increased macrophage responses to native LDL, including release of inflammatory chemokines, production of IL-1b and activation of inflammasome[30,31].
The link between increased cardiovascular risk and continuous mild elevation of C-reactive protein (CRP), as a marker of persistent low grade systemic inflammation, was initially described in the general population[32-34]. Rheumatoid arthritis (RA), the prototype systemic inflammatory joint disease, characterized by high levels of CRP and other inflammatory cytokines, leads to increased mortality mainly due to CVD[35]. In fact, RA has been recently recognized as an independent risk factor for CVD, analogous to diabetes mellitus[36,37]. Cytokines such as TNF-a and IL-6 have central role in the pathophysiology of RA. The direct impact of such cytokines on human arterial endothelial cells (HAECs) greatly supports their role in atherogenesis. In particular, TNF-a induced upregulation of scavenger receptors (SR) LOX-1 and SR-A[38] in HAECs and THP-1/macrophages cell line[39]. IL-6 also induced upregulation of SR-A in HAECs and macrophage while both TNF-a and IL-6 led to the accumulation of oxidized LDL in THP-1/macrophages transforming them to foam cells[38,39]. Thus, the contribution of systemic inflammation to the increased CVD risk in patients with RA appears to be true but the exact impact in addition to traditional risk factors is still under investigation, where RA-related complications can furthermore act as confounding factors. For instance, in consequence of inflamed joints and increased disease burden, patients with RA display decreased activity, are subjected to increased steroid exposure and are characterized by sarcopenic obesity where loss of muscle mass is combined with increased abdominal fat[40,41]. All these factors could also have an impact to CVD risk. It should be also added that CVD risk in patients with RA, apart from increased atherosclerosis, is also related to non-ischaemic heart disease stemming from conditions such as myocarditis, left ventricular diastolic dysfunction and pulmonary hypertension[42,43].
Patients with other chronic rheumatic diseases were also found to have increased CVD risk, namely systemic lupus erythematosus, ankylosing spondylitis and psoriatic arthritis[44-46]. TNF-a and recently IL-17 have been recognized as significant mediators in the pathogenesis of spondylarthropathies. It was shown that IL-17 and particularly in combination with TNF-a promote pro-inflammatory, pro-coagulant and pro-thrombotic effects in blood vessels. For instance, in primary endothelial cells, IL-17 up-regulated 248 pro-inflammatory gens, and when combined with TNF-a this number increased to 9803[47]. In addition, IL-17 up-regulated genes critical for coagulation, such as tissue factor, whereas supernatants from IL-17-treated endothelial cells induced strong platelet aggregation[47].
Attenuation of inflammation should logically diminish the incidence of atherosclerosis and CVD. However, drugs that combat inflammation do not necessarily protect against CVD. On the contrary, potent anti-inflammatory agents such as steroids and non-steroidal anti-inflammatory drugs (NSAIDs) bare warnings regarding associated cardiovascular risk. However, which is their cumulative result on CVD when used in the context of chronic inflammation needs careful consideration. Regarding the use of steroids, a metanalysis with more than 100000 participants, including a large number of patients with RA, showed that the use of glucocorticosteroids is clearly linked with increased incidence of cardiovascular events21[48]. Things are more complicated when NSAIDs, including selective inhibitors of cyclooxygenase-2 (COX-2) are examined. Rofecoxib for example was withdrawn from the market due to cardiovascular harm, while celecoxib - another COX-2 inhibitor - appears to be much safer[49]. Interestingly, celecoxib has been shown to have a protective effect on vasculature[50]. Diverse effects between different NSAIDs however are proposed to stem from differential actions involving COX-2 independent pathways[51]. In particular, contrary to naproxen and ibuprofen, celecoxib activates COX-2-independent AMPK-CREB-Nrf2 pathways resulting in significant anti-inflammatory effects including inhibition of TNF-α-mediated NF-κB signaling, and IL-1β induction of IL-6[51].
