Published online Sep 22, 2015. doi: 10.5498/wjp.v5.i3.255
Peer-review started: March 12, 2015
First decision: May 13, 2015
Revised: June 30, 2015
Accepted: September 1, 2015
Article in press: September 2, 2015
Published online: September 22, 2015
Processing time: 201 Days and 16.7 Hours
Suicide risk constitutes a complex set of interacting demographic, clinical, psychobiological and environmental variables. Impulsivity is a long-known risk factor for suicide attempts. However, research based on clearer conceptual refinement in this area is imperative. One emerging field of study is that of decision-making. Impulsivity involves a failure of higher-order control, including decision-making. Using standardized operational definitions that take into consideration relevant aspects of impulsivity, including state- and trait-components and a deeper understanding of the process of decision-making in the suicidal mind, we may come a step closer to understanding suicidality and winning the fight in this scourge of human suffering.
Core tip: Impulsivity is a long-known risk factor for suicide attempts. Impulsivity involves a failure of higher-order control, including decision-making. Thus, decision-making may be particularly pertinent to suicidal behavior. Deficits in decision-making may impair people’s ability to resolve problems and dilemmas and thus create an accumulation of stressors leading to further pain. These may give rise to risky choices such as self- harm or suicide behaviors.
- Citation: Gvion Y, Levi-Belz Y, Hadlaczky G, Apter A. On the role of impulsivity and decision-making in suicidal behavior. World J Psychiatr 2015; 5(3): 255-259
- URL: https://www.wjgnet.com/2220-3206/full/v5/i3/255.htm
- DOI: https://dx.doi.org/10.5498/wjp.v5.i3.255
Suicide is a leading cause of death worldwide and accounts for 1.5% of all deaths in developed countries[1]. Unfortunately, despite increased prevention efforts, suicide rates over the past several decades have remained high and thus the question of what causes a person to commit suicide, remains one of the central issues in psychiatry.
Suicide risk constitutes a complex set of interacting demographic, clinical, psychobiological and environmental variables[1-3]. To reduce death from suicide, the field needs to better understand the causes of suicide and suicide related behaviors and its correlates.
Suicidal behavior is a continuum with various terms incorporated in it, including deliberate self-harm, suicide attempts and eventually completed suicide. Moreover, there is also diversity in suicide attempts, mainly between violent and nonviolent failed attempts. However, the main difference in the literature is the one between suicide ideation from the one hand and suicide attempts from the other hand.
Klonsky et al[4] already suggested that one reason for the limited progress in suicide prevention might be a lack of knowledge about the transition from suicidal ideation to suicidal actions. Most people who consider suicide do not necessarily put their thoughts into action. For example, data from the 2008 National Survey on Drug Use and Health show that although 3.7% of adults age 18 and older in the United States had thought about suicide, 1.0% had made plans to commit suicide, and only 0.5% had actually attempted suicide[5]. It is therefore critical to better delineate the differences between suicide ideators and suicide attempters, and to identify which ideators are at greatest risk of attempting suicide. This could greatly improve risk assessment[4] and prevention strategies.
Impulsivity, is a multidimensional concept that encompasses a broad range of behaviors that reflect poor planning, premature responding before considering consequences, sensation-seeking, risk-taking, an inability to inhibit responses, and preference for immediate over delayed rewards[6]. The difficulty to control one’s behavior is thought to stem from deficits in the self-regulation of affect, motivation arousal and deficits in working memory and higher order cognitive functions. This failure is connected to brain systems modulating behavioral inhibition[7].
Some studies have suggested aggressive-impulsive behavior as the underlying link between family history of suicide and new attempts by probands especially in youth[8-10]. The inheritance of suicidal behavior is probably linked to the predisposition to psychiatric disorders combined with the tendency an individual has towards aggressive-impulsive behaviors[11].
Impulsivity has been assumed to facilitate the transition from suicidal ideations to attempts[12] and has even been suggested to be “a more significant indicator of suicide attempt than the presence of a specific suicide plan p.195”[13]. Although the relationship between impulsivity and suicide behavior is well-established in the literature[8], empirical findings have failed to consistently distinguish between suicide ideators and attempters[12]. One possibility is that other factors skew the relationship between impulsivity and suicide behavior or that the problem lies in the definitions and measures of the concept of impulsivity.
The literature on impulsivity and its relationship to mental health is also somewhat confusing in part due to the use of different semantic and operational definitions of impulsivity across studies. In addition, the trait and state aspects of impulsivity are usually not delineated in suicide research. Thus, an important distinction is between the state and trait dimensions of the impulsivity-suicide relationship, that is, impulsivity of the attempt (state) and impulsivity of the attempter (trait). These may not completely overlap or be equivalent. It may thus be crucial to distinguish between a suicidal act that is impulsive (or not) and a person who can be impulsive or not[14]. Different studies have shown that although people who attempt suicide tend to be more impulsive than those who do not, the actual act of completed suicide is often not made impulsively[15,16]. Impulsive suicide attempts involve little or no preparation or premeditation while preparation and forethought precede non-impulsive suicide attempts[17]. Suicidal planning is related to, but not synonymous with, suicidal intent. Planned suicide is a more complicated construct that involves a more subjective element drawn from the desired outcome and perceived lethality of the act of self-harm[18].
Despite these methodological problems, both clinical experience and research highlight the importance of impulsivity in the understanding of suicide behavior[16]. Further research based on clearer conceptual refinements in this area is imperative. The emerging field of study of decision-making may shed light on this issue since impulsivity involves a failure in higher-order control, including decision-making.
Over the last five decades, economists have influenced the field of psychology and psychiatry by describing different components of decision-making in healthy populations. In their everyday lives, people are constantly exposed to huge amounts of information and to situations in which decisions have to be made on the basis of available information. These decisions (e.g., to buy a specific house) may then interact with external factors (such as the number of other bidders) to bring about outcomes. Together, the decisions and their outcomes essentially define our lives. Our brain screens, gathers and analyzes information before each decision, and makes an attempt to find an optimal solution (even if we are not always aware of the processes involved). Cognitive and affective neural systems have been implicated in this process[19]. Decision-making covers all decision related features, including reward learning[20]. Several studies have described a number of neural and behavioral components of human (and animal) decision-making processes that are central to healthy human decision-making. These include probabilistic cognition[21,22], causal inference[23] and logical reasoning[24]. Others have identified a number of heuristics and biases such as loss aversion and risk aversion[19], the availability bias, the gambler’s fallacy, the conjunction fallacy, etc[25].
Dombrovski et al[26] argue that suicide attempts are the result of a “suboptimal” decision. They claim that the tendency to make bad decisions might be one of the pathways to suicidal behavior. Several behavioral and neurological studies have explored the associations between suicidal behavior and decision-making. For example, in a cohort of 53 participants it was found that impulsivity and a history of suicide attempts (particularly poorly planned ones) were associated with a weakened expected reward signal in the paralimbic cortex[26]. Furthermore, higher suicidal intent and higher lethality suicide attempts have been associated with decreased activity in the VMPFC[27]. Post-mortem studies have also associated a damaged ventral prefrontal cortex with suicidal behavior[28]. Specifically, decreased grey matter volume in the OFC was reported in individuals with a history of suicide attempts as compared to non-suicidal patients[29] and healthy people[30]. In other studies, the same areas have been implicated in different facets of decision-making and impulsivity[31-34]. These neurophysiological similarities further suggest that decision-making and impulsivity may play an important role in suicidal behavior. Behavioral studies have also found correlations between suicide behavior, and behaviors defined as disadvantageous (such as drug addiction and gambling)[35,36]. Nevertheless, it remains unclear how studies involving decision-making tasks contribute to a better understanding of the behavioral mechanisms behind suicide attempts, and in particular specific personality dimensions including impulsivity. Garcia Espinosa et al[37], for example, showed that patients with temporal lobe epilepsy who exhibit executive dysfunction on behavioral tasks are at an elevated risk of attempting suicide, unlike self-reported impulsivity. Jollant et al[38] reported a difference in performance on the iowa gambling task (IGT) between violent and non-violent types of suicide attempters compared to control groups of healthy subjects and patients suffering from affective disorders. The Iowa Gambling Task scores in this study were not correlated with impulsivity[38]. Bridge et al[39] studied adolescent suicidal attempters and non-attempters and found that performance on the IGT was significantly worse for suicide attempters compared to non-attempters, although in the attempters group overall task performance did not correlate with different personality dimensions including impulsivity[39]. Westheide et al[40] found that suicidal ideation was associated with impaired decision-making on several executive tasks including the IGT and a go/no-go task. They also indicated that depressive suicide attempters had a state-dependent component of decision-making, derived from the fact that former suicide attempters who did not have suicide ideations at the time of the study performed noticeably better[40]. This state dependent process may also be related to cognitive load, in the same way as somatic pain affects performance on decision-making tasks[41]. The impact of continuous emotionally negative thoughts or psychological pain, may preoccupy cognitive resources, and thus lead to inferior judgments and decisions.
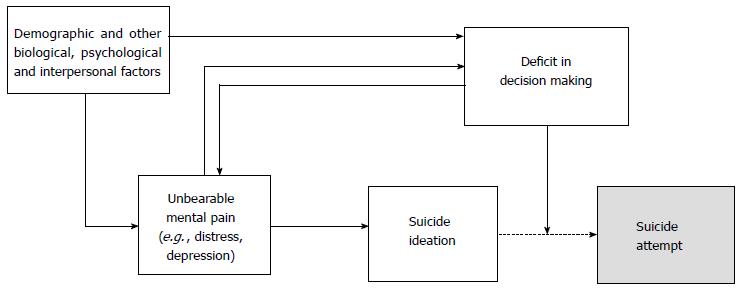
The relationship between poor decision-making and suicide attempts may thus unfold in the following way. People who are in agony and distress may see life as unceasing pain and suicide as an escape from unbearable punishment compared to any future rewards[26]. This way of thinking is analogous to Baumeister’s theory that views suicide as an escape from an aversive situation and an unbearable state of mind[42], as well as Shneidman’s concept of unbearable mental pain[43]. Along the same lines, Williams et al[44]’s entrapment theory views suicidal behavior as the instrumental result of a decision concerning two competing outcomes: a state of no suffering (through death), vs the state of an indefinite period of suffering (staying alive). Thus, decision-making may be particularly pertinent to suicidal behavior. Trait like deficits in decision-making may impair people’s ability to resolve problems and dilemmas and thus create an accumulation of stressors leading to further pain. These may give rise to risky choices such as self-harm or suicide behaviors. Deficits in decision-making may impair people’s ability to resolve problems and dilemmas and thus create an accumulation of stressors leading to further pain.
Figure 1 depicts this theoretical model of associating decision-making and suicidal behavior. The model is built on the well-known path that leads from unbearable mental pain to suicide through suicide ideation with different factors (demographic, biological, psychological and interpersonal) contributing to this path[45]. However, according to our model, unbearable mental pain also facilitates suicide attempts through changing decision making features, suggesting that at least some people who engage in suicidal behavior tend to overestimate the value of certain future outcomes and see suicide as attractive relative to other alternatives[46]. Yet, another direction of influence in our model is the effect of deficiencies in decision making, and the inability to accurately resolve problems on the level of mental pain, resulting in the increased risk of suicidal behavior.
Many factors influence suicidal behavior. Impulsivity and decision-making appear to be especially important in this context. The literature suggests that a better understanding of the principles of decision-making can contribute to a firmer grasp of the behavioral mechanisms behind suicide attempts, though the relationship to impulsivity remains unclear.
Standardized operational definitions that take the key features of impulsivity including state- and trait-components into account and a clearer understanding of the process of decision-making in the suicidal mind may bring practitioners a step closer to understanding suicidality and winning the battle against this form of human suffering.
P- Reviewer: Chakrabarti S, Yang YK S- Editor: Tian YL L- Editor: A E- Editor: Wu HL
| 1. | Hawton K, van Heeringen K. Suicide. Lancet. 2009;373:1372-1381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1310] [Cited by in RCA: 1289] [Article Influence: 80.6] [Reference Citation Analysis (0)] |
| 2. | Joshi HL, Parkash V, Kumar U. Conceptualizing suicidal behavior. Suicidal Behavior Underlying Dynamics. London and New York: Routledge 2015; 3-23. |
| 3. | Gvion Y, Apter A. Review on suicide behavior. Publ Health Rev. 2012;34:2. |
| 4. | Klonsky ED, May AM. Differentiating suicide attempters from suicide ideators: a critical frontier for suicidology research. Suicide Life Threat Behav. 2014;44:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 444] [Cited by in RCA: 497] [Article Influence: 45.2] [Reference Citation Analysis (0)] |
| 5. | The Substance Abuse and Mental Health Services Administration, National Survey on Drug Use and Health. [accessed 2008]. Available from: http://www.samhsa.gov/. |
| 6. | Whiteside SP, Lynam DR. The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. P. ersonality and Individual Differences. 2001;30:669-689. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2266] [Cited by in RCA: 2260] [Article Influence: 94.2] [Reference Citation Analysis (0)] |
| 7. | Mann JJ, Currier D. Biological predictors of suicidal behavior in mood disorders. In: Wasserman D, Wasserman C, editors. Oxford Textbook of Suicide Prevention. A Global Perspective. Oxford University Press 2009; 335-341. [DOI] [Full Text] |
| 8. | Brent DA, Melhem N. Familial transmission of suicidal behavior. Psychiatr Clin North Am. 2008;31:157-177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 233] [Cited by in RCA: 190] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 9. | Chachamovich E, Stefanello S, Botega N, Turecki G. Which are the recent clinical findings regarding the association between depression and suicide? Rev Bras Psiquiatr. 2009;31 Suppl 1:S18-S25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Diaconu G, Turecki G. Family history of suicidal behavior predicts impulsive-aggressive behavior levels in psychiatric outpatients. J Affect Disord. 2009;113:172-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Sarchiapone M, Iouse M. Genetics of suicidal behavior. Suicidal Behavior Underlying Dynamics. London and New York: Routledge 2015; 23-39. |
| 12. | Klonsky ED, May A. Rethinking impulsivity in suicide. Suicide Life Threat Behav. 2010;40:612-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 200] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 13. | Bryan CJ, Rudd MD. Advances in the assessment of suicide risk. J Clin Psychol. 2006;62:185-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 172] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 14. | Baca-Garcia E, Diaz-Sastre C, García Resa E, Blasco H, Braquehais Conesa D, Oquendo MA, Saiz-Ruiz J, de Leon J. Suicide attempts and impulsivity. Eur Arch Psychiatry Clin Neurosci. 2005;255:152-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 134] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 15. | Anestis MD, Selby EA, Joiner TE. The role of urgency in maladaptive behaviors. Behav Res Ther. 2007;45:3018-3029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 160] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 16. | Gvion Y, Apter A. Aggression, impulsivity, and suicide behavior: a review of the literature. Arch Suicide Res. 2011;15:93-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 264] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 17. | Conner KR. A call for research on planned vs. unplanned suicidal behavior. Suicide Life Threat Behav. 2004;34:89-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 68] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 18. | Beck AT, Schuyler D, Herman I. Development of suicidal intent scales. The prediction of suicide. Bowie, MD: Charles Press 1974; 45-56. |
| 19. | Rilling JK, Sanfey AG. The neuroscience of social decision-making. Annu Rev Psychol. 2011;62:23-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 441] [Cited by in RCA: 444] [Article Influence: 31.7] [Reference Citation Analysis (0)] |
| 20. | Kahneman D, Tversky A. Prospect Theory: An Analysis of Decision under Risk. Econometrica. 1979;47:263-291. [DOI] [Full Text] |
| 21. | Cosmides L, Tooby J. Are humans good intuitive satisfactions after all? Rethinking some conclusions from literature on judgment under uncertainty. Cognition. 1996;58:1-73. [RCA] [DOI] [Full Text] [Cited by in Crossref: 571] [Cited by in RCA: 347] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 22. | Huettel SA, Mack PB, McCarthy G. Perceiving patterns in random series: dynamic processing of sequence in prefrontal cortex. Nat Neurosci. 2002;5:485-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 225] [Cited by in RCA: 191] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 23. | Körding KP, Beierholm U, Ma WJ, Quartz S, Tenenbaum JB, Shams L. Causal inference in multisensory perception. PLoS One. 2007;2:e943. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 561] [Cited by in RCA: 621] [Article Influence: 34.5] [Reference Citation Analysis (0)] |
| 24. | Stollstorff M, Bean SE, Anderson LM, Devaney JM, Vaidya CJ. Rationality and emotionality: serotonin transporter genotype influences reasoning bias. Soc Cogn Affect Neurosci. 2013;8:404-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Tversky A, Kahneman D. Judgment under Uncertainty: Heuristics and Biases. Science. 1974;185:1124-1131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17249] [Cited by in RCA: 7218] [Article Influence: 481.2] [Reference Citation Analysis (0)] |
| 26. | Dombrovski AY, Szanto K, Clark L, Reynolds CF, Siegle GJ. Reward signals, attempted suicide, and impulsivity in late-life depression. JAMA Psychiatry. 2013;70:1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 137] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 27. | Oquendo MA, Placidi GP, Malone KM, Campbell C, Keilp J, Brodsky B, Kegeles LS, Cooper TB, Parsey RV, van Heertum RL. Positron emission tomography of regional brain metabolic responses to a serotonergic challenge and lethality of suicide attempts in major depression. Arch Gen Psychiatry. 2003;60:14-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 198] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 28. | Mann JJ, Huang YY, Underwood MD, Kassir SA, Oppenheim S, Kelly TM, Dwork AJ, Arango V. A serotonin transporter gene promoter polymorphism (5-HTTLPR) and prefrontal cortical binding in major depression and suicide. Arch Gen Psychiatry. 2000;57:729-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 414] [Cited by in RCA: 391] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 29. | Aguilar EJ, García-Martí G, Martí-Bonmatí L, Lull JJ, Moratal D, Escartí MJ, Robles M, González JC, Guillamón MI, Sanjuán J. Left orbitofrontal and superior temporal gyrus structural changes associated to suicidal behavior in patients with schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32:1673-1676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 76] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 30. | Monkul ES, Hatch JP, Nicoletti MA, Spence S, Brambilla P, Lacerda AL, Sassi RB, Mallinger AG, Keshavan MS, Soares JC. Fronto-limbic brain structures in suicidal and non-suicidal female patients with major depressive disorder. Mol Psychiatry. 2007;12:360-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 211] [Cited by in RCA: 220] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 31. | Tom SM, Fox CR, Trepel C, Poldrack RA. The neural basis of loss aversion in decision-making under risk. Science. 2007;315:515-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1026] [Cited by in RCA: 876] [Article Influence: 48.7] [Reference Citation Analysis (0)] |
| 32. | De Martino B, Camerer CF, Adolphs R. Amygdala damage eliminates monetary loss aversion. Proc Natl Acad Sci USA. 2010;107:3788-3792. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 329] [Cited by in RCA: 214] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 33. | Canessa N, Crespi C, Motterlini M, Baud-Bovy G, Chierchia G, Pantaleo G, Tettamanti M, Cappa SF. The functional and structural neural basis of individual differences in loss aversion. J Neurosci. 2013;33:14307-14317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 120] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 34. | Sokol-Hessner P, Camerer CF, Phelps EA. Emotion regulation reduces loss aversion and decreases amygdala responses to losses. Soc Cogn Affect Neurosci. 2013;8:341-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 150] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 35. | Wong PW, Cheung DY, Conner KR, Conwell Y, Yip PS. Gambling and completed suicide in Hong Kong: a review of coroner court files. Prim Care Companion J Clin Psychiatry. 2010;12:pii: PCC.09m00932. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 36. | Vijayakumar L, Kumar MS, Vijayakumar V. Substance use and suicide. Curr Opin Psychiatry. 2011;24:197-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 99] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 37. | Garcia Espinosa A, Andrade Machado R, Borges González S, García González ME, Pérez Montoto A, Toledo Sotomayor G. Wisconsin Card Sorting Test performance and impulsivity in patients with temporal lobe epilepsy: suicidal risk and suicide attempts. Epilepsy Behav. 2010;17:39-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 38. | Jollant F, Bellivier F, Leboyer M, Astruc B, Torres S, Verdier R, Castelnau D, Malafosse A, Courtet P. Impaired decision making in suicide attempters. Am J Psychiatry. 2005;162:304-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 356] [Cited by in RCA: 354] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 39. | Bridge JA, McBee-Strayer SM, Cannon EA, Sheftall AH, Reynolds B, Campo JV, Pajer KA, Barbe RP, Brent DA. Impaired decision making in adolescent suicide attempters. J Am Acad Child Adolesc Psychiatry. 2012;51:394-403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 87] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 40. | Westheide J, Quednow BB, Kuhn KU, Hoppe C, Cooper-Mahkorn D, Hawellek B, Eichler P, Maier W, Wagner M. Executive performance of depressed suicide attempters: the role of suicidal ideation. Eur Arch Psychiatry Clin Neurosci. 2008;258:414-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 140] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 41. | Apkarian AV, Sosa Y, Krauss BR, Thomas PS, Fredrickson BE, Levy RE, Harden RN, Chialvo DR. Chronic pain patients are impaired on an emotional decision-making task. Pain. 2004;108:129-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 358] [Cited by in RCA: 391] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 42. | Baumeister RF. Suicide as escape from self. Psychol Rev. 1990;97:90-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 987] [Cited by in RCA: 869] [Article Influence: 24.8] [Reference Citation Analysis (0)] |
| 43. | Shneidman ES. Suicide as psychache: A clinical approach to self-destructive behavior. Northvale, NJ: Jason Aronson 1993; . |
| 44. | Williams JMG, Crane C, Barnhofer T, Duggan D. Psychology and suicidal behaviour: elaborating the entrapment model. Prevention and Treatment of Suicidal Behaviour: From Science to Practice. New York: Oxford University Press 2005; 71-89. [DOI] [Full Text] |
| 45. | O’Connor RC. The integrated motivational-volitional model of suicidal behavior. Crisis. 2011;32:295-298. [PubMed] |
| 46. | Dombrovski AY, Clark L, Siegle GJ, Butters MA, Ichikawa N, Sahakian BJ, Szanto K. Reward/Punishment reversal learning in older suicide attempters. Am J Psychiatry. 2010;167:699-707. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 145] [Cited by in RCA: 121] [Article Influence: 8.1] [Reference Citation Analysis (0)] |