Published online Jul 19, 2025. doi: 10.5498/wjp.v15.i7.107130
Revised: April 25, 2025
Accepted: May 29, 2025
Published online: July 19, 2025
Processing time: 116 Days and 13.1 Hours
Atrial fibrillation (AF) is a very common tachyarrhythmia in clinical practice. Several risk factors, such as higher inflammatory marker levels, diabetes mellitus, hypertension, valvular disease, ischemic heart disease, heart failure, and obesity have been proposed to enhance the risk of AF, contributing to higher healthcare system utilization rates and socioeconomic costs. Some interesting studies also investigated the link between AF and psychiatric diseases. This article debates this link between AF and psychiatric diseases from the perspective of Ca2+/cAMP signaling.
Core Tip: Atrial fibrillation (AF) is recognized as one of the most frequently occurring tachyarrhythmias in clinical practice. This condition has been associated with an elevated risk of cardiovascular complications and increased mortality rates. Various contributing factors, including heightened levels of inflammatory markers, diabetes mellitus, hypertension, valvular disease, ischemic heart conditions, heart failure, and obesity, have been identified as potential influences on AF development. This article debates the link between AF and psychiatric diseases from the perspective of Ca2+/cAMP signaling.
- Citation: Bergantin LB. Debating the link between atrial fibrillation and psychiatric diseases through Ca2+/cAMP signaling. World J Psychiatry 2025; 15(7): 107130
- URL: https://www.wjgnet.com/2220-3206/full/v15/i7/107130.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i7.107130
Multiple studies have explored the connection between atrial fibrillation (AF) and mental health disorders[1-3]. AF is recognized as one of the most frequently occurring tachyarrhythmias in clinical practice[1]. This condition has been associated with an elevated risk of cardiovascular complications and increased mortality rates[1,2]. Various contributing factors, including heightened levels of inflammatory markers, diabetes mellitus, hypertension, valvular disease, ischemic heart conditions, heart failure, and obesity, have been identified as potential influences on AF development[4]. These risk factors further contribute to greater healthcare utilization and increased socioeconomic burdens[5]. This article debates this link between AF and psychiatric diseases from the perspective of Ca2+/cAMP signaling.
Interestingly, a study indicated a correlation between psychiatric conditions, such as depression and anxiety, and an increased likelihood of AF among individuals with diabetes[2]. Drawing from the Korea National Health Insurance Service database, researchers[2] included a cohort of 2512690 individuals diagnosed with diabetes who had no prior AF between 2009 and 2012. The study[2] examined the following five psychiatric conditions: expression, insomnia, anxiety, bipolar disorder, and schizophrenia. During the follow-up period, cases of newly diagnosed AF were identified, and a multivariate Cox regression analysis was conducted[2].
Another study[3] validated these findings indicating a higher occurrence of AF among individuals with psychiatric disorders, such as bipolar disorder and schizophrenia. Yang et al[3] analyzed data from the Taiwan National Health Insurance nationwide database to identify individuals diagnosed with bipolar disorder and schizophrenia, both with and without AF. The study examined a total of 927915 participants (463050 males and 464865 females) recorded between 2001 and 2008. Among them were 2963 (3.2%) individuals with schizophrenia (1650 males and 1313 females) and 5112 (5.5%) individuals diagnosed with bipolar disorder (1934 males and 3178 females)[3].
Several studies have examined the relationship between mental health disorders and the onset of AF. One multicenter cohort study[6] included 6644 patients in the United States, aged 45 to 84 years, who had no clinically recognized cardiovascular disease[6]. This study explored the association between depression and incident AF, revealing that depression increased the likelihood of developing AF by 34%[6]. Garg et al[6] concluded that depressive symptoms are associated with a heightened risk of AF. They also highlighted that their findings point to a significant segment of the American population that may face an elevated risk of AF and could benefit from targeted prevention strategies[6]. Additionally, another prospective cohort study[7] found that sleep disturbances predicted new-onset AF in both the Health eHeart Study and the Cardiovascular Health Study, with a median follow-up period of 11.6 years[7]. Christensen et al[7] concluded that sleep quality itself may be important in the pathogenesis of AF, potentially representing a novel target for prevention. These results are consistent with the findings already described in this article[2,3].