Successful control of inflammation and disease activity in patients with RA and other rheumatic diseases using conventional and biologic disease modifying anti-rheumatic drugs (DMARDs) appears in some studies to coincide with decreased risk of CVD. Indeed, a recent meta-analysis showed that anti-TNF-a biologic treatment, as well as use of methotrexate - a conventional DMARD - are associated with reduced risk of cardiovascular events[52]. Moreover, TNF inhibitors showed decreased risk of myocardial infarction when compared to methotrexate and other conventional DMARDs[53]. In an elegant study in patients with psoriasis and psoriatic arthritis, where men had significantly higher total carotid plaque progression as assessed by ultrasound, TNF-inhibitor treatment was associated with reduced atherosclerosis progression in men but not in women[54]. Also in PsA patients, aortic vascular inflammation, assessed by 18F-FDG PET CT scan, was reduced in men and women treated with TNF inhibitors[54]. It should be noted that focal vascular inflammation, assessed by 18F-FDG PET CT scan, precedes calcium deposition, a marker of atherosclerotic plaque progression[55]. These results provide evidence that TNF-inhibitors decrease vascular inflammation and thus may inhibit atherosclerosis progression but do not explain the difference of TNF-a inhibitor effect on carotid plaque progression between men and women.
Canakinumab is an anti-IL-2b monoclonal antibody that has been recently developed initially for the treatment of hereditary Cryopyrin-Associated Periodic Syndromes, which represent a subset of hereditary autoinflammatory diseases and is now used for a number of other autoinflammatory diseases such as juvenile idiopathic arthritis among others. In a recent groundbreaking study, canakinumab was however tested in another population. The Canakinumab Anti-inflammatory Thrombosis Outcomes Study (CANTOS), a randomized double-blind placebo-controlled trial of over 10000 patients with previous myocardial infarction and high sensitive CRP above 2 mg/L, showed that at median follow up of 3.7 years, canakinumab (150 mg/3 mo) significantly reduced cardiovascular events independent of lipid levels[56]. Although, a previous study had unexpectedly shown that mice lacking IL-1 receptor display advanced atherosclerosis[57], and thus disrupting our linear thinking regarding the pro-inflammatory atherogenic effects of IL-1, CANTOS, a large prospective trial, is the best proof of the pathogenic contribution of inflammation in atherosclerosis and CVD in humans to date.
Inflammation holds an integral role in atherogenesis and consequent CVD. Numerous mechanisms have been identified (Figure 1). It is expected that different mechanisms may not equally contribute to the development of CVD. Moreover, distinct clinical states may involve separate pathways. The ability to accurately assess the mechanisms underlying CVD risk in each patient represents a true challenge, which currently is only partially evaluated. Knowing which mechanism(s) are crucial among different groups of patients will guide us when and how to intervene. Several drugs used in clinical practice such as monoclonal antibodies, which specifically aim different targets involved in inflammatory interactions, may prove valuable tools towards the control of CVD.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country of origin: Greece
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Schoenhagen P, Soriano-Ursúa MA S- Editor: Cui LJ L- Editor: A E- Editor: Bian YN
| 1. | Moran AE, Roth GA, Narula J, Mensah GA. 1990-2010 global cardiovascular disease atlas. Glob Heart. 2014;9:3-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 93] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 2. | Steinberg D. Thematic review series: the pathogenesis of atherosclerosis. An interpretive history of the cholesterol controversy, part V: the discovery of the statins and the end of the controversy. J Lipid Res. 2006;47:1339-1351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 119] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 3. | Zhu Y, Xian X, Wang Z, Bi Y, Chen Q, Han X, Tang D, Chen R. Research Progress on the Relationship between Atherosclerosis and Inflammation. Biomolecules. 2018;8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 221] [Cited by in RCA: 587] [Article Influence: 83.9] [Reference Citation Analysis (0)] |
| 4. | Mayerl C, Lukasser M, Sedivy R, Niederegger H, Seiler R, Wick G. Atherosclerosis research from past to present--on the track of two pathologists with opposing views, Carl von Rokitansky and Rudolf Virchow. Virchows Arch. 2006;449:96-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 101] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Lobstein J. Traite d’Anatomie Pathologique. Paris: Levrault FG, 1829: 233. . |
| 6. | Leibowitz J. The history of coronary heart disease. Berkeley: University of California Press, 1970. . |
| 7. | Hodgson J. A treatise on the diseases of arteries and veins, containing the pathology and treatment of aneurisms and wounded arteries. London: Underwood, 1815: 1. . |
| 8. | The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. Am J Epidemiol. 1989;129:687-702. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2485] [Cited by in RCA: 2634] [Article Influence: 73.2] [Reference Citation Analysis (0)] |
| 9. | Folsom AR, Kronmal RA, Detrano RC, O'Leary DH, Bild DE, Bluemke DA, Budoff MJ, Liu K, Shea S, Szklo M, Tracy RP, Watson KE, Burke GL. Coronary artery calcification compared with carotid intima-media thickness in the prediction of cardiovascular disease incidence: the Multi-Ethnic Study of Atherosclerosis (MESA). Arch Intern Med. 2008;168:1333-1339. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 599] [Cited by in RCA: 552] [Article Influence: 32.5] [Reference Citation Analysis (0)] |
| 10. | Sharrett AR. Invasive versus noninvasive studies of risk factors and atherosclerosis. Circulation. 1993;87:II48-II53. [PubMed] |
| 11. | Kraehling JR, Chidlow JH, Rajagopal C, Sugiyama MG, Fowler JW, Lee MY, Zhang X, Ramírez CM, Park EJ, Tao B, Chen K, Kuruvilla L, Larriveé B, Folta-Stogniew E, Ola R, Rotllan N, Zhou W, Nagle MW, Herz J, Williams KJ, Eichmann A, Lee WL, Fernández-Hernando C, Sessa WC. Genome-wide RNAi screen reveals ALK1 mediates LDL uptake and transcytosis in endothelial cells. Nat Commun. 2016;7:13516. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 85] [Cited by in RCA: 127] [Article Influence: 14.1] [Reference Citation Analysis (0)] |
| 12. | Armstrong SM, Sugiyama MG, Fung KY, Gao Y, Wang C, Levy AS, Azizi P, Roufaiel M, Zhu SN, Neculai D, Yin C, Bolz SS, Seidah NG, Cybulsky MI, Heit B, Lee WL. A novel assay uncovers an unexpected role for SR-BI in LDL transcytosis. Cardiovasc Res. 2015;108:268-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 121] [Article Influence: 12.1] [Reference Citation Analysis (1)] |
| 13. | Kruth HS. Sequestration of aggregated low-density lipoproteins by macrophages. Curr Opin Lipidol. 2002;13:483-488. [PubMed] |
| 14. | Steinberg D. Atherogenesis in perspective: hypercholesterolemia and inflammation as partners in crime. Nat Med. 2002;8:1211-1217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 483] [Cited by in RCA: 479] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 15. | Marcovecchio PM, Thomas GD, Mikulski Z, Ehinger E, Mueller KAL, Blatchley A, Wu R, Miller YI, Nguyen AT, Taylor AM, McNamara CA, Ley K, Hedrick CC. Scavenger Receptor CD36 Directs Nonclassical Monocyte Patrolling Along the Endothelium During Early Atherogenesis. Arterioscler Thromb Vasc Biol. 2017;37:2043-2052. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 67] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 16. | Libby P. Inflammation in atherosclerosis. Arterioscler Thromb Vasc Biol. 2012;32:2045-2051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1404] [Cited by in RCA: 1637] [Article Influence: 125.9] [Reference Citation Analysis (0)] |
| 17. | Getz GS, Reardon CA. Atherogenic lipids and macrophage subsets. Curr Opin Lipidol. 2015;26:357-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Stewart CR, Stuart LM, Wilkinson K, van Gils JM, Deng J, Halle A, Rayner KJ, Boyer L, Zhong R, Frazier WA, Lacy-Hulbert A, El Khoury J, Golenbock DT, Moore KJ. CD36 ligands promote sterile inflammation through assembly of a Toll-like receptor 4 and 6 heterodimer. Nat Immunol. 2010;11:155-161. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1163] [Cited by in RCA: 1179] [Article Influence: 78.6] [Reference Citation Analysis (0)] |
| 19. | Duewell P, Kono H, Rayner KJ, Sirois CM, Vladimer G, Bauernfeind FG, Abela GS, Franchi L, Nuñez G, Schnurr M, Espevik T, Lien E, Fitzgerald KA, Rock KL, Moore KJ, Wright SD, Hornung V, Latz E. NLRP3 inflammasomes are required for atherogenesis and activated by cholesterol crystals. Nature. 2010;464:1357-1361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3165] [Cited by in RCA: 3017] [Article Influence: 201.1] [Reference Citation Analysis (0)] |
| 20. | Sheedy FJ, Grebe A, Rayner KJ, Kalantari P, Ramkhelawon B, Carpenter SB, Becker CE, Ediriweera HN, Mullick AE, Golenbock DT, Stuart LM, Latz E, Fitzgerald KA, Moore KJ. CD36 coordinates NLRP3 inflammasome activation by facilitating intracellular nucleation of soluble ligands into particulate ligands in sterile inflammation. Nat Immunol. 2013;14:812-820. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 588] [Cited by in RCA: 726] [Article Influence: 60.5] [Reference Citation Analysis (0)] |
| 21. | Libby P, Hansson GK. Taming Immune and Inflammatory Responses to Treat Atherosclerosis. J Am Coll Cardiol. 2018;71:173-176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 22. | Ketelhuth DF, Hansson GK. Adaptive Response of T and B Cells in Atherosclerosis. Circ Res. 2016;118:668-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 204] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 23. | Hermann S, Kuhlmann MT, Starsichova A, Eligehausen S, Schäfers K, Stypmann J, Tiemann K, Levkau B, Schäfers M. Imaging Reveals the Connection Between Spontaneous Coronary Plaque Ruptures, Atherothrombosis, and Myocardial Infarctions in HypoE/SRBI-/- Mice. J Nucl Med. 2016;57:1420-1427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Gonzalez L, Trigatti BL. Macrophage Apoptosis and Necrotic Core Development in Atherosclerosis: A Rapidly Advancing Field with Clinical Relevance to Imaging and Therapy. Can J Cardiol. 2017;33:303-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 96] [Article Influence: 10.7] [Reference Citation Analysis (0)] |
| 25. | Kojima Y, Weissman IL, Leeper NJ. The Role of Efferocytosis in Atherosclerosis. Circulation. 2017;135:476-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 214] [Article Influence: 26.8] [Reference Citation Analysis (0)] |
| 26. | Yurdagul A, Doran AC, Cai B, Fredman G, Tabas IA. Mechanisms and Consequences of Defective Efferocytosis in Atherosclerosis. Front Cardiovasc Med. 2018;4:86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 27. | Leeper NJ. The role of necroptosis in atherosclerotic disease. JACC Basic Transl Sci. 2016;1:548-550. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 28. | Coornaert I, Hofmans S, Devisscher L, Augustyns K, Van Der Veken P, De Meyer GRY, Martinet W. Novel drug discovery strategies for atherosclerosis that target necrosis and necroptosis. Expert Opin Drug Discov. 2018;13:477-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 29. | Steensma DP, Bejar R, Jaiswal S, Lindsley RC, Sekeres MA, Hasserjian RP, Ebert BL. Clonal hematopoiesis of indeterminate potential and its distinction from myelodysplastic syndromes. Blood. 2015;126:9-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1086] [Cited by in RCA: 1426] [Article Influence: 142.6] [Reference Citation Analysis (0)] |
| 30. | Jaiswal S, Natarajan P, Silver AJ, Gibson CJ, Bick AG, Shvartz E, McConkey M, Gupta N, Gabriel S, Ardissino D, Baber U, Mehran R, Fuster V, Danesh J, Frossard P, Saleheen D, Melander O, Sukhova GK, Neuberg D, Libby P, Kathiresan S, Ebert BL. Clonal Hematopoiesis and Risk of Atherosclerotic Cardiovascular Disease. N Engl J Med. 2017;377:111-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1338] [Cited by in RCA: 1869] [Article Influence: 233.6] [Reference Citation Analysis (0)] |
| 31. | Fuster JJ, MacLauchlan S, Zuriaga MA, Polackal MN, Ostriker AC, Chakraborty R, Wu CL, Sano S, Muralidharan S, Rius C, Vuong J, Jacob S, Muralidhar V, Robertson AA, Cooper MA, Andrés V, Hirschi KK, Martin KA, Walsh K. Clonal hematopoiesis associated with TET2 deficiency accelerates atherosclerosis development in mice. Science. 2017;355:842-847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 722] [Cited by in RCA: 1096] [Article Influence: 137.0] [Reference Citation Analysis (0)] |
| 32. | Liuzzo G, Biasucci LM, Gallimore JR, Grillo RL, Rebuzzi AG, Pepys MB, Maseri A. The prognostic value of C-reactive protein and serum amyloid a protein in severe unstable angina. N Engl J Med. 1994;331:417-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1615] [Cited by in RCA: 1583] [Article Influence: 51.1] [Reference Citation Analysis (0)] |
| 33. | Ridker PM, Hennekens CH, Buring JE, Rifai N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000;342:836-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4096] [Cited by in RCA: 4134] [Article Influence: 165.4] [Reference Citation Analysis (0)] |
| 34. | Emerging Risk Factors Collaboration; Kaptoge S, Di Angelantonio E, Lowe G, Pepys MB, Thompson SG, Collins R, Danesh J. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet. 2010;375:132-140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1615] [Cited by in RCA: 1863] [Article Influence: 124.2] [Reference Citation Analysis (0)] |
| 35. | Gabriel SE. Cardiovascular morbidity and mortality in rheumatoid arthritis. Am J Med. 2008;121:S9-14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 206] [Cited by in RCA: 198] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 36. | Warrington KJ, Kent PD, Frye RL, Lymp JF, Kopecky SL, Goronzy JJ, Weyand CM. Rheumatoid arthritis is an independent risk factor for multi-vessel coronary artery disease: a case control study. Arthritis Res Ther. 2005;7:R984-R991. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 104] [Cited by in RCA: 104] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 37. | Peters MJ, van Halm VP, Voskuyl AE, Smulders YM, Boers M, Lems WF, Visser M, Stehouwer CD, Dekker JM, Nijpels G, Heine R, Dijkmans BA, Nurmohamed MT. Does rheumatoid arthritis equal diabetes mellitus as an independent risk factor for cardiovascular disease? A prospective study. Arthritis Rheum. 2009;61:1571-1579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 257] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 38. | Hashizume M, Mihara M. Blockade of IL-6 and TNF-α inhibited oxLDL-induced production of MCP-1 via scavenger receptor induction. Eur J Pharmacol. 2012;689:249-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 40] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 39. | Hashizume M, Mihara M. Atherogenic effects of TNF-α and IL-6 via up-regulation of scavenger receptors. Cytokine. 2012;58:424-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 84] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 40. | Westhovens R, Nijs J, Taelman V, Dequeker J. Body composition in rheumatoid arthritis. Br J Rheumatol. 1997;36:444-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 76] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 41. | Giles JT, Bartlett SJ, Andersen R, Thompson R, Fontaine KR, Bathon JM. Association of body fat with C-reactive protein in rheumatoid arthritis. Arthritis Rheum. 2008;58:2632-2641. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 63] [Cited by in RCA: 64] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 42. | Gonzalez-Juanatey C, Testa A, Garcia-Castelo A, Garcia-Porrua C, Llorca J, Ollier WE, Gonzalez-Gay MA. Echocardiographic and Doppler findings in long-term treated rheumatoid arthritis patients without clinically evident cardiovascular disease. Semin Arthritis Rheum. 2004;33:231-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 80] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 43. | Davis JM, Roger VL, Crowson CS, Kremers HM, Therneau TM, Gabriel SE. The presentation and outcome of heart failure in patients with rheumatoid arthritis differs from that in the general population. Arthritis Rheum. 2008;58:2603-2611. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 137] [Cited by in RCA: 129] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 44. | Nurmohamed MT, Heslinga M, Kitas GD. Cardiovascular comorbidity in rheumatic diseases. Nat Rev Rheumatol. 2015;11:693-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 235] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 45. | Arida A, Protogerou AD, Kitas GD, Sfikakis PP. Systemic Inflammatory Response and Atherosclerosis: The Paradigm of Chronic Inflammatory Rheumatic Diseases. Int J Mol Sci. 2018;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 86] [Cited by in RCA: 131] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 46. | Cooksey R, Brophy S, Kennedy J, Gutierrez FF, Pickles T, Davies R, Piguet V, Choy E. Cardiovascular risk factors predicting cardiac events are different in patients with rheumatoid arthritis, psoriatic arthritis, and psoriasis. Semin Arthritis Rheum. 2018;48:367-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 47. | Hot A, Lenief V, Miossec P. Combination of IL-17 and TNFα induces a pro-inflammatory, pro-coagulant and pro-thrombotic phenotype in human endothelial cells. Ann Rheum Dis. 2012;71:768-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 123] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 48. | Souverein PC, Berard A, Van Staa TP, Cooper C, Egberts AC, Leufkens HG, Walker BR. Use of oral glucocorticoids and risk of cardiovascular and cerebrovascular disease in a population based case-control study. Heart. 2004;90:859-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 354] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 49. | Nissen SE, Yeomans ND, Solomon DH, Lüscher TF, Libby P, Husni ME, Graham DY, Borer JS, Wisniewski LM, Wolski KE, Wang Q, Menon V, Ruschitzka F, Gaffney M, Beckerman B, Berger MF, Bao W, Lincoff AM; PRECISION Trial Investigators. Cardiovascular Safety of Celecoxib, Naproxen, or Ibuprofen for Arthritis. N Engl J Med. 2016;375:2519-2529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 498] [Cited by in RCA: 525] [Article Influence: 58.3] [Reference Citation Analysis (0)] |
| 50. | Chenevard R, Hürlimann D, Béchir M, Enseleit F, Spieker L, Hermann M, Riesen W, Gay S, Gay RE, Neidhart M, Michel B, Lüscher TF, Noll G, Ruschitzka F. Selective COX-2 inhibition improves endothelial function in coronary artery disease. Circulation. 2003;107:405-409. [PubMed] |
| 51. | Al-Rashed F, Calay D, Lang M, Thornton CC, Bauer A, Kiprianos A, Haskard DO, Seneviratne A, Boyle JJ, Schönthal AH, Wheeler-Jones CP, Mason JC. Celecoxib exerts protective effects in the vascular endothelium via COX-2-independent activation of AMPK-CREB-Nrf2 signalling. Sci Rep. 2018;8:6271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 39] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 52. | Roubille C, Richer V, Starnino T, McCourt C, McFarlane A, Fleming P, Siu S, Kraft J, Lynde C, Pope J, Gulliver W, Keeling S, Dutz J, Bessette L, Bissonnette R, Haraoui B. The effects of tumour necrosis factor inhibitors, methotrexate, non-steroidal anti-inflammatory drugs and corticosteroids on cardiovascular events in rheumatoid arthritis, psoriasis and psoriatic arthritis: a systematic review and meta-analysis. Ann Rheum Dis. 2015;74:480-489. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 692] [Cited by in RCA: 656] [Article Influence: 65.6] [Reference Citation Analysis (0)] |
| 53. | Low AS, Symmons DP, Lunt M, Mercer LK, Gale CP, Watson KD, Dixon WG, Hyrich KL; British Society for Rheumatology Biologics Register for Rheumatoid Arthritis (BSRBR-RA) and the BSRBR Control Centre Consortium. Relationship between exposure to tumour necrosis factor inhibitor therapy and incidence and severity of myocardial infarction in patients with rheumatoid arthritis. Ann Rheum Dis. 2017;76:654-660. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 122] [Cited by in RCA: 117] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 54. | Eder L, Joshi AA, Dey AK, Cook R, Siegel EL, Gladman DD, Mehta NN. Association of Tumor Necrosis Factor Inhibitor Treatment With Reduced Indices of Subclinical Atherosclerosis in Patients With Psoriatic Disease. Arthritis Rheumatol. 2018;70:408-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 55. | Abdelbaky A, Corsini E, Figueroa AL, Fontanez S, Subramanian S, Ferencik M, Brady TJ, Hoffmann U, Tawakol A. Focal arterial inflammation precedes subsequent calcification in the same location: a longitudinal FDG-PET/CT study. Circ Cardiovasc Imaging. 2013;6:747-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 133] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 56. | Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, Fonseca F, Nicolau J, Koenig W, Anker SD, Kastelein JJP, Cornel JH, Pais P, Pella D, Genest J, Cifkova R, Lorenzatti A, Forster T, Kobalava Z, Vida-Simiti L, Flather M, Shimokawa H, Ogawa H, Dellborg M, Rossi PRF, Troquay RPT, Libby P, Glynn RJ; CANTOS Trial Group. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N Engl J Med. 2017;377:1119-1131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4997] [Cited by in RCA: 6586] [Article Influence: 823.3] [Reference Citation Analysis (0)] |
| 57. | Rader DJ. IL-1 and atherosclerosis: a murine twist to an evolving human story. J Clin Invest. 2012;122:27-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |