Published online Jul 19, 2021. doi: 10.5498/wjp.v11.i7.337
Peer-review started: February 8, 2021
First decision: May 5, 2021
Revised: May 13, 2021
Accepted: June 23, 2021
Article in press: June 23, 2021
Published online: July 19, 2021
Processing time: 157 Days and 10 Hours
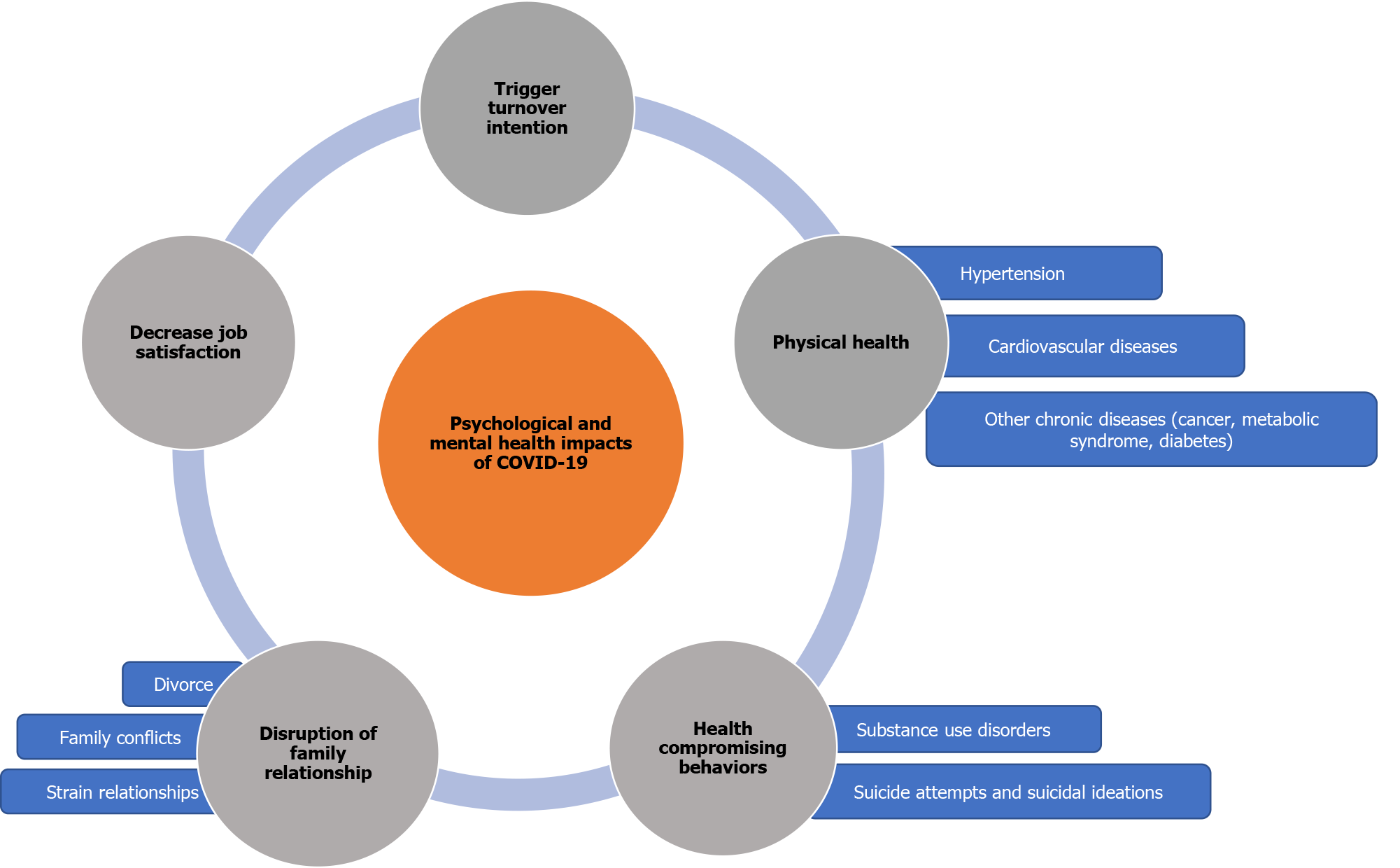
The coronavirus disease-19 (COVID-19) pandemic has put healthcare workers in an unprecedented situation, increasing their psychological and mental health distress. Much research has focused on the issues surrounding anxiety, depression, and stress among healthcare workers. The consequences of mental health problems on healthcare workers’ physical health, health-compromising behaviours, suicide ideation, family relationships, and job satisfaction during the COVID-19 pandemic are not well studied. Enhanced psychological stress has known effects on an individual’s physical health. In healthcare workers with pre-existing comorbidities, psychological stressors may exacerbate their current health problems. Healthcare professionals are known to have a high risk of substance use, hence they may be at risk of development of substance use addiction or vulnerable to addiction relapse. Frontline COVID-19 healthcare workers are being pushed above and beyond their limits, possibly resulting in suicidal tendencies. Furthermore, the burden of high workload and burnout may also have serious manifestations in relationships with family and an intention to quit their jobs. Future studies should explore the above-mentioned deleterious consequences to provide insight into the development of mental healthcare strategies to combat the psychological impact of COVID-19 on healthcare workers during the COVID-19 emergency. It is imperative to employ strategies to care for and policies to protect the psychological well-being of healthcare workers.
Core Tip: Much has been investigated surrounding the issue of anxiety, depression, and stress during the coronavirus disease-19 (COVID-19) pandemic among the healthcare workers in China. Nonetheless, the consequences of psychological and mental distress on healthcare workers’ physical health, general well-being, family relationships, job satisfaction, and anticipated turnover are not well studied. We herein discuss the multi-faceted consequences of psychological and mental health on healthcare workers in China during the COVID-19 pandemic. This review also highlights the important areas overlooked in research and mental health policies.
- Citation: Cai CZ, Lin YL, Hu ZJ, Wong LP. Psychological and mental health impacts of COVID-19 pandemic on healthcare workers in China: A review. World J Psychiatr 2021; 11(7): 337-346
- URL: https://www.wjgnet.com/2220-3206/full/v11/i7/337.htm
- DOI: https://dx.doi.org/10.5498/wjp.v11.i7.337
Coronavirus disease-19 (COVID-19) infection was first reported in Wuhan, China in December 2019, and spread rapidly throughout China. Just 3 mo later, the World Health Organization (WHO) declared the spread of the COVID-19 as a pandemic. In a short one year, the COVID-19 pandemic has become a major global health crisis. While the pandemic is still a crisis in many countries worldwide, China has managed to control the pandemic rapidly and effectively in just over 3 mo after its onset[1]. As of the end of December 2020, China had confirmed 96324 cases of COVID-19 and 4777 deaths, while there have been over 79.2 million cases and over 1.7 million deaths globally since the start of the pandemic[2].
The COVID-19 pandemic is not only a threat to human life. Beyond the direct impacts of the virus, the mental health of the entire population is profoundly impacted. More importantly, the psychological and mental health of healthcare workers has been greatly challenged during this pandemic owing to their often extensive and close contact with COVID-19 patients in healthcare settings. High rates of infections and deaths among the healthcare workers involved in the fight against COVID-19 are causing them to experience high levels of distress and fear[3,4]. Worldwide, COVID-19 has affected large numbers of frontline healthcare workers. As of April 8, 2020, the WHO estimated that over 20000 health workers in 52 countries had contracted COVID-19[5]. In China, the outbreak has forced health professionals to work under extreme pressure and uncertainty, battling the novel coronavirus that is not fully understood and has claimed many lives. In a short intense 3 mo of battle against the coronavirus, the outbreak has exerted significant negative psychological impacts on healthcare professionals, particularly frontline health workers. A study of over 72000 patients with COVID-19 by the Chinese Centre for Disease Control and Prevention showed that around 3000 healthcare workers had become infected by February, accounting for 3.8% of all cases of COVID-19[6]. In addition to the fear of contagion during the early phase of the outbreak, healthcare workers in Wuhan also faced enormous pressure, including inadequate protection from contamination, work burden, isolation, witnessing patients suffering and dying, a lack of contact with their families, fear of transmitting the disease to families and loved ones, and exhaustion, which collectively contributed to serious mental health problems such as stress, anxiety, depressive symptoms, and insomnia[4,7].
Since the onset of the pandemic, there have been many published studies on the mental health of healthcare workers in the COVID-19 pandemic in China and other countries impacted by the COVID-19 pandemic. There were also several systematic reviews and meta-analyses that synthesised the findings of all published studies. A systematic review and meta-analysis of 13 studies of mental health during the COVID-19 pandemic published up to April 17, 2020, of which 12 were from China and one from Singapore, reported a pooled prevalence of 23.2% for anxiety, 22.8% for depression, and 38.9% for insomnia[8]. An integrative review of the mental health of healthcare professionals in China during the new coronavirus pandemic found intense psychological experiences, traumatization, and various mental health disorders among healthcare workers, while also describing the importance of self-coping and psychological needs[9]. A recently published meta-analysis of eight studies of frontline healthcare workers in China reported that the pooled prevalence of depression and anxiety was 31.5% and 23.7%, respectively[10], which was relatively higher than the former.
Although much has been investigated surrounding the issue of psychological and mental health impacts of the COVID-19 pandemic, most of the current published literature and reviews have investigated the level of anxiety, depression, and stress. The negative consequences of psychological and mental impacts during the era of the COVID-19 pandemic remain a relatively neglected area of inquiry. Among these are physical health, health-compromising behaviours, such as substance use disorders, suicide attempts or suicidal ideation, the disruption of family relationships, and the intention to leave jobs. To date, it has been over a year since COVID-19 first emerged in China. Many countries in the world are facing a resurgence of COVID-19 cases as the pandemic progresses. Healthcare workers in China may once again resume the COVID-19 battlefield and continue facing psychological distress. In light of the preceding discussion, this article discusses the multi-faceted consequences of psychological and mental health on healthcare workers in China during the COVID-19 pandemic.
Recent research continues to demonstrate that poor mental health is related to adverse physical health[11]. Mounting evidence is showing associations between psychological distress and physical health such as hypertension and cardiovascular diseases[12]. Emerging evidence indicates that the COVID-19 pandemic has posed significant psychological stress on the community with emerging cardiovascular implications[13]. Recent reports show the link between emotional pressure caused by COVID-19 and takotsubo cardiomyopathy presenting as acute heart failure[14]. Despite this, increasing trends in the prevalence of chronic diseases are not prominent. This could be due to a large delay in treatment-seeking during the pandemic[13]. Henceforth, public as well as healthcare workers with pre-existing cardiovascular comorbidities and psychological stressors may exacerbate their current health conditions. More importantly, a study in China showed that patients with hypertension were associated with severe outcomes from COVID-19[15]. Furthermore, there is also a significant association between the fatality rate in COVID-19 patients and cardiovascular metabolic diseases[16]. As in many developing countries, in China, hypertension remains a pervasive problem among Chinese adults. Results from the China Hypertension Survey 2012–2015 stated that 23.2% (approximately 244.5 million) of the Chinese adult population ≥ 18 years of age had hypertension[17]. The high prevalence of cardiovascular risk factors was also reported among healthcare workers in China and is of growing concern. The prevalence of hypertension among nurses in China was reported to be close to 30%[18]. Although it is well established that stressful life events are a factor mediating the progression of chronic diseases such as cancer growth and development of metastases[19], as well as metabolic syndrome and type II diabetes mellitus[20], direct evidence linking to COVID-19 pandemic related stress has yet been reported. Considering that untreated psychological and mental health problems may cause severe physical health problems, it is of utmost importance not to downplay the psychological and mental health of healthcare workers with cardiovascular risk factors or chronic illnesses during their fight against COVID-19.
Thus, it is essential to build a work environment where there is some recognition of mental health as a dangerous risk factor to physical health, particularly during the current pandemic situation. Raising awareness of mental health as a dangerous risk factor to physical health is also important because mental health literacy may help an individual to cope, seek help, or self-advocate for health improvement[21]. Having a workplace mental health policy that looks into the well-being of healthcare staff with health issues or comorbidities is of paramount importance. Local evidence on the interlink of physical and mental health problems remains a crucial area of investigation in China.
The COVID-19 pandemic has serious implications for people with substance use disorders. Fear of contagion, uncertainty and anxiety, social distancing and isolation, loneliness, and economic repercussions were among the factors that promote substance use during the pandemic[22]. Deaths from alcohol, drugs, and suicide, collectively known as “deaths of despair”, are receiving growing international attention[23,34]. According to the findings of a study from the Well Being Trust released in May 2020, an estimate of 75000 “deaths of despair” associated with drug, alcohol, and suicide has been directly related to the COVID-19 pandemic[25]. Recently, it is estimated that the number of “deaths of despair” could double up to 150000 due to the pandemic’s slow recovery[26]. Stressful events have long been known to also cause increased substance use risk in healthcare workers[27-29]. An issue that is overlooked in the COVID-19 pandemic crisis among healthcare workers is the reactive behaviour to negative impacts of disasters such as the development of addiction and addiction relapse vulnerability. There has been a report of an increase in substance use among people who have existing substance problems in China in the era of the COVID-19 pandemic[30]. Nevertheless, to date, relatively little has been reported in substance use among healthcare workers in China during the COVID-19 pandemic. Healthcare workers may similarly be vulnerable to substance use disorders during the COVID-19 pandemic. In a previous report, post-traumatic stress disorder (PTSD) and alcohol abuse or dependence symptoms 3 years post Beijing's 2003 SARS outbreak were prevalent among hospital employees who lived through the outbreak[31]. Substance use prevention and cessation support should be provided in healthcare settings. Increased substance abuse during the COVID-19 pandemic among people without a substance abuse history has not been reported and warrants further observation. Despite this, psychological intervention and advice for preventing substance use during the COVID-19 pandemic should be disseminated to the public at large and specifically targeted at people with a history of substance abuse. Given the amount of intensified psychological and mental issues facing medical care workers during the pandemic, understanding the extent and nature of healthcare workers’ substance use disorders is essential for appropriate psychosocial management and successful treatment. However, the stigma associated with substance use disorders covers the entire trajectory of diagnosis, prevention, treatment, and recovery; hence, this is a major obstacle for healthcare-providers seeking diagnosis and treatment. There is a need to sensitise the public and healthcare organisations about addiction-related issues among healthcare workers during this pandemic. Family members' awareness and involvement in the treatment of substance use disorders are imperative[32]. Health systems should also facilitate access to substance use disorder treatment for healthcare workers, particularly those with pre-existing psychiatric conditions.
Suicide is a worldwide phenomenon and studies have shown that suicide deaths are related to mental health disorders. There is growing concern that multiple lines of evidence point towards the increase in the rates of suicide attempts and completed suicides during the COVID-19 pandemic[22,32-35]. The profound pandemic related psychological impacts associated with prolonged social isolation, loneliness, fear of COVID-19 infection, uncertainty, occupational deprivation, and economic difficulties lead to the development or exacerbation of depression and anxiety, and ultimately aggravate vulnerability to suicidal thoughts and behaviours[22]. Vulnerable populations to the exacerbation of psychological or mental-related disorders and suicidal thoughts include individuals with pre-existing psychiatric disorders, less resilient people, those living in high COVID-19 prevalence areas, and people who have lost loved ones to COVID-19[36,37]. People in the medical-related profession have also been known to have a high prevalence of suicide attempts and suicidal ideation[38]. It was noted that the COVID-19 pandemic has increased the risk of suicide among healthcare workers due to the increased psychological distress, including witnessing COVID-19 patients’ deaths, a lack of feelings of control, personal blame for the inability to do more for patients, and increased working hours[39]. Suicide cases among healthcare workers have been reported across many countries including the United States, England, Italy, Mexico, and India[40-42].
In China, relatively little has been reported on suicidal ideation or suicide attempts among the healthcare workers in Wuhan, the epicentre of the coronavirus outbreak, despite a high level of psychological and mental disorders during the early phase of the outbreak. China has promptly launched a psychological intervention and mental health support system to cope with the widespread psychological stress during the COVID-19 pandemic[43,44]. Psychological assistance hotlines providing online psychological counselling services have been established by mental health professionals in medical institutions, universities, and academic societies throughout all provinces and regions in mainland China, which provide free 24-h services that were widely made available to the public and healthcare workers. The online psychological self-help intervention systems include online cognitive behavioural therapy for depression, anxiety, and insomnia[45]. Of note, the current literature is lacking on suicide attempts or suicidal ideation in healthcare workers in China. It is unclear whether the lack of evidence is due to under-reporting or under-diagnosis. It is well known that despite the high rates of depressive and anxiety disorders among physicians, dealing with suicide is challenging as stigma and embarrassment prevent a large number of them from seeking care for mental health diagnosis and treatment[46].
Although the COVID-19 pandemic is largely under control in China now, PSTD in the aftermath of the COVID-19 pandemic is an issue that should not be overlooked. The impact on mental health can be long-lasting for large-scale crisis events like the COVID-19 pandemic[47]. The distressing events of the past 3 mo, particularly among the frontline healthcare workers providing care to patients with COVID-19, witnessing the pandemic’s massive death and trauma, could lead to long-term mental health problems. A study reported that a total of 3.8% of 377 healthcare workers in China reported PTSD a month after the outbreak and those with PTSD had a significantly higher probability of experiencing poor sleep quality[48]. Another study of 863 medical care workers from seven provinces in China reported that 40.2% were positive for PTSD[49]. PTSD is known to be a risk factor for suicide and was found to account for 0.6% of suicides in men and 3.5% in women[50]. The psychological sequelae of the pandemic will probably persist for months and years to come and suicide is probably going to become an even more significant concern as the pandemic unfolds[35]. Suicide prevention research emphasises that building meaningful social connections and interventions to decrease burdensomeness among healthcare workers are urgently needed.
The coronavirus pandemic has profound negative emotional impacts affecting personal and family harmony worldwide. The fear and uncertainty associated with pandemics provide an enabling environment that may aggravate family conflicts or violence in a family or relationship[51-53]. Prolonged lockdown and long-term home isolation measures and the stress of the COVID-19 pandemic have aggravated family conflicts and strained relationships, leading to a variety of family problems, including family violence and divorce. In China, after the 2-mo lockdown, the number of cases of family violence and divorces surged in March[51]. It is unclear if the strain of life under lockdown has contributed to the increase in divorce rate as the unprecedented number of divorces could also be due to backlog in cases as the pandemic has forced offices to close for months. Little is known about whether the adverse psychological or mental health of healthcare workers during the COVID-19 pandemic has negative effects on their families or personal lives. It is well established that the high workload of healthcare workers has restricted their family life, leading to burnout and distress, which consequently have serious manifestations on family relationships and marital complications[54,55].
More research is needed to assess the experience of family turbulence due to the COVID-19 pandemic among healthcare workers in China. Sudden changes in daily work lives during the pandemic and high exposure to psychological distress are situations that put healthcare providers at an increased risk of negative effects on family relationships. Policies should take into consideration the implications of the pandemic on the family members of healthcare providers. Current mental health services and interventions for healthcare providers should adopt a more holistic approach, including supportive care for their family members and loved ones.
As the pandemic progressed, evidence began to show a deterioration in the psychological and mental well-being of healthcare workers, resulting in decreased job satisfaction and triggering turnover intention[56,57]. In China, although the statistics of healthcare workers quitting their jobs during the COVID-19 pandemic are unknown, poor psychological well-being and heightened turnover intention were evident in healthcare workers fighting COVID-19 during the peak of the outbreak[58,59]. It is crucial for healthcare workers to feel satisfied with their jobs during the COVID-19 pandemic. Poor level job satisfaction among healthcare workers during the COVID-19 pandemic has been reported in several studies worldwide. Mean occupational satisfaction of 3.6 (score range, 1-5) was reported during the COVID-19 pandemic among Israeli nurses[60]. Job satisfaction score of 2.8 (out of a possible score of 4) was reported in a large-scale study among healthcare workers in Italy[61]. Large-scale empirical study assessing the level of job satisfaction of healthcare workers in China is lacking. To date, two small-scale studies reported a job satisfaction score of 32 (out of possible 48)[59] and 82 (out of possible 100)[62] in healthcare workers in China during the COVID-19 pandemic. Further large-scale studies are warranted to accurately determine the level of job satisfaction of healthcare workers in China in the era of the COVID-19 pandemic. The shortage of healthcare professionals in China is an issue that has long been at the forefront of the healthcare industry before the COVID-19 pandemic, and the COVID-19 pandemic has simply increased the demand for healthcare professionals in China, resulting in the heightened importance of preventing the loss of the medical workforce in the healthcare service[63]. It is important to identify specific psychological or work problems surrounding poor job satisfaction and turnover intention among healthcare workers to enable more accurate targeted interventions. The catastrophic toll on mental health, inadequate protection, and fear of safety, along with that of their families, may cause many healthcare workers to choose to step away from their jobs[58]. As the need for medical doctors continues to increase with the world facing the unprecedented global health threat of coronavirus infection, the government must do everything in its power to retain employees in the healthcare setting.
The summary of psychological and mental health impacts of COVID-19 pandemic discussed is illustrated in Figure 1.
There is a need to recognise the adverse consequences of psychological and mental health problems on the well-being of healthcare workers. Poor psychological and mental health among healthcare workers is harmful not only to themselves, but also to their patients, families, organisations, and healthcare services. The public, healthcare organisations, and government authorities should be made aware of the manifestations of mental health among healthcare workers, their correlations, and the fact that any strategies to manage them must encompass all levels of society. The lacunae in the existing literature on the consequences of psychological and mental problems on healthcare workers may need to be completed over time through further research. Psychiatry and psychological first aid should be considered broadly during a crisis such as the COVID-19 pandemic. Efforts to destigmatise help-seeking behaviour for psychological and mental health problems are warranted. A workplace mental health strategy and policy are essential for a healthy workplace environment during a pandemic crisis.
Manuscript source: Invited manuscript
Specialty type: Behavioral sciences
Country/Territory of origin: Malaysia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Li BF S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Ma YJ
| 1. | Burki T. China's successful control of COVID-19. Lancet Infect Dis. 2020;20:1240-1241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 95] [Article Influence: 19.0] [Reference Citation Analysis (1)] |
| 2. | WHO. COVID-19 Weekly Epidemiological Update. [cited 29 Dec 2020]. Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update---29-december-2020. |
| 3. | Zhu Z, Xu S, Wang H, Liu Z, Wu J, Li G, Miao J, Zhang C, Yang Y, Sun W, Zhu S, Fan Y, Chen Y, Hu J, Liu J, Wang W. COVID-19 in Wuhan: Sociodemographic characteristics and hospital support measures associated with the immediate psychological impact on healthcare workers. EClinicalMedicine. 2020;24:100443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 156] [Cited by in RCA: 183] [Article Influence: 36.6] [Reference Citation Analysis (0)] |
| 4. | Hu D, Kong Y, Li W, Han Q, Zhang X, Zhu LX, Wan SW, Liu Z, Shen Q, Yang J, He HG, Zhu J. Frontline nurses' burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study. EClinicalMedicine. 2020;24:100424. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 401] [Cited by in RCA: 467] [Article Influence: 93.4] [Reference Citation Analysis (0)] |
| 5. |
WHO.
Situation Report Coronavirus Disease 2019 (Covid-19) Situation Report–82. [cited 11 Apr 2020]. Available from: |
| 6. | Epidemiology Working Group for NCIP Epidemic Response; Chinese Center for Disease Control and Prevention. [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China]. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41:145-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1341] [Reference Citation Analysis (0)] |
| 7. | Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, Wang Y, Hu J, Lai J, Ma X, Chen J, Guan L, Wang G, Ma H, Liu Z. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7:e14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1321] [Cited by in RCA: 1060] [Article Influence: 212.0] [Reference Citation Analysis (0)] |
| 8. | Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020;88:901-907. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1812] [Cited by in RCA: 2251] [Article Influence: 450.2] [Reference Citation Analysis (0)] |
| 9. | Paiano M, Jaques AE, Nacamura PAB, Salci MA, Radovanovic CAT, Carreira L. Mental health of healthcare professionals in China during the new coronavirus pandemic: an integrative review. Rev Bras Enferm. 2020;73:e20200338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 10. | Bareeqa SB, Ahmed SI, Samar SS, Yasin W, Zehra S, Monese GM, Gouthro RV. Prevalence of depression, anxiety and stress in china during COVID-19 pandemic: A systematic review with meta-analysis. Int J Psychiatry Med. 2021;56:210-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 108] [Article Influence: 27.0] [Reference Citation Analysis (0)] |
| 11. | Ohrnberger J, Fichera E, Sutton M. The relationship between physical and mental health: A mediation analysis. Soc Sci Med. 2017;195:42-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 274] [Cited by in RCA: 412] [Article Influence: 51.5] [Reference Citation Analysis (0)] |
| 12. | Cuevas AG, Williams DR, Albert MA. Psychosocial Factors and Hypertension: A Review of the Literature. Cardiol Clin. 2017;35:223-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 72] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 13. | Tsamakis K, Triantafyllis AS, Tsiptsios D, Spartalis E, Mueller C, Tsamakis C, Chaidou S, Spandidos DA, Fotis L, Economou M, Rizos E. COVID-19 related stress exacerbates common physical and mental pathologies and affects treatment (Review). Exp Ther Med. 2020;20:159-162. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 42] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 14. | Meyer P, Degrauwe S, Van Delden C, Ghadri JR, Templin C. Typical takotsubo syndrome triggered by SARS-CoV-2 infection. Eur Heart J. 2020;41:1860. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 123] [Cited by in RCA: 142] [Article Influence: 28.4] [Reference Citation Analysis (0)] |
| 15. | Huang S, Wang J, Liu F, Liu J, Cao G, Yang C, Liu W, Tu C, Zhu M, Xiong B. COVID-19 patients with hypertension have more severe disease: a multicenter retrospective observational study. Hypertens Res. 2020;43:824-831. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 133] [Cited by in RCA: 136] [Article Influence: 27.2] [Reference Citation Analysis (0)] |
| 16. | Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, Bi Z, Zhao Y. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109:531-538. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1374] [Cited by in RCA: 1237] [Article Influence: 247.4] [Reference Citation Analysis (0)] |
| 17. | Wang Z, Chen Z, Zhang L, Wang X, Hao G, Zhang Z, Shao L, Tian Y, Dong Y, Zheng C, Wang J, Zhu M, Weintraub WS, Gao R; China Hypertension Survey Investigators. Status of Hypertension in China: Results From the China Hypertension Survey, 2012-2015. Circulation. 2018;137:2344-2356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 681] [Cited by in RCA: 1183] [Article Influence: 169.0] [Reference Citation Analysis (0)] |
| 18. | Zhao B, Li J, Liu J, Hao Y, Zhen Y, Feng D, Xu M, Chen X, Yang X, Zuo A, Jia R, Zhang R, Fan A, Wang Y, Yuan M, Tong L, Chen S, Cui J, Zhao M, Cui W. Hypertension prevalence alteration in 92 815 nurses based on the new standard by 2017 ACC/AHA hypertension guideline: observational cross-sectional study from China. BMJ Open. 2019;9:e027201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Mravec B, Tibensky M, Horvathova L. Stress and cancer. Part I: Mechanisms mediating the effect of stressors on cancer. J Neuroimmunol. 2020;346:577311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 51] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 20. | Rutters F, Pilz S, Koopman AD, Rauh SP, Pouwer F, Stehouwer CD, Elders PJ, Nijpels G, Dekker JM. Stressful life events and incident metabolic syndrome: the Hoorn study. Stress. 2015;18:507-513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 21. | Kutcher S, Wei Y, Coniglio C. Mental Health Literacy: Past, Present, and Future. Can J Psychiatry. 2016;61:154-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 371] [Article Influence: 41.2] [Reference Citation Analysis (0)] |
| 22. | Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020;113:707-712. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 503] [Cited by in RCA: 542] [Article Influence: 108.4] [Reference Citation Analysis (0)] |
| 23. | Chiappini S, Guirguis A, John A, Corkery JM, Schifano F. Front Psychiatry. 2020; COVID-19: The Hidden Impact on Mental Health and Drug Addiction. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 89] [Cited by in RCA: 91] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 24. | Allik M, Brown D, Dundas R, Leyland AH. Deaths of despair: cause-specific mortality and socioeconomic inequalities in cause-specific mortality among young men in Scotland. Int J Equity Health. 2020;19:215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 25. |
Petterson S, Westfall JM, Miller BF.
Projected deaths of despair from COVID-19. Well Being Trust 2020. Available from: |
| 26. | Ward M. Pandemic-related ‘deaths of despair’ were forecase at about 75,000 back in May- now they could be up to 150,000. Business Insider 26 Aug 2020. Available from: https://www.businessinsider.com/coronavirus-deaths-suicide-drugs-alcohol-depression-unemployment-2020-8. |
| 27. | Bennett J, O’Donovan D. Substance misuse by doctors, nurses and other healthcare workers. Curr Opin Psychiatry. 2001;14:195-199. [DOI] [Full Text] |
| 28. | Saridi M, Karra A, Kourakos M, Souliotis K. Assessment of alcohol use in health professionals during the economic crisis. Br J Nurs. 2016;25:396-398, 400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 29. | McKay D, Asmundson GJG. Substance use and abuse associated with the behavioral immune system during COVID-19: The special case of healthcare workers and essential workers. Addict Behav. 2020;110:106522. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 30. | Sun Y, Li Y, Bao Y, Meng S, Sun Y, Schumann G, Kosten T, Strang J, Lu L, Shi J. Brief Report: Increased Addictive Internet and Substance Use Behavior During the COVID-19 Pandemic in China. Am J Addict. 2020;29:268-270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 219] [Cited by in RCA: 263] [Article Influence: 52.6] [Reference Citation Analysis (0)] |
| 31. | Wu P, Liu X, Fang Y, Fan B, Fuller CJ, Guan Z, Yao Z, Kong J, Lu J, Litvak IJ. Alcohol abuse/dependence symptoms among hospital employees exposed to a SARS outbreak. Alcohol Alcohol. 2008;43:706-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 246] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 32. | Lander L, Howsare J, Byrne M. The impact of substance use disorders on families and children: from theory to practice. Soc Work Public Health. 2013;28:194-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 206] [Cited by in RCA: 213] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 33. | Bachmann S. Epidemiology of Suicide and the Psychiatric Perspective. Int J Environ Res Public Health. 2018;15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 642] [Cited by in RCA: 761] [Article Influence: 108.7] [Reference Citation Analysis (0)] |
| 34. | Simon GE, Rutter CM, Peterson D, Oliver M, Whiteside U, Operskalski B, Ludman EJ. Does response on the PHQ-9 Depression Questionnaire predict subsequent suicide attempt or suicide death? Psychiatr Serv. 2013;64:1195-1202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 360] [Cited by in RCA: 399] [Article Influence: 33.3] [Reference Citation Analysis (0)] |
| 35. | Joseph SJ, Bhandari SS. Dealing with the rising tide of suicides during the COVID-19 pandemic: Strengthening the pillars of prevention and timely intervention. Int J Soc Psychiatry. 2020;20764020962146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 36. |
Dunmore R.
Coronavirus-related suicides surface amid increased anxiety. Newsone. [cited 31 Mar 2020]. Available from: |
| 37. |
Lieberman JA, Olfson M.
Meeting the mental health challenge of the COVID-19 pandemic. Psychiatric Times. 25 Apr 2020. Available from: |
| 38. | Dutheil F, Aubert C, Pereira B, Dambrun M, Moustafa F, Mermillod M, Baker JS, Trousselard M, Lesage FX, Navel V. Suicide among physicians and health-care workers: A systematic review and meta-analysis. PLoS One. 2019;14:e0226361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 270] [Cited by in RCA: 281] [Article Influence: 46.8] [Reference Citation Analysis (0)] |
| 39. | Kingston AM. Break the Silence: Physician Suicide in the Time of COVID-19. Mo Med. 2020;117:426-429. [PubMed] |
| 40. | Kapilan N. Suicides cases among nurses in India due to COVID-19 and possible prevention strategies. Asian J Psychiatr. 2020;54:102434. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 41. | Gulati G, Kelly BD. Physician suicide and the COVID-19 pandemic. Occup Med (Lond). 2020;kqaa104. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 42. | Rahman A, Plummer V. COVID-19 related suicide among hospital nurses; case study evidence from worldwide media reports. Psychiatry Res. 2020;291:113272. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 55] [Article Influence: 11.0] [Reference Citation Analysis (0)] |
| 43. | Ju Y, Zhang Y, Wang X, Li W, Ng RMK, Li L. China's mental health support in response to COVID-19: progression, challenges and reflection. Global Health. 2020;16:102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 44. | Chen Q, Liang M, Li Y, Guo J, Fei D, Wang L, He L, Sheng C, Cai Y, Li X, Wang J, Zhang Z. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e15-e16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1253] [Cited by in RCA: 1236] [Article Influence: 247.2] [Reference Citation Analysis (0)] |
| 45. | Liu S, Yang L, Zhang C, Xiang YT, Liu Z, Hu S, Zhang B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020;7:e17-e18. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1118] [Cited by in RCA: 1087] [Article Influence: 217.4] [Reference Citation Analysis (0)] |
| 46. | Ross M. Suicide among physicians. A psychological study. Dis Nerv Syst. 1973;34:145-150. [PubMed] |
| 47. | Galea S, Merchant RM, Lurie N. The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention. JAMA Intern Med. 2020;180:817-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1231] [Cited by in RCA: 1257] [Article Influence: 251.4] [Reference Citation Analysis (0)] |
| 48. | Yin Q, Sun Z, Liu T, Ni X, Deng X, Jia Y, Shang Z, Zhou Y, Liu W. Posttraumatic stress symptoms of health care workers during the corona virus disease 2019. Clin Psychol Psychother. 2020;27:384-395. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 152] [Cited by in RCA: 131] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 49. | Si MY, Su XY, Jiang Y, Wang WJ, Gu XF, Ma L, Li J, Zhang SK, Ren ZF, Ren R, Liu YL, Qiao YL. Psychological impact of COVID-19 on medical care workers in China. Infect Dis Poverty. 2020;9:113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 123] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 50. | Fox V, Dalman C, Dal H, Hollander AC, Kirkbride JB, Pitman A. Suicide risk in people with post-traumatic stress disorder: A cohort study of 3.1 million people in Sweden. J Affect Disord. 2021;279:609-616. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 60] [Article Influence: 15.0] [Reference Citation Analysis (0)] |
| 51. | Zhang H. The Influence of the Ongoing COVID-19 Pandemic on Family Violence in China. J Fam Violence. 2020;1-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 52. | Pereda N, Díaz-Faes DA. Family violence against children in the wake of COVID-19 pandemic: a review of current perspectives and risk factors. Child Adolesc Psychiatry Ment Health. 2020;14:40. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 117] [Cited by in RCA: 85] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 53. | Usher K, Bhullar N, Durkin J, Gyamfi N, Jackson D. Family violence and COVID-19: Increased vulnerability and reduced options for support. Int J Ment Health Nurs. 2020;29:549-552. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 627] [Cited by in RCA: 436] [Article Influence: 87.2] [Reference Citation Analysis (0)] |
| 54. | Balch CM, Freischlag JA, Shanafelt TD. Stress and burnout among surgeons: understanding and managing the syndrome and avoiding the adverse consequences. Arch Surg. 2009;144:371-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 263] [Cited by in RCA: 287] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 55. | Zil-E-Ali A, Awana MT, Aadil M. Relationship Issues and High Divorce Rate among Surgeons. J Coll Physicians Surg Pak. 2017;27:739-740. [PubMed] |
| 56. | Giménez-Espert MDC, Prado-Gascó V, Soto-Rubio A. Psychosocial Risks, Work Engagement, and Job Satisfaction of Nurses During COVID-19 Pandemic. Front Public Health. 2020;8:566896. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 121] [Cited by in RCA: 131] [Article Influence: 26.2] [Reference Citation Analysis (0)] |
| 57. | Zhang SX, Chen J, Afshar Jahanshahi A, Alvarez-Risco A, Dai H, Li J, Patty-Tito RM. Succumbing to the COVID-19 Pandemic-Healthcare Workers Not Satisfied and Intend to Leave Their Jobs. Int J Ment Health Addict. 2021;1-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 75] [Article Influence: 18.8] [Reference Citation Analysis (0)] |
| 58. | Li Q, Chen J, Xu G, Zhao J, Yu X, Wang S, Liu L, Liu F. The Psychological Health Status of Healthcare Workers During the COVID-19 Outbreak: A Cross-Sectional Survey Study in Guangdong, China. Front Public Health. 2020;8:562885. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 59. | Zhang X, Bian L, Bai X, Kong D, Liu L, Chen Q, Li N. The influence of job satisfaction, resilience and work engagement on turnover intention among village doctors in China: a cross-sectional study. BMC Health Serv Res. 2020;20:283. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 44] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 60. | Savitsky B, Radomislensky I, Hendel T. Nurses' occupational satisfaction during Covid-19 pandemic. Appl Nurs Res. 2021;59:151416. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 63] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 61. | Puci MV, Nosari G, Loi F, Puci GV, Montomoli C, Ferraro OE. Risk Perception and Worries among Health Care Workers in the COVID-19 Pandemic: Findings from an Italian Survey. Healthcare (Basel). 2020;8:535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 62. | Yu X, Zhao Y, Li Y, Hu C, Xu H, Zhao X, Huang J. Factors Associated With Job Satisfaction of Frontline Medical Staff Fighting Against COVID-19: A Cross-Sectional Study in China. Front Public Health. 2020;8:426. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 63. | Wu Q, Zhao L, Ye XC. Shortage of healthcare professionals in China. BMJ. 2016;354:i4860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 49] [Article Influence: 5.4] [Reference Citation Analysis (0)] |