Peer-review started: June 16, 2016
First decision: July 27, 2016
Revised: October 17, 2016
Accepted: November 1, 2016
Article in press: November 2, 2016
Published online: January 6, 2017
Processing time: 198 Days and 4.2 Hours
Hypertonicity causes severe clinical manifestations and is associated with mortality and severe short-term and long-term neurological sequelae. The main clinical syndromes of hypertonicity are hypernatremia and hyperglycemia. Hypernatremia results from relative excess of body sodium over body water. Loss of water in excess of intake, gain of sodium salts in excess of losses or a combination of the two are the main mechanisms of hypernatremia. Hypernatremia can be hypervolemic, euvolemic or hypovolemic. The management of hypernatremia addresses both a quantitative replacement of water and, if present, sodium deficit, and correction of the underlying pathophysiologic process that led to hypernatremia. Hypertonicity in hyperglycemia has two components, solute gain secondary to glucose accumulation in the extracellular compartment and water loss through hyperglycemic osmotic diuresis in excess of the losses of sodium and potassium. Differentiating between these two components of hypertonicity has major therapeutic implications because the first component will be reversed simply by normalization of serum glucose concentration while the second component will require hypotonic fluid replacement. An estimate of the magnitude of the relative water deficit secondary to osmotic diuresis is obtained by the corrected sodium concentration, which represents a calculated value of the serum sodium concentration that would result from reduction of the serum glucose concentration to a normal level.
Core tip: States of hypertonicity cause transfer of fluid from inside the body cells into the fluid compartment surrounding the cells. The shrinking of the brain cells in hypertonicity causes severe manifestations and even death. The management of hypertonicity requires administration of intravenous solutions. The volume and the composition of the administered solutions are calculated by various equations. Close monitoring of the condition of the patient and frequent measurements of appropriate blood chemistries during treatment are critical steps for a favorable outcome. The two major states of hypertonicity are hypernatremia, an elevation of the concentration of sodium in the blood, and hyperglycemia, an elevation of the concentration of glucose in the blood. The management of severe hypertonicity in hypernatremia and hyperglycemia encounters different obstacles and requires different equations for the quantitative replacement of body fluid deficits.
- Citation: Rondon-Berrios H, Argyropoulos C, Ing TS, Raj DS, Malhotra D, Agaba EI, Rohrscheib M, Khitan ZJ, Murata GH, Shapiro JI, Tzamaloukas AH. Hypertonicity: Clinical entities, manifestations and treatment. World J Nephrol 2017; 6(1): 1-13
- URL: https://www.wjgnet.com/2220-6124/full/v6/i1/1.htm
- DOI: https://dx.doi.org/10.5527/wjn.v6.i1.1
A previous report discussed pathophysiological aspects, quantitative predictions and experimental testing of hypertonicity[1]. Knowledge of these fields is critical in understanding the clinical consequences of hypertonicity and in guiding their correction. Hypertonicity causes severe clinical manifestations and death. In addition to the degree of hypertonicity, the rapidity of its development is an important factor in the severity of its clinical manifestations, whether one deals with hypertonicity developing de novo or as a complication of treatment of a hypotonic state. In the second case, severe neurological manifestations may develop after rapid rises in tonicity even when it does not reach hypertonicity levels[2]. The neurological manifestations of hypertonicity are secondary to cell shrinking due to osmotic transfer of water out of cells[1]. Spontaneous restoration of cell volume after development of hypertonicity is achieved following cellular solute gain by intracellular transfer of extracellular electrolytes and both intracellular entry and cellular formation of new organic osmolytes[1].
Intracellular acquisition of organic osmolytes following a hypertonic stimulus is slower than electrolyte acquisition because it depends on slow tonicity-induced transcription and expression of genes regulating osmolyte transport and generation processes[1]. Consequently cellular acquisition of organic osmolytes characterizes the chronicity of a hypertonic state. Hypertonicity of less than 48 h duration is categorized as acute while hypertonicity of longer that 48 h duration is categorized as chronic. The slow nature of organic osmolyte acquisition has clinical consequences both during rapid development of hypertonicity when rates of increase in tonicity exceed the capacity of the brain to acquire organic osmolytes and during its treatment when the slow loss of brain osmolytes may cause swelling of the brain cells[3-6]. This report presents the pathology, clinical manifestations, major categories, and principles of correction of hypertonicity.
The pathology of the brain has been studied in both patients who died during hypertonic episodes[7] and experiments in animals subjected acutely to severe hypertonicity[8]. The histologic changes are the consequence of decrease in the brain cell volume. In acute hypertonicity the brain looks shrunken with many petechial hemorrhages and larger hemorrhages in the subarachnoid space. The hemorrhages are a consequence of brain shrinking. They result from tearing of bridging veins which cross the subdural space. There are also subdural fluid collections and hematomas, vascular congestion and venous occlusion and thrombosis[7,8].
The clinical manifestations of acute hypertonicity result from both shrinking of the brain cells and vascular changes. Very young and very old patients are most commonly affected by this disorder. The manifestations of acute hypertonicity vary between these two age groups. Children with acute hypertonicity typically present with symptoms that progress in severity from irritability, restlessness and muscular twitching to hyperreflexia and seizures[9,10]. Elderly with hypertonicity may present with lethargy, delirium and coma, but rarely if ever develop seizures[10,11]. Patients with hypertonicity may develop fever, nausea and vomiting[10]. Intense thirst is a frequent complaint of patients with hypertonicity who are not comatose[9,10]. Clinical signs of hypovolemia (orthostatic hypotension and pulse increase, decreased skin turgor, flat neck veins, dry mucous membranes) may be present when the hypertonic state was created by net loss of hypotonic fluids[9,10]. Death may follow coma and seizures[7]. Mortality is high in children with acute hypertonicity[10]. One study reported severe neurological deficits in the majority of infants who survived severe episodes of hypertonicity[12]. However, these infants were also suffering from other illnesses that can cause permanent neurological damage (e.g., meningitis). The degree of hypertonicity correlates with the depression of sensorium in hospitalized elderly patients with hypernatremia[13].
Chronic hypertonic states may manifest with only subtle neurological changes even when hypertonicity is severe. However, mortality in adults with chronic hypertonicity is also high[11]. The osmotic demyelination syndrome following rapid rise in serum tonicity during correction of hyponatremia or during acute hypernatremia has a high mortality and may cause severe neurological deficits[14].
Hypertonicity denotes relative excess of solute with extracellular distribution over body water regardless of whether body water is normal, reduced or excessive. Relative excess of solutes distributed in body water cause rises in the osmolality of body fluids, but has no effects on tonicity. Sodium salts, including sodium chloride and sodium bicarbonate, are the major extracellular solutes. Although the largest, by far, amount of sodium easily accessible to osmotic events is in the extracellular compartment, its apparent volume of distribution is total body water. This means that extracellular sodium concentration represents the fraction of total extracellular sodium and total intracellular potassium over total body water when there are no excesses of other extracellular solutes[15]. Hypernatremia from relative excess of sodium salts represents a major category of hypertonicity[16-18]. Unlike hyponatremia, which may be associated with hypotonicity, isotonicity or hypertonicity, hypernatremia routinely indicates hypertonicity. A rare exception is encountered when the serum sodium concentration ([Na]S) is overestimated if it is measured by indirect ion-selective potentiometry in subjects with decreased serum solid content[19]. The degree of overestimation of [Na]S in this instance is modest. For example, indirect potentiometry would report a [Na]S value of 148.5 mmol/L in a patient with true [Na]S equal to 145 mmol/L and serum solids equal to an extremely low 2% of his/her serum volume[19].
In addition to sodium salts, other solutes with extracellular distribution can cause hypertonicity. As in the case of relative sodium excess, gain in other extracellular solutes leads to osmotic exit of water from the intracellular compartment. The osmotic water transfer dilutes the extracellular solutes. Sodium salts normally represent the great majority of these solutes. As a consequence of the osmotic fluid shift into the intracellular compartment, hypertonicity is typically associated with hyponatremia in case of excess of extracellular solutes other than sodium salts. Solutes responsible for hypertonic hyponatremia may be exogenous, e.g., mannitol, or endogenous, e.g., glucose[20,21]. This report will analyze the topics of hypernatremia and hyperglycemia, which represent the most common syndromes of hypertonicity. However, it should be remembered that hypertonicity secondary to exogenous solutes is the source of diagnostic miscues and potential mismanagement of patients presenting with hyponatremia if the previous infusion history is not known to the treating medical practitioners[22].
Hypernatremia, defined as a [Na]S exceeding 145 mmol/L, has an estimated prevalence of 2% among patients admitted to hospitals and is less common than hyponatremia, which is seen in about 10% of this population[23].
The determinants of [Na]S, when there are no excesses of other extracellular solutes, are total exchangeable body sodium, total exchangeable body potassium and total body water[24]. Like hyponatremia[14,25,26], hypernatremia results from isolated or combined changes of these determinants. While hyponatremia secondary to potassium deficits has been documented, hypernatremia secondary to potassium excess has not been reported, to our knowledge. This may be due to the limitations of available methods measuring total body potassium, to the lethal consequences of even small potassium gains, or to a combination of the two mechanisms. Anyway, hypernatremia should be analyzed as a disorder of the relationship between body sodium and body water. Table 1 shows potential combinations of changes in body sodium and water resulting in hypernatremia and clinical examples for each pathophysiologic combination.
| Nae | Body H2O | Clinical example |
| ↔ | ↓ | Diabetes insipidus |
| ↑ | ↔ | Salt tablet ingestion |
| ↑↑ | ↑ | Hypertonic infusions containing sodium salts |
| ↓ | ↓↓ | Loop diuretics, excessive sweating, osmotic diarrhea, osmotic diuresis |
| ↑ | ↓ | Not seen in practice |
Body water abnormalities are the cause of hypernatremia in a large number of cases. In these subjects hypernatremia develops following a discrepancy between water intake and water output resulting in net water deficit. This discrepancy is usually the result of inadequate water intake in the setting of normal or increased water losses. Table 2 shows clinical conditions characterized by inadequate water intake and leading to hypernatremia.
| Lack of water sources |
| Subject lost in desert |
| Inability of patient to drink water or ask for it |
| Tracheal intubation and sedation |
| Dementia |
| Delirium |
| Paranoia |
| Severe depression |
| Adipsia or hypodipsia caused by central nervous system disorder compromising the neural pathways of thirst |
| Granulomas, e.g., sarcoidosis |
| Tumors, e.g., craniopharyngioma, seminoma, lymphoma, astrocytoma |
| Degenerative processes, e.g., Parkinson’s disease |
| Congenital syndromes, e.g., ectodactyly-ectodermal dysplasia- cleftlip-palate syndrome |
| Diabetes insipidus (a fraction of the patients) |
Under normal conditions, water losses through respiration, the gastrointestinal fluids, the urine and the skin constitute the obligatory water loss. Obligatory water loss is normally in relative excess to the losses in sodium and potassium. Patients unable to replete their obligatory losses of water are prone to hypernatremia. However, even increased water loss does not cause hypernatremia in conscious individuals, except in exceptional cases. Hypertonicity is the major stimulus of thirst[27]. Nephrectomized animals subjected to hypertonic stimuli consumed enough water to maintain their serum tonicity within the baseline normal levels[28]. Increased water loss leads to increased water intake in conscious individuals having free access to water. Consequently, large water loss does not result in significant hypernatremia unless it is enormous or it is combined with inability to drink water for various reasons (Table 2).
Table 3 shows clinical states causing excessive water loss. Large water losses causing hypernatremia can be of extrarenal or renal origin. Extrarenal sites of water loss are the skin, the respiratory system and the gastrointestinal tract. Fluid losses from the gastrointestinal tract can be of enormous magnitude, are routinely hypotonic and lead to hypernatremia particularly in infants or children[29,30]. Table 4 shows the electrolyte composition of gastrointestinal fluids[31].
| Extrarenal water loss |
| Gastrointestinal losses |
| Vomiting |
| Nasogastric drainage |
| Ileostomy |
| Pancreatobiliary fistula |
| Diarrhea (non-secretory) |
| Laxatives, e.g., lactulose |
| Skin |
| Excessive sweating |
| Respiratory airways |
| Hyperpnea |
| Tracheal intubation |
| Mechanical ventilation |
| Excessive renal water losses |
| Osmotic (solute) diuresis |
| Osmotic diuretics, e.g., mannitol |
| Glucosuria, e.g., hyperglycemia, sodium-glucose transporter 2 (SGLT2) inhibitors |
| Urea diuresis, e.g., diuresis post-acute tubular necrosis, post- obstructive diuresis, use of catabolic medications (corticosteroids, tetracyclines, etc.), high protein intake, urea treatment for hyponatremia |
| Salt diuresis, e.g., intravenous infusion of saline, high salt intake |
| Water diuresis |
| Central diabetes insipidus |
| Idiopathic (most common) |
| Genetic: Familial (mutation causing misfolding of vasopressin), congenital hypopituitarism, Wolfram syndrome (diabetes insipidus, diabetes mellitus, optic atrophy, deafness) |
| Acquired: Neurosurgery, head trauma, brain tumors, infiltrative disorders (sarcoidosis, Langerhans cell histiocytosis, etc.) |
| Nephrogenic diabetes insipidus |
| Genetic: Inactivating mutations of V2 receptor gene (most common) or aquaporin 2 gene |
| Acquired: |
| Renal disease (chronic renal failure, post-acute tubular necrosis, obstructive nephropathy, sickle cell disease, autosomal dominant polycystic kidney disease) |
| Electrolyte disorders: Hypokalemia, hypercalcemia |
| Drugs: Lithium, amphotericin, demeclocycline, ifosfamide, V2 receptor antagonists |
| Gestation: Increased placental production of vasopressinase |
| Upward resetting of the osmostat (reset osmostat): Primary hyperaldosteronism (thought to be secondary to volume expansion and resulting in modest hypernatremia, up to 147 mmol/L) |
| Fluid source | Sodium (mmol/L) | Potassium (mmol/L) |
| Vomiting, nasogastric drainage | 20-100 | 10-15 |
| Secretory diarrhea | 40-140 | 15-40 |
| Non-secretory diarrhea | 50-100 | 15-20 |
| Adapted ileostomy | 40-90 | 5 |
| New ileostomy | 115-140 | 5-15 |
| Sweat | 38-45 | 5 |
The ability of the kidneys to concentrate the urine constitutes the main defense against excessive water loss[10]. Two general mechanisms are responsible for renal water loss secondary to reduced urinary concentrating capacity: (1) decreased vasopressin production (diabetes insipidus) or impaired renal response to vasopressin (nephrogenic diabetes insipidus)[19,32]; and (2) increased urinary solute excretion (solute or osmotic diuresis). Osmotic diuresis leads to increased losses of both water and monovalent cations. The tendency to develop hypernatremia in this setting is due to the lower cation concentration (sodium plus potassium) in the urine than in plasma which leads to water loss in excess of the cation loss[33,34].
In a minority of cases, hypernatremia results from pure sodium excess, although this is usually associated with a lack of access to water. Isolated increase in body sodium may occur as a result of intake of salt tablets or infusion of hypertonic solutions of sodium salts. Salt poisoning from near-drowning in sea water[35], during environmental disasters or after suicidal attempts with soy sauce ingestion[36] have also been reported.
Like hyponatremia, hypernatremia is classified as hypervolemic, hypovolemic, or euvolemic[10,37]. The history and physical examination assist in the diagnosis of the type of hypernatremia and of its pathogenesis. Hypervolemic hypernatremia is encountered after ingestion of salt, often in the form of salt tablets. Both accidental and suicidal salt ingestion leading to severe hypernatremia have been reported. In hospitalized patients, hypervolemic hypernatremia develops after infusion of saline or sodium bicarbonate solutions without adequate water content[38-40]. Hypervolemic hypernatremia, with weight gain and edema formation is the most common category of hypernatremia developing after saline infusions in patients exhibiting difficulty in excreting solute loads[40]. Hypervolemic hypernatremia without edema may develop in patients with primary hyperaldosteronism, Cushing syndrome, or after ingestion of salt tablets or infusion of hypertonic sodium bicarbonate and has been noticed in the past immediately following dialysis with a dialysate containing high concentrations of dextrose[10].
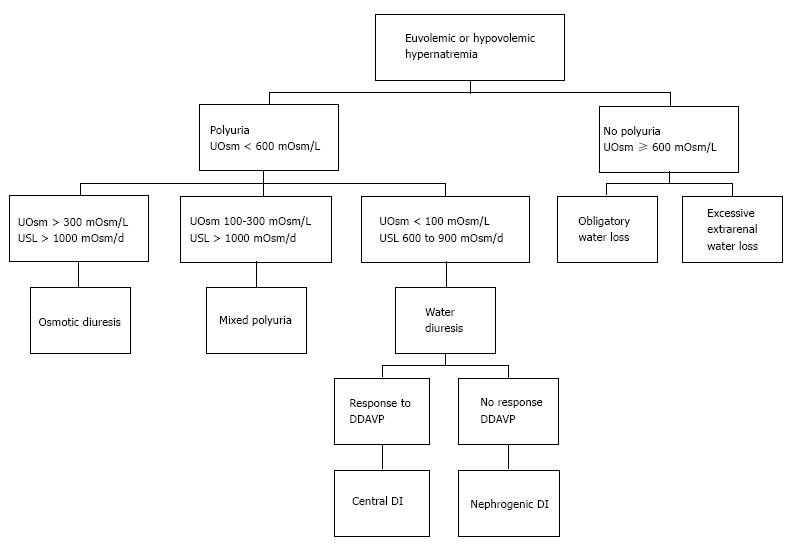
Hypovolemic or euvolemic hypernatremia occur in clinical settings that may be similar. The contribution of physical examination in the differential diagnosis between these two categories of hypernatremia is questionable when there are no clear-cut clinical signs of hypovolemia. History is of greater assistance in differentiating between hypovolemic and euvolemic hyponatremia in this case. Careful questioning addressing the presence or absence of thirst and the volume of urine allows further categorization of both hypovolemic and euvolemic hypernatremia. Figure 1 shows a diagnostic scheme for these two categories of hypernatremia.
Presence or absence of thirst and polyuria, and daily urinary solute load are the three characteristics of hypovolemic or euvolemic hypernatremias allowing a correct diagnosis of their pathophysiology (Figure 1). The combination of urine with high osmolality, and absence of polyuria and of high urinary solute output indicates either extrarenal water loss, when it is associated with thirst, or adipsia or hypodipsia, when thirst is absent. Polyuria associated with high urine osmolality and consequently with high urine solute load is a sign of osmotic diuresis. Polyuria associated with dilute urine and normal urine solute load is a sign of diabetes insipidus. In this last case, the response to desmopressin infusion leads to distinction between central and nephrogenic diabetes insipidus.
Acute hypernatremia, which is not encountered often, should be considered a medical emergency in the presence of severe neurological manifestations, e.g., seizures, or when [Na]S exceeds 160 mmol/L. Its treatment consists of intravenous infusion of large volumes of 5% dextrose in water (D5/W). The goal is to normalize [Na]S within 24 h. Hypotonic saline should be infused instead of D5/W when hypernatremia and volume deficit are present together.
Hypernatremia is chronic in the majority of instances. Chronic hypernatremia typically causes minimal symptoms or may be asymptomatic. The treatment of chronic hypernatremia has two aims. The first aim is to correct the existing deficit of water, and the deficit of sodium when present, by administration of water or hypotonic saline. Cerebral edema secondary to excessive entry of water into brain cells, primarily astrocytes, may complicate a rapid decline in [Na]S in severe chronic hypernatremia. Rapid correction of chronic hypernatremia in infants and children has resulted in seizures[7]. The target rate of decrease in [Na]S is 10 mmol/L in 24 h. The volume of hypotonic saline (V3) that is needed to produce a desired decrease in [Na]S is calculated as follows: The determinants of the final serum sodium concentration ([Na]S2) include V3, the presenting serum sodium concentration ([Na]S1), the sodium concentration in the infused hypotonic saline ([Na]S3) and the initial body water (V1). The value of the desired serum sodium concentration is calculated as[1]: [Na]S2 = ([Na]S1xV1 + [Na]S3xV3])/(V1 + V3) (1).
By rearranging equation 1, the following value of V3 for a desired [Na]S2 is: V3 = V1x([Na]S1 - [Na]S2)/([Na]S2 - [Na]S3) (2).
