Published online Oct 19, 2023. doi: 10.5498/wjp.v13.i10.753
Peer-review started: August 7, 2023
First decision: August 24, 2023
Revised: September 1, 2023
Accepted: September 11, 2023
Article in press: September 11, 2023
Published online: October 19, 2023
Processing time: 65 Days and 19.9 Hours
Patients with chronic hepatitis B (CHB) experience various problems, including low psychological flexibility, negative emotions, and poor sleep quality. Therefore, effective nursing interventions are required to reduce adverse events. Acceptance and commitment therapy (ACT) combined with enabling cognitive-behavioral education (ECBE) can improve patients' psychological and sleep. Therefore, we speculate that this may also be effective in patients with CHB.
To investigate the effects of different intervention methods on psychological flexibility, negative emotions, and sleep quality in patients with CHB.
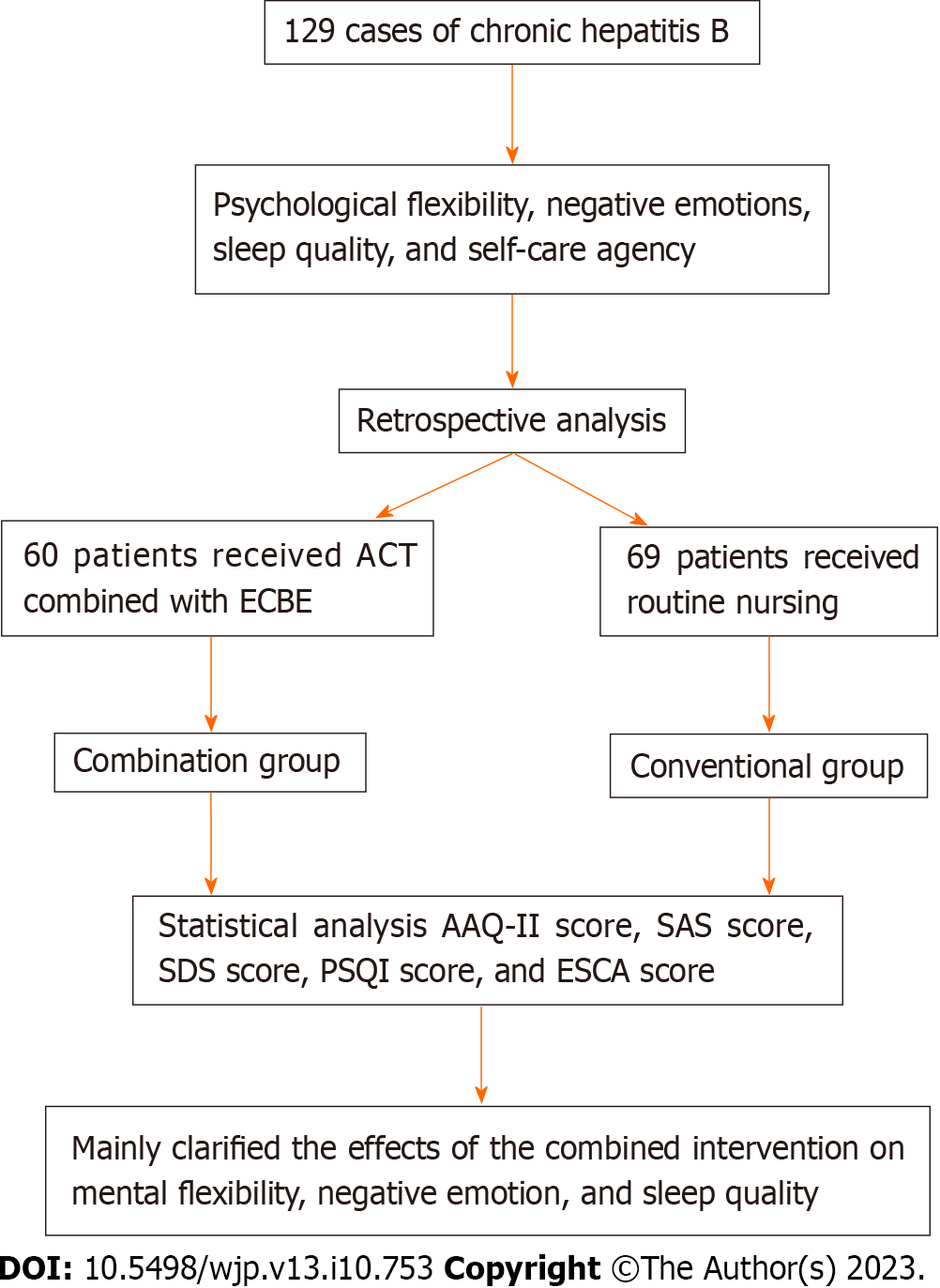
This retrospective study examined clinical and evaluation data of 129 patients with CHB. Intervention methods were divided into a conventional group (routine nursing, n = 69) and a combination group (ACT combined with ECBE, n = 60). We observed changes in psychological flexibility, negative emotions, sleep quality, and self-care ability in both groups. Observation items were evaluated using the Acceptance and Action Questionnaire-2nd Edition (AAQ-II), Self-Rating Anxiety Scale (SAS), Self-Rating Depression Scale (SDS), Pittsburgh Sleep Quality Index (PSQI), and Exercise of Self-Care Agency Scale (ESCA).
Compared with the conventional group, the AAQ-II score of the combined group was lower (Fbetween-group effect = 8.548; Ftime effects = 25.020; Finteraction effects = 52.930; all P < 0.001), the SAS score (t = 5.445) and SDS score (t = 7.076) were lower (all P < 0.001), as were the PSQI dimensions (tsleep quality = 4.581, tfall sleep time = 2.826, tsleep time = 2.436, tsleep efficiency = 5.787, tsleep disorder = 5.008, thypnotic drugs = 3.786, tdaytime dysfunction = 4.812); all P < 0.05). The ESCA scores for all dimensions were higher (thealth knowledge level = 6.994, tself-concept = 5.902, tself-responsibility = 19.820, tself-care skills = 8.470; all P < 0.001).
ACT combined with ECBE in patients with CHB can improve psychological flexibility and sleep quality, alleviate negative emotions, and improve self-care.
Core Tip: Chronic hepatitis B (CHB) is an infectious and progressive disease requiring basic treatment supplemented with effective nursing interventions. We analyzed the clinical data of 129 patients with CHB. Acceptance and commitment therapy combined with cognitive-behavioral education improved the psychological flexibility and sleep quality of patients with CHB, relieve negative emotions, and improve self-care ability, making a breakthrough in the problem of insufficient routine care.
- Citation: Zheng Y, Wang XW, Xia CX. Effects of different intervention methods on psychological flexibility, negative emotions and sleep quality in chronic hepatitis B. World J Psychiatry 2023; 13(10): 753-762
- URL: https://www.wjgnet.com/2220-3206/full/v13/i10/753.htm
- DOI: https://dx.doi.org/10.5498/wjp.v13.i10.753
Chronic hepatitis B (CHB) is a frequent chronic infectious disease. According to the World Health Organization in 2017[1], the number of CHB infections worldwide reached 257 million. Approximately 900000 people worldwide die each year from hepatitis B virus (HBV) infection or its complications[1]. Due to the mutual influence of physiological, psychological, and social factors, patients with CHB often have various sleep disorders, thus reducing the therapeutic effect[2]. Drug therapies such as conventional antiviral therapy combined with effective nursing interventions can control disease progression[3].
Bedside delivery of health education to the patient improves understanding and self-management[4]. However, after receiving education, patients still have an insufficient sense of participation, low mastery of disease knowledge, and no change in incorrect understandings. Additionally, their psychological and behavioural adaptation to the disease is not obvious, and most patients have unresolved problems such as anxiety, depression, and poor sleep. This is related to the lack of conventional health education and targeted psychological counselling[5]. Moreover, the lack of routine CHB care is a clinical problem that needs to be resolved.
Acceptance and commitment therapy (ACT) is a new type of cognitive behavioral therapy based on functional contextualism and relational reference theory, which promotes individual acceptance of the present and self, and increases psychological flexibility[6]. Additionally, enabling cognitive-behavioral education (ECBE) is a psychological behavior therapy that aims to explore individual-centered problems; help individuals reconstruct cognitive processes; solve emotional, cognitive, and behavioral disorders; and promote the development of skills and positive beliefs that enable the individual to effectively deal with problems associated with their disease[7]. ACT and ECBE have been applied to the nursing care of patients with diabetes[8], cancer[9], and other diseases[10] and have achieved good results. However, the combination of these two therapies has not been previous investigated in the treatment of CHB. This study explored the effects ACT combined with ECBE on psychological flexibility, negative emotions, and sleep quality in patients with CHB.
A total of 129 patients with CHB treated at The First People’s Hospital of Wenling between January 2021 and June 2022 were retrospectively selected. Patients were divided into two groups, depending on whether they received routine care or ACT combined with ECBE intervention.
The inclusion criteria were as follows: (1) Diagnosis of CHB according to the criteria; (2) normal vision and hearing function; (3) a complete record of baseline data (sex, age, disease course, and liver function); and (4) assessment of psychological flexibility, negative emotions, and sleep quality.
The diagnostic criteria for CHB included a positive results for both serum surface antigen and HBV DNA[11]. Additionally, liver function index alanine aminotransferase continually increased and liver histological examination showed hepatitis lesions.
The following exclusion criteria was applied: (1) Severe sleep disorders or insomnia caused by other diseases; (2) Combined heart, liver, kidney, and other organ lesions; (3) Viral hepatitis other than CHB; and (4) Malignant tumors.
According to the different nursing intervention methods applied, the patients were classified into a conventional group (routine nursing care, n = 69) and a combination group (ACT combined with ECBE, n = 60). The research concepts used are presented in Figure 1.
We collected baseline patient data from the electronic medical records, including sex, age, disease course, and evaluation data of psychological flexibility, negative emotions, sleep quality, and self-care agency.
Routine nursing: Based on principles of nursing practice, nursing staff provided nutritional interventions, medication guidance and safety nursing, early rehabilitation training, and relevant health education. Health education for patients with CHB was delivered through one-to-one communication or distribution of educational manuals to disseminate knowledge on the causes of CHB, treatment methods, risk factors, and other aspects of the disease. Relevant psychological counseling; daily personal self-care skills in a home setting and life guidance were discussed with patients on discharge from hospital.
ACT: Acceptance perception: Medical staff provided health education using graphic publicity pages or short videos to inform patients of the pathogenesis, routine treatment options, and precautions of CHB, to help increase understanding of CHB and the ramifications of the disease.
Cognitive disengagement: Family members were guided to encourage patients to actively cooperate with drug treatment or psychotherapy and strengthen family awareness of CHB to reduce the impact of adverse events or negative emotions. Under the guidance of nutritionists, dietary management and stress reduction training was also strengthened to adjust patients' negative emotions.
Experience life: Patients were encouraged to exchange experiences with their friends to can share the burden of disease and integrate into surrounding life and work. The encouragement and support of family and patient friends enabled patients to develop a good understanding of their disease and alleviate negative emotions such as fear, anxiety, and depression. Patients were also encouraged to share their experiences and empathize with life experiences, diverting patients' attention.
Self-awareness: Through patient communication and doctor-patient communication, patient awareness of the disease was strengthened, establishing confidence in treating the disease to establish correct cognition and attitude and understanding the disease.
Values: With the support of family members and medical staff, patients established social values, adjusted their mentality, returned to society and work, and developed positive attitudes towards life.
Positive coping: Through drug treatment, psychological intervention, and moderate exercise, patients strengthened their confidence, modified negative emotions, and actively cooperated with treatment.
ECBE: Clarify themes and processes: To understand the most harmful, extensive, and high-incidence problems and in CHB care, the nursing content included identifying problem(s), expressing feelings, setting goals, and making plans.
Clarify patient needs (problem establishment): Patient's thoughts and educational needs, such as changes during illness, daily mood and reasons, family support and care, disease knowledge, support, and help were identified.
Scale assessments: Acceptance and Action Questionnaire-2nd Edition (AAQ-II), Self-Rating Anxiety Scale (SAS), Self-Rating Depression Scale (SDS), Pittsburgh Sleep Quality Index (PSQI), Exercise of Self-Care Agency Scale (ESCA), and Master of psychological flexibility, negative emotions, sleep quality, and self-care abilities scores were observed.
Goal setting Cognitive aspects: (1) CHB Education. By playing videos, issuing manuals or one-on-one communication, and conducting collective lectures, patients could fully understand the harm caused by CHB, importance of a good mentality, importance of drug treatment, and side effects; and (2) diet education. Based on the health belief model[12], a reasonable diet knowledge education plan was developed for patients to understand the importance of nutritional balance and related information. Specific information about nutritional balance for example, dietary calcium supplements (China's recommended amount of calcium is 800 mg per day), and increased fresh fruits and vegetable and protein-rich food (such as milk, poultry, fish) intake was provided. Education was delivered through videos, pictures, animations, and text.
Behavior: (1) Improved family support. Family members or spouses were included in the synchronous education program to develop basic knowledge of CHB nursing and psychological and physiological support. Family members were also instructed to create a good family atmosphere and environment, pay attention to the patients’ psychological state, and provide timely counseling to reduce the negative emotions caused by loneliness and family apathy; and (2) Improve self-care. Help was provided to patients to understand the importance of self-care and prevention and treatment of common health problems in CHB. Nursing staff focused on the mental health of patients, teaching them physical and mental adjustment methods to prevent anxiety and depression.
Psychological flexibility: Before the intervention, 3 mo after intervention, and 6 mo after, the psychological flexibility of the patients was evaluated using the AAQ-II scale[13]. The seven items were scored from 1 (never) to 7 (always) with a total score of 7-49 points. Higher scores indicated higher empirical avoidance and psychological flexibility. Cronbach's α coefficient of the scale was 0.880, indicating good reliability.
Negative emotions: The SAS and SDS[14] were used to evaluate the degree of anxiety and depression before and 6 mo after the intervention. The two scales were composed of 20 items scored according to a four-level scoring method (score 1-4 points). Higher scores indicated more severe anxiety and depression.
Sleep quality: The PSQI[15] was used to evaluate sleep quality before and after the intervention. This scale included the following seven dimensions: sleep quality, sleep time, sleep time, sleep efficiency, sleep disorders, use of hypnotic drugs, and daytime dysfunction. Each dimension was scored on a scale of 0-3 points. Higher scores indicated worse sleep quality.
Self-care ability: Before and 6 mo after the intervention[16], self-care abilities, including health knowledge (14 items), self-concept (nine items), self-responsibility (eight items), self-care skills (12 items) and four other dimensions (health knowledge level, self-concept, self-responsibility, and self-care skills). The 43 items were scored using the five-level scoring method (0-4 points). Higher scores indicated better self-care ability. Cronbach's α coefficient was 0.76-0.87, indicating good internal consistency.
SPSS 20.0 [IBM SPSS Statistics software, IBM Corp (version 20.0), NY, United States] was used to analyze the data. The data are presented as mean ± SD. The t-test was used to compare the difference between two sets of data. One-way analysis of variance was used to compare the two groups. The Bonferroni t-test was used for multiple comparisons between multiple samples. Repeated-measures analysis of variance was used to compare data at different time points between groups. The number of cases and chi-square test were used to analyze the count data. A test value = 0.05 was used. P < 0.05 was considered statistically significant.
Baseline data such as sex, age, and course of disease were compared between the two groups. No significant differences were observed (all P > 0.05), indicating comparability (Table 1).
| Group | Gender (n, male/female) | Age (mean ± SD, yr) | Number of units(n, first visit/return visit) | Course of disease (mean ± SD, yr) | Educational level (n) | Child-Pugh grade | ||||
| Course of CHB | Course of insomnia | Junior high school and below | High school | Bachelor’s degree and above | Grade A | Grade B | ||||
| Combination group (n = 60) | 38/22 | 48.36 ± 10.25 | 19/41 | 12.25 ± 3.17 | 2.51 ± 0.86 | 15 | 28 | 17 | 39 | 21 |
| Conventional group (n = 69) | 41/28 | 49.21 ± 11.12 | 24/45 | 13.07 ± 3.58 | 2.22 ± 0.88 | 18 | 31 | 20 | 42 | 27 |
| χ2/t | 0.207 | 0.449 | 0.140 | 1.368 | 1.887 | 0.041 | 0.234 | |||
| P | 0.649 | 0.654 | 0.708 | 0.174 | 0.061 | 0.980 | 0.628 | |||
The AAQ-II score in the combination group was significantly lower than that in the conventional group. The AAQ-II scores of both groups decreased with time, with an interaction effect between group and time (Fbetween-group effect = 8.548;
| Time | Combination group (n = 60) | Conventional group (n = 69) | t | P |
| Before intervention | 39.27 ± 6.22 | 38.72 ± 5.69 | 0.524 | 0.601 |
| 3 mo after intervention | 31.26 ± 7.15 | 36.28 ± 6.67 | 4.123 | < 0.001 |
| 6 mo after intervention | 28.11 ± 6.32 | 33.51 ± 6.63 | 4.715 | < 0.001 |
| F | 45.920 | 11.640 | — | — |
| P | < 0.001 | < 0.001 | — | — |
Multiple comparison results of PSQI scores at each time point between the conventional and combination groups showed significant differences in AAQ-II scores between the two time points in each group (all P < 0.05) (Table 3).
| Group | (I) Time | (J) Time | Mean difference (I-J) | Standard error | P | 95%CI | |
| Lower limit | Upper limit | ||||||
| Combination group | |||||||
| Before intervention | 3 mo after intervention | 8.017 | 1.198 | 0.001 | 5.121 | 10.913 | |
| 6 mo after intervention | 11.167 | 1.198 | 0.001 | 8.271 | 14.063 | ||
| 3 mo after intervention | before intervention | -8.017 | 1.198 | ˂0.001 | -10.913 | -5.121 | |
| 6 mo after intervention | 3.150 | 1.198 | 0.028 | 0.254 | 6.046 | ||
| 6 mo after intervention | Before intervention | -11.167 | 1.198 | 0.001 | -14.063 | -8.271 | |
| 3 mo after intervention | -3.150 | 1.198 | 0.028 | -6.046 | -0.254 | ||
| Conventional group | |||||||
| Before intervention | 3 mo after intervention | 2.449 | 1.080 | 0.073 | -0.157 | 5.056 | |
| 6 mo after intervention | 5.217 | 1.080 | 0.001 | 2.611 | 7.824 | ||
| 3 mo after intervention | Before intervention | -2.449 | 1.080 | 0.073 | -5.056 | 0.157 | |
| 6 mo after intervention | 2.768 | 1.080 | 0.033 | 0.162 | 5.375 | ||
| 6 mo after intervention | Before intervention | -5.217 | 1.080 | 0.000 | -7.824 | -2.611 | |
| 3 mo after intervention | -2.768 | 1.080 | 0.033 | -5.375 | -0.162 | ||
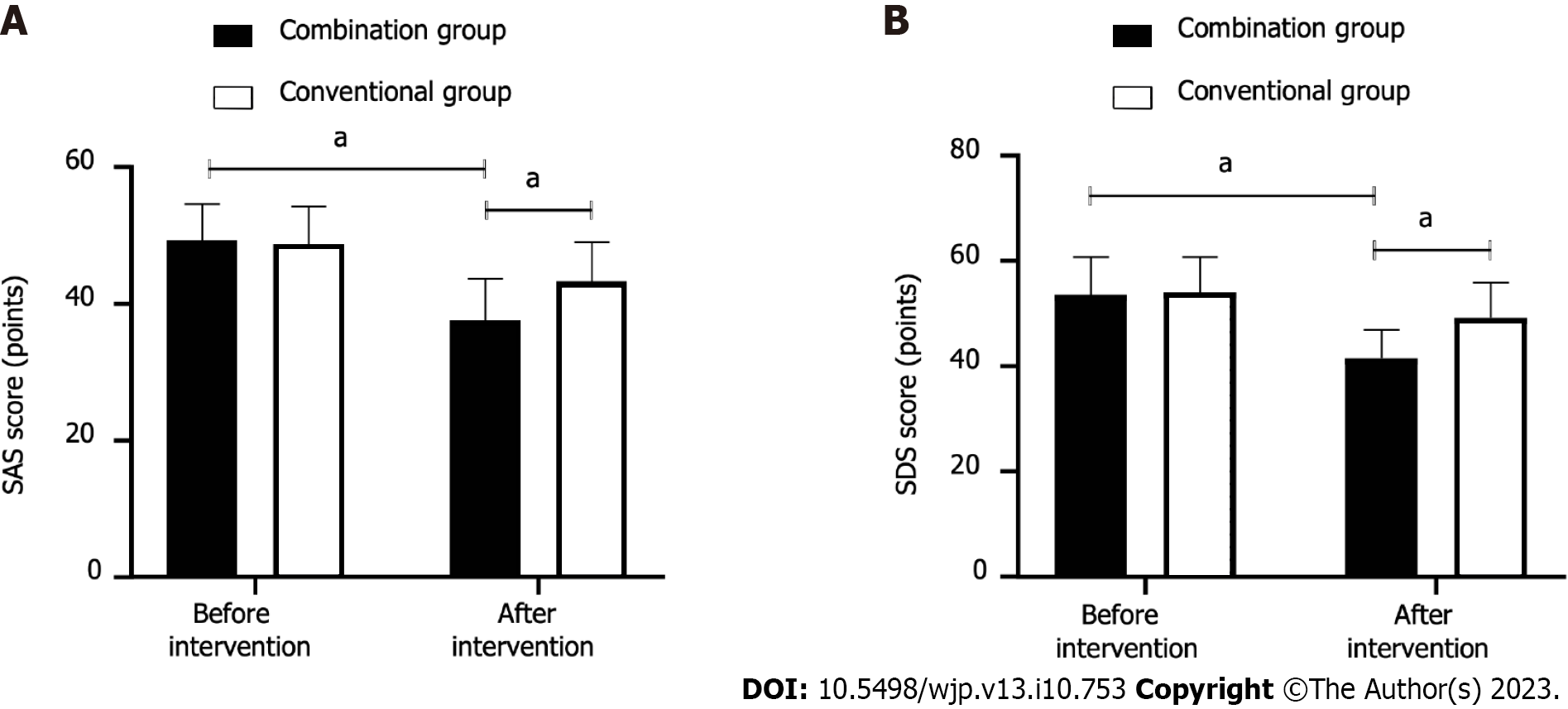
The SAS scores of the combination group were 49.25 ± 5.35 and 37.56 ± 6.11, before and after intervention, respectively; t = 11.150, P < 0.001. The SDS scores were 53.58 ± 7.12 and 41.56 ± 5.38, before and after intervention, respectively; t = 10.430, P < 0.001.
The SAS scores of the conventional group were as follows: before intervention (48.68 ± 5.52), and after intervention (43.27 ± 5.79), t = 5.618, P < 0.001. The SDS scores were, before intervention (54.03 ± 6.69), after intervention (49.20 ± 6.69), t = 4.241, P < 0.001.
In comparison with the conventional group, the SAS (t = 5.445) and SDS (t = 7.076) scores of the combination group were lower after the intervention (both P < 0.001) (Figure 2).
The post-intervention scores for sleep quality, fall sleep time, sleep time, sleep efficiency, sleep disorders, use of hypnotic drugs, daytime dysfunction, and other dimensions in the combination group and the conventional group were lower than the corresponding pre-intervention scores (all P < 0.001). The scores for each dimension in the combination group were lower than those in the conventional group (P < 0.05) (Table 4).
| Group and time | Statistics | Sleep quality | Fall sleep time | Sleep time | Sleep efficiency | Sleep disorder | Hypnotic drugs | Daytime dysfunction |
| Combination group (n = 60) | ||||||||
| Before intervention | 2.35 ± 0.65 | 2.43 ± 0.66 | 2.52 ± 0.61 | 2.33 ± 0.58 | 1.98 ± 0.52 | 2.05 ± 0.52 | 2.18 ± 0.54 | |
| After intervention | 0.82 ± 0.421 | 0.85 ± 0.441 | 0.78 ± 0.481 | 0.75 ± 0.461 | 0.77 ± 0.521 | 0.86 ± 0.361 | 1.16 ± 0.311 | |
| t | 15.310 | 15.430 | 17.360 | 16.530 | 12.750 | 14.570 | 12.690 | |
| P | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | |
| Conventional group (n = 69) | ||||||||
| Before intervention | 2.26 ± 0.57 | 2.35 ± 0.62 | 2.49 ± 0.64 | 2.29 ± 0.62 | 1.95 ± 0.47 | 2.01 ± 0.55 | 2.15 ± 0.56 | |
| After intervention | 1.06 ± 0.35 | 1.06 ± 0.53 | 0.97 ± 0.58 | 1.05 ± 0.32 | 1.02 ± 0.37 | 1.02 ± 0.22 | 1.41 ± 0.58 | |
| t | 14.900 | 13.140 | 14.620 | 14.760 | 12.910 | 13.880 | 7.624 | |
| P | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 | 0.001 |
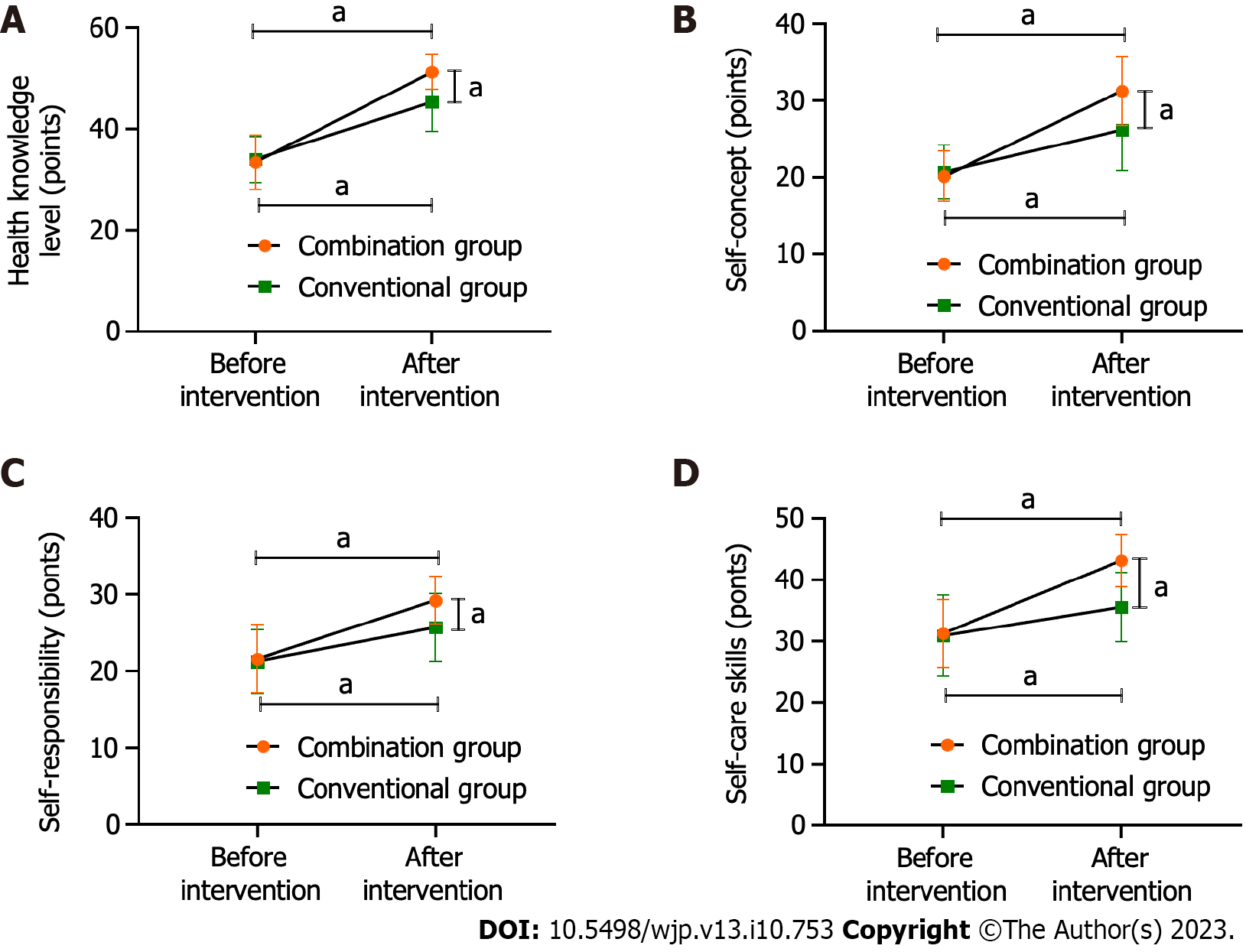
The pre-intervention scores of health knowledge level, self-concept, self-responsibility, and self-care skills in the combination group were: 33.48 ± 5.36, 20.16 ± 3.25, 21.58 ± 4.39, and 31.25 ± 5.54 points. The same pre-intervention scores in the conventional group were: 34.02 ± 4.54, 20.67 ± 3.51, 21.24 ± 4.13, and 30.86 ± 6.62 points.
After the intervention, the scores of the above dimensions in the combination group were 51.27 ± 3.39, 31.25 ± 4.42, 29.17 ± 3.08, and 43.12 ± 4.24 points. The scores in the conventional group were 45.36 ± 5.73, 26.17 ± 5.24, 25.68 ± 4.42, and 35.56 ± 5.67 points.
Scores in both groups were higher after the interventions (all P < 0.001). The scores for each dimension in the combined group were higher than those in the conventional group (t: 6.994, 5.902, 5.128, and 8.470; all P < 0.001) (Figure 3).
As CHB easily progresses to cirrhosis or liver cancer[17], there are considerable changes in the psychological, emotional, and living conditions of patients; effective nursing interventions are needed. Insomnia, a decline in sleep quality, is a common symptom in patients with CHB. primarily caused by an increase in endotoxin levels, unbalanced hormone secretion, and increased psychological burden which negatively impacts quality of life.
We found that the AAQ-II scores of both groups were lower after the intervention, and the combined group scores were lower, indicating that ACT combined with ECBE could reduce patient empirical avoidance behavior and enhance psychological flexibility. This is consistent with previous studies on adult patients with chronic pain [18]. Psychological flexibility refers to psychological and behavioral adaptations to changing situations during interactions between individuals and the environment[19], a protective factor for mental health[20].
CHB is characterized by progression to cirrhosis or liver cancer and a heavy economic burden, which can easily cause negative emotions and need for patients to escape and control their worries. ACT guides and encourages patients to accept all negative and positive experiences with an open and optimistic attitude. After ACT intervention, patients may no longer resist, control, or evade CHB but observe and accept it objectively. Additionally, patients with CHB can cope more effectively with the stimulation of surrounding environmental factors and take positive actions to reduce psychological pressure, anxiety and depression.
ECBE focuses on four aspects: Establishing problems, expressing emotions, setting goals, and formulating plans. It focuses on patients' psychological changes, unhealthy emotions, and sleep quality and adopts targeted interventions and supervision. ECBE also encourages patients to gradually reduce avoidance behaviours, anxiety, depression, insomnia, and other problems, improves psychological flexibility, and relieves negative emotions. Previous research[21] has demonstrated that psychological flexibility is closely related to anxiety and depression. According to the results of this study, the SAS and SDS scores of patients receiving ACT combined with ECBE nursing were significantly reduced, indicating that anxiety and depression were significantly alleviated, highlighting the effectiveness of the combined intervention in relieving negative emotions in patients with CHB.
In this study, the scores of the PSQI were lower and ESCA scores were higher in the combination group, demonstrating that ACT combined with ECBE also played a significant role in regulating sleep quality and patient self-care ability. The sleep quality of patients with CHB is typically much lower[22]. For ACT combined with ECBE, nursing staff developed patient knowledge of CHB and helped to correct misunderstandings about the disease, reducing excessive worrying and negative emotions, and improving sleep quality.
Moreover, the low self-care ability of patients with CHB has been demonstrated[23]. Improving self-care ability is the final step in the implementation of ECBE. Nursing staff guide patients to understand the importance of self-care and the prevention and treatment of common health problems associated with CHB. They also promote patient self-care ability, an important component that is lacking in routine nursing. Furthermore, providing effective relief from negative emotions encourages patients to actively cooperate with treatment and related auxiliary interventions, accept guidance and transmission of nursing knowledge; it also enhances patient understanding of the disease and nursing measures, indirectly improving self-care abilities[24,25].
Some limitations should be noted. First, this was a single-center study; therefore, the application of these findings to those in different centers needs to be approached with caution and the results need to be corroborated in future studies. Second, this was a retrospective study, and the data may be subject to selection, information, and confounding biases. Therefore, prospective randomized controlled studies are required to obtain more accurate clinical data and generate more robust evidence.
The combination of ACT and ECBE in patients with CHB can improve psychological flexibility and sleep quality, alleviate negative emotions, and improve self-care abilities.
Chronic hepatitis B (CHB) is an infectious, progressive disease. Patients experience a heavy psychological burden and severe insomnia symptoms.
Patients with CHB urgently require effective nursing interventions to alleviate mental flexibility, negative emotions, and sleep quality problems.
To analyze the effects of acceptance and commitment therapy (ACT) combined with enabling cognitive-behavioral education (ECBE) on mental flexibility, negative emotions, and sleep quality in CHB patients.
We retrospectively analyzed the clinical data of 129 patients with CHB and observed changes and differences in Acceptance and Action Questionnaire-2nd edition (AAQ-II), Self-Rating Anxiety Scale (SAS), Self-Rating Depression Scale (SDS), Pittsburgh Sleep Quality Index (PSQI), and Exercise of Self-Case Agency Scale (ESCA) scores after routine nursing and ACT combined with ECBE intervention.
Compared to patients receiving conventional care, the AAQ-II, SAS, SDS, and PSQI scores in patients receiving ACT combined with ECBE were lower and ESCA scores were higher.
ACT combined with ECBE is effective for CHB patients in China and overcomes the problem of nursing defects in CHB.
We observed the mental flexibility, negative emotions, and sleep quality of patients with CHB according to two different nursing interventions: routine nursing and ACT combined with ECBE.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Insel PS, Sweden; Shin H, South Korea S-Editor: Lin C L-Editor: A P-Editor: Zhang XD
| 1. | GBD 2017 Cirrhosis Collaborators. The global, regional, and national burden of cirrhosis by cause in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5:245-266. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1080] [Cited by in RCA: 992] [Article Influence: 198.4] [Reference Citation Analysis (4)] |
| 2. | Yao Y, Zhang HJ, Wang DH. Mediating effect of psychological distress on perceived stress on sleep quality in elderly patients with chronic viral hepatitis B. Zhongguo Laonianxue Zazhi. 2019;39:5627-5630. [DOI] [Full Text] |
| 3. | Loureiro D, Tout I, Narguet S, Bed CM, Roinard M, Sleiman A, Boyer N, Pons-Kerjean N, Castelnau C, Giuly N, Tonui D, Soumelis V, El Benna J, Soussan P, Moreau R, Paradis V, Mansouri A, Asselah T. Mitochondrial stress in advanced fibrosis and cirrhosis associated with chronic hepatitis B, chronic hepatitis C, or nonalcoholic steatohepatitis. Hepatology. 2023;77:1348-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 31] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 4. | Li JR, Pan JM, Liang ML, Meng HX, Meng YX. Study on the Bedside Education Video Application during the Perioperative Period of Percutaneous Nephrolithotomy. Shanghai Huli. 2019;19:13-16. [DOI] [Full Text] |
| 5. | Tomar A, Bhardwaj A, Choudhary A, Bhattacharyya D. Association of Obstructive Sleep Apnea with Nocturnal Hypoxemia in Metabolic-Associated Fatty Liver Disease Patients: A Cross-sectional Analysis of Record-based Data. J Family Med Prim Care. 2021;10:3105-3110. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Chapoutot M, Peter-Derex L, Bastuji H, Leslie W, Schoendorff B, Heinzer R, Siclari F, Nicolas A, Lemoine P, Higgins S, Bourgeois A, Vallet GT, Anders R, Ounnoughene M, Spencer J, Meloni F, Putois B. Cognitive Behavioral Therapy and Acceptance and Commitment Therapy for the Discontinuation of Long-Term Benzodiazepine Use in Insomnia and Anxiety Disorders. Int J Environ Res Public Health. 2021;18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 7. | Nolan DR, Gupta R, Huber CG, Schneeberger AR. An Effective Treatment for Tinnitus and Hyperacusis Based on Cognitive Behavioral Therapy in an Inpatient Setting: A 10-Year Retrospective Outcome Analysis. Front Psychiatry. 2020;11:25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Sakamoto R, Ohtake Y, Kataoka Y, Matsuda Y, Hata T, Otonari J, Yamane A, Matsuoka H, Yoshiuchi K. Efficacy of acceptance and commitment therapy for people with type 2 diabetes: Systematic review and meta-analysis. J Diabetes Investig. 2022;13:262-270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 9. | Zhang Z, Leong Bin Abdullah MFI, Shari NI, Lu P. Acceptance and commitment therapy versus mindfulness-based stress reduction for newly diagnosed head and neck cancer patients: A randomized controlled trial assessing efficacy for positive psychology, depression, anxiety, and quality of life. PLoS One. 2022;17:e0267887. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Liu SM, Ma YZ, Wang C, Yang QJ. Application of Acceptance Commitment Therapy in Patients after Amputation. Qilu Huli Zazhi. 2022;28:24-27. |
| 11. | Shi YW, Yang RX, Fan JG. Chronic hepatitis B infection with concomitant hepatic steatosis: Current evidence and opinion. World J Gastroenterol. 2021;27:3971-3983. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 30] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 12. | Zhao YC, Zhao M, Song S. Online Health Information Seeking Among Patients With Chronic Conditions: Integrating the Health Belief Model and Social Support Theory. J Med Internet Res. 2022;24:e42447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 13. | Zarvijani SAH, Moghaddam LF, Parchebafieh S. Acceptance and commitment therapy on perceived stress and psychological flexibility of psychiatric nurses: a randomized control trial. BMC Nurs. 2021;20:239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Zhang JW, Wang Y, Shan HH, Duan JY, Yu J. The Application of Focused Care Model in the Management of Hepatitis B Patients in a Tertiary Care Hospital and the Impact on Patients' Quality of Life. Comput Math Methods Med. 2022;2022:7770955. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 15. | Yi CH, Bair MJ, Wang JH, Wong MW, Liu TT, Lei WY, Liang SW, Lin L, Hung JS, Huang JF, Hsu YC, Chen CL. Improvement of patient-reported outcomes in patients achieving sustained virologic response with direct-acting antivirals for hepatitis C virus infection. J Microbiol Immunol Infect. 2022;55:643-650. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Cho H, Park E. Canonical Correlation Between Self-Care Agency and Health-Related Self-Efficacy with Chronic Viral Hepatitis Patients. Osong Public Health Res Perspect. 2019;10:281-288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Ji D, Chen Y, Bi J, Shang Q, Liu H, Wang JB, Tan L, Wang J, Li Q, Long Q, Song L, Jiang L, Xiao G, Yu Z, Chen L, Wang X, Chen D, Li Z, Dong Z, Yang Y. Entecavir plus Biejia-Ruangan compound reduces the risk of hepatocellular carcinoma in Chinese patients with chronic hepatitis B. J Hepatol. 2022;77:1515-1524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 37] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 18. | Godfrey E, Wileman V, Galea Holmes M, McCracken LM, Norton S, Moss-Morris R, Noonan S, Barcellona M, Critchley D. Physical Therapy Informed by Acceptance and Commitment Therapy (PACT) Versus Usual Care Physical Therapy for Adults With Chronic Low Back Pain: A Randomized Controlled Trial. J Pain. 2020;21:71-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 59] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 19. | Dai CH, Wang X, Huang QH, Zeng XM, Xu PX. Effect of acceptance and commitment therapy on psychological flexibility and posttraumatic growth in patients with stroke. Hushi Jinxiu Zazhi. 2020;35:592-595. [DOI] [Full Text] |
| 20. | Li J, Zhao N, Zhang HY, Yang H, Yang J. Analysis of the mental health status and impact factors of middle-aged and elderly patients with chronic disea-ses in a rural area of Beijing. Zhongguo Jiankang Jiaoyu. 2022;38:322-327. [DOI] [Full Text] |
| 21. | Davis AK, Barrett FS, Griffiths RR. Psychological flexibility mediates the relations between acute psychedelic effects and subjective decreases in depression and anxiety. J Contextual Behav Sci. 2020;15:39-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 187] [Article Influence: 37.4] [Reference Citation Analysis (0)] |
| 22. | Huang X, Zhang H, Qu C, Liu Y, Bian C, Xu Y. Depression and Insomnia Are Closely Associated with Thyroid Hormone Levels in Chronic Hepatitis B. Med Sci Monit. 2019;25:2672-2678. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Wu DX, Wu Y, Li YH, Wang ZY, Li Y. Correlation analysis of self-care ability, self-efficacy and social support in outpatient patients with chronic hepatitis B. Beijing Yixue. 2022;44:188-190. [DOI] [Full Text] |
| 24. | Zhou DD. Effect of empathic intervention on negative emotions and self-care ability in patients with decompensated hepatitis B cirrhosis. Yixue Linchuang Yanjiu. 2019;36:2484-2486. [DOI] [Full Text] |
| 25. | Akbulut S, Ozer A, Saritas H, Yilmaz S. Factors affecting anxiety, depression, and self-care ability in patients who have undergone liver transplantation. World J Gastroenterol. 2021;27:6967-6984. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 15] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (3)] |