Published online May 19, 2025. doi: 10.5498/wjp.v15.i5.104113
Revised: January 20, 2025
Accepted: March 6, 2025
Published online: May 19, 2025
Processing time: 137 Days and 23.1 Hours
China has recently encountered severe challenges associated with population aging. Parents of first-generation only children face significant challenges regar
To analyze the elderly care needs of first-generation only child parents in China and identify factors that influence negative emotions.
This study used a cross-sectional design. Convenience sampling was used to select 1580 elderly individuals who met the inclusion criteria in a Chinese city between June and September 2022. A questionnaire was administered to collect general information about participants. Depression and anxiety were assessed using the patient health questionnaire-9 and generalized anxiety disorder-7 scale, respectively. A logistic regression analysis was performed to evaluate the relevant correlations.
Among 1580 first-generation only child parents, 1120 (70.89%) preferred family based care, 324 (20.51%) opted for community care, and 136 (8.61%) chose institutional care, with 460 (29.11%) reporting negative emotions. Significant differences in the distribution of negative emotions among only child parents were observed based on age, marital status, living conditions, disability, type of chronic disease, frailty status, and family support (P < 0.05). The regression analysis indicated that disability, type of chronic disease, living environment, frailty status, and level of family support were independent risk factors for negative emotions among parents with only children (P < 0.05).
Elderly care for parents of only children is primarily family-based. Independent risk factors for negative emotions in this group include disability, chronic disease type, and living environment.
Core Tip: The rapid aging of the Chinese population has created significant challenges for first-generation only child parents concerning their elderly care needs and associated negative emotions. This study therefore assessed the elderly care needs of first-generation parents of only children in a Chinese city, to identify factors that influence negative emotions. Our findings indicate that these parents primarily rely on family-based care, with only a small proportion opting for community or institutional care. The independent risk factors for negative emotions include disability, chronic disease, living environment, frailty status, and family support. Health managers should screen for these risk factors, implement early preventive strategies, and enhance family support to alleviate negative emotions.
- Citation: Dong R, Wang XX, Zhang LJ. Elderly care needs and factors influencing negative emotions among first-generation only child parents in a Chinese city. World J Psychiatry 2025; 15(5): 104113
- URL: https://www.wjgnet.com/2220-3206/full/v15/i5/104113.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i5.104113
The global concern of population aging is particularly pronounced in China, the most populous country in the world[1]. According to United Nations aging standards, China officially became an aging society in 2000[2]. The latest data from the seventh national census indicate that the population aged ≥ 60 years has reached 264 million, accounting for 18.7% of the total population, with those aged ≥ 65 years reaching 190 million or 13.5%[3]. China has become the country with the largest global elderly population. Moreover, the elderly population is projected to approach 500 million by 2050, marking a transition into a phase of deep aging in which elderly care concerns will become even more pronounced[4]. Currently, the elderly care model of China relies primarily on family support. Approximately 90% of elderly individuals reportedly depend on their families for self-care, 7% benefit from community home care services, while only 3% receive care from institutions[5,6]. This indicates that despite the gradual development of community and institutional care, family based elderly care remains the core model within the elderly care system in China. However, as the elderly population and the degree of aging continue to increase, the burden of elderly care becomes increasingly heavy.
The implementation of the family planning policy has effectively controlled the growth of the population in China and improved the quality of life of its citizens; however, it has also elicited certain social issues. Only children must now take care of their own families and work while also taking care of their parents. Such overwhelming pressure often makes them feel helpless, which has emerged as a problem that parents of only children have to face in the pension system and will exist for an extended duration into the future.
Notably, parents of first-generation only children in urban areas are gradually entering old age. Because these only children have largely entered the workforce and established new families, the traditional “4-2-1” family structure (comprising 4 grandparents, 2 middle-age parents, and 1 child) has become more prevalent[7]. This unique family background has led to the gradual weakening of traditional elderly care resources and functions, resulting in increasingly prominent issues regarding elderly care for parents of first-generation only children[8]. Elderly parents in these families are at higher risk of depression[9,10]. The incidence of depressive symptoms among parents of only children can reportedly be as high as 20%-40%[11-13]. However, research investigating the factors that influence negative emotions (such as depression and anxiety) in this population remains relatively scarce.
To explore elderly care needs and factors influencing negative emotions among first-generation only child parents, this study focuses on a specific city in China. We used the generalized anxiety disorder-7 (GAD-7) scale[14] and the patient health questionnaire-9 (PHQ-9)[15] as assessment tools to identify the presence of negative emotions among the study participants. We aimed to analyze elderly care needs and factors influencing negative emotions among parents of the first generation of only children in the context of aging in a specific city in China. Our goal was to provide a theoretical basis and empirical support for the relevant policies formulated by the Civil Affairs and Social Security Departments of China.
This study used a cross-sectional design, with a self-designed questionnaire and existing scales, to conduct field visits between June and September, 2022. A stratified random cluster sampling method was used to select elderly individuals ≥ 60 years of age in XX City. In a certain city, stratified random sampling was planned based on administrative regions, using a reliable and valid questionnaire to analyze the basic conditions of the randomly selected communities' parents of first-generation only children, including sex, age, occupation, monthly income level, education level, health status, and living arrangements. We also analyzed the elderly care needs of the first generation only children, including their economic security, emotional support, daily care, medical care, and social interaction needs. A total of 1624 questionnaires were distributed and 1580 valid responses were collected, corresponding to a response rate of 97.3%.
Residents of XX city who were ≥ 60 years old and parents of only children were included. Individuals with severe acute or chronic illnesses and those who were unable to communicate effectively were excluded.
This study was approved by the Research Ethics Committee, and participation was voluntary.
Collection of general information: Information regarding sex, age, educational level, occupation before retirement, marital status, living situation, monthly income, disability status, medical payment methods, and types of chronic diseases was collected.
Negative emotions (anxiety/depression): The presence of negative emotions was defined as having ≥ 1 of either anxiety or depression. Depression was assessed using the PHQ-9, which consists of nine items rated on a four-point Likert scale ranging from 0 (never) to 3 (every day). Scores can range from 0 to 27, with a score ≥ 10 indicating the presence of de
The GAD-7 scale was used to evaluate anxiety levels. This scale comprises seven symptom items aimed at measuring the severity and functional impact of anxiety symptoms experienced over the previous 2 weeks. Responses were rated on a four-point Likert scale, ranging from 0 (never) to 3 (every day), resulting in a total score from zero to 21. A score ≥ 10 indicated the presence of anxiety. The Chinese version of GAD-7 is commonly used to evaluate anxiety severity in the Chinese population, with a Cronbach’s alpha coefficient of 0.938 in a previous study[14].
Fried frailty phenotype[16]: The frailty status of the participants was assessed using a combination of self-reporting and objective measurements, including fatigue, decreased walking speed, reduced grip strength, and decreased physical activity. Each of the above criteria counted as 1 point, with a scoring range of 0 to 5, as follows: 0 points, indicated health; 1-2 points, indicated pre-frailty; and ≥ 3 points indicated frailty. Higher scores indicated greater frailty, with an internal consistency coefficient of 0.818.
Family Apgar index scale[17]: This scale assesses adaptability, partnership, growth, affection, and intimacy. Each item was scored from 0 to 2, resulting in a total score ranging from 0 to 10. Scores of 0-3 indicated severe family dysfunction, 4-6 indicated mild-to-moderate dysfunction, and 7-10 indicated good family support. Higher scores reflected greater family support, with an internal consistency coefficient of 0.872.
Data entry was performed using Epidata version 3.1 (www.epidata.dk), which enables efficient and accurate data management through double entry by two individuals, to minimize data entry errors. Statistical analyses were performed using SPSS (version 22.0; IBM Corp., Armonk, NY, United States), a widely used statistical analysis software that offers robust tools for data management and a variety of statistical tests, making it suitable for the comprehensive analyses of complex datasets. Continuous variables reported as descriptive statistics are expressed as means and standard deviations, and categorical variables are expressed as counts and percentages. Pearson’s χ² test was used to compare categorical variables. Owing to the non-normal distribution of the dependent variable and collinearity issues, a binary logistic regression (using the stepwise likelihood ratio method) was employed for the multi-factor analysis. The odds ratio (OR) was employed to determine the ratio of the odds and the 95% confidence interval (CI) for an event occurring in the negative emotion group compared to its occurrence in the group without negative emotions. Negative emotions were defined as the outcome variable, categorizing participants into two groups: Those who experienced negative emotions and those who did not. Two-sided statistical tests were used in the regression model, and differences with P < 0.05 were considered significant.
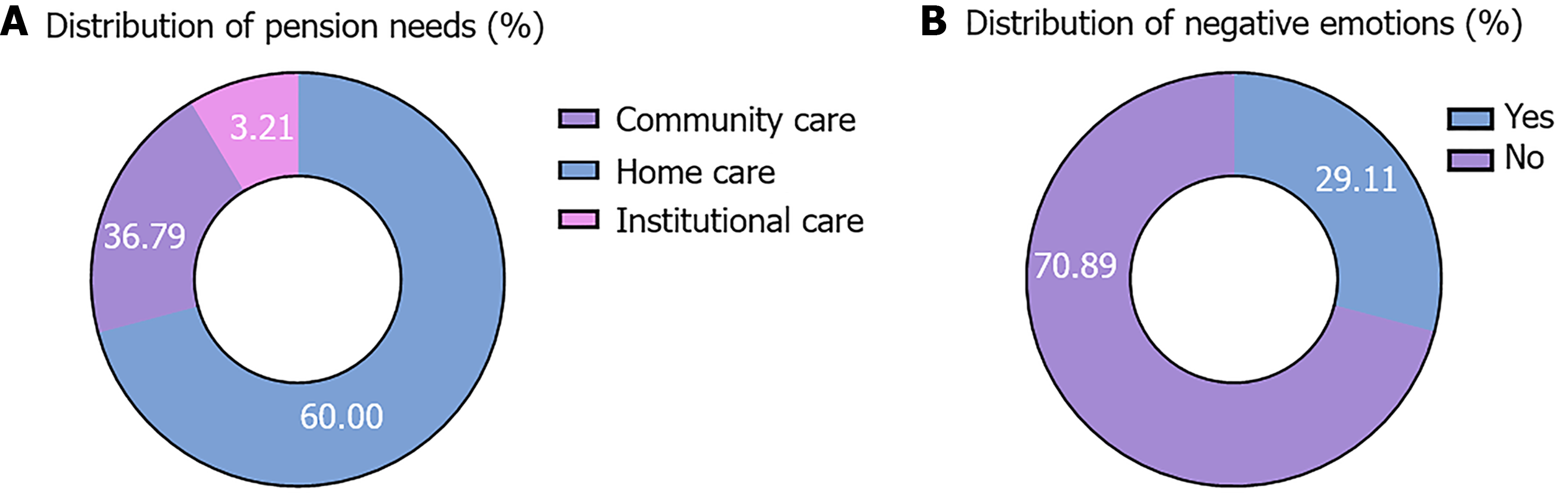
The demographic and clinical information of the participants is summarized in Table 1. Among the 1580 parents of only children, 781 (49.43%) were men and 799 (50.57%) were women. Age distribution among the cohort was as follows: 60-69 years [48.35% (n = 764)]; 70-79 [n = 566 (35.82%)]; 80-89 [n = 220 (13.92%)]; and ≥ 90 [n = 30 (1.90%)]. The educational levels of the cohort were as follows: Illiterate [n = 541 (34.24%)], primary [n = 601 (38.04%)], junior high school [n = 296 (18.73%)], vocational/high school [n = 106 (6.71%)], and college education or above [n = 36 (2.28%)]. Regarding preferred living arrangements, 1120 participants chose family care (70.89%), and 324 (20.51%) and 136 (8.61%) chose community and institutional care, respectively. A total of 460 (29.11%) participants reported experiencing negative emotions. The distribution of elderly care needs among parents of only children is illustrated in Figure 1A and a comparison of negative emotions among parents is presented in Figure 1B.
| Variable | People (n = 1580) | Percentage (%) |
| Sex | ||
| Male | 781 | 49.43 |
| Female | 799 | 50.57 |
| Age (year) | ||
| 60-69 | 764 | 48.35 |
| 70-79 | 566 | 35.82 |
| 80-89 | 220 | 13.92 |
| ≥ 90 | 30 | 1.90 |
| Education | ||
| Illiteracy | 541 | 34.24 |
| Primary | 601 | 38.04 |
| Secondary | 296 | 18.73 |
| Technical secondary school/high school | 106 | 6.71 |
| College and above | 36 | 2.28 |
| Distribution of pension needs | ||
| Home care | 1120 | 70.89 |
| Community care | 324 | 20.51 |
| Institutional care | 136 | 8.61 |
| Negative emotions | ||
| Yes | 460 | 29.11 |
| No | 1120 | 70.89 |
Significant differences exist in negative emotions among parents of only children based on age, marital status, living situation, disability, chronic disease type, frailty status, and family support (P < 0.05). Compared with patients with negative emotions, those without were younger, and a higher proportion were married, living with a spouse, and not disabled. However, no significant differences were found in the choice of elderly care method based on sex, pre-retirement occupation, education level, monthly income, or medical payment method (P > 0.05) (Table 2).
| Variable | Without negative emotions (n = 1120) | Negative emotions (n = 460) | P value |
| Gender | 0.181 | ||
| Male | 537 (47.95) | 244 (53.04) | |
| Female | 583 (52.05) | 216 (46.96) | |
| Age (years) | 0.033 | ||
| 60-69 | 565 (50.45) | 199 (43.26) | |
| 70-79 | 390 (34.82) | 176 (38.26) | |
| 80-89 | 140 (12.5) | 80 (17.39) | |
| ≥ 90 | 25 (2.23) | 5 (1.09) | |
| Education | 0.363 | ||
| Illiterate | 369 (32.95) | 165 (35.87) | |
| Primary school | 427 (38.13) | 174 (37.83) | |
| Junior high | 222 (19.82) | 81 (17.61) | |
| Vocational/high school | 80 (7.14) | 26 (5.65) | |
| College and above | 22 (1.96) | 14 (3.04) | |
| Occupation before retirement | 0.341 | ||
| None | 338 (30.18) | 123 (26.74) | |
| Some | 782 (69.82) | 337 (73.26) | |
| Marital status | < 0.001 | ||
| Unmarried | 22 (1.96) | 23 (5) | |
| Married | 862 (76.96) | 319 (69.35) | |
| Widowed | 223 (19.91) | 110 (23.91) | |
| Divorced | 13 (1.16) | 8 (1.74) | |
| Living situation | < 0.001 | ||
| Living alone | 88 (7.86) | 67 (14.57) | |
| Living with spouse | 664 (59.29) | 237 (51.52) | |
| Living with children | 350 (31.25) | 101 (21.96) | |
| Other | 18 (1.61) | 55 (11.96) | |
| Monthly income (yuan) | 0.759 | ||
| < 1000 | 755 (67.41) | 291 (63.26) | |
| 1000-2000 | 241 (21.52) | 108 (23.48) | |
| 2001-3000 | 88 (7.86) | 45 (9.78) | |
| > 3000 | 36 (3.21) | 16 (3.48) | |
| Disability | 0.022 | ||
| None | 984 (87.86) | 389 (84.57) | |
| Yes | 136 (12.14) | 71 (15.43) | |
| Medical payment method | 0.721 | ||
| Urban employee basic | 532 (47.5) | 225 (48.91) | |
| Urban resident basic | 67 (5.98) | 23 (5) | |
| New rural cooperative | 481 (42.95) | 186 (40.43) | |
| Commercial health insurance | 2 (0.18) | 1 (0.22) | |
| Other | 38 (3.39) | 25 (5.43) | |
| Chronic diseases | < 0.001 | ||
| None | 561 (50.09) | 195 (42.39) | |
| 1 type | 367 (32.77) | 163 (35.43) | |
| 2 types | 132 (11.79) | 76 (16.52) | |
| ≥ 3 types | 60 (5.36) | 26 (5.65) | |
| Frailty status | < 0.001 | ||
| Healthy | 660 (58.93) | 130 (28.26) | |
| Pre-frail | 343 (30.63) | 180 (39.13) | |
| Frail | 117 (10.45) | 150 (32.61) | |
| Family support | < 0.001 | ||
| Good | 612 (54.64) | 160 (34.78) | |
| Mild to moderate impairment | 330 (29.46) | 162 (35.22) | |
| Severe impairment | 178 (15.89) | 138 (30) |
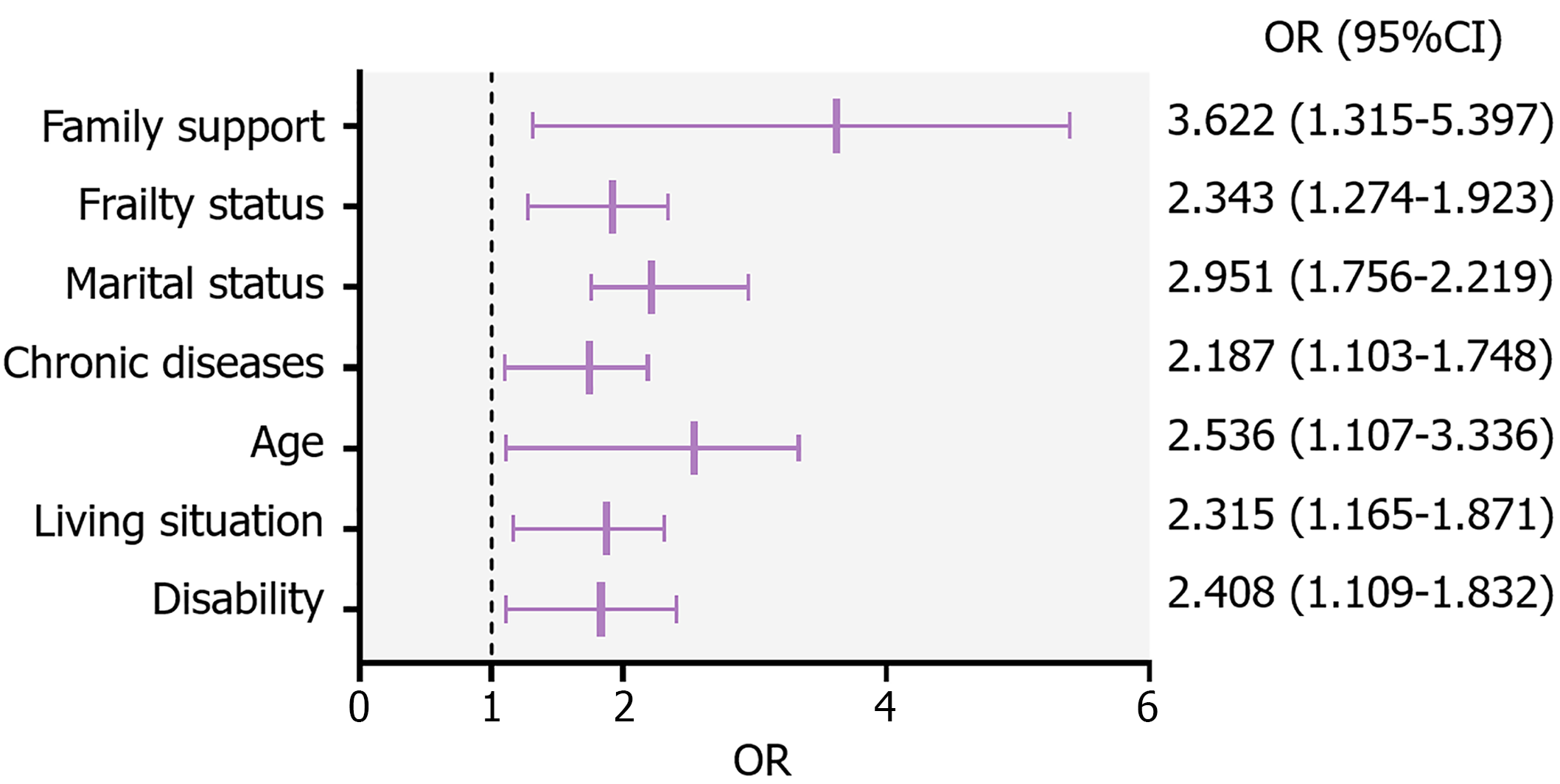
Using negative emotions as the dependent variable (0 = no, 1 = yes), statistically significant variables from the univariate analysis (Table 2) were incorporated as independent variables. Binary logistic regression analysis was performed to identify the independent factors influencing negative emotions. The regression model and variable assignments are summarized in Table 3. Results of analysis indicated that disability (OR = 2.408, 95%CI: 1.109-1.832), chronic disease type (OR = 2.187, 95%CI: 1.103-1.748), frailty status (OR = 2.343, 95%CI: 1.274-1.923), family support/care level (OR = 3.622, 95%CI: 1.315-5.397), frailty status (OR = 2.343, 95%CI: 1.274-1.923), and living arrangement (OR = 2.315, 95%CI: 1.165-1.871) were significant factors that influenced negative emotions. These findings are summarized in Table 4 and illustrated in Figure 2.
| Item | Assignment |
| Age | 60-69 years = 1, 70-79 years = 2, 80-89 years = 3, ≥ 90 years = 4 |
| Marital status | Single = 1, married = 2, widowed = 3, divorced = 4 |
| Living situation | Living alone = 1, living with spouse = 2, living with children = 3, other = 4 |
| Disability | No = 0, yes = 1 |
| Chronic disease types | None = 0, 1 type = 1, 2 types = 2, ≥ 3 types = 3 |
| Frailty status | Healthy period = 1, pre-frailty = 2, frailty period = 3 |
| Family support | Good = 1, mild to moderate impairment = 2, severe impairment = 3 |
| Variable | OR | 95%CI | P value |
| Disability | 2.408 | 1.109-1.832 | 0.043 |
| Living situation | 2.315 | 1.165-1.871 | 0.036 |
| Age | 2.536 | 1.107-3.336 | 0.917 |
| Chronic diseases | 2.187 | 1.103-1.748 | < 0.001 |
| Marital status | 2.951 | 1.756-2.219 | 0.876 |
| Frailty status | 2.343 | 1.274-1.923 | 0.025 |
| Family support | 3.622 | 1.315-5.397 | < 0.001 |
This study provides a comprehensive analysis of the demographic and clinical characteristics of parents of only children, highlighting the independent risk factors associated with negative emotions in this population. Our results revealed that 29.11% of the 1580 participants reported experiencing negative emotions. This high prevalence underscores the psychological health challenges faced by older adults, particularly the parents of only children. This is consistent with the results of a previous study[10].
Demographic data revealed a balanced sex distribution, with 49.43% of participants being men and 50.57% being women. The age distribution indicated that the majority of participants were in the 60-69 years age group (48.35%), followed by the 70-79 years age group (35.82%). This suggests that most parents of only children are in the early stages of old age, a critical period when the risk for psychological health issues exists due to declining health and increased social isolation[18]. The educational level of the participants was relatively low, with a significant proportion being illiterate (34.24%) or having completed only primary education (38.04%). Liang et al[19] reported that in China, the education level of the elderly is relatively low and that they experience memory loss and poor comprehension ability, which is consistent with the results of this study. Low educational attainment may contribute to lack of awareness of mental health resources and coping strategies, potentially exacerbating feelings of helplessness and depression.
The distribution of elderly care needs among parents of only children presented a predominance of family (70.89%), community (20.51%), and institutional (8.61%) care. Reliance on family care may impose greater emotional burden on parents, particularly when family members are unable to provide adequate support[20]. A considerable proportion of the participants lived alone or in environments with poor support, which could further exacerbate feelings of loneliness and depression. This finding aligns with previous research and highlights the importance of social support networks in mitigating psychological distress in older adults.
Univariate analysis revealed significant differences in negative emotional status among participants based on age, marital status, living situation, disability, type of chronic disease, frailty status, and family care level (P < 0.05). Mul
Compared to previous studies, our findings are consistent with the observed prevalence of negative emotions in older adults, which suggests that a large portion of this demographic faces similar psychological challenges. However, our study uniquely highlights the specific role played by educational attainment as a factor for promoting mental health awareness, which differs from previous studies that focused primarily on health status.
Therefore, an urgent need exists for targeted mental health interventions for parents of children who experience negative emotions, and future research should implement early prevention strategies that target the risk factors identified in this study. These strategies include community-based programs, family education regarding mental health resources, workshops to improve coping skills, and initiatives to promote social engagement and reduce isolation. In addition, the incorporation of mental health screening into the routine medical care of older adults will facilitate the early identification and intervention of those at risk.
This study has several limitations that should be noted when interpreting our findings, the first of which is its cross-sectional design and data collection at a single time point. This restricts our ability to make causal inferences about the relationships between demographic and clinical factors and negative emotions. Future longitudinal studies are needed to better understand the evolution of these relationships. Second, the assessment of negative emotions, frailty, and family care levels relied on self-administered questionnaires. This may have introduced bias because participants may have underestimated or overestimated their emotional states or health conditions due to social desirability or lack of self-awareness. Future research should combine objective measures with self-reporting to enhance the validity of findings. Additionally, although this study used stratified random sampling, the results may not be generalizable to all parents of only children from different regions or cultural contexts. This study was conducted in a specific urban area and the unique sociocultural dynamics of this region may have influenced the results. Further studies conducted in diverse settings are required to validate these findings. Future studies should consider a broader range of variables to provide a deeper understanding of independent factors affecting negative emotions in this population.
In summary, in the context of ageing, parents of only children rely primarily on family care, with only a small proportion opting for community or institutional care. Disability, chronic disease, living environment, frailty status, and family care level were independent risk factors for negative emotions among parents. Therefore, health managers should screen for these risk factors, implement early prevention strategies, and enhance family care to mitigate negative emotions.
| 1. | Huang Y, Xu T, Yang Q, Pan C, Zhan L, Chen H, Zhang X, Chen C. Demand prediction of medical services in home and community-based services for older adults in China using machine learning. Front Public Health. 2023;11:1142794. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Li X, Li C, Huang Y. Spatial-temporal analysis of urban-rural differences in the development of elderly care institutions in China. Front Public Health. 2022;10:1086388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 3. | Wang X, Lee CF, Jiang J, Zhu X. Factors Influencing the Aged in the Use of Mobile Healthcare Applications: An Empirical Study in China. Healthcare (Basel). 2023;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 4. | Ren W, Chen D, Tarimo CS, Tian Q, Wu J, Wang Y, Li S. A study on the current state and equity level of social participation ability among older adults in Henan Province, China. BMC Geriatr. 2022;22:340. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 5. | Ren M, Chang X, Du S, Liu L. Who would rescue the dilemma of Chinese elderly care? An evolutionary game analysis and simulation research on the formalization of the domestic service industry with subsidy policy. Front Public Health. 2023;11:1111208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 6. | Zhang J, Xu X, Zhang X, Yin Y, Wang J. Self-perceived care needs and quality of life in people with cognitive impairment during routine care at home: cross-sectional results of the interventional study. BMC Geriatr. 2023;23:185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 7. | Wang H, Guan Y, Hu R, Bragg F, Yu M, Zhong J. Willingness for community-based and institutional eldercare among older adults: a cross-sectional study in Zhejiang, China. BMJ Open. 2022;12:e055426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Zhang Y, Zhang L, Li F, Deng L, Cai J, Yu L. Offspring Education and Parents' Health Inequality in China: Evidence from Spillovers of Education Reform. Int J Environ Res Public Health. 2022;19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Song L, Wang Y, Zhang Q, Yin J, Gan W, Shang S, Qi L, Chen S, Liu T. The mediating effect of resilience on mental health literacy and positive coping style among Chinese empty nesters: A cross-sectional study. Front Psychol. 2023;14:1093446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 10. | Zhao Y, Mai H, Bian Y. Associations between the Number of Children, Depressive Symptoms, and Cognition in Middle-Aged and Older Adults: Evidence from the China Health and Retirement Longitudinal Study. Healthcare (Basel). 2024;12. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Ye YP, Wang JN, Li QC, Xu CM, Rong C. Factors associated with the depression status of Chinese parents who have lost their only child. Front Public Health. 2022;10:931945. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 12. | Rong C, Zheng LJ, Zhang Q, Cao YD, Shen SH, Gao ZQ, Wan D, Shen WW, Xu CM, Wang XL. Factors Associated With Health-Related Quality of Life of Parents Who Lost Their Only Child: A Cross-Sectional Study in Central China. Front Public Health. 2020;8:507785. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 13. | Rong C, Wan D, Xu CM, Xiao LW, Shen SH, Lin JM. Factors associated with preferences for elderly care mode and choice of caregivers among parents who lost their only child in a central China city. Geriatr Gerontol Int. 2020;20:112-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 14. | Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11947] [Cited by in RCA: 18879] [Article Influence: 993.6] [Reference Citation Analysis (0)] |
| 15. | Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21545] [Cited by in RCA: 28941] [Article Influence: 1205.9] [Reference Citation Analysis (0)] |
| 16. | Navarrete-Villanueva D, Gómez-Cabello A, Marín-Puyalto J, Moreno LA, Vicente-Rodríguez G, Casajús JA. Frailty and Physical Fitness in Elderly People: A Systematic Review and Meta-analysis. Sports Med. 2021;51:143-160. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 70] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 17. | Mayorga-Muñoz C, Gallardo-Peralta L, Galvez-Nieto JL. [Psychometric properties of APGAR-family scale in a multiethnic sample of Chilean older people]. Rev Med Chil. 2019;147:1283-1290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Zhang Y, Yu X. Evaluation of Long-Term Care Insurance Policy in Chinese Pilot Cities. Int J Environ Res Public Health. 2019;16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Liang R, Zhang H, Xie L, Sun A, Wang J, Chen J. Application of medical-nurse integration health education in aged patients undergoing percutaneous vertebroplasty. Medicine (Baltimore). 2023;102:e33879. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 20. | Qu B, Li X, Liu J, Mao J. Analysis of the current situation regarding the aging rural population in China and proposed countermeasures. Popul Health Manag. 2012;15:181-185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 21. | Wang N, Chu T, Li F, Wang Z, Liu D, Chen M, Wang H, Niu G, Liu D, Zhang M, Xu Y, Zhang Y, Li J, Li Z, You J, Mao L, Li H, Chen Y, Liu H, Zhang F. The role of an active surveillance strategy of targeting household and neighborhood contacts related to leprosy cases released from treatment in a low-endemic area of China. PLoS Negl Trop Dis. 2020;14:e0008563. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 22. | Neumann JT, Thao LTP, Murray AM, Callander E, Carr PR, Nelson MR, Wolfe R, Woods RL, Reid CM, Shah RC, Newman AB, Williamson JD, Tonkin AM, McNeil JJ; ASPREE investigators. Prediction of disability-free survival in healthy older people. Geroscience. 2022;44:1641-1655. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 18] [Reference Citation Analysis (0)] |