Several hypotheses suggest a potential link between AF and mental disorders. One such hypothesis involves neurotransmitters, such as dopamine, norepinephrine (NE), and serotonin, which have been recognized as contributing factors in the development of mental disorders[1]. Notably, elevated NE signaling outside the brain, indicative of sympathetic hyperactivity, has been observed in individuals with bipolar disorder and may play a role in the onset of AF[8]. Furthermore, research has identified abnormal autonomic nervous system activation in individuals with depression, specifically in the form of heightened sympathetic activity and diminished vagal regulation[9]. Interestingly, both depressive and hypertensive individuals exhibit sympathetic hyperactivity[9], suggesting a possible reciprocal influence between depression and hypertension. Additionally, autonomic nervous system imbalance, such as sympathetic hyperactivity, has been associated with the development of AF[10].
Our studies[9,11-15] provide valuable insights into this field. We have demonstrated that an imbalance in Ca2+ signaling is associated with sympathetic hyperactivity, which subsequently leads to hypertension, a factor that could also establish a connection between AF and mental disorders[9,12]. As previously mentioned, mental disorders such as depression and anxiety contribute to autonomic dysregulation, leading to increased catecholamine levels (sympathetic hyperactivity) and a diminished parasympathetic response[16]. Disruptions in autonomic tone, particularly sympathetic hyperactivity resulting from autonomic imbalance, have been linked to a greater occurrence of paroxysmal AF and the development of an arrhythmogenic environment in the atrium[16].
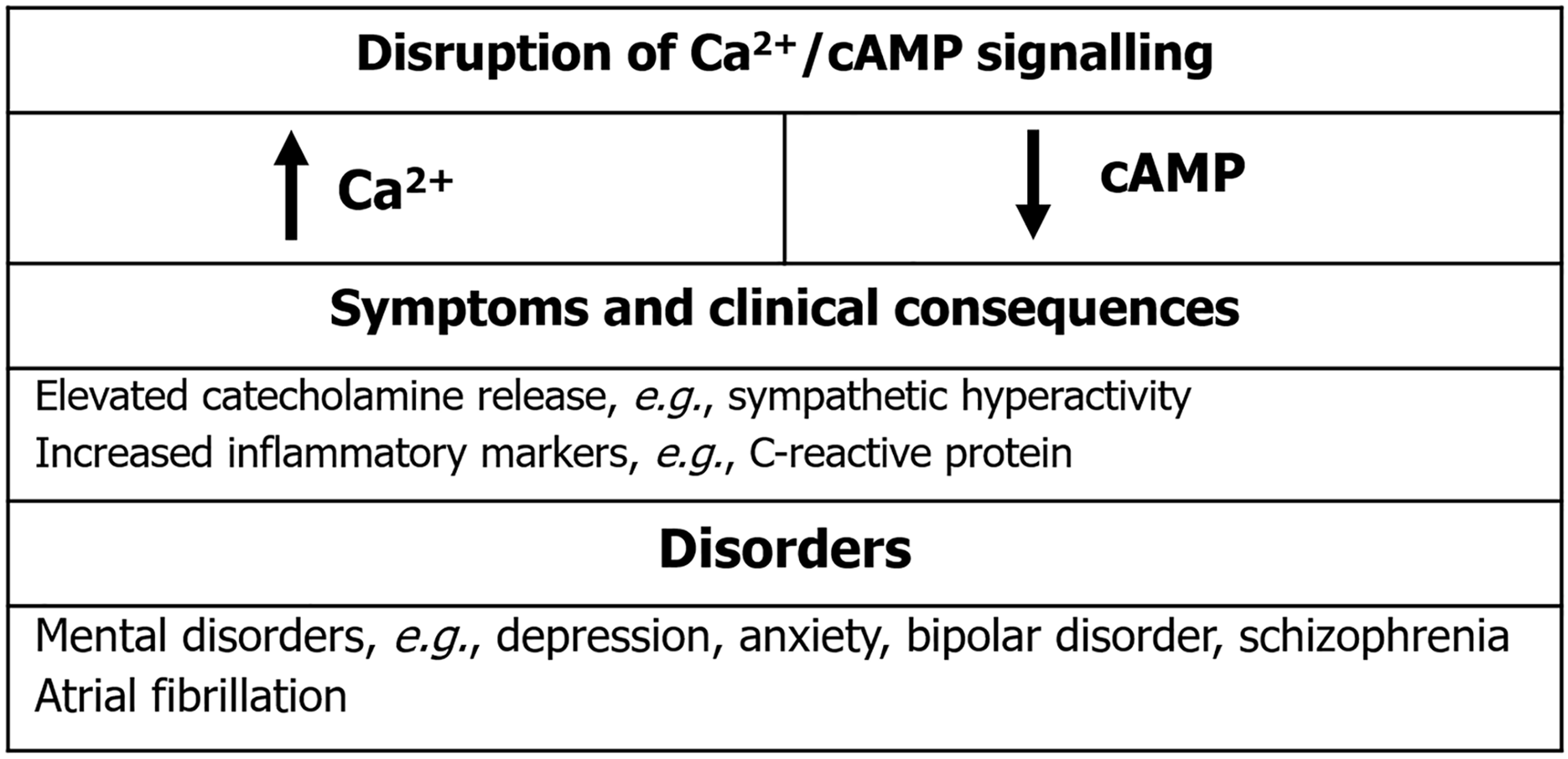
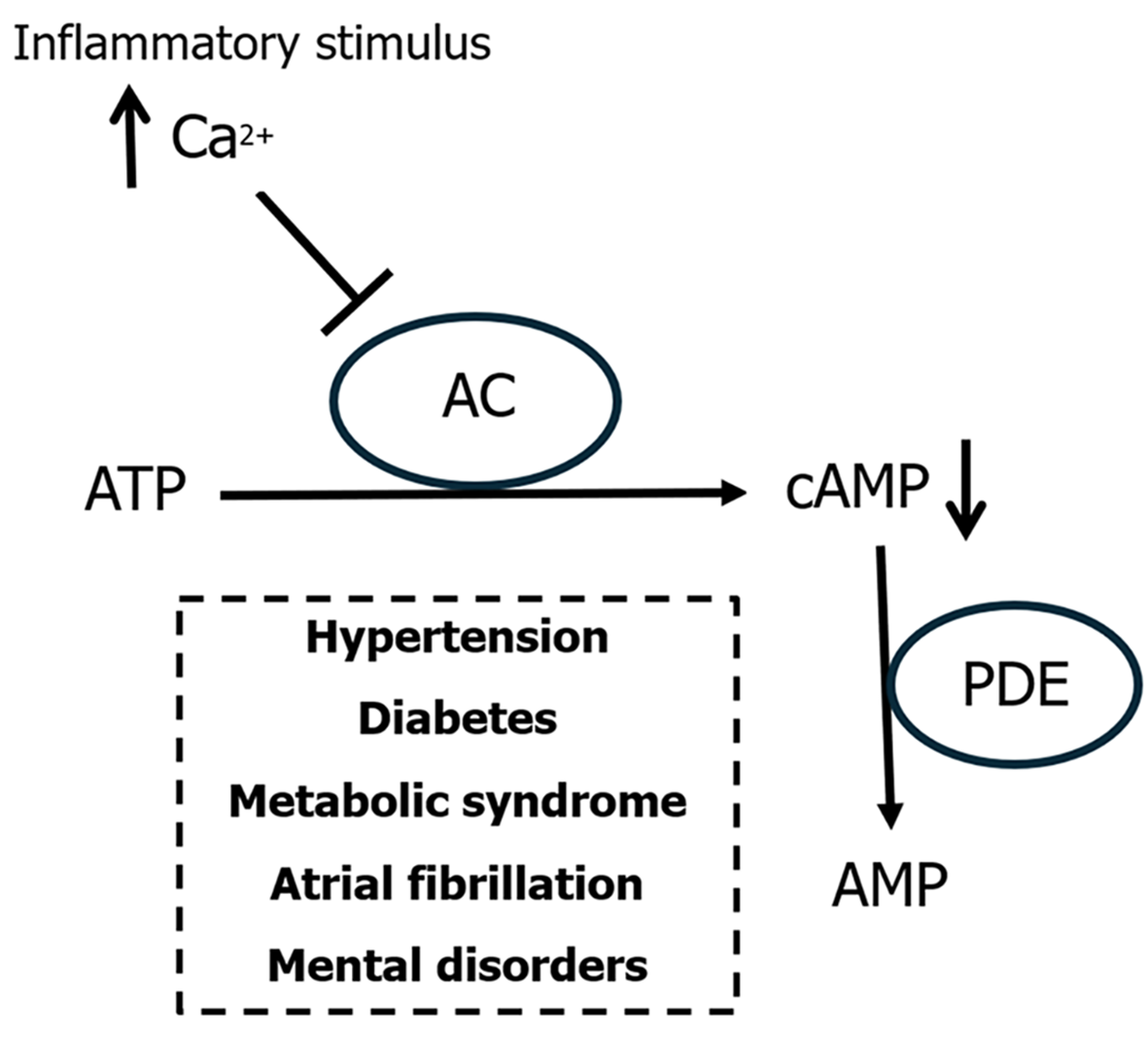
Additionally, inflammatory markers, such as C-reactive protein, which are often elevated in individuals with mental disorders[14], have also been associated with an increased risk of AF onset[17]. Our findings[11,14,15] reveal a strong relationship between Ca2+ signaling dysregulation and inflammation. Moreover, our studies[11-15] have established that higher cAMP concentrations can stimulate Ca2+ release from the endoplasmic reticulum, emphasizing the Ca2+/cAMP signaling interaction. Interestingly, increased Ca2+ levels can result in lower cAMP concentrations due to a negative feedback mechanism. Disruptions in this Ca2+/cAMP signaling dynamic may contribute to both mental disorders and AF[11,14,15]. Given that the interplay between these disorders may involve elevated Ca2+ concentrations[18-20], disturbances in Ca2+/cAMP signaling interactions become a plausible contributing factor. Supporting this hypothesis, research has detected cAMP signaling imbalances in the platelets of individuals with schizophrenia[18]. Further studies analyzing cerebrospinal fluid, blood platelets, and postmortem brain samples from schizophrenia patients have confirmed this dysregulation[18]. Similarly, disturbances in cAMP signaling have been observed in individuals with depression[9,19]. Figure 1 visually summarizes these findings.
Since the first Nobel Prize which was awarded for the discovery of cAMP in 1971[21], other Nobel prizes related to cAMP have been awarded[22,23], e.g., in 1992 and 1994. Furthermore, Nobel prizes related to Ca2+ have also been awarded[24-26]. Considering the relevance of this field for medicine and physiology, it would be plausible to speculate that more Nobel prizes related to cAMP and Ca2+ may be awarded in the near future. Within this field, Expertscape has ranked Dr. Leandro Bueno Bergantin as one of the leading experts on cAMP in the United States from 2013 to 2023. Specifically, Expertscape.com has recognized Dr. Bergantin as a "World Expert" in cAMP, placing him as the second-ranked global authority on the subject during this period (2013-23). This prestigious designation highlights his significant expertise, as Expertscape relies on data from the National Institute of Health’s PubMed database to objectively assess and rank physicians and researchers based on their contributions to specific topics. Additionally, Dr. Bergantin has been acknowledged by Expertscape as an "Expert" in Ca2+ from 2013 to 2023.
It has now become evident that a dysregulation of Ca2+/cAMP signaling[11-15,18-20] is implicated in the link between inflammatory diseases, e.g., depression and obesity, and an interesting report published in 2025 validated this conclusion, reinforcing the concept of an interplay between inflammatory diseases[27]. The report concluded that poor nutritional status was linked to neuropsychiatric symptom deterioration[27]. A diet lacking essential nutrients has been found to induce depression- and anxiety-like behaviors in APP/PS1 mice[27]. Specifically, malnutrition worsened neuropsychiatric symptoms linked to the cAMP signaling pathway within the midbrain and striatum[27]. The authors referenced our previous study[19], reinforcing our findings that dysregulation of the Ca2+/cAMP signaling pathway might serve as an initial mechanism connecting obesity and depression, potentially influencing neurotransmitter and hormone release and suggesting a relationship between nutritional status and neuropsychiatric conditions[19,27]. The study underscored that the aggravation of affective symptoms in APP/PS1 mice due to malnutrition was associated with downregulation of the cAMP signaling pathway in both the midbrain and striatum[27]. A reduction in cAMP/PKA signaling activity may disrupt neuronal excitation and impair synaptic plasticity, contributing to depression[19,27], whereas stimulation of the cAMP/PKA signaling pathway has been linked to rapid antidepressant effects[19,27]. Finally, this study[27] contributes to validating our unified theory[28] that connects inflammation and Ca2+/cAMP signaling. Indeed, these results have been validated by a longitudinal study that analyzed the link between serum Ca2+ levels and the incidence of inflammatory disorders, e.g., metabolic syndrome (MetS), diabetes, and hypertension[29]. This report[29] was performed through cross-sectional and longitudinal analyses (period 2010-2016). At baseline, there were 27364 patients in this analysis. Chou et al[29] concluded that higher serum Ca2+ levels were linked with an enhanced risk of inflammatory disorders, e.g., MetS, diabetes, and hypertension; thus, corroborating our findings and conclusions[11-15,18-20]. Diabetes, MetS and hypertension are considered independent risk factors for AF[30-32]. Figure 2 summarizes previous discussion.
In conclusion, it would be fascinating to analyze the Ca2+/cAMP ratio in clinical studies related to AF and mental disorders[33]. There is a well-established connection between Ca2+ signaling, such as intensified Ca2+ signals, and inflammatory responses. Additionally, cAMP plays a role in regulating anti-inflammatory mechanisms. It is concluded that both signaling pathways play a significant role in the link between AF and mental disorders, thus impacting the pharmacotherapy involving Ca2+ channel blockers and pharmaceuticals which increase the levels of cAMP. Finally, it is recommended that future research includes clinical trials or experimental studies. Such clinical validation would provide concrete evidence to support the hypotheses discussed in this article, and will enhance the credibility of this article for clinical application.
| 1. | Chung FP, Lin YJ. The Connection between Cardiac and Mental Disorder: Atrial Fibrillation in Patients with Psychiatric Disorder. Acta Cardiol Sin. 2014;30:53-55. [PubMed] |
| 2. | Bae NY, Lee SR, Choi EK, Ahn HJ, Ahn HJ, Kwon S, Han KD, Lee KN, Oh S, Lip GYH. Impact of mental disorders on the risk of atrial fibrillation in patients with diabetes mellitus: a nationwide population-based study. Cardiovasc Diabetol. 2022;21:251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 3. | Yang HY, Huang JH, Lin YK, Hsu CY, Chen SA, Chen YJ. Bipolar Disorder and Schizophrenia Present Different Risks of Atrial fibrillation: A Nationwide Population-Based Analysis. Acta Cardiol Sin. 2014;30:46-52. [PubMed] |
| 4. | Magnani JW, Rienstra M, Lin H, Sinner MF, Lubitz SA, McManus DD, Dupuis J, Ellinor PT, Benjamin EJ. Atrial fibrillation: current knowledge and future directions in epidemiology and genomics. Circulation. 2011;124:1982-1993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 212] [Article Influence: 17.7] [Reference Citation Analysis (0)] |
| 5. | Miyasaka Y, Barnes ME, Gersh BJ, Cha SS, Bailey KR, Seward JB, Tsang TS. Changing trends of hospital utilization in patients after their first episode of atrial fibrillation. Am J Cardiol. 2008;102:568-572. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Garg PK, O'Neal WT, Diez-Roux AV, Alonso A, Soliman EZ, Heckbert S. Negative Affect and Risk of Atrial Fibrillation: MESA. J Am Heart Assoc. 2019;8:e010603. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 7. | Christensen MA, Dixit S, Dewland TA, Whitman IR, Nah G, Vittinghoff E, Mukamal KJ, Redline S, Robbins JA, Newman AB, Patel SR, Magnani JW, Psaty BM, Olgin JE, Pletcher MJ, Heckbert SR, Marcus GM. Sleep characteristics that predict atrial fibrillation. Heart Rhythm. 2018;15:1289-1295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 68] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 8. | Fitzgerald PJ. Elevated norepinephrine may be an etiological factor in a wide range of diseases: age-related macular degeneration, systemic lupus erythematosus, atrial fibrillation, metabolic syndrome. Med Hypotheses. 2013;80:558-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 9. | Bergantin LB. Depression Rises the Risk of Hypertension Incidence: Discussing the Link through the Ca2+/cAMP Signalling. Curr Hypertens Rev. 2020;16:73-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 10. | Park HW, Shen MJ, Lin SF, Fishbein MC, Chen LS, Chen PS. Neural mechanisms of atrial fibrillation. Curr Opin Cardiol. 2012;27:24-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 66] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 11. | Bergantin LB. Diabetes and inflammatory diseases: An overview from the perspective of Ca(2+)/3'-5'-cyclic adenosine monophosphate signaling. World J Diabetes. 2021;12:767-779. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 17] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (7)] |
| 12. | Bergantin LB. Hypertension, Diabetes and Neurodegenerative Diseases: Is there a Clinical Link through the Ca2+/cAMP Signalling Interaction? Curr Hypertens Rev. 2019;15:32-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 13. | Caricati-Neto A, García AG, Bergantin LB. Pharmacological implications of the Ca(2+)/cAMP signaling interaction: from risk for antihypertensive therapy to potential beneficial for neurological and psychiatric disorders. Pharmacol Res Perspect. 2015;3:e00181. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 2.6] [Reference Citation Analysis (1)] |
| 14. | Bergantin LB. A Timeline of Ca(2+)/cAMP Signalling: From Basic Research to Potential Therapeutics for Dementia. Curr Alzheimer Res. 2022;19:179-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Bergantin LB. The Interactions among Hypertension, Cancer, and COVID-19: Perspective with Regard to Ca(2+)/cAMP Signalling. Curr Cancer Drug Targets. 2022;22:351-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Segan L, Prabhu S, Kalman JM, Kistler PM. Atrial Fibrillation and Stress: A 2-Way Street? JACC Clin Electrophysiol. 2022;8:1051-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 17] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 17. | Patel D, Mc Conkey ND, Sohaney R, Mc Neil A, Jedrzejczyk A, Armaganijan L. A systematic review of depression and anxiety in patients with atrial fibrillation: the mind-heart link. Cardiovasc Psychiatry Neurol. 2013;2013:159850. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 75] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 18. | Bergantin LB. A link among schizophrenia, diabetes, and asthma: Role of Ca2(+)/cAMP signaling. Brain Circ. 2020;6:145-151. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Bergantin LB. The clinical link between depression and obesity: Role of Ca(2+)/cAMP signalling. Psychiatry Res. 2020;291:113167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 20. | Bergantin L. Ca(2+)/cAMP ratio: An inflammatory index for diabetes, hypertension, and COVID-19. World J Diabetes. 2023;14:343-346. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (4)] |
| 21. | Nobel Prize: cyclic AMP recognized. Nature. 1971;233:513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Walaas O, Jahnsen T, Walaas SI, Hansson V. [The 1992 Nobel Prize in physiology and medicine]. Tidsskr Nor Laegeforen. 1992;112:3775. [PubMed] |
| 23. | Lefkowitz RJ. Rodbell and Gilman win 1994 Nobel Prize for Physiology and Medicine. Trends Pharmacol Sci. 1994;15:442-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 24. | Galli T, Kuster A, Tareste D. [Nobel Prize in Physiology and Medicine 2013 - an award for the discovery of the actors and fundamental molecular mechanisms of intracellular vesicle trafficking]. Med Sci (Paris). 2013;29:1055-1058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Brose N. All roads lead to neuroscience: the 2013 Nobel Prize in Physiology or Medicine. Neuron. 2014;81:723-727. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 26. | Greger R. [Nobel Prize for Medicine and Physiology 1991. Analysis of the function of single ion channel]. Dtsch Med Wochenschr. 1991;116:1849-1851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 27. | Jiang J, Jiang T, Wang X, Zhao M, Shi H, Zhang H, Li W, Jiang S, Zhang X, Zhou J, Ren Q, Wang L, Yang S, Yao Z, Liu Y, Xu J. Malnutrition exacerbating neuropsychiatric symptoms on the Alzheimer's continuum is relevant to the cAMP signaling pathway: Human and mouse studies. Alzheimers Dement. 2025;21:e14506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 28. | Bergantin LB. The Connections between Inflammaging and Ca(2+)/cAMP Signalling: A Unified Theory. Curr Top Med Chem. 2024;24:1359-1361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 29. | Chou CW, Fang WH, Chen YY, Wang CC, Kao TW, Wu CJ, Chen WL. Association between Serum Calcium and Risk of Cardiometabolic Disease among Community-dwelling Adults in Taiwan. Sci Rep. 2020;10:3192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 30. | PhD LGMP. Association of Atrial Fibrillation with Diabetes Mellitus, High Risk Comorbidities. Maedica (Bucur). 2022;17:143-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 31. | Aronow WS. Hypertension associated with atrial fibrillation. Ann Transl Med. 2017;5:457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 32. | Watanabe H, Tanabe N, Watanabe T, Darbar D, Roden DM, Sasaki S, Aizawa Y. Metabolic syndrome and risk of development of atrial fibrillation: the Niigata preventive medicine study. Circulation. 2008;117:1255-1260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 333] [Cited by in RCA: 319] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 33. | Bergantin LB. The Connections between Atrial Fibrillation and Mental Disorders: Role of Ca2+/cAMP Signalling. Curr Signal Transduct Ther. 2024;19. [RCA] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |