Published online Jun 19, 2022. doi: 10.5498/wjp.v12.i6.787
Peer-review started: August 20, 2021
First decision: October 4, 2021
Revised: October 15, 2021
Accepted: May 5, 2022
Article in press: May 5, 2022
Published online: June 19, 2022
Processing time: 297 Days and 16.8 Hours
Treatment efficacy for attention-deficit/hyperactivity disorder (ADHD) is reported to be poor, possibly due to heterogeneity of ADHD symptoms. Little is known about poor treatment efficacy owing to ADHD heterogeneity.
To use generalized structural equation modeling (GSEM) to show how the heterogeneous nature of hyperactivity/impulsivity (H/I) symptoms in ADHD, irritable oppositional defiant disorder (ODD), and the presentation of aggression in children interferes with treatment responses in ADHD.
A total of 231 children and adolescents completed ADHD inattention and H/I tests. ODD scores from the Swanson, Nolan, and Pelham, version IV scale were obtained. The child behavior checklist (CBCL) and parent’s satisfaction questionnaire were completed. The relationships were analyzed by GSEM.
GSEM revealed that the chance of ADHD remission was lower in children with a combination of H/I symptoms of ADHD, ODD symptoms, and childhood aggressive behavior. ODD directly mediated ADHD symptom severity. The chance of reaching remission based on H/I symptoms of ADHD was reduced by 13.494% [= exp (2.602)] in children with comorbid ADHD and ODD [odds ratio (OR) = 2.602, 95% confidence interval (CI): 1.832-3.373, P = 0.000] after adjusting for the effects of other factors. Childhood aggression mediated ODD symptom severity. The chance of reaching remission based on ODD symptoms was lowered by 11.000% [= 1 - exp (-0.117)] in children with more severe baseline symptoms of aggression based on the CBCL score at study entry [OR = -0.117, 95%CI: (-0.190)-(-0.044), P = 0.002].
Mediation through ODD symptoms and aggression may influence treatment effects in ADHD after adjusting for the effects of baseline ADHD symptom severity. More attention could be directed to the early recognition of risks leading to ineffective ADHD treatment, e.g., symptoms of ODD and the presentation of aggressive or delinquent behaviors and thought problems in children with ADHD.
Core Tip: It is important to understand the factors that influence treatment outcomes for those with attention-deficit/hyperactivity disorder (ADHD). This generalized structural equation modeling pathway analysis studied heterogeneity in ADHD. We found that higher irritable oppositional defiant disorder (ODD) symptom levels mediated the treatment outcomes in children with ADHD. Treating children with ADHD is not only a matter of treating inattentive symptoms alone. Earlier recognition of risky hyperactivity/impulsivity ADHD symptoms + irritable ODD + childhood aggression as a particular subgroup and earlier provision of a more intensive combination of pharmacotherapy and cognitive behavior therapy modalities are essential.
- Citation: Tzang RF, Chang YC. Generalized structural equation modeling: Symptom heterogeneity in attention-deficit/hyperactivity disorder leading to poor treatment efficacy. World J Psychiatry 2022; 12(6): 787-800
- URL: https://www.wjgnet.com/2220-3206/full/v12/i6/787.htm
- DOI: https://dx.doi.org/10.5498/wjp.v12.i6.787
Attention-deficit/hyperactivity disorder (ADHD) is the most common neurodevelopmental disorder among children and adolescents, with a high prevalence ranging from 5.00% to 12.76%[1], and definitely needs early treatment. Although we know quite well the importance of early treatment of ADHD, approximately 25% to 30% of treated ADHD patients remain nonresponsive to treatment[2]. ADHD is a heterogeneous disorder in clinical presentation. The heterogeneity of ADHD in terms of clinical symptom profiles in children with co-occurring ADHD and oppositional defiant disorder (ODD) involves differentially higher levels of behavioral and emotional difficulties. ADHD comorbid with ODD is common and presents clinically in more than half of children with ADHD[3].
Another commonly seen clinical phenomenon is childhood aggression, which plays an essential role in the heterogeneity of ADHD. Clinically, childhood aggression commonly co-occurs in children with ADHD and ODD. As a result, these combinations of ADHD and other symptom comorbidities might further increase the highest levels of behavioral and emotional difficulties in children[4,5]. Furthermore, the treatment efficacy for ADHD in children with the commonly seen irritable subtype of ADHD presenting with childhood aggression remains ineffective. Indeed, many parents seek help from mental health experts due to irritability in children with ADHD, but they do not obtain proper treatment efficacy owing to undertreated emotional dysregulation problems associated with ADHD[6].
In the real world, up to 80% of children with ADHD report an irritable subtype of ADHD[7]; here, we examined the heterogeneity of ADHD comorbid with ODD and aggression. As we reviewed studies on ODD, comorbidities between ADHD and ODD in children ranged from at least 40.6% to 60.0%[8,9]. Children with ADHD comorbid with ODD may have inattentive or hyperactivity/impulsivity (H/I) symptoms of ADHD and frequently have temper tantrums, excessive arguments with family, and uncooperative, deliberately annoying, or mean and spiteful behavior when younger[10], but the ODD comorbidity problems in children with ADHD remain underdiagnosed[11]. The more irritable ODD symptoms noticed in children with ADHD, the more increased the risk of behavioral and emotional difficulties in these children with ADHD[12,13]. Clinically, there is more parental concern about this irritable mood associated with ADHD than inattentive symptoms of ADHD. Thus, ODD symptoms in ADHD may play mediating roles that impede treatment effects for ADHD, but little is known about these associations.
Additionally, when seeing the heterogeneity of ADHD from a childhood aggression perspective, child aggression is commonly seen in children with ADHD comorbid with ODD who have increased symptoms of irritable emotional difficulties associated with ODD[14-16]. Recently, childhood aggressive behavior was found to be closely associated with symptoms of ODD[17]. However, there is a gap in the study of childhood aggression in children with irritable ADHD because ODD commonly coexists with conduct disorder (CD)[18]. An earlier study focused more on childhood CD comorbid with ADHD. We know that any kind of childhood aggression may be a small part of the symptomatology of CD. However, in the real world, children with CD are not generally noticed in the clinic as more likely to have any kind of aggressive behavior. For example, the presentation of any kind of aggressive behavior was noticed to be as high as in 58% of preschool children[19]. A higher proportion of children with ADHD will present aggressiveness without meeting the full diagnostic criteria for CD[3]. Therefore, ODD plus aggression in children can be a bad predictor for children’s future criminal behavior, social problems, and internalizing problems[20]. There is a lack of studies examining heterogeneity across symptom dimensions of ADHD + ODD + aggression. Here, we suggest that current child ADHD expertise should use updated latent class and factor analysis to account for all related levels of heterogeneity in ADHD.
To provide an evidence-based understanding of the heterogeneity of ADHD to optimally reflect real-world variation among children with ADHD, multiple symptoms should be simultaneously evaluated. Structural equation modeling (SEM) is necessary to show the theoretical relationships among symptom heterogeneity in ADHD and poor treatment outcomes with quite different implications. Because treatment responses are usually expressed as binary data (yes/no), the traditional SEM method is not appropriate to explore the pathway of how ODD and aggression interfere with treatment efficacy for ADHD. A new pathway analysis, called generalized SEM (GSEM), can use more normally distributed observed variables by adding the logistic regression model into the SEM (StataCorp., 2013). By using GSEM pathway analysis, we can fit logistic, probit, poisson, multinomial logistic, ordered logit, ordered probit, and other models. In other words, the observed variables used in GSEM can be continuous, binary, countable, categorical, and ordered variables. GSEM can detail the pathways by which ODD mutually increases the symptom severity of ADHD (expressed by inattentive and H/I symptoms) and problematic aggressiveness. Furthermore, using GSEM pathway analysis can be a good way to detail how ODD and aggressive behavior possibly interfere with the treatment efficacy for ADHD due to their interacting joint influence on ADHD symptom severity[21].
In this study, we hypothesized that when children and adolescents with ADHD and ODD also present with any kind of aggression, treatment efficacy is poor. Regarding inattention, H/I, and ODD symptom severity and any kind of aggression at study entry, it is expected that all these risks may affect the pathways influencing treatment efficacy for ADHD. Indirectly, we hypothesized that ODD with various aggressive symptoms in children might play a mediating role in treatment efficacy for ADHD.
We used GSEM to test the hypothesis that ODD is essentially an intermediate mediator of treatment effectiveness for ADHD (in terms of odds of reaching remission or the chance of remission) by direct and indirect pathway analysis. We hope that mental health professionals can regard the combination of ODD and aggression in children with ADHD as a warning risk for difficulty achieving remission in treating the ADHD and taking earlier steps to properly manage the symptoms of ODD and the presentation of any kind of aggressive behavior.
Patients for this study were children recruited from the outpatient unit of Mackay Memorial Hospital, a major medical center in Taipei, Taiwan. The hospital’s institutional review board approved the design of the study (Institutional Review Board No: MMH-I-S-489; name of project: Exploring the symptomatology on children with internet addiction and attention deficit hyperactivity disorder and their parent). After receiving a complete description of the study, potential participants (children and their parents) provided written informed consent in line with the institutional review board’s guidelines. A total of 231 children (mean age ± standard deviation = 10.17 ± 2.59) with a clinical diagnosis of ADHD based on the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) were enrolled in this study. An experienced child and adolescent psychiatrist confirmed the clinical diagnosis of ADHD based on the DSM-IV criteria.
ADHD and ODD symptoms: The primary measures in this study reflected the core symptoms of ADHD (18 items) and ODD (8 items) as defined in the DSM-IV and included the inattention subscale, H/I subscale, and the ODD subscale of the Swanson, Nolan, and Pelham, version IV scale (SNAP-IV)[22]. Each item was scored by severity based on a 4-point scale (0-3 points, where 0: Not at all, 1: Just a little, 2: Quite a bit, and 3: Very much). The intraclass correlation coefficients for the three subscales of the Chinese-language SNAP-IV (SNAP-IV-C) ranged from 0.59 to 0.72 for the parent form and from 0.60 to 0.84 for the teacher form. All subscales of both the parent and teacher forms showed excellent internal consistency with Cronbach’s α greater than 0.88[23].
Remission rate measurements: The remission criteria on the SNAP were defined as 0 (no) or equal to 1 (yes) for each of the symptoms or a total score that was < 9 (not at all-0 or just a little-1 for the ADHD symptoms) on the SNAP after treatment. More specifically, a patient was in remission with regard to inattention, hyperactivity, and ODD if after 6 wk of treatment, the three subscales of the SNAP-IV were ≤ 9, ≤ 9, and ≤ 8, respectively. Parents and investigators rated ADHD symptoms using the SNAP-IV-C at every follow-up session to measure remission after treatment.
Aggressive behavior: The child behavior checklist (CBCL) was designed to determine competencies and behavioral problems of children aged 4-18 years. The questionnaires, completed by the parents, contain 118 items to assess specific behavioral and emotional problems. The CBCL was translated into Chinese via a two-stage translation process[24]. The internal consistency and 1-mo test-retest reliability (all α values and reliabilities > 0.6, except for thought problems) of the Chinese version were satisfactory for Taiwanese patients[25]. The present study analyzed the following 6 scales: Aggressive behaviors (tpagbeh), attention problems (tpattpr), anxiety/depression (tpandep), social problems (tpsocpr), delinquent behaviors (tpdebeh), and somatic complaints (tpsoma).
Caregiver satisfaction: To assess the medication adherence of children with ADHD, parents/caregivers completed the caregiver’s satisfaction form, which included the frequency of adverse events and the mean dose of methylphenidate (MPH), to understand the noncompliance risk. Parent/caregiver satisfaction with the current ADHD treatment was measured on a 5-point Likert scale as follows: (1) Completely dissatisfied; (2) Somewhat dissatisfied; (3) Neutral; (4) Somewhat satisfied; and (5) Completely satisfied. The only treatment was MPH (long- or short-acting formulations).
In this study, we wanted to simultaneously explore the potential relationships among the remission odds (based on inattention, H/I, and ODD symptoms) and the aforementioned measurements. We used a typical multiple-indicators and multiple-causes model. The GSEM method was used to include the logistic regression model in the SEM first with Stata 13 for Windows to test the mediation model that specified the relationships between inattention, H/I, and ODD symptom severity, any kind of aggression, and remission (StataCorp., 2013). First, we used multiple logistic regression models using GSEM notations to understand the odds of remission based on each measure. The goodness-of-fit indices in this part were P values of the fitted coefficients, deviance, and McFadden’s pseudo R2. The second part was the (combined) mediation model, which combined those three multiple logistic regression models in the first part presented by GSEM notations. All statistical analyses were performed using STATA v.13.0 (StataCorp., 2013). Statistical significance was defined as a P < 0.05.
Overall, 231 eligible patients with ADHD were enrolled. In terms of patient characteristics, 158 ADHD patients had a combined subtype (68.7%). The comorbidity rate was 73.0%. The remission rates with regard to inattention, H/I, and ODD symptoms were 30.7%, 53.7%, and 49.4%, respectively (Table 1).
| Characteristics | N | Mean, n (%) | SD |
| Age | 231 | 10.17 | 2.59 |
| Male (%) | 231 | 175 (75.8) | |
| Comorbidity | |||
| Yes | 230 | 168 (73.0) | |
| No | 230 | 62 (27.0) | |
| Subtype | |||
| Combined | 230 | 158 (68.7) | |
| Inattentive | 230 | 72 (31.3) | |
| Education | |||
| Elementary school | 228 | 171 (75.0) | |
| Junior high school | 228 | 54 (23.7) | |
| Senior high school | 228 | 3 (1.3) | |
| ADHD | |||
| Inattention | 231 | 17.19 | 4.50 |
| Hyperactivity | 231 | 12.43 | 6.46 |
| Disruptive child symptom | |||
| Oppositional defiant disorder | 231 | 12.25 | 5.82 |
| Aggression | 231 | 13.32 | 7.23 |
| Remission | |||
| Inattention | 231 | 71 (30.7) | |
| Hyperactivity | 231 | 124 (53.7) | |
| Disruptive child symptom | |||
| Oppositional defiant disorder | 231 | 114 (49.4) | |
| SCL | |||
| Somatization | 231 | 4.53 | 6.19 |
| Obsessive compulsive | 231 | 5.68 | 5.53 |
| Interpersonal sensitivity | 231 | 3.31 | 4.10 |
| Depression | 231 | 5.11 | 6.08 |
| Anxiety | 231 | 2.54 | 3.43 |
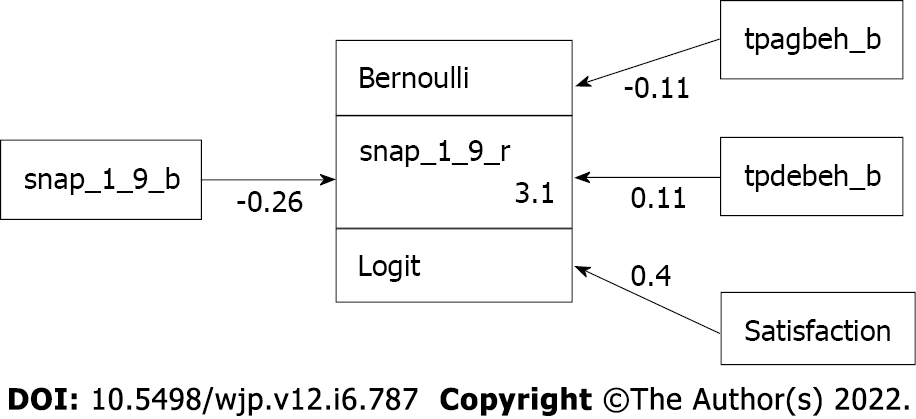
As shown in Table 2, the results of the logistic regression showed that the chance of reaching remission based on inattentive symptoms of ADHD was significantly reduced by 22.7% [= 1 - exp (-0.258)] in those with more severe inattentive symptoms [odds ratio (OR) = -0.258, 95% confidence interval (CI): (-0.350)-(-0.167), P < 0.001] after adjusting for the effects of other factors. This means that the more severe the inattention problem at study entry, the poorer the ADHD treatment response. The chance of reaching remission was significantly reduced by 10.6% [= 1 - exp (-0.112)] in those with higher baseline CBCL aggression scores [OR = -0.112, 95%CI: (-0.186)-(-0.038), P = 0.003] after adjusting for the effects of other factors. The results of deviance, D (226) = 214.144 (P = 0.704), and McFadden’s pseudo R2 = 0.2485 indicated a very good model fit (Table 2, Figure 1).
| Coef | SE | z | P value | 95%CI | |
| Remission I | |||||
| ADHD-I B | -0.258 | 0.047 | -5.53 | < 0.001 | (-0.350)-(-0.167) |
| Aggression_B | -0.112 | 0.038 | -2.96 | 0.003 | (-0.186)-(-0.038) |
| Delinquent B | 0.112 | 0.038 | 2.96 | 0.003 | 0.038-0.186 |
| Satisfaction | 0.402 | 0.147 | 2.74 | 0.006 | 0.114-0.689 |
| _cons | 3.065 | 0.834 | 3.68 | < 0.001 | 1.431-4.699 |
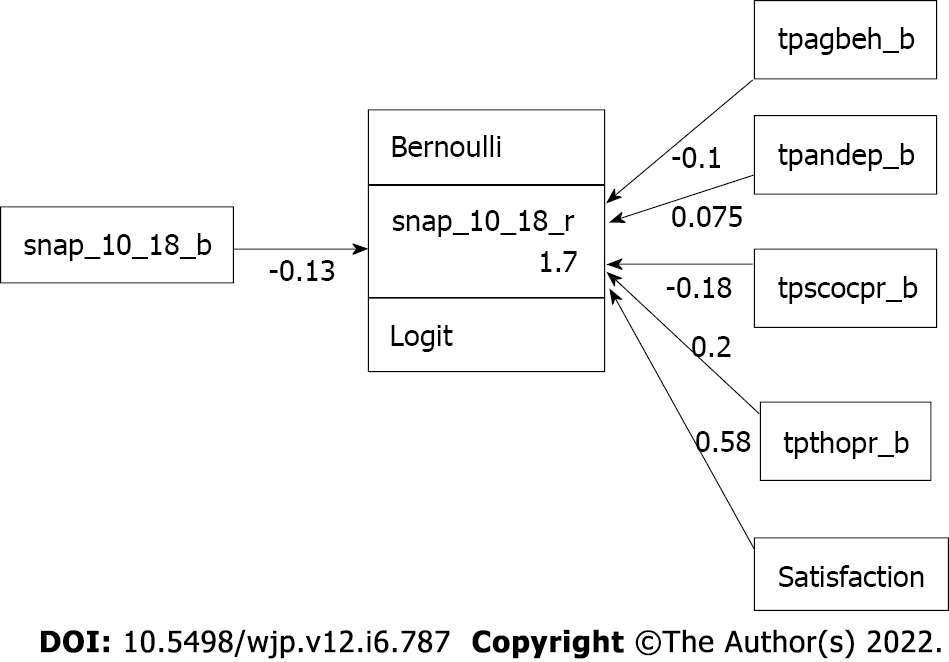
Similarly, as shown in Table 3, the chance of reaching remission based on H/I symptoms of ADHD was significantly reduced by 9.7% [= 1 - exp (-0.102)] for each increase in the baseline CBCL aggression score [OR = -0.102, 95%CI: (-0.170)-(-0.073), P = 0.004) after adjusting for the effects of other factors. Moreover, for each increase in the parental satisfaction level, the chance of reaching remission based on H/I symptoms was significantly increased by 57.4% [= exp (0.579) – 1]. The results of goodness-of-fit indices, namely, deviance and McFadden’s pseudo R2, were D (224) = 242.862 (P = 0.184) and pseudo R2= 0.2386, respectively, which indicated a very good model fit. The corresponding multiple logistic regression model presented by GSEM is shown in Figure 2.
| Coef | SE | z | P value | 95%CI | |
| Remission H/I | |||||
| ADHD-H/I B | -0.132 | 0.030 | -4.39 | < 0.001 | (-0.191)-(-0.073) |
| Aggression_B | -0.102 | 0.035 | -2.92 | 0.004 | (-0.170)-(-0.033) |
| Anx/dep B | 0.075 | 0.046 | 1.64 | 0.101 | (-0.015)-0.164 |
| Social pro. B | -0.177 | 0.076 | -2.34 | 0.019 | (-0.325)-(-0.029) |
| Thought pro. B | 0.204 | 0.070 | 2.92 | 0.004 | 0.067-0.340 |
| Satisfaction | 0.579 | 0.133 | 4.34 | < 0.001 | 0.317-0.840 |
| _cons | 1.743 | 0.518 | 3.36 | 0.001 | 0.727-2.759 |
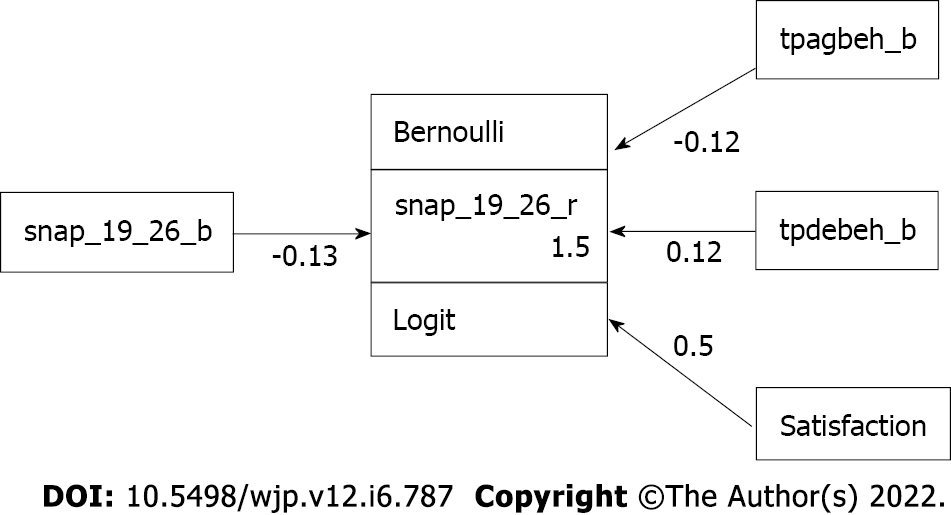
The chance of reaching remission based on ODD symptoms decreased by 11.0% [= 1 - exp (-0.117)] with each increase in the baseline CBCL aggression score [OR = -0.117, 95%CI: (-0.190)-(-0.044), P = 0.002] (Table 4). Again, the deviance and McFadden’s pseudo R2, D (226) = 255.740 (P = 0.085) and pseudo R2 = 0.2013, indicated that the model fit was good. The corresponding multiple logistic regression model of remission based on ODD symptoms presented by GSEM is shown in Figure 3.
| Coef | SE | z | P value | 95%CI | |
| Remission ODD | |||||
| ODD B | -0.130 | 0.033 | -3.97 | < 0.001 | (-0.195)-(-0.066) |
| Aggression B | -0.117 | 0.037 | -3.15 | 0.002 | (-0.190)-(-0.044) |
| Delinquent B | 0.117 | 0.037 | 3.15 | 0.002 | 0.044-0.190 |
| Satisfaction | 0.505 | 0.127 | 3.98 | < 0.001 | 0.256-0.754 |
| _cons | 1.453 | 0.516 | 2.82 | 0.005 | 0.442-2.464 |
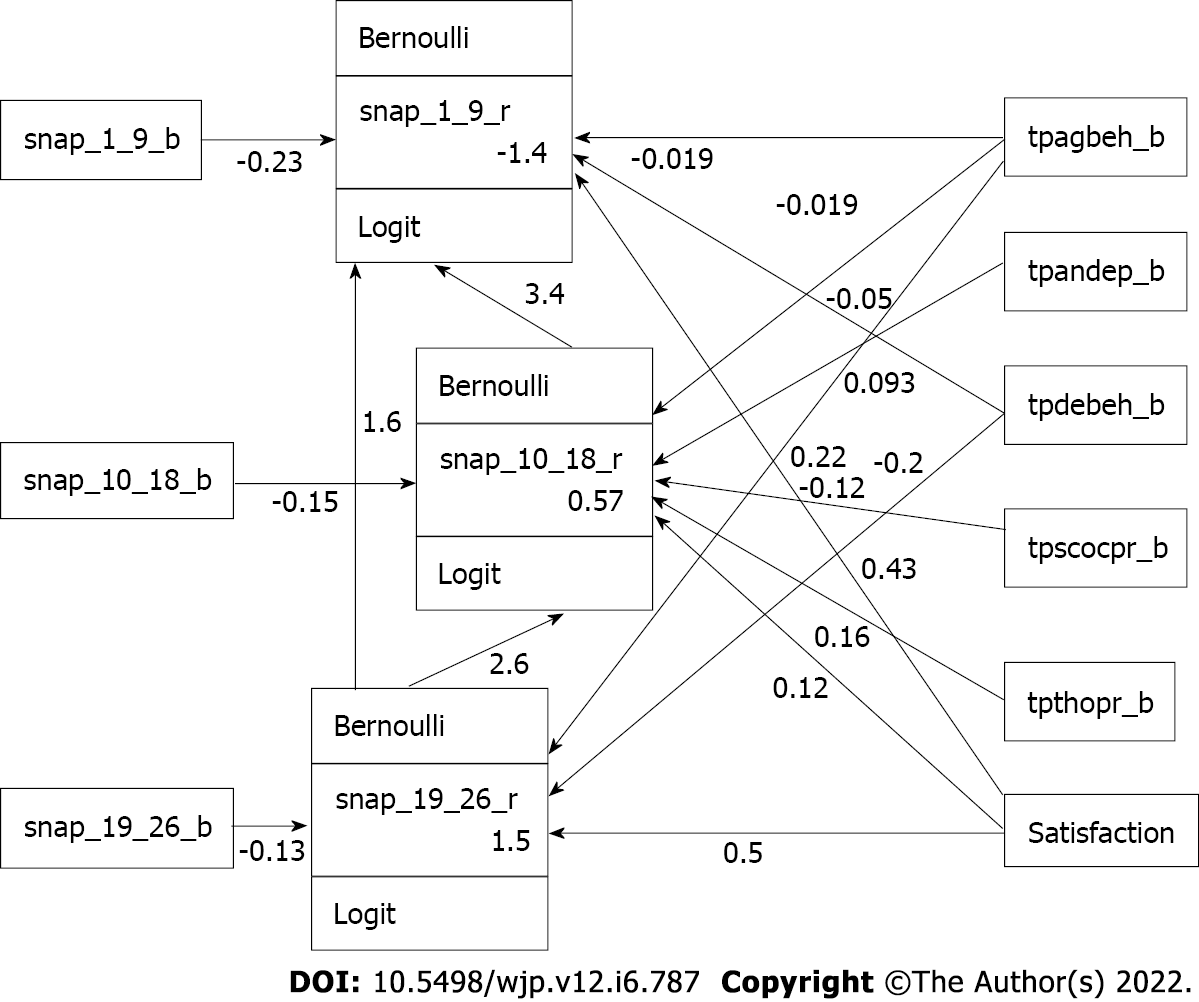
Regarding the combined (mediation) model (Table 5), we first noted that the chance of reaching remission based on H/I ADHD symptoms was reduced by 13.494% [= exp (2.602)] in the children with ODD (OR = 2.602, 95%CI: 1.832-3.373, P = 0.000) after adjusting for the effects of other factors. Moreover, the chance of reaching remission based on inattention ADHD symptoms was reduced by 29.785% [= exp (3.394)] in children with H/I ADHD symptoms (OR = 3.394, 95%CI: 1.862-4.927, P = 0.000) and reduced by 5.094% [= exp (1.628)] in children with ODD symptoms (OR = 1.628, 95%CI: 0.600-2.656, P = 0.002) after adjusting for the effects of other factors. The chance of reaching remission based on ODD symptoms was lowered by 11.000% [= 1 - exp (-0.117)] in children with more severe baseline symptoms of aggression in the CBCL scores at study entry [OR = -0.117, 95%CI: (-0.190)-(-0.044), P = 0.002]. The corresponding combined (mediation) model presented by GSEM is shown in Figure 4.
| Coef | SE | z | P value | 95%CI | |
| Remission I | |||||
| Remission H/I | 3.394 | 0.782 | 4.340 | 0.000 | 1.862-4.927 |
| Remission ODD | 1.628 | 0.524 | 3.100 | 0.002 | 0.600-2.656 |
| ADHD-I B | -0.234 | 0.058 | -4.050 | 0.000 | (-0.348)-(-0.121) |
| Aggression_B | -0.019 | 0.043 | -0.440 | 0.661 | (-0.104)-0.066 |
| Delinquent_B | 0.019 | 0.043 | 0.440 | 0.660 | -0.066-0.104 |
| Satisfaction | 0.216 | 0.173 | 1.250 | 0.212 | (-0.124)-0.556 |
| _cons | -1.433 | 1.196 | -1.200 | 0.231 | (-3.777)-0.910 |
| Remission H/I | |||||
| Remission ODD | 2.602 | 0.393 | 6.620 | 0.000 | 1.832-3.373 |
| ADHD-H/I B | -0.148 | 0.036 | -4.150 | 0.000 | (-0.218)-(-0.078) |
| Aggression_B | -0.050 | 0.039 | -1.270 | 0.205 | (-0.127)-0.027 |
| Anx/dep B | 0.093 | 0.054 | 1.710 | 0.087 | (-0.014)-0.200 |
| Social pro. B | -0.203 | 0.086 | -2.380 | 0.017 | (-0.371)-(-0.036) |
| Thought pro. B | 0.160 | 0.078 | 2.050 | 0.040 | 0.007-0.313 |
| Satisfaction | 0.431 | 0.153 | 2.810 | 0.005 | 0.130-0.731 |
| _cons | 0.567 | 0.607 | 0.930 | 0.350 | (-0.622)-1.756 |
| Remission ODD | |||||
| ODD B | -0.130 | 0.033 | -3.970 | 0.000 | (-0.195)-(-0.066) |
| Aggression_B | -0.117 | 0.037 | -3.150 | 0.002 | (-0.190)-(-0.044) |
| Delinquent B | 0.117 | 0.037 | 3.150 | 0.002 | 0.044-0.190 |
| Satisfaction | 0.505 | 0.127 | 3.980 | 0.000 | 0.256-0.754 |
| _cons | 1.453 | 0.516 | 2.820 | 0.005 | 0.442-2.464 |
This study examined the structure of ADHD symptoms in child adolescent samples using GSEM. This GSEM pathway analysis first supported that poor treatment outcomes in ADHD can be predicted as irritable ODD subtype of ADHD with aggressive behavior. This pathway analysis indicated higher ODD symptom levels mediated treatment outcomes for ADHD through enhancing inattentive and H/I symptoms. Treating children with ADHD is not only a matter of treating inattentive symptoms alone, but there is also a need to recognize and manage symptoms of ODD and the presented aggressive behavior, delinquent behavior, and thought problems in children with ADHD to improve ADHD treatment outcomes.
Hinshaw et al[26] suggested that only detailed pathway analysis can further assist clinicians in understanding the internal joint relationships among aggressive behavior, symptoms of ODD, and symptom severity of ADHD. Such pathway analysis might remind clinicians to recognize earlier risky irritable symptoms of ADHD + ODD + childhood aggression as a special subgroup and provide more effective therapeutic treatment modalities earlier.
Aggression in children and adolescents with irritable ADHD is a serious clinical and public health problem. Especially in the recent internet age, many children and adolescents present inattentive symptoms, externalizing behavior, or risk-taking behavior after excessive use of the internet[27,28]. We know that this unrecognized aggression in early childhood becomes more aggressive or violent behavior later in these irritable children[5,29]. Alternatively, the results of this study indicated that children with the irritable ODD subtype of ADHD characterized by symptoms of irritable ODD and aggressive behavior is harder to treat well. However, previous studies have focused more on conduct behavior (CD)[30,31] instead of any kind of aggression in children with ODD, which warrants more attention. Therefore, the implication of this study is that we suggest using a CBCL scale to identify aggressive children and adolescents in child and adolescent clinics or internet gaming disorder clinics in the future. The presented aggressive behavior we derived from CBCL included relational aggression (argues a lot, bragging, boasting, demands much attention), disobedience at home, disobedience at school, easily jealous, screams a lot, showing off or clowning, stubborn, sullen or irritable, sudden changes in mood or feelings, talks too much, teases a lot, temper tantrums or hot temper, direct aggression (cruelty, bullying or meanness to others, destroys his or her own things, destroys things belonging to his or her family or others), and gets in many fights (physically attacks people, threatens other people), which can all be regarded as early recognition of any kind of aggression in children with ADHD and ODD. Earlier and effective treatment inventions for children with particular heterogeneous subtypes of ADHD should be provided by ADHD experts in these days with digital technology.
In the present study, the GSEM results found that ADHD symptom severity was determined by the joint effects between ODD, aggression, and delinquent behavior symptoms. With the under recognition and undertreatment of ODD and aggression in children with ADHD, there is always a significant risk that predicts poor treatment efficacy. Here, we suggest that children and psychiatrists should record a more extensive history of oppositional symptoms because one previous study indicated that there was an underdiagnosed ODD comorbidity problem in children with ADHD[11]. The treatment effects on ODD depend on how the underlying comorbid ADHD is treated. Usually, the core symptoms of ODD are not amenable to pharmacotherapy alone[32]. For children with ADHD with ODD, treatments with only pharmacotherapy for inattention alone always remains noneffective for these ODD symptoms[33,34]. The use of nonstimulant drugs such as atomoxetine was recently noticed to be effective in treating ODD symptoms in children with ADHD[35,36]. However, for children with ADHD with severe ODD and behavioral symptoms, there is still a need to use pharmacotherapy with stimulants (MPH), mood stabilizers such as sodium valproate (Depakin), and antipsychotics such as risperidone with concurrent behavioral therapy[37].
Cognitive behavior psychotherapy in children with ADHD is also essential to regulate emotion regulation circuitry by reducing reactive aggression[38]. Essentially, clinicians should provide effective combined pharmacotherapies with additional effective behavioral modification interventions, parenting programs, and cognitive behavioral therapy to improve treatment outcomes in this particular group of children with ADHD.
Based on the pathway analysis, both ODD and aggressive symptoms interacted as joint effects to exacerbate ADHD symptom severity, as a previous study had noticed[15,16]. We revealed the insight that aggression during childhood rarely occurs alone and is closely correlated with other symptoms of childhood psychopathology. Both ODD symptoms and aggression are important influences on the efficacy of ADHD treatment[39]. Clinicians should consider additional assessments to detect dimensional behavioral symptoms such as childhood aggressive or destructive behaviors to further provide effective treatment modalities to achieve remission of ADHD[40].
Regarding the childhood H/I symptoms of ADHD, previous findings showed that hyperactive ADHD symptoms had a role in predicting children becoming more socially immature, aggressive, and peer rejected[41]. Additionally, one recent meta-analysis indicated more severe symptoms of H/I, and children with ADHD were less likely to obtain better treatment outcomes[42]. In this GSEM, we found that childhood H/I symptoms resulted in a greater risk of increasing the inattention symptom severity, leading to subsequent poor treatment outcomes for ADHD. ODD symptoms and the presentation of aggressive behavior mediated an increase in inattentive and H/I symptom severity of ADHD. Nevertheless, children and adolescents need more attention regarding the diagnosing and managing of H/I symptoms of ADHD. ODD, aggression, and H/I symptoms of ADHD interactively increased the symptom severity of ADHD.
A previous study indicated that the coexistence of a diagnosis of ODD/CD, learning difficulties, anxiety, younger age, family dysfunction, and socioeconomic adversity were all risk factors for predicting poor treatment efficacy for ADHD[43]. This pathway analysis further focused on children with ADHD with ODD, and aggression led to poor treatment outcomes. ADHD is a heterogeneous disorder with complicated emotional and impulsivity deficits. From the Research Domain Criteria perspective, ADHD patients have deficits in the domains of cognition (specifically in working memory) and positive valence (in rewarding anticipation/delay/receipt)[44]. Emotional dysregulation defects may be highly associated with abnormal reward processing systems[45]. Therefore, for children with ADHD presenting symptoms of irritable ODD and aggression, our pathway analysis suggests that the children may have deficits in both cognition and reward domains. Thus, the children with symptoms of ADHD + ODD + aggression should be a clinically distinct emotional irritability subgroup, and clinicians should provide more specific treatment guidelines for these children with ADHD. Future DSM systems need to regard ODD as an essential risk for poor treatment effects for ADHD.
This study has the following limitations. First, the construction of the subscale of the SNAP and CBCL, without a direct interview with the parents, seems to be arbitrary. Additionally, the fact that most of the scale is provided by a main caregiver, mainly mothers and teachers, may lead to sampling bias. Another limitation is the cross-sectional design of the study, which may not necessarily represent the longitudinal relationships among ADHD, ODD, aggression, and remission rate. As the main purpose of this study was to explore the association among disruptive symptoms in children and remission rates, aggression scores from the CBCL were used to represent disruptive child behaviors instead of CD measures. This was a naturalistic observational study performed in Taiwan. Most patients from the outpatient department at that time received psychopharmacologic treatment, including short-term or long-acting MPH, or long-acting drugs such as atomoxetine rather than parenting behavior therapy. However, the thrust of this study was to predict poor treatment efficacy in the children with co-occurring ADHD, ODD, and aggressive symptoms by special GSEM statistical analysis. Therefore, we did not show the detailed treatment response after different kinds of drugs or other psychosocial interventions. Finally, the definitions of direct, indirect, and total effects in SEM have not yet been established in the GSEM. Although three out of four requirements for the mediation model were satisfied in our GSEM, it might not be appropriate to call the results in Figure 4 a mediation model. Here, we only borrowed the concept and spirit of the mediation model to emphasize the relationships among remissions based on ODD, H/I, and inattention symptoms for treating children with ADHD.
Despite these limitations, to the best of our knowledge, this is the first study to determine mediators in reaching remission of ADHD. ODD is a categorical diagnosis, and aggressive behavior is a dimensional problem. Such interactive categorical and dimensional information provides an added dimension in the understanding of the etiology of heterogenicity of ADHD. This pathway study revealed additional insights into devising more efficacious pharmacotherapies and cognitive behavior therapies. Clinicians should regard ADHD + ODD + aggression comorbidity as a distinct entity that needs an early and combined intensive biopsychosocial model approach, as recent research demonstrated[46]. Future longitudinal and systemic research is needed to validate this as a potential obstacle, with the ODD symptoms dynamically interacting with childhood aggressive behavior symptoms.
GSEM pathway analysis was used to demonstrate that disruptive childhood symptoms, including categorical diagnoses such as ODD and dimensional problems such as aggressive symptoms before treatment, apparently lower the remission rate for those with ADHD. This paper suggests that clinicians should directly examine the joint effects of ADHD, ODD, and aggression to assess the risk for poor treatment outcomes. An early and more intensive combined biopsychosocial model approach for ADHD should be warranted for these children.
Many parents seek help from mental health experts due to irritability in children with attention-deficit/hyperactivity disorder (ADHD). But treatment efficacy for irritable and aggressive ADHD in children remains ineffective. Therefore, the heterogeneity to ADHD treatment should be proposed by a specific mathematical method.
Treating children with ADHD is not only a matter of treating inattentive symptoms alone. It is important to understand the factors that influence treatment outcomes for those with ADHD.
This study used the generalized structural equation modeling (GSEM) pathway analysis to analyze heterogeneity in ADHD.
We used the GSEM to test the hypothesis that ODD is essentially an intermediate mediator of treatment effectiveness for ADHD (in terms of odds of reaching remission or the chance of remission) by direct and indirect pathway analysis.
Higher irritable oppositional defiant disorder (ODD) symptom levels mediated the treatment outcomes in children with ADHD. Earlier recognition of risky hyperactivity/impulsivity ADHD symptoms + irritable ODD + childhood aggression as a particular subgroup and earlier provision of a more intensive combination of pharmacotherapy and cognitive behavior therapy modalities are essential.
Treating children with ADHD is not only a matter of treating inattentive symptoms alone, but there is also a need to recognize and manage symptoms of ODD and the presented aggressive behavior, delinquent behavior, and thought problems in children with ADHD to improve ADHD treatment outcomes.
Poor treatment outcomes in ADHD can be predicted as irritable ODD subtype of ADHD with aggressive behavior. An early and more intensive combined biopsychosocial model approach for ADHD should be warranted for these children. This study revealed additional insights into devising more efficacious pharmacotherapies and cognitive behavior therapies.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Xiong A, China S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Wang JJ
| 1. | Ercan ES, Kandulu R, Uslu E, Ardic UA, Yazici KU, Basay BK, Aydın C, Rohde LA. Prevalence and diagnostic stability of ADHD and ODD in Turkish children: a 4-year longitudinal study. Child Adolesc Psychiatry Ment Health. 2013;7:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Spencer TJ, Abikoff HB, Connor DF, Biederman J, Pliszka SR, Boellner S, Read SC, Pratt R. Efficacy and safety of mixed amphetamine salts extended release (adderall XR) in the management of oppositional defiant disorder with or without comorbid attention-deficit/hyperactivity disorder in school-aged children and adolescents: A 4-week, multicenter, randomized, double-blind, parallel-group, placebo-controlled, forced-dose-escalation study. Clin Ther. 2006;28:402-418. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 53] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | McBurnett K, Pfiffner LJ. Treatment of aggressive ADHD in children and adolescents: conceptualization and treatment of comorbid behavior disorders. Postgrad Med. 2009;121:158-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Mandy W, Roughan L, Skuse D. Three dimensions of oppositionality in autism spectrum disorder. J Abnorm Child Psychol. 2014;42:291-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Stringaris A, Goodman R. Three dimensions of oppositionality in youth. J Child Psychol Psychiatry. 2009;50:216-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 251] [Cited by in RCA: 247] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 6. | Sullivan EL, Holton KF, Nousen EK, Barling AN, Sullivan CA, Propper CB, Nigg JT. Early identification of ADHD risk via infant temperament and emotion regulation: a pilot study. J Child Psychol Psychiatry. 2015;56:949-957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 57] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 7. | Karalunas SL, Gustafsson HC, Fair D, Musser ED, Nigg JT. Do we need an irritable subtype of ADHD? Psychol Assess. 2019;31:236-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 90] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 8. | Kadesjö C, Hägglöf B, Kadesjö B, Gillberg C. Attention-deficit-hyperactivity disorder with and without oppositional defiant disorder in 3- to 7-year-old children. Dev Med Child Neurol. 2003;45:693-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Elia J, Ambrosini P, Berrettini W. ADHD characteristics: I. Concurrent co-morbidity patterns in children & adolescents. Child Adolesc Psychiatry Ment Health. 2008;2:15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 134] [Cited by in RCA: 117] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 10. | Ogundele MO. Behavioural and emotional disorders in childhood: A brief overview for paediatricians. World J Clin Pediatr. 2018;7:9-26. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 287] [Cited by in RCA: 177] [Article Influence: 25.3] [Reference Citation Analysis (20)] |
| 11. | Yuki K, Bhagia J, Mrazek D, Jensen PS. How does a real-world child psychiatric clinic diagnose and treat attention deficit hyperactivity disorder? World J Psychiatry. 2016;6:118-127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 12. | Kuhne M, Schachar R, Tannock R. Impact of comorbid oppositional or conduct problems on attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 1997;36:1715-1725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 124] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 13. | Frick PJ, Nigg JT. Current issues in the diagnosis of attention deficit hyperactivity disorder, oppositional defiant disorder, and conduct disorder. Annu Rev Clin Psychol. 2012;8:77-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 149] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 14. | Biederman J, Ball SW, Monuteaux MC, Kaiser R, Faraone SV. CBCL clinical scales discriminate ADHD youth with structured-interview derived diagnosis of oppositional defiant disorder (ODD). J Atten Disord. 2008;12:76-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Becker SP, Luebbe AM, Fite PJ, Greening L, Stoppelbein L. Oppositional defiant disorder symptoms in relation to psychopathic traits and aggression among psychiatrically hospitalized children: ADHD symptoms as a potential moderator. Aggress Behav. 2013;39:201-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Holtmann M, Goth K, Wöckel L, Poustka F, Bölte S. CBCL-pediatric bipolar disorder phenotype: severe ADHD or bipolar disorder? J Neural Transm (Vienna). 2008;115:155-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 61] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 17. | Ghosh A, Ray A, Basu A. Oppositional defiant disorder: current insight. Psychol Res Behav Manag. 2017;10:353-367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 18. | Tuvblad C, Zheng M, Raine A, Baker LA. A common genetic factor explains the covariation among ADHD ODD and CD symptoms in 9-10 year old boys and girls. J Abnorm Child Psychol. 2009;37:153-167. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 98] [Cited by in RCA: 88] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 19. | Tremblay RE, Nagin DS, Séguin JR, Zoccolillo M, Zelazo PD, Boivin M, Pérusse D, Japel C. Physical aggression during early childhood: trajectories and predictors. Pediatrics. 2004;114:e43-e50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 698] [Cited by in RCA: 503] [Article Influence: 24.0] [Reference Citation Analysis (1)] |
| 20. | Sitnick SL, Galán CA, Shaw DS. Early childhood predictors of boys' antisocial and violent behavior in early adulthood. Infant Ment Health J. 2019;40:67-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Sibley MH, Pelham WE, Molina BS, Waschbusch DA, Gnagy EM, Babinski DE, Biswas A. Inconsistent self-report of delinquency by adolescents and young adults with ADHD. J Abnorm Child Psychol. 2010;38:645-656. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 44] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 22. | Swanson JM, Kraemer HC, Hinshaw SP, Arnold LE, Conners CK, Abikoff HB, Clevenger W, Davies M, Elliott GR, Greenhill LL, Hechtman L, Hoza B, Jensen PS, March JS, Newcorn JH, Owens EB, Pelham WE, Schiller E, Severe JB, Simpson S, Vitiello B, Wells K, Wigal T, Wu M. Clinical relevance of the primary findings of the MTA: success rates based on severity of ADHD and ODD symptoms at the end of treatment. J Am Acad Child Adolesc Psychiatry. 2001;40:168-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 725] [Cited by in RCA: 719] [Article Influence: 30.0] [Reference Citation Analysis (0)] |
| 23. | Liu YC, Liu SK, Shang CY, Lin CH, Tu C, Gau SS. Norm of the Chinese Version of the Chinese version of the Swanson, Nolan, and Pelham, version IV scale for ADHD. Taiwanese J Psychiatry. 2006;20:290-304. |
| 24. | Huang HL, Chuang SF, Wang YC. Developing the multiaxial behavioral assessment of children in Taiwan. In: Chinese Assessment Association, editor. Psychological Assessment in Chinese-Speaking Society. Taipei: Psychology Press, 1994: 259-310. |
| 25. | Yang HJ, Soong WT, Chiang CN, Chen WJ. Competence and behavioral/emotional problems among Taiwanese adolescents as reported by parents and teachers. J Am Acad Child Adolesc Psychiatry. 2000;39:232-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 96] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 26. | Hinshaw SP, Owens EB, Zalecki C, Huggins SP, Montenegro-Nevado AJ, Schrodek E, Swanson EN. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into early adulthood: continuing impairment includes elevated risk for suicide attempts and self-injury. J Consult Clin Psychol. 2012;80:1041-1051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 209] [Article Influence: 16.1] [Reference Citation Analysis (0)] |
| 27. | Tamana SK, Ezeugwu V, Chikuma J, Lefebvre DL, Azad MB, Moraes TJ, Subbarao P, Becker AB, Turvey SE, Sears MR, Dick BD, Carson V, Rasmussen C; CHILD study Investigators, Pei J, Mandhane PJ. Screen-time is associated with inattention problems in preschoolers: Results from the CHILD birth cohort study. PLoS One. 2019;14:e0213995. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 164] [Cited by in RCA: 135] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 28. | Rikkers W, Lawrence D, Hafekost J, Zubrick SR. Internet use and electronic gaming by children and adolescents with emotional and behavioural problems in Australia - results from the second Child and Adolescent Survey of Mental Health and Wellbeing. BMC Public Health. 2016;16:399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 66] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 29. | Anderson NE, Kiehl KA. Psychopathy and aggression: when paralimbic dysfunction leads to violence. Curr Top Behav Neurosci. 2014;17:369-393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 30. | Pringsheim T, Hirsch L, Gardner D, Gorman DA. The pharmacological management of oppositional behaviour, conduct problems, and aggression in children and adolescents with attention-deficit hyperactivity disorder, oppositional defiant disorder, and conduct disorder: a systematic review and meta-analysis. Part 2: antipsychotics and traditional mood stabilizers. Can J Psychiatry. 2015;60:52-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 63] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 31. | Connor DF, Doerfler LA. ADHD with comorbid oppositional defiant disorder or conduct disorder: discrete or nondistinct disruptive behavior disorders? J Atten Disord. 2008;12:126-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 75] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 32. | Hood BS, Elrod MG, DeWine DB. Treatment of Childhood Oppositional Defiant Disorder. Curr Treat Options Peds. 2015;1:155-167. [DOI] [Full Text] |
| 33. | Gajria K, Lu M, Sikirica V, Greven P, Zhong Y, Qin P, Xie J. Adherence, persistence, and medication discontinuation in patients with attention-deficit/hyperactivity disorder - a systematic literature review. Neuropsychiatr Dis Treat. 2014;10:1543-1569. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 107] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 34. | Frank E, Ozon C, Nair V, Othee K. Examining why patients with attention-deficit/hyperactivity disorder lack adherence to medication over the long term: a review and analysis. J Clin Psychiatry. 2015;76:e1459-e1468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 41] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 35. | Mueller AK, Fuermaier AB, Koerts J, Tucha L. Stigma in attention deficit hyperactivity disorder. Atten Defic Hyperact Disord. 2012;4:101-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 154] [Cited by in RCA: 133] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 36. | Asherson P, Stes S, Nilsson Markhed M, Berggren L, Svanborg P, Kutzelnigg A, Deberdt W. The effects of atomoxetine on emotional control in adults with ADHD: An integrated analysis of multicenter studies. Eur Psychiatry. 2015;30:511-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 37. | Jahangard L, Akbarian S, Haghighi M, Ahmadpanah M, Keshavarzi A, Bajoghli H, Sadeghi Bahmani D, Holsboer-Trachsler E, Brand S. Children with ADHD and symptoms of oppositional defiant disorder improved in behavior when treated with methylphenidate and adjuvant risperidone, though weight gain was also observed - Results from a randomized, double-blind, placebo-controlled clinical trial. Psychiatry Res. 2017;251:182-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 38. | Sukhodolsky DG, Vander Wyk BC, Eilbott JA, McCauley SA, Ibrahim K, Crowley MJ, Pelphrey KA. Neural Mechanisms of Cognitive-Behavioral Therapy for Aggression in Children and Adolescents: Design of a Randomized Controlled Trial Within the National Institute for Mental Health Research Domain Criteria Construct of Frustrative Non-Reward. J Child Adolesc Psychopharmacol. 2016;26:38-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 39. | Connor DF, Steeber J, McBurnett K. A review of attention-deficit/hyperactivity disorder complicated by symptoms of oppositional defiant disorder or conduct disorder. J Dev Behav Pediatr. 2010;31:427-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 131] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 40. | Baweja R, Belin PJ, Humphrey HH, Babocsai L, Pariseau ME, Waschbusch DA, Hoffman MT, Akinnusi OO, Haak JL, Pelham WE, Waxmonsky JG. The Effectiveness and Tolerability of Central Nervous System Stimulants in School-Age Children with Attention-Deficit/Hyperactivity Disorder and Disruptive Mood Dysregulation Disorder Across Home and School. J Child Adolesc Psychopharmacol. 2016;26:154-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 41. | Carpenter Rich E, Loo SK, Yang M, Dang J, Smalley SL. Social functioning difficulties in ADHD: association with PDD risk. Clin Child Psychol Psychiatry. 2009;14:329-344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 58] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 42. | Xue J, Hao Y, Li X, Guan R, Wang Y, Li Y, Tian H. Meta-Analysis Study on Treatment of Children's Attention Deficit Disorder with Hyperactivity. J Healthc Eng. 2021;2021:8229039. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 43. | Young S, Asherson P, Lloyd T, Absoud M, Arif M, Colley WA, Cortese S, Cubbin S, Doyle N, Morua SD, Ferreira-Lay P, Gudjonsson G, Ivens V, Jarvis C, Lewis A, Mason P, Newlove-Delgado T, Pitts M, Read H, van Rensburg K, Zoritch B, Skirrow C. Failure of Healthcare Provision for Attention-Deficit/Hyperactivity Disorder in the United Kingdom: A Consensus Statement. Front Psychiatry. 2021;12:649399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 46] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 44. | Musser ED, Raiker JS Jr. Attention-deficit/hyperactivity disorder: An integrated developmental psychopathology and Research Domain Criteria (RDoC) approach. Compr Psychiatry. 2019;90:65-72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 45. | Nusslock R, Alloy LB. Reward processing and mood-related symptoms: An RDoC and translational neuroscience perspective. J Affect Disord. 2017;216:3-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 216] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 46. | Saylor KE, Amann BH. Impulsive Aggression as a Comorbidity of Attention-Deficit/Hyperactivity Disorder in Children and Adolescents. J Child Adolesc Psychopharmacol. 2016;26:19-25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 73] [Article Influence: 8.1] [Reference Citation Analysis (0)] |