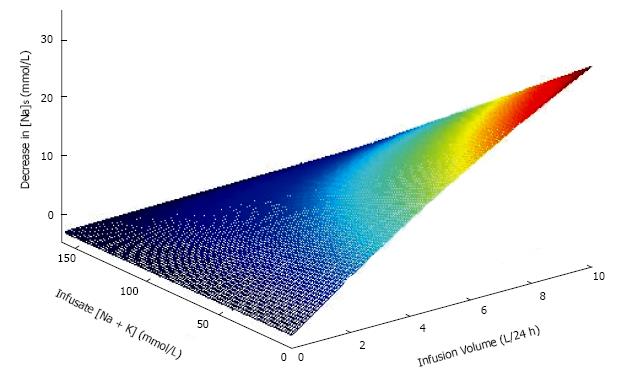
For example, equation 2 calculates that the volume V3 of half-normal saline ([Na]S3 = 77 mmol/L) needed to reduce [Na]S from a [Na]S1 value of 150 mmol/L to a [Na]S2 value of 140 mmol/L in a person with initial body water (V1) equal to 40 L is 6.67 L. Emphasis should be placed on entering as [Na]S3 in equation 2 the sum of sodium plus potassium concentrations in the infusate[18,25]. Figure 2 shows the effect on [Na]S of infusion of various volumes of solutions containing various combinations of sodium and potassium concentrations.
When the replacement fluid consists only of water, e.g., when 5% dextrose in water is infused, equation 2 takes the form: V3 = V1x([Na]S1 - [Na]S2)/[Na]S2 (3).
According to equation 3, the volume of dextrose in water required to reduce [Na]S from 150 to 140 mmol/L in a person with V1 equal to 40 L is 2.86 L.
The calculation of the volume of hypotonic saline or water required for a desired decrease in [Na]S by the method presented is subject to two types of error. The first potential error stems from the estimate of initial body water introduced in equations 2 and 3. Body water is calculated by formulas derived by comparing measurements of body water by dilution of an index substance (e.g., heavy water, tritiated water, and antipyrine) to anthropometric measurements. For adult patients, the anthropometric Watson formulas calculate body water as a function of gender, height, weight and, in men only, age[41]. For children, body water is calculated by the Mellits-Cheek formulas by the use of gender, weight and height[42]. Both the Watson and Mellits-Cheek formulas were derived from studies in subjects with euvolemia. Consequently, these formulas should be expected to provide a reasonable approximation of body water in subjects with euvolemia, but will systematically overestimate body water in subjects with hypovolemia and underestimate body water in subjects with hypervolemia[43]. If the weight at euvolemia has been recorded recently, an approximation of the body water at hypovolemia or hypervolemia can be obtained by calculating body water at the euvolemic weight and then subtracting from or adding to the euvolemic value of body water the difference between the euvolemic weight and the weight at presentation with volume abnormality[44]. This adjustment of body water is not feasible in most instances, particularly in chronic hypernatremia. In any case, the estimate of body water at presentation with hypernatremia is prone to significant errors.
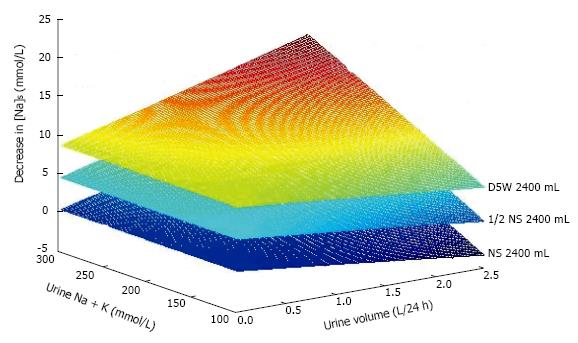
The second source of error is ongoing losses of fluid and monovalent cations during treatment. These losses, from the urinary tract, the gastrointestinal tract, the airways or the skin can be large but are not predictable and are not included in the equations calculating the volumes infused. Figure 3 shows the effects of varying urine volume with varying urinary monovalent cation (sodium plus potassium) concentrations on the change in [Na]S in a patient infused with the same volume of solutions containing various sodium concentrations.
Because of the potential magnitude of the errors introduced by body water estimates and urinary loses, close monitoring of the patient during treatment of hypernatremia is the critical measure of success. In addition to the clinical status and both [Na]S and serum glucose concentration ([Glu]S), the volume and electrolyte composition of external losses should be monitored. Serum measurements should be done frequently, e.g., every 4-6 h. Fluid and electrolyte losses should be replaced concomitantly with the calculated replacement fluid for correction of hypernatremia. Differences between changes in [Na]S observed and predicted by formulas 2 or 3 should lead to a search for the cause of these differences (i.e., erroneous values for body water used in the formulas or not accounted for losses in water and monovalent cations). Emergency hemodialysis[45,46] or peritoneal dialysis[47] should be considered in extreme cases of symptomatic hypernatremia or in severe hypernatremia in patients with end-stage renal disease with volume overload who may tolerate poorly even 5% dextrose in water infusions.
The second treatment aim is to manage the underlying cause of hypernatremia. For example, administration of corticosteroids may correct adipsia caused by neurosarcoidosis; intranasal or subcutaneous desmopressin (dDAVP) corrects the urinary concentrating defect of central diabetes insipidus; in nephrogenic diabetes insipidus, a diet low in sodium and protein reduces the urinary solute load and volume and thiazide diuretics induce hypovolemia which causes increased proximal tubular reabsorption of sodium and water, decreased delivery of water to the vasopressin-sensitive sites in the collecting tubules and reduction in the urine output.
Hypertonicity is one of the cardinal manifestations of hyperglycemic crises[48]. Assessment and management of hypertonicity in severe hyperglycemia are critical[49].
Serum tonicity([Ton]), in mOsm/L or mmol/L, is calculated in hyperglycemia as [Glu]S + 2x[Na]S with [Glu]S expressed in mmol/L[20]. The error from considering the osmotic coefficient of sodium salts in the serum as equal to 2 in this calculation is insignificant in most instances. When [Na]S is determined by indirect potentiometry, a significant underestimation of tonicity calculated by this formula occurs in hyperglycemic states associated with decreased water fraction of the serum, e.g., in patients with hyperlipidemia or elevated serum protein concentration. The normal range of serum tonicity is 280-290 mOsm/L.
Evaluation of the degree of hypertonicity in hypernatremia is simple. The rise in tonicity (Δ[Ton]) in this case is equal to 2 ×Δ[Na]S where Δ[Na]S is the rise in [Na]S above a normal level. In contrast to hypernatremia, evaluation of the degree of hypertonicity in hyperglycemia is complex. In this case, the mechanism of hypertonicity consists of two major influences, the primary (direct) effect of rise in extracellular solute content secondary to glucose gain and the secondary effects of hyperglycemia on solute and water balances. These effects are analyzed below.
The solute gain during development of hyperglycemia results in rises of different magnitude in serum glucose concentration (Δ[Glu]S) and tonicity(Δ[Ton]). The difference between Δ[Glu]S and Δ[Ton], when they are both expressed in mOsm/L, results from the fact that Δ[Glu]S represents the fraction solute (glucose) gain over extracellular volume (Ve) while Δ[Ton] represents the fraction solute gain over body water (V)[1,16]. The relationship between Δ[Ton] and Δ[Glu]S can be visualized as follows: At first approximation the amount of glucose gained, expressed in mmol or mOsm, and the amount of total solute gained are equal, or: Δ[Ton] × V = Δ[Glu]S× Ve (4).
Division of both sides of equation 4 by Δ[Glu]S× V reveals: Δ[Ton]/Δ[Glu]S = Ve/V (5).
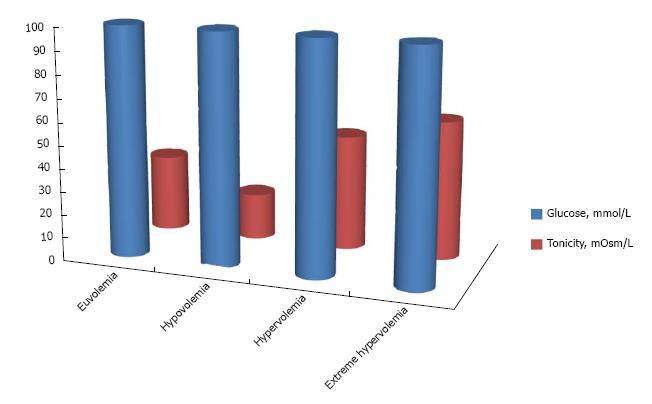
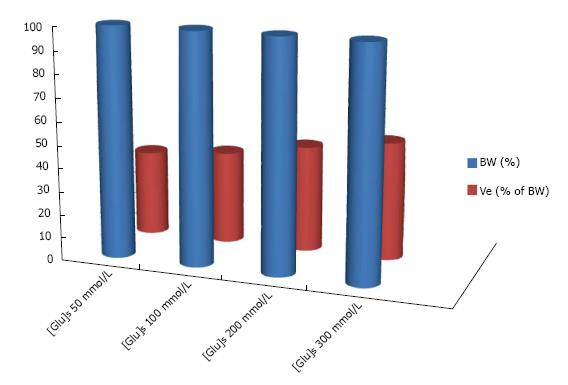
Equation 5 is the key to understanding the internal factors that affect the rise in tonicity in hyperglycemia. Extracellular volume status influences the degree of hypertonicity in hyperglycemic episodes[50,51]. Figure 4 shows examples of Δ[Ton] at the same Δ[Glu]S (100 mmol/L or 1800 mg/dL) in euvolemia, hypovolemia, hypervolemia and extreme hypervolemia. In euvolemia, extracellular volume is approximately one-third of body water and, therefore, the fraction Δ[Ton]/Δ[Glu]S should be around 0.33. Δ[Ton]/Δ[Glu]S values lower than 0.33 should be encountered in hypovolemia and values higher than 0.33 should be encountered in hypervolemia[50-52].
The degree of hyperglycemia is another factor potentially influencing the relationship between Δ[Ton] and Δ[Glu]S. Robin and collaborators calculated a progressive rise of the value ΔTon/Δ[Glu]S as [Glu]S increases progressively[53]. The effect of hyperglycemia on Δ[Ton] is mediated by the commensurate increase in extracellular volume, which increases progressively, while intracellular volume decreases by the same volume as [Glu]S increases, if external losses of water and solute are negligible[52]. Figure 5 shows calculations of the extracellular fraction of body water in various degrees of hyperglycemia. The degree of hyperglycemia that can be expected to have clinically relevant effects on the rise in tonicity is extreme[52].
Δ[Ton] values lower than the corresponding Δ[Glu]S values are obtained in hyperglycemia because of the osmotic translocation of intracellular fluid into the extracellular compartment secondary to extracellular solute (glucose) gain. The net osmotic fluid shift stops when intracellular osmolality, which is increasing with the loss of intracellular fluid, becomes equal to the extracellular osmolality, which is decreasing with the extracellular gain of fluid. The attenuation of the rise in extracellular osmolality secondary to the internal osmotic fluid shift is expressed as a decrease in [Na]S. In this case, Δ[Ton] is the algebraic sum of the rise in serum glucose concentration (Δ[Glu]S) and the decrease in serum sodium salt concentration (2 × [Na]S). Therefore: Δ[Ton] = Δ[Glu]S - 2 × [Na]S (6).
where [Na]S is the baseline euglycemic [Na]S minus the hyperglycemic [Na]S. Thus the effect of the various internal factors affecting the rise in tonicity for any given rise in [Glu]S is mediated through the decrease in [Na]S. The decrease in [Na]S caused by hyperglycemia, therefore, becomes an important part of the calculations of the tonicity of the replacement solutions.
The decrease in [Na]S as a result of osmotic fluid addition to the extracellular compartment during development of hyperglycemia should be equal to the increase in [Na]S after correction of hyperglycemia when there are no other influences on [Na]S. Estimating the drop in [Na]S for a given rise in [Glu]S and therefore predicting the rise in [Na]S after correction of the hyperglycemia has important therapeutic implications. The effects of internal osmotic fluid transfers on [Na]S will be reversed with correction of hyperglycemia without the need for additional interventions. These effects should be differentiated from the effects of other processes affecting [Na]S routinely in severe hyperglycemic episodes because these other influences on [Na]S require additional therapeutic measures[20,54]. The Katz formula, which calculates only the effects of the internal osmotic fluid shift resulting from hyperglycemia, predicts a decrease in [Na]S by 1.6 mmol/L for each 100 mg/dL (5.6 mmol/L) increase in [Glu]S[55]. Using formula 6, the fraction Δ[Ton]/Δ[Glu]S predicted by the Katz formula is equal to 0.43[49]. This fraction, which represents a modest degree of hypervolemia (Figure 2), reflects the extracellular expansion that results from the internal osmotic fluid shift during development of hyperglycemia[56].
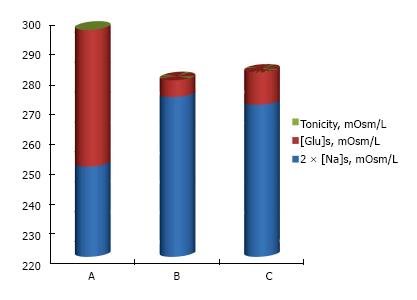
Clinical evaluation of the Katz formula is complicated by the indirect effects of hyperglycemia on serum tonicity[54]. Hyperglycemia in oligoanuric patients allows the study of this formula with minimal interference from these indirect effects. Studies of Δ[Ton]/Δ[Glu]S in hyperglycemic patients on chronic dialysis observed mean Δ[Ton]/Δ[Glu]S values very close to 0.43[56,57]. Figure 6 shows the mean changes in tonicity predicted by the Katz formula and observed in severe hyperglycemic episodes in patients on chronic dialysis treated with insulin infusion and no other interventions[56]. Predicted and observed Δ[Ton]/Δ[Glu]S values were close.
High Δ[Ton]/Δ[Glu]S values were observed during treatment of hyperglycemia only in a small number of dialysis patients with profound hypervolemia[56]. The relationship Δ[Ton]/Δ[Glu]S during treatment of severe hyperglycemic episodes in patients on dialysis with insulin infusion and no other measures was used to evaluate the state of extracellular volume in one study[58]. In this study, the observed Δ[Ton]/Δ[Glu]S values allowed proper characterization of the volume status in a small number of patients with pronounced edema and a larger number of subjects whose body weight was close to their dry weight[58]. We did not find any reports documenting the effect of the degree of hyperglycemia on Δ[Ton]/Δ[Glu]S. We suggest that the Katz formula can be expected to predict with reasonable accuracy the value of Δ[Ton]/Δ[Glu]S that results from the direct effect of correction of hyperglycemia in patients with absence of severe hypervolemia. Application of the Katz formula in the prediction of the change in tonicity secondary to correction of hyperglycemia in patients with severe volume disturbances will require special caution[49,56].
In addition to its hypertonic effect from accumulation of glucose in extracellular fluids, hyperglycemia has two other indirect influences on tonicity. The first indirect effect of hyperglycemia is the result of osmotic diuresis secondary to glucosuria. Osmotic diuresis in severe or protracted hyperglycemia can be massive and leads to water losses in excess of monovalent cation losses[20,21]. Loss of water in excess of the losses of potassium and sodium leads to elevation in [Na]S[21] which in several studies analyzing severe hyperglycemic episodes was within the normal range or even in the hypernatremic range in the face of profound hyperglycemia[21,56].
The second indirect effect of hyperglycemia is fluid intake secondary to thirst. Hyperglycemia causes a lesser degree of thirst than hypernatremia causing similar levels of hypertonicity[16]. Water gain secondary to thirst and fluid intake during development of hyperglycemia is not enough to compensate for the water loss through osmotic diuresis in severe cases of hyperglycemia. Hyperglycemic patients with oligoanuria develop minimal or no osmotic diuresis. In the absence of any other change in solute and water balance in these patients, water intake driven by hyperglycemic thirst should lead to hyponatremia after correction of hyperglycemia even though [Na]S rises as [Glu]S decreases[49]. Hyponatremia after correction of severe hyperglycemia with insulin infusion and no other interventions was documented in approximately one third of the cases in patients on chronic dialysis[59].
In addition to correction of hyperglycemia and ketoacidosis, when present, the treatment of hyperglycemic crises addresses the critical areas of hypovolemia, potassium deficit and hypertonicity plus less frequently other deficits, e.g., deficits of phosphate or magnesium[49,60]. Current guidelines address all these disturbances of hyperglycemic crises[48]. This report will focus on the management of hyperglycemic hypertonicity.
Hyperglycemic hypertonicity has two components, gain in solute secondary to the rise in [Glu]S and excessive loss of water over sodium and potassium secondary to hyperglycemic osmotic diuresis. The second component represents a relatively small part of hypertonicity in reported series of diabetic ketoacidosis and the major component of hypertonicity in reported series of hyperosmolar hyperglycemic syndrome[56]. The management of hyperglycemic hypertonicity requires setting of specific targets for each one of these two components. Correction of hyperglycemia without any other change in body water or solute leads to loss of extracellular solute and decrease in tonicity[61,62].
Calculation of the degree of hypertonicity secondary to osmotic diuresis is obscured for the duration of hyperglycemia by the effect of elevated [Glu]S on [Na]S levels. The calculation of the corrected [Na]S by Al-Kudsi and collaborators[63] provides a valuable tool allowing quantitative evaluation of the component of hyperglycemic hypertonicity that results from osmotic diuresis[64,65]. The corrected [Na]S uses Katz’s formula to compute the value of [Na]S that would result from correction of the hyperglycemia if there are no changes in the balances of water, sodium and potassium, as follows[63]:
Corrected [Na]S = [Na]S1 + 1.6 × ([Glu]S1 -100)100 (7).
where [Na]S1 and [Glu]S1 are respectively the sodium and glucose concentrations at hyperglycemia. [Glu]S1 is expressed in mg/dL in formula 7. Both [Glu]S and corrected [Na]S are treatment targets of hyperglycemic hypertonicity.
As in hypernatremia, rapid correction of hypertonicity has the risk of causing cerebral edema in hyperglycemia[66]. The decrease in tonicity during correction of hyperglycemia should not exceed 3 mOsm/L per hour[67]. The hourly rate of decrease in [Glu]S proposed in guidelines is 50-75 mg/dL or 2.8-4.2 mmol/L[67]. At this rate of decline in [Glu]S, the rate of decline in tonicity will be 1.2-1.8 mOsm/L if [Na]S rises concomitantly at the rate predicted by the Katz formula[49]. If this rate of decline in [Glu]S is achieved, the proposed maximal hourly rate of decline in the corrected [Na]S is 0.6-0.9 mmol/L[49]. The corrected [Na]S should be computed after each measurement of serum chemistries and its value should be used as [Na]S1 in the calculation of the infused volume of hypotonic fluids by equation 2. In this way, the corrected [Na]S is used in the same manner as the serum sodium concentration during treatment of hypernatremia. The treatment should aim to a continuous decrease in corrected [Na]S as long as its values remain elevated.
The management of hypertonicity in severe hyperglycemia encounters even greater difficulties than its management in severe hypernatremia. In hyperglycemic crises water, sodium and potassium deficits are routinely large and can be massive. Their severity may draw attention away from hypertonicity[49]. In addition, the calculation of corrected [Na]S with the use of the Katz formula adds another degree of uncertainty. As noted, the value Δ[Ton]/Δ[Glu]S receives a significant influence from the relationship between extracellular volume and body water, which is subjected to great variation in hyperglycemia. Finally, osmotic diuresis persists as long as [Glu]S remains elevated and may even increase when volume deficits are replaced and renal function is restored causing large losses of water and electrolytes during treatment of hyperglycemia[49]. For these reasons, the need to monitor the clinical status of the patient, serum chemistries and urinary losses is, if anything, even more important during treatment of severe hyperglycemia than during treatment of hypernatremia.
Hypertonicity secondary to hypernatremia or hyperglycemia is the source of life-threatening clinical manifestations and its treatment provides great challenges to clinicians. Equations calculating the fluid and electrolyte deficits are of help in the prescription of hypertonicity treatment and in following its results. Comparison of observed and predicted by these equations changes should be used to detect and correct potential errors in the calculations from the predictive equations (e.g., body water estimates) and problems caused by large fluid losses during treatment. Close monitoring during treatment of clinical status, appropriate serum chemistries and external losses of fluid and monovalent cations is a critical step. Adjustment of treatment guided by the findings in each monitoring step is essential for successful outcomes.
The authors appreciate the research service of the Raymond G. Murphy VA Medical Center.
Manuscript source: Invited manuscript
Specialty type: Urology and nephrology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A, A, A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Eirini G, Nechifor G, Ohashi N, Yorioka N S- Editor: Kong JX L- Editor: A E- Editor: Lu YJ
| 1. | Argyropoulos C, Rondon-Berrios H, Raj DS, Malhotra D, Agaba EI, Rohrscheib M, Khitan Z, Murata GH, Shapiro JI, Tzamaloukas AH. Hypertonicity: Pathophysiologic Concept and Experimental Studies. Cureus. 2016;8:e596. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Mohmand HK, Issa D, Ahmad Z, Cappuccio JD, Kouides RW, Sterns RH. Hypertonic saline for hyponatremia: risk of inadvertent overcorrection. Clin J Am Soc Nephrol. 2007;2:1110-1117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 123] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 3. | Lien YH, Shapiro JI, Chan L. Study of brain electrolytes and organic osmolytes during correction of chronic hyponatremia. Implications for the pathogenesis of central pontine myelinolysis. J Clin Invest. 1991;88:303-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 187] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 4. | Soupart A, Stenuit A, Perier O, Decaux G. Limits of brain tolerance to daily increments in serum sodium in chronically hyponatraemic rats treated with hypertonic saline or urea: advantages of urea. Clin Sci (Lond). 1991;80:77-84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Verbalis JG, Gullans SR. Rapid correction of hyponatremia produces differential effects on brain osmolyte and electrolyte reaccumulation in rats. Brain Res. 1993;606:19-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 62] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 6. | Burg MB, Ferraris JD. Intracellular organic osmolytes: function and regulation. J Biol Chem. 2008;283:7309-7313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Finberg L. Pathogenesis of lesions in the nervous system in hypernatremic states. I. Clinical ovservations of infants. Pediatrics. 1959;23:40-45. [PubMed] |
| 8. | Finberg L, Luttrell C, Redd H. Pathogenesis of lesions in the nervous system in hypernatremic states. II. Experimental studies of gross anatomic changes and alterations of chemical composition of the tissues. Pediatrics. 1959;23:46-53. [PubMed] |
| 9. | Snyder NA, Arieff AI. Neurologic manifestations of hypernatremia. Metabolic Brain Dysfunction in Systemic Disorders. In: AI Arieff, RC Griggs editors. Boston: Little, Brown and Co. 1992; 87-106. |
| 10. | Kumar S, Berl T. Sodium. Lancet. 1998;352:220-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 259] [Cited by in RCA: 212] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 11. | Lipowski ZJ. Delirium: Acute Confusional States. New York: Oxford University Press 1990; 308-356. |
| 12. | Macaulay D, Watson M. Hypernatraemia in infants as a cause of brain damage. Arch Dis Child. 1967;42:485-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 86] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Snyder NA, Feigal DW, Arieff AI. Hypernatremia in elderly patients. A heterogeneous, morbid, and iatrogenic entity. Ann Intern Med. 1987;107:309-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 162] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 14. | Rondon-Berrios H, Agaba EI, Tzamaloukas AH. Hyponatremia: pathophysiology, classification, manifestations and management. Int Urol Nephrol. 2014;46:2153-2165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 44] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Sam R, Feizi I. Understanding hypernatremia. Am J Nephrol. 2012;36:97-104. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Feig PU, McCurdy DK. The hypertonic state. N Engl J Med. 1977;297:1444-1454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Gennari FJ. Current concepts. Serum osmolality. Uses and limitations. N Engl J Med. 1984;310:102-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 169] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 18. | Adrogué HJ, Madias NE. Hypernatremia. N Engl J Med. 2000;342:1493-1499. [PubMed] [DOI] [Full Text] |
| 19. | Goldwasser P, Ayoub I, Barth RH. Pseudohypernatremia and pseudohyponatremia: a linear correction. Nephrol Dial Transplant. 2015;30:252-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 20. | McCurdy DK. Hyperosmolar hyperglycemic nonketotic diabetic coma. Med Clin North Am. 1970;54:683-699. [PubMed] |
| 21. | Arieff AI, Carroll HJ. Nonketotic hyperosmolar coma with hyperglycemia: clinical features, pathophysiology, renal function, acid-base balance, plasma-cerebrospinal fluid equilibria and the effects of therapy in 37 cases. Medicine (Baltimore). 1972;51:73-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 164] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 22. | Kapsner CO, Tzamaloukas AH. Understanding serum electrolytes. How to avoid mistakes. Postgrad Med. 1991;90:151-154, 157, 158, 161. [PubMed] |
| 23. | Arampatzis S, Frauchiger B, Fiedler GM, Leichtle AB, Buhl D, Schwarz C, Funk GC, Zimmermann H, Exadaktylos AK, Lindner G. Characteristics, symptoms, and outcome of severe dysnatremias present on hospital admission. Am J Med. 2012;125:1125.e1-1125.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 94] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 24. | Edelman IS, Leibman J, O’Meara MP, Birkenfeld LW. Interrelations between serum sodium concentration, serum osmolarity and total exchangeable sodium, total exchangeable potassium and total body water. J Clin Invest. 1958;37:1236-1256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 388] [Cited by in RCA: 375] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 25. | Adrogué HJ, Madias NE. Hyponatremia. N Engl J Med. 2000;342:1581-1589. [PubMed] [DOI] [Full Text] |
| 26. | Lien YH, Shapiro JI. Hyponatremia: clinical diagnosis and management. Am J Med. 2007;120:653-658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 76] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 27. | Welt LG, Seldin DW, Nelson WP, German WJ, Peters JP. Role of the central nervous system in metabolism of electrolytes and water. AMA Arch Intern Med. 1952;90:355-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 28. | Fitzsimons JT. Drinking by nephrectomized rats injected with various substances. J Physiol. 1961;155:563-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 29. | Moll FC, Skinner AL. Hypernatremia accompanying infant diarrhea. AMA J Dis Child. 1956;92:562-575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 30. | Ahmed I, Agusto-Odutola TB. Hypernatraemia in diarrhoeal infants in Lagos. Arch Dis Child. 1970;45:97-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 31. | Gennari FJ, Weise WJ. Acid-base disturbances in gastrointestinal disease. Clin J Am Soc Nephrol. 2008;3:1861-1868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 32. | Agaba EI, Rohrscheib M, Tzamaloukas AH. The renal concentrating mechanism and the clinical consequences of its loss. Niger Med J. 2012;53:109-115. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 33. | Leehey DJ, Daugirdas JT, Manahan FJ, Kellner KJ, Ing TS. Prolonged hypernatremia associated with azotemia and hyponatriuria. Am J Med. 1989;86:494-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 34. | Popli S, Tzamaloukas AH, Ing TS. Osmotic diuresis-induced hypernatremia: better explained by solute-free water clearance or electrolyte-free water clearance? Int Urol Nephrol. 2014;46:207-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 35. | Ellis RJ. Severe hypernatremia from sea water ingestion during near-drowning in a hurricane. West J Med. 1997;167:430-433. [PubMed] |
| 36. | Carlberg DJ, Borek HA, Syverud SA, Holstege CP. Survival of acute hypernatremia due to massive soy sauce ingestion. J Emerg Med. 2013;45:228-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 37. | Kim SW. Hypernatemia : successful treatment. Electrolyte Blood Press. 2006;4:66-71. [PubMed] [DOI] [Full Text] |
| 38. | Kahn T. Hypernatremia with edema. Arch Intern Med. 1999;159:93-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 39. | Milionis HJ, Liamis G, Elisaf MS. Hypernatremia in hospitalized patients: a sequel of inadvertent fluid administration. Arch Intern Med. 2000;160:1541-1542. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 40. | Sarahian S, Pouria MM, Ing TS, Sam R. Hypervolemic hypernatremia is the most common type of hypernatremia in the intensive care unit. Int Urol Nephrol. 2015;47:1817-1821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 41. | Watson PE, Watson ID, Batt RD. Total body water volumes for adult males and females estimated from simple anthropometric measurements. Am J Clin Nutr. 1980;33:27-39. [PubMed] |
| 42. | Mellits ED, Cheek DB. The assessment of body water and fatness from infancy to adulthood. Monogr Soc Res Child Dev. 1970;35:12-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 106] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 43. | Tzamaloukas AH. Effect of edema on urea kinetic studies in peritoneal dialysis patients. Perit Dial Int. 1994;14:398-401. [PubMed] |
| 44. | Tzamaloukas AH, Malhotra D, Rosen BH, Raj DS, Murata GH, Shapiro JI. Principles of management of severe hyponatremia. J Am Heart Assoc. 2013;2:e005199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 36] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 45. | Pazmiño PA, Pazmiño BP. Treatment of acute hypernatremia with hemodialysis. Am J Nephrol. 1993;13:260-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 46. | Nur S, Khan Y, Nur S, Boroujerdi H. Hypernatremia: correction rate and hemodialysis. Case Rep Med. 2014;2014:736073. [PubMed] |
| 47. | el-Dahr S, Gomez RA, Campbell FG, Chevalier RL. Rapid correction of acute salt poisoning by peritoneal dialysis. Pediatr Nephrol. 1987;1:602-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 48. | Kitabchi AE, Umpierrez GE, Miles JM, Fisher JN. Hyperglycemic crises in adult patients with diabetes. Diabetes Care. 2009;32:1335-1343. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1090] [Cited by in RCA: 1181] [Article Influence: 73.8] [Reference Citation Analysis (3)] |
| 49. | Tzamaloukas AH, Sun Y, Konstantinov NK, Ing TS, Dorin RI, Malhotra D, Murata GH, Shapiro JI. Principles of quantitative fluid and cation replacement in extreme hyperglycemia. Cureus. 2013;5:3110. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 50. | Moran SM, Jamison RL. The variable hyponatremic response to hyperglycemia. West J Med. 1985;142:49-53. [PubMed] |
| 51. | Tzamaloukas AH, Kyner WT, Galey WR. Determinants of osmotic phenomena created by an isolated change in extracellular solute in anuria. Miner Electrolyte Metab. 1987;13:117-125. [PubMed] |
| 52. | Tzamaloukas AH, Ing TS, Siamopoulos KC, Rohrscheib M, Elisaf MS, Raj DS, Murata GH. Body fluid abnormalities in severe hyperglycemia in patients on chronic dialysis: theoretical analysis. J Diabetes Complications. 2007;21:374-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 53. | Robin AP, Ing TS, Lancaster GA, Soung LS, Sparagana M, Geis WP, Hano JE. Hyperglycemia-induced hyponatremia: a fresh look. Clin Chem. 1979;25:496-497. [PubMed] |
| 54. | Rohrscheib M, Rondon-Berrios H, Argyropoulos C, Glew RH, Murata GH, Tzamaloukas AH. Indices of serum tonicity in clinical practice. Am J Med Sci. 2015;349:537-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 55. | Katz MA. Hyperglycemia-induced hyponatremia--calculation of expected serum sodium depression. N Engl J Med. 1973;289:843-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 352] [Cited by in RCA: 316] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 56. | Tzamaloukas AH, Ing TS, Siamopoulos KC, Rohrscheib M, Elisaf MS, Raj DS, Murata GH. Body fluid abnormalities in severe hyperglycemia in patients on chronic dialysis: review of published reports. J Diabetes Complications. 2008;22:29-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 57. | Penne EL, Thijssen S, Raimann JG, Levin NW, Kotanko P. Correction of serum sodium for glucose concentration in hemodialysis patients with poor glucose control. Diabetes Care. 2010;33:e91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 58. | Tzamaloukas AH. Characterization of the state of body fluids in anuric hyperglycemic humans. Miner Electrolyte Metab. 1987;13:126-132. [PubMed] |
| 59. | Tzamaloukas AH, Rohrscheib M, Ing TS, Siamopoulos KC, Elisaf MF, Spalding CT. Serum tonicity, extracellular volume and clinical manifestations in symptomatic dialysis-associated hyperglycemia treated only with insulin. Int J Artif Organs. 2004;27:751-758. [PubMed] |
| 60. | Konstantinov NK, Rohrscheib M, Agaba EI, Dorin RI, Murata GH, Tzamaloukas AH. Respiratory failure in diabetic ketoacidosis. World J Diabetes. 2015;6:1009-1023. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (2)] |
| 61. | Tomkins AM, Dormandy TL. Osmolal pattern during recovery from diabetic coma. Lancet. 1971;2:952-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 62. | Tzamaloukas AH, Levinstone AR, Gardner KD. Hyperglycemia in advanced renal failure: sodium and water metabolism. Nephron. 1982;31:40-44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 63. | Al-Kudsi RR, Daugirdas JT, Ing TS, Kheirbek AO, Popli S, Hano JE, Gandhi VC. Extreme hyperglycemia in dialysis patients. Clin Nephrol. 1982;17:228-231. [PubMed] |
| 64. | Liamis G, Gianoutsos C, Elisaf MS. Hyperosmolar nonketotic syndrome with hypernatremia: how can we monitor treatment? Diabetes Metab. 2000;26:403-405. [PubMed] |
| 65. | Milionis HJ, Liamis G, Elisaf MS. Appropriate treatment of hypernatraemia in diabetic hyperglycaemic hyperosmolar syndrome. J Intern Med. 2001;249:273-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 66. | Maccario M. Neurological dysfunction associated with nonketotic hyperglycemia. Arch Neurol. 1968;19:525-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 77] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 67. | Kitabchi AE, Umpierrez GE, Murphy MB, Kreisberg RA. Hyperglycemic crises in adult patients with diabetes: a consensus statement from the American Diabetes Association. Diabetes Care. 2006;29:2739-2748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 315] [Cited by in RCA: 289] [Article Influence: 15.2] [Reference Citation Analysis (1)] |