Published online May 19, 2025. doi: 10.5498/wjp.v15.i5.101844
Revised: December 31, 2024
Accepted: March 31, 2025
Published online: May 19, 2025
Processing time: 153 Days and 2.2 Hours
The surgical treatment of pelvic fractures is challenging, particularly after lum
To investigate the clinical effect of the transrectus lateral approach on pelvic fractures complicated by lumbosacral plexus injuries as well as anxiety and depression.
Data of 136 patients with pelvic fractures complicated by lumbosacral plexus injuries treated by the transrectus lateral approach (January 2011 to May 2024) were retrospectively analyzed. The patients' general data were collected via questionnaire. The Self-rating Anxiety Scale (SAS) and Self-rating Depression Scale (SDS) were used to assess anxiety and depression, respectively. We adopted a numerical rating scale (NRS) to evaluate pain degree, the Pittsburgh Sleep Quality Index (PSQI) to assess sleep quality, and Medical Research Council (MRC) Scale for Muscle Strength to evaluate treatment efficacy and complications.
The 136 included patients (92 male, 44 female) were a mean 48.02 ± 15.72 years old. The mean SAS score was 66.36 ± 5.15 preoperatively vs 42.15 ± 4.36 postoperatively, while the mean SDS score was 65.61 ± 5.02 preoperatively vs 43.83 ± 4.54 postoperatively, showing statistically significant differences (P < 0.05). The mean NRS and PSQI scores were significantly lower pre- vs postoperatively (P < 0.05). Postoperatively, 67 patients with fresh pelvic fractures plus nerve injuries achieved an MRC of M5, 22 achieved an M1-M4, and four achieved an M0. Postoperative motor function improved by a mean 4.20 grades (scale, 0-5). Among the patients with old pelvic fractures and nerve injuries, 19 achieved an M5, 16 achieved an M1-M4, and eight achieved an M0. Motor function improved significantly by a mean 3.30 grades (scale, 0-5; P < 0.05). No serious postoperative complications occurred.
The transrectus lateral approach to treating pelvic fractures plus lumbosacral plexus injuries can safely alleviate anxiety and depression, relieve pain, improve sleep quality, reduce intraoperative blood loss, and improve postoperative recovery.
Core Tip: To investigate the clinical effect of the transrectus lateral approach in the treatment of pelvic fractures complicated by lumbosacral plexus injuries as well as its influence on anxiety and depression. We conclude that the transrectus lateral approach for the treatment of pelvic fractures complicated by lumbosacral plexus injuries can alleviate anxiety and depression, relieve pain, improve sleep quality, reduce intraoperative blood loss, improve postoperative recovery, and provide high safety.
- Citation: Yang XD, Lu YT, Lai Z, Wang JJ, Jiang HC, Gu C, Fan SC. Clinical efficacy and psychological influence of lateral rectus approach for treating pelvic fracture with lumbosacral plexus injury. World J Psychiatry 2025; 15(5): 101844
- URL: https://www.wjgnet.com/2220-3206/full/v15/i5/101844.htm
- DOI: https://dx.doi.org/10.5498/wjp.v15.i5.101844
Pelvic fractures are common and prone to inducing venous injury and local symptoms of peripheral nerve injury, which seriously threaten patient safety[1]. A lumbosacral plexus injury is a common complication of pelvic fracture that often leads to complications such as lower-limb dysfunction, pain, and abnormal urinary tract function, which can seriously affect patient physical and mental health[2]. Moreover, mental health problems targeting this group have attracted increasing attention from the medical community, and anxiety and depression are often particularly pronounced among patients with fractures[3]. According to relevant studies, patients with fractures undergoing surgical treatment commonly experience fluctuations in their psychological states such as anxiety and depression, especially in the face of chronic pain, movement limitations, and poor recovery[4]. Therefore, understanding how surgical methods affect patients' psychological states is crucial for improving treatment options and patient satisfaction levels.
The transrectus lateral approach is a new surgical method that has recently shown good prospects for the treatment of pelvic fractures[5]. With the development of modern medical technology, the surgical treatment of pelvic fractures has continuously evolved[6]. The deficiencies of traditional posterior and lateral approaches in technique and effect have prompted surgeons to gradually explore new surgical options[7]. Being relatively small, the transrectus lateral approach not only effectively reduces the incidence of surgery-related complications but it maximizes protection of the lumbosacral nerve and surrounding tissues, thus promoting postoperative recovery[8]. Although some studies have demonstrated the advantages of this approach, relatively few have investigated its psychological effects in the treatment of pelvic fractures with lumbosacral plexus injuries.
Therefore, studying the clinical efficacy of the transrectus lateral approach in the treatment of pelvic fractures is of great significance for improving fracture treatment success rates, shortening hospital stays, and improving patient quality of life. This study aimed to evaluate the clinical efficacy of the transrectus lateral approach in the treatment of pelvic fractures complicated by lumbosacral plexus injuries and further investigate its effect on anxiety and depression. Through a comprehensive analysis of postoperative clinical indicators and psychological states, we hope to provide more effective strategies for reducing postoperative pain and psychological burden among this population in clinical practice.
The data of 136 patients with pelvic fractures and comorbid lumbosacral plexus injuries treated with a lateral rectus incision between January 2011 and May 2024 were retrospectively analyzed.
This study was approved by the Ethics Committee of the Third Affiliated Hospital of Southern Medical University. All patients provided signed informed consent.
The inclusion criteria were as follows[9]: (1) Definite symptoms of posterior pelvic ring instability combined with a lumbosacral plexus injury, admission to the Third Affiliated Hospital of Southern Medical University between January 2011 and May 2024, and lower-limb motor function loss or decline; (2) Obvious fracture displacement at the lumbosacral plexus nerve anterior to the sacroiliac joint on imaging and a nerve injury suspected to be caused by anterior compression or traction; and (3) The use of a single transrectus lateral approach to explore and release the nerve but no nerve tears and fractures identified intraoperatively.
The exclusion criteria were as follows: (1) The use of a combined anterior and posterior approach to explore patients with release and fracture fixation; (2) Posterior pelvic ring instability without symptoms of a nerve injury; (3) A history of ipsilateral abdominal surgery; and (4) A history of intraoperative exploration of the lumbosacral plexus for a laceration or fracture.
All patients underwent tracheal intubation and general anesthesia prior to surgery and were placed in the supine position. The surgical incision was started at the outer one-third of the line connecting the anterior superior iliac spine and the umbilicus, with the endpoint at the midpoint of the inguinal ligament. A subfascial wedge-shaped incision was started at the inner edge of the superficial inguinal ring and extended through the external oblique aponeurosis, tran
The dissection began in the extraperitoneal space with careful retraction of the peritoneum and pelvic tissues. The sacroiliac joint was first exposed and the dissection continued along the sacroiliac joint toward the medial auricular surface of the sacrum. The lumbosacral plexus was then explored and freed. Bipolar coagulation may be considered in cases of bleeding from the presacral venous plexus. Once the fracture ends were exposed, the surrounding soft tissues were cleared and the lumbosacral plexus nerves embedded in the fracture ends released and protected, followed by fracture reduction.
Depending on the patient’s specific condition, a presacral plate or sacroiliac joint screw was chosen for fixation. For sacral Denis I zone fractures, the use of a presacral plate for fixation is recommended, whereas screws are chosen for other fracture types. Postoperatively, the wound was washed routinely, bleeding controlled, and the incision closed. Prophylactic antibiotics were administered to prevent infection and measures were taken to prevent thrombosis.
The collected data included age, sex, Young-Burgess pelvic fracture classification[10] [anteroposterior compression (APC), lateral compression (LC), vertical shear (VS), and combined mechanism (CM)], lower-limb motor function, nerve injury grade, intraoperative nerve injury, operative time, intraoperative blood loss, fracture healing time, postoperative muscle strength recovery, and complications (urine extravasation, aggravated nerve injury, femoral nerve injury, and lateral femoral cutaneous nerve injury).
The Self-rating Anxiety Scale (SAS) and Self-rating Depression Scale (SDS) were used to evaluate anxiety and depression, respectively. The SAS was divided into 50 lines in which the higher the score, the more serious the anxiety, whereas the SDS was divided into 53 lines in which the higher the score, the more serious the depression. The Cronbach's α coefficients of the two scales were 0.782 and 0.777, respectively, indicating good reliability and validity[11].
A numerical rating scale (NRS) was used to evaluate the degree of pain (range, 0-10), with 10 indicating the most painful and 0 indicating no pain[12].
Sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI), which includes seven dimensions: Sleep efficiency, quality, disturbance, time, use of hypnotic drugs, sleep latency, and daytime dysfunction (19 items total). A four-point scoring method was used to obtain a maximum score of 21 points. Higher scores indicated worse sleep quality. The Cronbach's α coefficient of this scale was 0.710, indicating good reliability and validity[13].
The Medical Research Council (MRC) scale for muscle strength was used to evaluate the postoperative effect of treatment as follows[14]: M0, no muscle contraction; M1, visible contraction of the proximal muscles; M2, visible contractions of the proximal and distal muscles; M3, all important muscles contract against resistance; M4, ability to perform independent and coordinated movements; and M5, completely normal.
The statistical analyses were performed using SPSS Statistics for Windows (version 26.0; IBM). Continuous variables were analyzed using descriptive statistics and are presented as mean and standard deviation, whereas categorical variables are shown as count and percentage (%). The regression model used two-sided tests with a significance threshold of P < 0.05.
Of the 136 included patients (92 male, 44 female), the mean age was 48.02 ± 15.72 years (range, 16-69 years). The Young-Burgess classification of the pelvic fractures was as follows: APC, 21 cases (15.44%); LC, 35 cases (25.74%); VS, 62 cases (45.59%); and CM, 28 cases (20.59%). All 136 patients had lower-limb motor dysfunction, and the overall MRC scale score was M0.
All surgeries were performed using the transrectus lateral approach. Nerve entrapment or traction injury were confirmed intraoperatively. The mean operative time was 98 ± 35.27 minutes (range, 65-224 minutes), while the mean intraoperative blood loss was 550 ± 302.03 mL (range, 240-2760 mL; Table 1).
| Variable | Patients (n = 136) | Percentage (%) |
| Sex | ||
| Male | 92 | 67.65 |
| Female | 44 | 32.35 |
| Age (year) | 48.02 ± 15.72 | / |
| Age (year) | 16-69 | / |
| Young-Burgess | ||
| APC | 21 | 15.44 |
| LC | 35 | 25.74 |
| VS | 62 | 45.59 |
| CM | 28 | 20.59 |
| Lower extremity motor dysfunction | ||
| Yes | 136 | 100.00 |
| No | 0 | 0.00 |
| BMRC | ||
| M0 | 136 | 100.00 |
| Mode of operation | ||
| Lateral approach to rectus abdominis | 136 | 100.00 |
| Operation time (min) | 65-224 | / |
| Operation time (min) | 98 ± 35.27 | / |
| Intraoperative blood loss (mL) | 240-2760 | / |
| Average blood loss (mL) | 550 ± 302.03 | / |
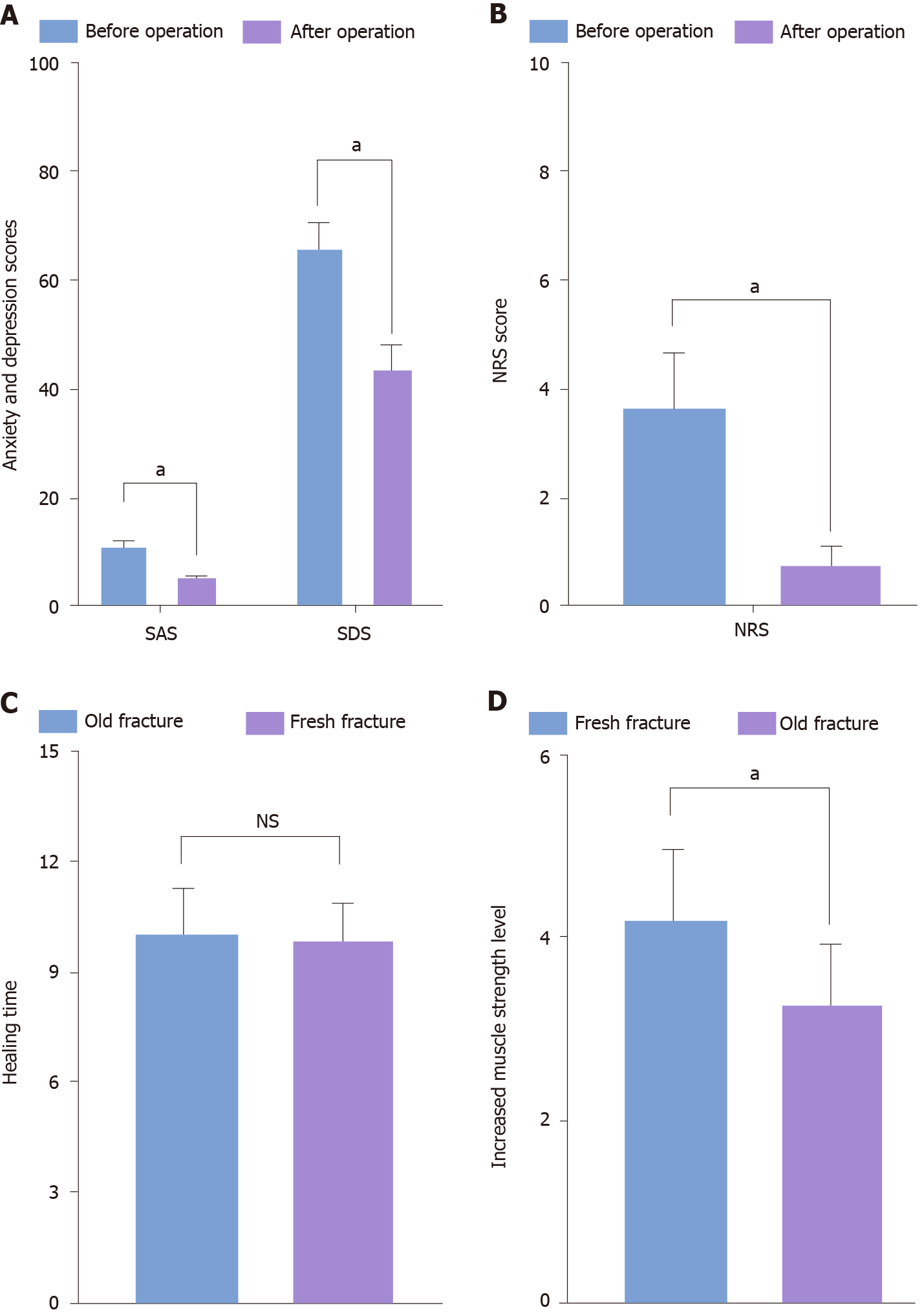
The SAS and SDS scores were significantly lower post- (42.15 ± 4.36 and 43.83 ± 4.54, respectively) vs preoperatively (66.36 ± 5.15 and 65.61 ± 5.02, respectively; P < 0.001; Table 2, Figure 1A).
| Group | Before operation | After operation | P value |
| SAS | 66.36 ± 5.15 | 42.15 ± 4.36 | < 0.001 |
| SDS | 65.61 ± 5.02 | 43.83 ± 4.54 | < 0.001 |
The mean NRS score was significantly lower post- (0.79 ± 0.36) vs preoperatively (3.65 ± 1.03; P < 0.001; Figure 1B).
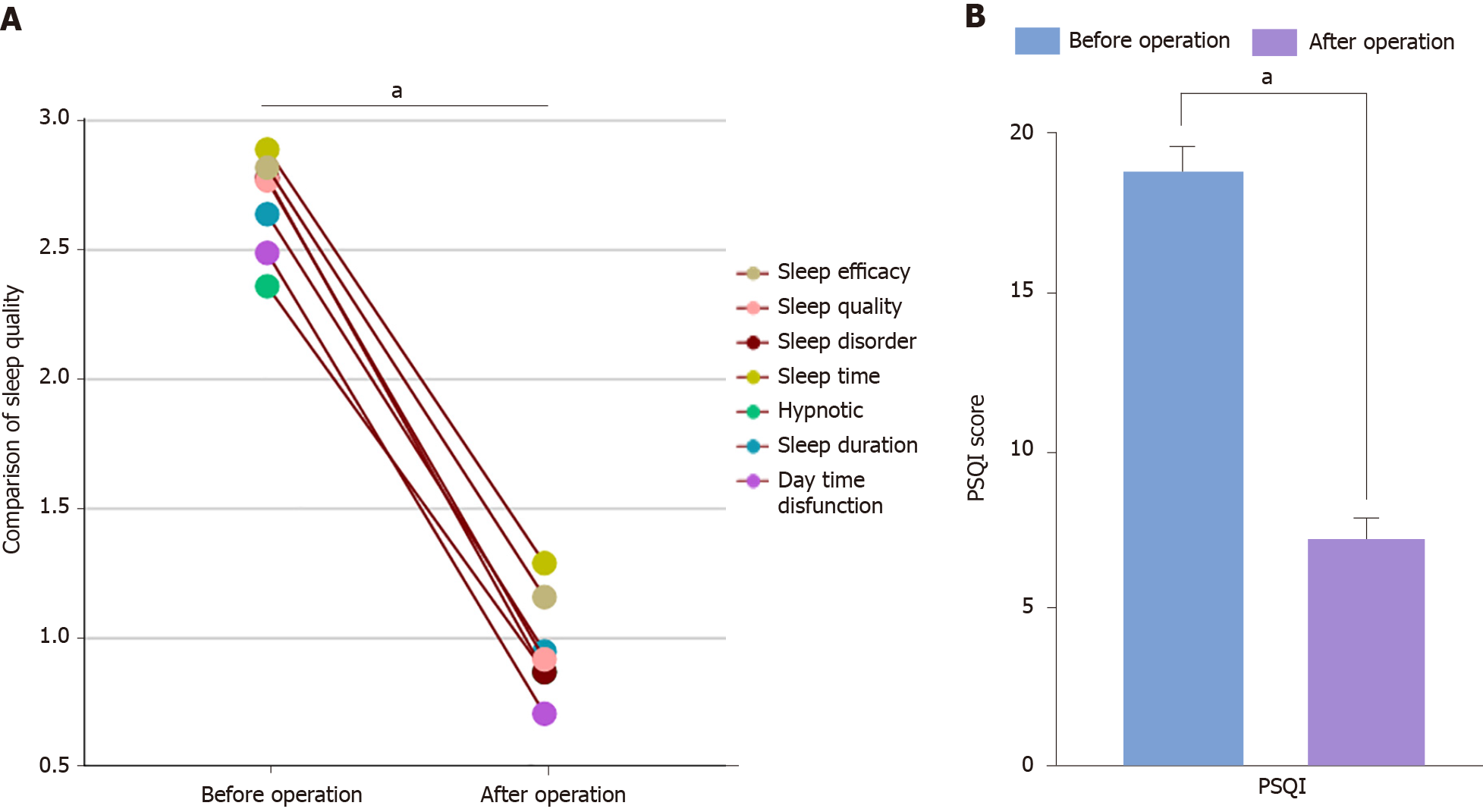
All PSQI and total scores were significantly lower post- (7.32 ± 0.56) vs preoperatively (18.89 ± 0.68; P < 0.001; Figure 2).
All fractures healed clinically within 8-12 weeks. No significant difference was noted in fracture healing time between the old and fresh fracture groups (Figure 1C).
According to the evaluation criteria for postoperative efficacy proposed by the MRC, the final follow-up results were as follows. Among the patients with fresh pelvic fractures combined with nerve injuries, 67 achieved an M5, 22 achieved an M1-M4, and four achieved an M0. Motor function improved postoperatively by a mean 4.20 grades (range, 0-5 grades). Among the patients with old pelvic fractures combined with nerve injuries, 19 achieved an M5, 16 achieved an M1-M4, and eight achieved an M0. Motor function improved postoperatively by a mean 3.30 grades (range, 0-5), and the intergroup difference was statistically significant (P < 0.05; Table 3, Figure 1D).
| Group | Old fracture (n = 93) | Fresh fracture (n = 43) | P value |
| Grade M0 | 4 | 8 | 0.002 |
| Grade M1-M4 | 22 | 16 | |
| Grade M5 | 67 | 19 |
Among patients with old pelvic fractures combined with bladder rupture (surgically repaired at a mean 59 days post-injury), urine extravasation recurred postoperatively in one and was treated with an indwelling urinary catheter. The bladder self-repaired in approximately 2 weeks, and the patient was discharged. There were no cases of aggravated nerve injuries or complications such as femoral or lateral femoral cutaneous nerve injuries. All the wounds healed in a single stage.
Patients with pelvic fractures and lumbosacral plexus injuries are prone to venous and peripheral nerve injuries; therefore, increasing attention has been paid to this issue in clinical practice[15]. However, most affected patients are middle-aged or elderly with poor psychological endurance, slow responses, unclear language expression, poor knowledge about diseases and surgeries, and excessive worry about postoperative recovery, which can easily lead to negative emotions such as anxiety and depression[16]. Postoperative psychological changes and poor sleep quality are not conducive to a patient's postoperative recovery; in fact, they slow recovery and cause poor autonomous exercise ability[4,17]. Therefore, identifying scientific and efficient surgical methods has clinical significance for relieving depression and anxiety in patients with pelvic fractures complicated by lumbosacral plexus injuries.
The results of this study showed that the mean preoperative SAS score (66.36 ± 5.15) was significantly reduced postoperatively (42.15 ± 4.36). This change reflected a significant improvement in anxiety levels. Similarly, SDS scores decreased from 65.61 ± 5.02 preoperatively to 43.83 ± 4.54 postoperatively, showing a statistically significant difference (P < 0.05). These results suggest that the transrectus lateral approach positively affects the mental health of patients with pelvic fractures and lumbosacral plexus injuries. Moreover, Liu et al[18] compared the efficacy of the para-rectus approach with that of the modified Stoppa approach in the treatment of pelvic and acetabular fractures and showed that the former featured superior operation time, incision length, and blood loss while effectively improving fracture reduction satisfaction. Although the differences in hip function scores and complication rates between the two methods were not significant, the para-rectus approach was still considered the preferred treatment for complex pelvic and acetabular fractures, consistent with the results of the present study.
Pain is an important factor affecting quality of life, especially among patients with pelvic fractures[19]. The patients in this study had lower post- vs preoperative NRS scores, possibly related to improvements in surgical techniques and effective fracture-site fixation. Effective pain management helps patients recover physically and creates a good foundation for their mental health. Improving sleep quality is an important aspect of patient rehabilitation since good sleep can promote body healing[20]. In this study, the PSQI item and total scores were significantly lower post- vs preoperatively (P < 0.05). All fractures healed clinically within 8-12 weeks. No significant difference was noted in fracture healing time between old and fresh fractures (P > 0.05), indicating the reliability and effectiveness of this surgical method as described in a previous study[5]. This finding is consistent with the findings of Yu et al[21], who aimed to evaluate the early functional and radiographic outcomes of a subrectal approach in patients with AO B2.2 pelvic fractures and demon
The anterior and posterior approaches are currently used to treat pelvic fractures complicated by nerve injuries according to the preoperative site[22]. Tang et al[23] reported the efficacy of the lateral rectus and ilioinguinal approaches in open reduction and internal fixation for Torode-Zieg type IV pelvic fractures in children. Patients with nerve injuries achieve good curative effects after minimally invasive pelvic reduction and neurolysis. In 2020, Zhan et al[24] sum
In this study, 67 patients with fresh pelvic fractures combined with lumbosacral plexus injury recovered completely, 22 partially recovered, and four incompletely recovered. The postoperative motor function improved by a mean 4.2 grades. Thus, we believe that early nerve exploration and release can effectively prevent the degeneration of nerve function caused by old fractures and long-term nerve injuries. In addition, old pelvic fractures combined with lumbosacral plexus nerve injuries treated via the lateral approach of rectus abdominis decompression are not always effective because of old pelvic fracture callus growth, surrounding soft-tissue contractures, fracture reduction difficulties, fracture hematoma organization, scar hyperplasia, nerve injury caused by long-term nerve degeneration, or other reasons. Most doctors have relatively negative views about treating old pelvic fractures combined with lumbosacral plexus nerve injuries due to technical difficulties, trauma, and poor results. This study examined 43 patients with old pelvic fractures complicated by nerve injuries. Of them, 19 recovered completely, 16 recovered partially, and eight recovered incompletely. This finding is consistent with the results of another retrospective study demonstrating that the lateral rectus approach to lumbosacral plexus injury-associated VS pelvic fractures is a safe and effective surgical option that facilitates fracture reduction and neurolysis[26].
This study had several limitations. First, the transrectal lateral incision approach differs significantly from the traditional anterior approach. Therefore, surgeons must strictly master the surgical indications, become familiar with the hierarchical structure of the anatomical approach, and complete formal anatomical surgical training. Patient imaging data must be analyzed preoperatively, as sufficient surgical experience is required to successfully treat simple pelvic acetabular fractures using this approach. Our results may have been influenced by these factors. Second, the use of self-administered questionnaires to understand patients' basic information and mental health is flawed, as it may have led to recall bias; in some cases, a questionnaire cannot truly reflect the extent of patients' mental health issues. Third, this study was conducted at a single central hospital in China and included only Chinese patients. Thus, its findings are difficult to generalize to other populations, and larger and more rigorous prospective studies are required to confirm our findings.
In conclusion, the treatment of patients with pelvic fractures complicated by lumbosacral plexus nerve injuries using the transrectus lateral approach can significantly reduce anxiety and depression levels, relieve pain, improve sleep quality, and significantly improve the bone healing efficiency and recovery degree with fewer postoperative complications and greater safety. Future studies should further explore the long-term impact of this technique on patients' psychological states and explore targeted interventions to improve their quality of life.
| 1. | Zhao C, Wang Y, Wu X, Zhu G, Shi S. Design and evaluation of an intelligent reduction robot system for the minimally invasive reduction in pelvic fractures. J Orthop Surg Res. 2022;17:205. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 2. | Liu L, Fan S, Zeng D, Song H, Zeng L, Wen X, Jin D. Identification of safe channels for screws in the anterior pelvic ring fixation system. J Orthop Surg Res. 2022;17:312. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 3. | Hoppe BS, Petersen IA, Wilke BK, DeWees TA, Imai R, Hug EB, Fiore MR, Debus J, Fossati P, Yamada S, Orlandi E, Zhang Q, Bao C, Seidensaal K, May BC, Harrell AC, Houdek MT, Vallow LA, Rose PS, Haddock MG, Ashman JB, Goulding KA, Attia S, Krishnan S, Mahajan A, Foote RL, Laack NN, Keole SR, Beltran CJ, Welch EM, Karim M, Ahmed SK. Pragmatic, Prospective Comparative Effectiveness Trial of Carbon Ion Therapy, Surgery, and Proton Therapy for the Management of Pelvic Sarcomas (Soft Tissue/Bone) Involving the Bone: The PROSPER Study Rationale and Design. Cancers (Basel). 2023;15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 4. | Xu Z, Jiang Y, Mu W, Li W, Zhang G, Jiang S, Xu P. Electrophysiological, biomechanical, and finite element analysis study of sacral nerve injury caused by sacral fracture. Front Bioeng Biotechnol. 2022;10:920991. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 5. | Liu B, Shang H, Dong G, Zhang N, Wang S. Comparison of clinical effects of two surgical approaches in the treatment of acetabular fractures. Pak J Med Sci. 2023;39:1057-1061. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Jindal K, Aggarwal S, Kumar P, Kumar V. Complications in patients of acetabular fractures and the factors affecting the quality of reduction in surgically treated cases. J Clin Orthop Trauma. 2019;10:884-889. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Li X, Xu J. Comparison of proximal femoral nail antirotation and total hip arthroplasty in the treatment of femoral intertrochanteric fracture. Pak J Med Sci. 2022;38:1016-1020. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 8. | Al Adawy AS, Aziz AHA, El Sherief FA, Mahmoud WS, Mabrook M, Hassan YE. Modified Stoppa as an alternative surgical approach for fixation of anterior fracture acetabulum: a randomized control clinical trial. J Orthop Surg Res. 2020;15:154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 9. | Shi B, Peng Y, Zhang G, Zhang S, Luo Y, Lv F, Hu Y, Zhang L. Spinopelvic dissociation: extended definition, physical examination, classification, and therapy. J Orthop Surg Res. 2023;18:56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 10. | Kunii M, Nakao S, Nakagawa Y, Shimazaki J, Ogura H. Impact of Pelvic Fracture Sites on Fibrinogen Depletion in Patients with Blunt Trauma: A Single-Center Cohort Study. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 11. | Wu Y, Wang G, Zhang Z, Fan L, Ma F, Yue W, Li B, Tian J. Efficacy and safety of unrestricted visiting policy for critically ill patients: a meta-analysis. Crit Care. 2022;26:267. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 10] [Reference Citation Analysis (0)] |
| 12. | Hjermstad MJ, Gibbins J, Haugen DF, Caraceni A, Loge JH, Kaasa S; EPCRC, European Palliative Care Research Collaborative. Pain assessment tools in palliative care: an urgent need for consensus. Palliat Med. 2008;22:895-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 13. | Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17520] [Cited by in RCA: 21913] [Article Influence: 608.7] [Reference Citation Analysis (0)] |
| 14. | Ille S, Schwendner M, Zhang W, Schroeder A, Meyer B, Krieg SM. Tractography for Subcortical Resection of Gliomas Is Highly Accurate for Motor and Language Function: ioMRI-Based Elastic Fusion Disproves the Severity of Brain Shift. Cancers (Basel). 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Durand A, Keenihan E, Schweizer D, Maiolini A, Guevar J, Oevermann A, Gutierrez-Quintana R. Clinical and magnetic resonance imaging features of lymphoma involving the nervous system in cats. J Vet Intern Med. 2022;36:679-693. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 16. | Holderread BM, Shin CP, Syed IY, Avramis I, Rizkalla JM. Sacral insufficiency fracture after lumbosacral decompression and fusion. Proc (Bayl Univ Med Cent). 2022;35:451-454. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Revuri VR, Moody K, Lewis V, Mejia R, Harrison DJ, Ahmad AH. Pain and Analgesia in Children with Cancer after Hemipelvectomy: A Retrospective Analysis. Children (Basel). 2022;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Liu W, Yang H, Yu Z, Zhao Y, Hu J, Li B, Zhu Y. Comparison of Therapeutic Outcomes of Transabdominal Pararectus Approach and Modified Stoppa Approach in Treating Pelvic and Acetabular Fractures. Indian J Orthop. 2022;56:829-836. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Florio M, Capasso L, Olivi A, Vitiello C, Leone A, Liuzza F. 3D - Navigated percutaneous screw fixation of pelvic ring injuries - a pilot study. Injury. 2020;51 Suppl 3:S28-S33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Kevin M, William H, Chilton M, Michael M, Alice H, Gregory A, Daniel A, Erik HJ. Intraoperative computerised tomography scan for percutaneous fixation of the pelvis: a retrospective case series. Int Orthop. 2024;48:2743-2748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 21. | Yu YH, Liu CH, Hsu YH, Chou YC, Chen IJ. Pararectus approach to the AO B2.2 pelvic fracture: early functional and radiological outcomes. Eur J Orthop Surg Traumatol. 2023;33:829-836. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Chen X, Liu H, Wang H, Zheng L, Li J, Yan L. Case report: A 3-year follow-up study of simultaneous bilateral total hip arthroplasty for Femoral head necrosis in a patient with Kashin-Beck Disease. Front Surg. 2022;9:978697. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 23. | Tang YJ, Yang CL, Gu C, Yang XD, Mai QG, Li T, Chen YH, Zhu ZH, Liao JW, Fan SC. [Effect comparison of lateral-rectus approach and ilioinguinal approach in the treatment of toddlers with Torode-Zieg type IV pelvic fracture]. Zhonghua Chuangshang Zazhi. 2022;38:40-46. [DOI] [Full Text] |
| 24. | Zhan XR, Zheng QB, Huang FM, Wen XY, Liu YC, Mai QG, Li T, Huang H, Yang C, Liao JW, Fan SC. [Treatment of vertical shear pelvic fracture combined with lumbosacral plexus injury through the lateral-rectus approach]. Zhonghua Chuangshang Guke Zazhi. 2020;22:482-488. [DOI] [Full Text] |
| 25. | Zheng QB, Fan SC, Hou ZY, Yi CL, Mai QG, Li T, Zhan XR, Huang FM, Wen XY, Liu YC. [The diagnosis and surgical treatment of sacral fracture (Denis Ⅱ fracture) with sacral neurological damage]. Zhonghua Chuangshang Guke Zazhi. 2021;23:47-54. [DOI] [Full Text] |
| 26. | Zhan X, Xu K, Zheng Q, Chen S, Li J, Huang H, Chen Y, Yang C, Fan S. Surgical Treatment of Vertical Shear Pelvic Fracture Associated with a Lumbosacral Plexus Injury through the Lateral-Rectus Approach: Surgical Techniques and Preliminary Outcomes. Orthop Surg. 2022;14:1723-1729. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |