Published online Dec 19, 2021. doi: 10.5498/wjp.v11.i12.1328
Peer-review started: February 23, 2021
First decision: July 15, 2021
Revised: July 19, 2021
Accepted: November 20, 2021
Article in press: November 20, 2021
Published online: December 19, 2021
Processing time: 294 Days and 17.8 Hours
A recent meta-analysis has confirmed that the effects of psychotherapy on patients with borderline personality disorders (BPD) are still insufficiently understood. Evidence of differences between different types of therapies has been questioned.
To study repetitive interaction patterns in patients with BPD undergoing either psychoanalysis or psychodynamic therapy.
Psychoanalysis (PSA) or psychodynamic psychotherapy (PDT) was administered to 10 patients each, the two groups were matched. Therapy regimens were applied according to care as usual/manualized including quality control and supervision as usual. Randomization to one of the groups was done after baseline assessment. During classical PSA (n = 10) and PDT (n = 10), semiannually, recordings (audio or video) of five consecutive therapy sessions were taken over three years for an ex-post analysis. The patients' characteristics, such as affect parameters [Affect regulation and experience Q-sort (AREQ)], quality of object relations (quality of object relations scale) and personality traits [Shedler-Westen Assessment Procedure (SWAP-200)] were analyzed retrospectively by independent raters. Therapeutic action (psychotherapy process Q-sort) and affective (re)actions of the patients (AREQ) were then analyzed in relation to changes found in the patients' characteristics.
During the first year of therapy (PSA: n = 10; PDT: n = 9), the therapeutic method PSA was associated with significant improvements in the variable "SWAP Borderline", while in PDT change was not significantly different to baseline (PSA: P = 0.04; PDT: P = 0.33). Long-term results and follow up was available for seven participants in PSA and for five in PDT after three years; change in SWAP borderline for the whole sample was not significant at this time point when confronting to baseline (P = 0.545). However, differences between PSA and PDT were significant when analyzing the “mean change” in the SWAP Borderline variable after one year of therapy (P = 0.024): PSA led to slightly increased BPD symptoms, while PDT to a decrease; for the long run, variance of observed change was higher in PSA than in PDT (SDPSA ± 9.29 vs SDPDT ± 7.94). Our assumption that transference interpretations, closely followed by affective changes in the patient, could be useful modes of interaction was reproducible in our findings, especially when looking at the descriptive findings in the long-term data. The analysis of repetitive interaction structures demonstrated a very specific "time-lag" between therapeutic intervention and a corresponding increase in positive affect in successful therapy cases.
Exploring the change processes in the patients' characteristics and linking these changes to specific treatment strategies is of clinical importance when starting treatment and for its long-term progress.
Core Tip: This is a retrospective study to evaluate similarities and differences between psychoanalysis (PSA) and psychodynamic psychotherapy (PDT) in patients with borderline personality disorder. Both treatments were adequately effective. However, interactional aspects varied between PSA and PDT, requiring further investigation and consideration in therapy.
- Citation: Steinmair D, Wong G, Frantal S, Rohm C, Löffler-Stastka H. Affect regulation in psychoanalytic treatments of patients with a borderline personality disorder–psychoanalysis and psychodynamic psychotherapy–a comparison. World J Psychiatr 2021; 11(12): 1328-1345
- URL: https://www.wjgnet.com/2220-3206/full/v11/i12/1328.htm
- DOI: https://dx.doi.org/10.5498/wjp.v11.i12.1328
In treatment research and outcome studies, the specific factors within the therapeutic process which lead to clinically significant progress are often not as apparent as one might hope. This applies to classical psychoanalysis (PSA)[1] as well as to psychoanalytically oriented psychotherapy/psychodynamic psychotherapy (PDT)[2]. There is a lack of empirical data, particularly studies regarding psychoanalytic techniques, demonstrating the need for further research in this field[3]. Studies examining factors at work in the psychoanalytic process which determine outcome measures are rare[4,5]. A major objective in psychoanalytic process research is the identification and validation of factors that lead to structural change and changes in maladaptive emotional patterns[6]. Intended for evaluating treatment progress, by examining process factors in connection to outcome measures, the following variables were of importance for the present study.
One important point is that experiences that are affectively meaningful[7] and/or affects that are difficult to tolerate represent the essential catalysts for change. Several treatment studies have examined or even verified this hypothesis[8-10]. Affective instability and impulsivity due to impaired affect perception and regulation leading to intra- and interpersonal dysfunction are key features in patients with borderline personality disorder (BPD). Clinical researchers have suggested that attention be paid to affective experience, for it determines positive outcomes[11] (see also[12-14]). In this matter, one should attempt to specify which affective state in connection with a particular personality pathology (e.g., quality of object relation[5]) should be dealt with, in order to achieve satisfying treatment outcomes. The next logical step would then be to identify to what extent therapeutic action during the analytic process is responsible for the observed therapeutic results[15].
Psychoanalytic treatment studies investigating therapeutic interventions, which are mainly based on psychoanalytic models of mental functioning[16], are quite rare. However, Jones and Ablon[17] and Jones[18] conceptualized the mode of therapeutic action, describing it as a "repetitive interaction structure"[17,18]. This empirically derived conceptualization, of the therapist-patient interaction, covers both therapeutic actions [e.g., clarification, confrontation, (transference) interpretation] and the patient's (re)actions. Depending on the perspective, a patient's (re)action may be seen as a reflection of his/her own psychic structure, object representation, compromise formation or impulse-defence configuration. A similar concept is known as the "transference-countertransference-process"[4]. Kantrowitz[4] and Jones[18] were one of the first to claim that dynamic aspects in patient-therapist interactions, being resonant or dissonant, are essential to therapy results[4,18]. The "two-person-process" should therefore be explored, to widen our knowledge of patient characteristics, particularly of influencing factors (such as affect parameters, transference patterns, or object relations patterns), and most notably regarding the agents of therapeutic action. The role these influencing factors play in therapy outcomes is currently quite well researched (see the quality of object relations[5]). The mediating function of the quality of the therapeutic relationship between patient and therapist, which is configured early on in therapy (in general as early as in the 2nd session), has already been described by Blatt and Zuroff[19] (2005) as being extremely important for the therapeutic process[19].
Hence, questions arise of how therapeutic interaction styles during psychoanalytic treatments come about, how they are displayed and explored and how these modes of interaction can create a foundation for treatment progress and the change process in general. In the current study, affect parameters and character traits (item constellations), which have already shown predictive power for therapy outcomes in other samples[20], were compared to differentiate types of interaction styles. Our investigation was applied to PSA and PDT of BPD patients in a retrospective study: By analyzing recordings of sets of consecutive sessions of two matched groups of BPD patients. The hypothesis was that changes during the treatment process would only occur if specific therapist-patient interactions emerge. The therapist-patient interaction was hypothetically defined as being effective when therapeutic action was met, after a particular time interval, with an affective (re)action (meaning an increase in positive affects) in the patient.
Based on the hypothesis, that significant therapeutic interactions occur in both treatment forms, the objective of the study was to explore the differences between "classical psychoanalysis–PSA" and "psychodynamic psychotherapy–PDT". By employing therapy concomitant evaluations, first treatment outcomes and second interaction styles of the repetitive interaction structure were examined for differences.
Our study group took audio/videotapes of PSA sessions and PDT sessions semiannually. All participants and the therapists involved gave their informed consent.
PSA: Ten patients were treated at four sessions a week with PSA. Each patient was treated by a different therapist. The analysts had a minimum of five years of clinical experience in conducting psychoanalytic treatment and had completed their training at the Vienna Psychoanalytic Society [German: Wiener Psychoanalytische Vereinigung (WPV)/IPA]. Weekly supervisions, based on a modern, object-relational Kleinian model[21,22] and additionally two external supervisions, each performed every three months by two training analysts from the British Psychoanalytic Society (Segal H and Daniel P), verify the analytic quality of and therapy adherence to the therapeutic model.
PDT: Ten further patients were treated at two sessions a week with PDT. In this group also, each patient was treated by a different therapist. The therapists had completed their psychotherapeutic training according to the manual for PDT[14]. Supervisions, ensuring the quality of therapy and therapy adherence, were performed weekly by an experienced training analyst and PDT supervisor.
Psychoanalysis: In psychoanalytic treatment, non-directive listening is carried out with a neutral attitude, aiming to overcome sources of resistance, with the method of free association at the heart of the technique. Thus, although the analyst must get involved with the patient, he remains "equidistant" from the id, ego, and superego, as well as with respect to conflicts in the relationship and within the therapist himself[23]. Key psychoanalytic concepts (the unconscious, drives, defenses, object relations, Oedipus complex, transference) have a direct impact upon concepts for treatment technique (countertransference, interpretation, resistance)[24]. The analyst's focus is on the patient's mind during the therapy session rather than on the patient's existence in "external reality". The treatment goal is the development of ability for self-reflection and analysis, symbolizing and engaging in object relations.
Unlike in psychoanalytic oriented therapy, the higher frequency of the sessions provides a suitable framework for the analysis of hitherto abstract fears, wishes, and unconscious conflicts. However, as distinguished from PDT, the indication for PSA is sometimes limited due to lacking reflective functioning skills, ego-integration, and externalizing defense processes.
Therapists' adherence to the method taught by the Vienna Psychoanalytic Society (WPV/IPA) was ensured by supervision carried out on a regular basis, as described above.
PDT in patients with a borderline personality: For a more thorough description of the applied method, see the textbook of Burian and Grossmann-Garger[25]. Psychodynamic or "psychoanalytic-oriented" psychotherapy is derived from psychoanalysis, but it differs from it not only by the frequency of sessions, but also by the lack of the use of a couch[26]. The therapeutic activity is defined, rather, by a clear problem statement and by work on the alleviation of symptoms or on identity integration. This method emphasizes the importance of the patient's actual external reality, and emphasis is brought to the here and now[25]. Transference interpretation and analysis of the transference relationship aims for modification of internalized patterns regarding object relations, behavior, and affect perception and regulation. Treatment goals often imply work on a sense of consistency about who oneself and others are across time and different contexts[26].
In contrast with psychoanalysis, neutrality frequently has to be sacrificed because of danger arising from possibly destructive enactment, when patients seem unable to contain their inner psychic conflicts. Supportive interventions are sometimes necessary.
Adherence of the therapists to the manual[14] was ensured by the supervision carried out at a regular basis mentioned above.
We applied a hot spot recruiting strategy that allowed for a matched pair design. The patient recruitment timeframe was four years. All patients willing to participate in the study, and fulfilling the inclusion criteria were included in the study. Participants treated with PSA and PDT were matched according to age, gender, DSM-IV-TR diagnosis[27] (Diagnostic and Statistical Manual of Mental Disorders, DSM, American Psychiatric Association 2000), pathological personality traits, assessed using Shedler-Westen Assessment Procedure-200 (SWAP-200)[28], and Kernberg[29]'s structural diagnosis. The audio/videotape analysis of recorded sessions and comparing the two therapeutic methods applied was carried out only after the completion of three years of psychotherapy. Thus the analysis's findings did not influence the therapeutic interventions. All patients showed the structural diagnosis of a BPD[29]. All participants underwent Structured Clinical Interview for the DSM-IV-TR Disorders and an examination by a psychiatrist (i.e., care and quality control as usual). Only participants fulfilling the DSM-IV diagnosis of BPD were included in the study. The participants had the following DSM-IV diagnosis of axis 1 comorbidities: Major depression, dysthymia, depression, anxiety disorder, eating disorder (22%: 296.00, 17%: 300.4, 10%: 311, 39%: 300.0, 12%: 307.0). The study included 20 patients, with an average age of 31 years (± 9). Patients were randomly assigned to therapists, often depending on the availability of a therapist.
The sample consisted of four (20%) male and 16 (80%) female patients with a relatively high level of education: While three patients (15%) only finished compulsory school, 14 patients (70%) were high school graduates and three (15%) had a university degree. Most of the patients (17) were single (85%); however, two (10%) were married, and one (5%) was divorced. One patient from the PDT group was excluded from the analysis since only baseline data were collected for the patient, and no further data on therapy development during the follow-ups were available. In Table 1, further descriptive analysis of the patient population, including mean SWAP profile scores, for both therapy groups (PSA vs PDT) is presented.
| PSA (n = 10) | PDT (n = 9) | P value1 | |
| Mean age (yr) | 30.4 ± 7.5 | 31.9 ± 10.2 | 0.719 |
| Sex | 8 f, 2 m | 7 f, 2 m | 0.912 |
| Therapeutic dose (mean) | 390 sessions | 124 sessions | 0.001 |
| DSM IV axis II diagnosis | Borderline personality disorder | ||
| Structural diagnosis | Borderline personality organization | ||
| SWAP diagnosis | |||
| Paranoid | 49.37 | 48.85 | 0.871 |
| Schizoid | 49.65 | 54.79 | 0.201 |
| Schizotypal | 51.27 | 53.72 | 0.475 |
| Antisocial | 49.22 | 45.62 | 0.132 |
| Borderline | 52.97 | 48.62 | 0.289 |
| Histrionic | 53.92 | 46.37 | 0.127 |
| Narcissistic | 50.86 | 46.56 | 0.249 |
| Avoidant | 47.78 | 54.18 | 0.037 |
| Dependent | 49.29 | 52.01 | 0.233 |
| Obsessive-compulsive | 47.65 | 52.51 | 0.245 |
Ethic: Approval from the ethics committee of the City of Vienna and the Medical University of Vienna was given; EK Nr.: 2169/2013. This study was done in accordance with the terms set forth in the Declaration of Helsinki. Written informed consent was given.
After obtaining informed consent for this observational study, treatment sessions of twenty patients were recorded semiannually over a period of three years. In the case of PSA, treatment sessions were assessed using verbatim transcripts and audio recordings of the peer-supervisions as well as external supervisions, while in the case of PDT, sessions were assessed using video recordings.
From the beginning of therapy, in an interval of six months, recordings (audio or video) of five consecutive therapy sessions were analyzed for patient characteristics and interactions, using the following instruments.
SWAP-200: Character traits were determined using the SWAP-200[24,26], assessed by two independent external raters, both of whom were medical students, each having at least six years of experience with the instrument; with adequate training, they regularly underwent assessments of inter-rater reliability. Their inter-rater reliability showed a constant κmean= 0.69. The SWAP-200 is a personality assessment instrument for use by clinically experienced mental health professionals requiring a professional assessment (e.g., during an ongoing therapeutic engagement) or a systematic clinical research interview. Test-retest reliability for the instrument is r = 0.85 for the SWAP's trait and personality disorder dimensions. The mean reliability when comparing to DSM-IV personality disorders was 0.90 for SWAP scales. Multiple research groups in multiple samples have provided strong evidence, qualifying SWAP-200 as a reliable and valid measure independent from applied methods[30]. The SWAP is based on the Q-sort method, and thus it uses a fixed score distribution, with items being rated as more or less descriptive of a person, with the possibility of detecting even fine nuances.
Based on the SWAP-200 scoring systems, personality score profiles are generated. The scores are standardized scores (T-scores) based on norms established in a clinical sample[28]. Scores indicate the match between a patient and a diagnostic prototype derived either from DSM-IV diagnostic categories (which include the personality disorders in DSM-IV as well as depressive personality disorder) and/or an alternative set of personality syndromes derived empirically (via Q-factor analysis, see SWAP manual). Thus, a high degree of overlap with the SWAP-profile "dysregulated/ borderline" (i.e., variable SWAP-borderline") indicates that the degree of resemblance between the actual patients with the diagnostic prototype representing the personality disorder is also very high. The "Borderline/Emotionally Dysregulated" personality is described as overlapping with the DSM-IV construct. Patients with this profile lack affect-regulation (intense and volatile affect) and show states of desperation and despair with a tendency to self-harm[31].
Affect experience and affect regulation Q-sort (AREQ): Affective experience and affect regulation were assessed using the affect regulation and experience Q-sort AREQ[32,33]. The AREQ is an expert-rating, 98-item Q-sort test, exploring affective functioning using an interview. Sufficient convergent and discriminant validity have been shown. Affect experience includes the following three factors: Socialized negative affect, positive and intense negative affect, and affect experience, the latter of which itself includes reality focused response, externalizing defense, and avoidant defense[32]. The inter-rater reliability of two independent raters, both having an average of six years of experience with the instrument, showed an average κ = 0.70. They were both medical students, undergoing regular training and quality assessment.
Quality of object relations scale (QORS): The quality of object relations was evaluated by two independent external raters, using the QORS[33,34], and showed an inter-rater reliability of κmean = 0.69. The raters were both medical students, undergoing regular training and quality assessment. The QORS is an interview-based expert-measure with adequate criterion-related, construct validity[35]. The QORS assesses personality pathology with respect to object-relational maturity. Object relations are intrapsychic representations of self- and objects which arise out of emotionally important early relationships. The level of object relations is a known factor related to the outcome of psychotherapy. The interview scale consists of five levels of object-relational patterns with the manual giving explicit criteria for each of them and a description of prototypical cases. The rater distributes a total of 100 points, allocating them to five object-relational levels: Primitive, searching, triangular, controlling, and mature (for a thorough description of the method see[35]). According to Lindfors and colleagues, low quality of object relations is characterized by discontinuity and devaluation in relationships, with poor self-confidence and major separations in childhood identified as predictors of low-QOR[35].
Psychotherapy relationship questionnaire (PRQ): The quality of the psychotherapeutic relationship was assessed using the German version[36] of the PRQ[37]. With the help of 90 items, five dimensions of transference relationship patterns (hostile, narcissistic, anxious/preoccupied, avoidant/counter dependent, and sexualized) as well as a positive working alliance (secure/engaged) can be differentiated. The dimension "positive working alliance" is of particular interest to the current study, and as Bradley et al[37] and Tanzilli et al[38] have already shown, it acts as an indicator for the quality of the working relationship between patient and therapist, which in turn, strongly predicts treatment outcome in psychotherapy[39].
Psychotherapy process Q-sort (PQS): Patient-therapist interrelation variables were assessed using the PQS[40,41]. For this study, in order to analyze the process occurring during therapy, only items related to therapeutic action were utilized[41] (Table 2). From a psychoanalytic perspective, these items specifically covered transference interpretations considering the "total situation" described by Joseph/Astor[42]. The goal was to evaluate dyad-specific interaction structures, which are recurrent, mutually influencing patterns of interrelation between therapist and patient, whose experience, recognition, and understanding are fundamental elements of therapeutic action[17,34]. Therapeutic action was evaluated by two independent raters (κmean = 0.84) using the items presented in Table 2.
| Item | Description |
| 2 | Therapist draws attention to patient’s non-verbal behavior, e.g., body posture, gestures |
| 22 | Therapist focuses on patient’s feelings of guilt |
| 28 | Therapist accurately perceives the therapeutic process |
| 36 | Therapist points out patient’s use of defensive maneuvers, e.g., undoing, denial |
| 40 | Therapist makes interpretations referring to actual people in the patient’s life |
| 50 | Therapist draws attention to feelings regarded by the patient as unacceptable (e.g., anger, envy, excitement) |
| 62 | Therapist identifies a recurrent theme in the patient’s experience or conduct |
| 65 | Therapist clarifies, restates, or rephrases patient’s communication |
| 67 | Therapist interprets warded-off or unconscious wishes, feelings, or ideas |
| 79 | Therapist comments on changes in patient’s mood or affect |
| 80 | Therapist presents an experience or event in a different perspective |
| 82 | The patient’s behavior during the hour is reformulated by the therapist in a way not explicitly recognized previously |
| 93 | Therapist is neutral |
| 98 | The therapy relationship is a focus of discussion |
| 100 | Therapist draws connections between the therapeutic relationship and other relationships |
The raters were medical students, undergoing regular training, interrater assessments, and quality control.
The statistical methods of this study were performed and reviewed by a biomedical statistician, Sophie Frantal, from the Medical University of Vienna before submission.
To begin with, a descriptive analysis (mean, standard deviation, minimum and maximum) of the variables of interest was created. However, due to the rather small sample-size, also ranges were used to characterize the sample. Next, the differences between the two groups (PSA and PDT), based on pre-post comparison of the main factor "SWAP Borderline"[28], were examined. For this purpose, the scores at the beginning of therapy (t1), after one year of therapy (t3) and after three years of therapy (t7), were evaluated. Also, additional factors possibly influencing outcome, such as age, gender, education, family status and gender of the therapist, were included in the analysis. Missing values, detected after data documentation, were excluded from the analysis. To answer the question dealing with the differences between the two therapeutic methods in concern to the changes observed in the variable "SWAP Borderline", all variables of interest were tested in univariate analysis (linear regression or variance analyses). Only variables that showed statistically significant p-values in the univariate analysis were subsequently tested in a multivariate linear model (ANOVA or ANCOVA). Furthermore, effect size was also calculated for groups PSA and PDT.
In the following step, differences between the two therapy groups concerning the factors "positive affect" (AREQ), "QORS-total score", "therapeutic action" (PQS), and "positive working alliance" (PRQ) were assessed. These factors were explored in the same manner as the factor "SWAP Borderline". Similarly, in the cases, where the variable of interest "therapeutic method" did not show any statistically significant effects, no further risk factors were analyzed. The number of therapy sessions ("therapeutic dose"), defined as the mean number of sessions in which each therapeutic method (PSA vs PDT) was applied, was also tested as a factor possibly having influence on the variable "Borderline".
Analyses were performed using the "freeware" program R.2.8.0[43] and SPSS Statistics version 17.0. P < 0.05 were considered to be statistically significant.
The differences between the two therapeutic methods, PSA and PDT, with regards to the main variable "SWAP Borderline", are presented in Table 3. Even though the differences are not significant, a simple comparison between the mean values shows that borderline pathology, in the case of PSA, continuously decreases. However, in the PDT group, it primarily increases, particularly in the first year. This observation is also reflected in the effect size: d = 0.79 after one year of PSA, d = 0.88 after three years of PSA, d = 0.04 between first and third year of PSA; d = |0.40| after one year of PDT, d = 0.04 after three years of PDT, d = 0.33 between first and third year of PDT. After three years of PDT, the main variable "Borderline" improves considerably compared to the values measured after the first year of PDT, whereupon the therapeutic method PSA shows less change in the same time span. This, however, must be interpreted with caution, due to the fewer number of patients after three years of therapy (three dropouts in PSA, four dropouts in PDT after three years). Even tough, the dropout rate is not surprising, as it might be related to the frequent alliance ruptures typical for borderline pathology, and the naturalistic design must be considered before generalizing this finding. However, looking beyond the main variable and more at individual items in detail, in both groups, patients who dropped out were characterized by an increase of projective mechanisms (projection, projective identification) as displayed in SWAP-Item 076 and Item 116. This was observed mainly during the first year (Figure 1), but generally persisted until the moment a patient dropped out of therapy. Additionally, it was observed that these patients and their therapists showed low scores in the PQS-Item 36, 50 (displaying therapists' work on defensive mechanisms) and PQS-Item 28 (therapists' accurate perception of the therapy process) (Table 2). These ratings might display a lack of ability to perceive, contain and work through the projective mechanisms in the therapeutic relationship (Figure 1), which was also observed and discussed in the supervision group. Interestingly, drop-out patients' pressure and usage of projective mechanisms were low at the beginning of both forms of therapy compared to continuing and finishing patients, who presented higher amounts of projective identification at the beginning of therapy. Also, PQS Items 36, 50, and 28 (Table 2) were higher in cases where therapy reached completion. As far as the drop-out patients could be reached, they reported no increase in self-harming behavior; one was referred to supportive therapy by the therapist due to the development of psychotic transference.
| n (%) | Min | Max | P value1 | dt32 | dt72 | ||||
| Baseline (t1) | PSA | 10 | 52.97 | 8.73 | 42.69 | 71.88 | 0.79 | 0.88 | |
| PDT | 9 | 48.62 | 8.56 | 40.23 | 67.63 | |0.40| | 0.04 | ||
| Total | 19 | 50.90 | 8.70 | 40.23 | 71.88 | 0.289 | 0.24 | 0.45 | |
| After 1 yr of therapy (t3) | PSA | 10 | 46.26 | 8.21 | 29.99 | 60.21 | 0.04 | ||
| PDT | 9 | 51.80 | 7.49 | 40.26 | 65.30 | 0.33 | |||
| Total | 19 | 48.88 | 8.17 | 29.99 | 65.30 | 0.145 | 0.20 | ||
| After 3 yr of therapy (t7) | PSA | 7 | 45.96 | 6.75 | 37.63 | 56.78 | |||
| PDT | 5 | 49.01 | 10.20 | 38.90 | 61.33 | ||||
| Total | 12 | 47.23 | 8.07 | 37.63 | 61.33 | 0.545 |
Considering the patients' characteristics, changes in borderline pathology and, simultaneously, improvements in the quality of object relations were observed, when both forms of therapy were taken into account. With regard to the patient, an increase in the ability to recognize positive affects was observed during PSA, while a decrease in the same category was seen during PDT. However, an increase in therapeutic action was observed during PDT, while therapeutic action during PSA treatment stayed constant. Concerning the working alliance, a reduction in the positive working relationship between therapist and patient was noted during PSA treatment, whereas an increase in the same category was observed during PDT. The descriptive analysis of the pre-post variables (SWAP-Borderline, AREQ-positive affect, QORS-total score, PRQ-positive working alliance and PQS-therapeutic action), defined as the difference between the values of each variable at beginning of therapy (t1) and after one year of therapy (t3,) is presented in Table 4 ("SWAP-borderline" = SWAP personality syndrome "dysregulated/borderline"). All means were close to zero (with the exception of "SWAP-Borderline"), showing little to no difference between baseline and follow up (after one year) measurements (Table 4: "mean"). Only the variable "SWAP-Borderline" showed a negative response during the first year of PDT treatment (i.e., less BPD symptoms), and a positive value in the PSA treatment (i.e., more BPD symptoms) however, the standard deviation was in this case somewhat higher than in the other variables (mean SWAP Borderline PSA = 6.71; SD ± 9.29; mean SWAP Borderline PDT = -3.18; SD ± 7.94).
| Min | Max | P value | ||||
| SWAP Borderline | PSA | 6.71 | 9.29 | -1.58 | 29.58 | 0.024a |
| PDT | -3.18 | 7.94 | -10.61 | 15.22 | ||
| Total | 2.02 | 9.85 | -10.61 | 29.58 | ||
| AREQ positive affect | PSA | -0.11 | 0.98 | -1.57 | 1.86 | 0.513 |
| PDT | 0.19 | 0.86 | -0.94 | 1.43 | ||
| Total | 0.03 | 0.91 | -1.57 | 1.86 | ||
| QORS total score | PSA | -0.20 | 0.73 | -1.60 | 0.90 | 0.726 |
| PDT | -0.34 | 0.75 | -1.70 | 0.50 | ||
| Total | -0.26 | 0.72 | -1.70 | 0.90 | ||
| PRQ positive working alliance | PSA | 0.15 | 0.35 | -0.33 | 0.50 | 0.339 |
| PDT | -0.27 | 0.73 | -1.08 | 0.50 | ||
| Total | -0.08 | 0.60 | -1.08 | 0.50 | ||
| PQS therapeutic action | PSA | -0.00 | 0.60 | -0.73 | 1.00 | 0.318 |
| PDT | -0.28 | 0.45 | -1.07 | 0.47 | ||
| Total | -0.14 | 0.53 | -1.07 | 1.00 |
In univariate analysis, the difference between the two therapeutic methods in concern to changes in the variable "SWAP Borderline" was examined and was shown to be significantly different (PDT: Estimate 4.07; T = 2.19; SD ± 1.73; P = 0.402; Table 5). The age of the patients was found to not be significantly different, with a P = 0.087, however it still displayed a strong trend, with younger patients showing better results (Table 5). Thus, it is evident that during the first year of therapy, the therapeutic method PSA led to a higher decrease regarding the symptom profiles reproduced in the variable "SWAP Borderline" than the therapeutic approach PDT (Table 3). Nevertheless, a higher variance of individual therapy results after the first year occurred in PSA (Table 3). Thus, when looking at the mean change in the variable "SWAP Borderline" after one year, PDT showed a significantly more pronounced improvement (Table 4). Sex, education, and family status of the patient as well as the sex of the therapist were not found to be significant. A multivariate analysis, regarding the risk factors therapeutic method and patient age, was also performed and the following results were found: In both cases, the levels of significance did not change and the therapeutic method remained significant (PDT: Estimate 4.01; T = 2.33 ± 1.73; P = 0.033), while patient age continued to not reach the fixed significance level (Age: Estimate 0.40; T = 1.98 ± 0.20; P = 0.064).
| Patient characteristics | Estimate | T value | P value | |
| PDT group | 4.07 | 1.86 | 2.19 | 0.042a |
| Sex of patient | 2.89 | 5.18 | 0.56 | 0.584 |
| Sex of therapist | 7.15 | 4.24 | 1.68 | 0.109 |
| Education: Apprenticeship | 12.21 | 10.49 | 1.16 | 0.261 |
| Education: Vocational school | 3.15 | 8.29 | 0.38 | 0.709 |
| Education: High school | -2.80 | 5.78 | -0.48 | 0.635 |
| Married | -1.03 | 7.19 | -0.14 | 0.888 |
| Divorced | -0.39 | 9.90 | -0.04 | 0.969 |
| Age | 0.41 | 0.22 | 1.81 | 0.087 |
Examining the four secondary variables during the first year of therapy, no statistically significant differences could be found between the two types of therapeutic methods (PSA vs PDT): AREQ-positive affect (estimate -0.31; T = -1.70 ± 0.18; P = 0.117), QORS-total score (estimate 0.08; T = 0.38 ± 0.20; P = 0.714), PRQ-positive working alliance (estimate 0.00; T = 0.01 ± 0.26; P= 0.993) and PQS-therapeutic action (estimate 0.14; T = 1.01 ± 0.14; P = 0.333). Consequently, no further calculations and analyses were performed, regarding the secondary variables. Similarly, no significant changes were found in the variable "therapeutic dosage" (P = 0.298). However, the changes observed after time-point t5, i.e., after 2.5 years of PDT, resulting in a constant decrease in borderline pathology, is quite interesting (difference in "SWAP Borderline", in the 175th session mean was -9.08; in the 245th session mean was 15.22). In the therapeutic method PSA, a constant decrease in borderline pathology is seen from the start.
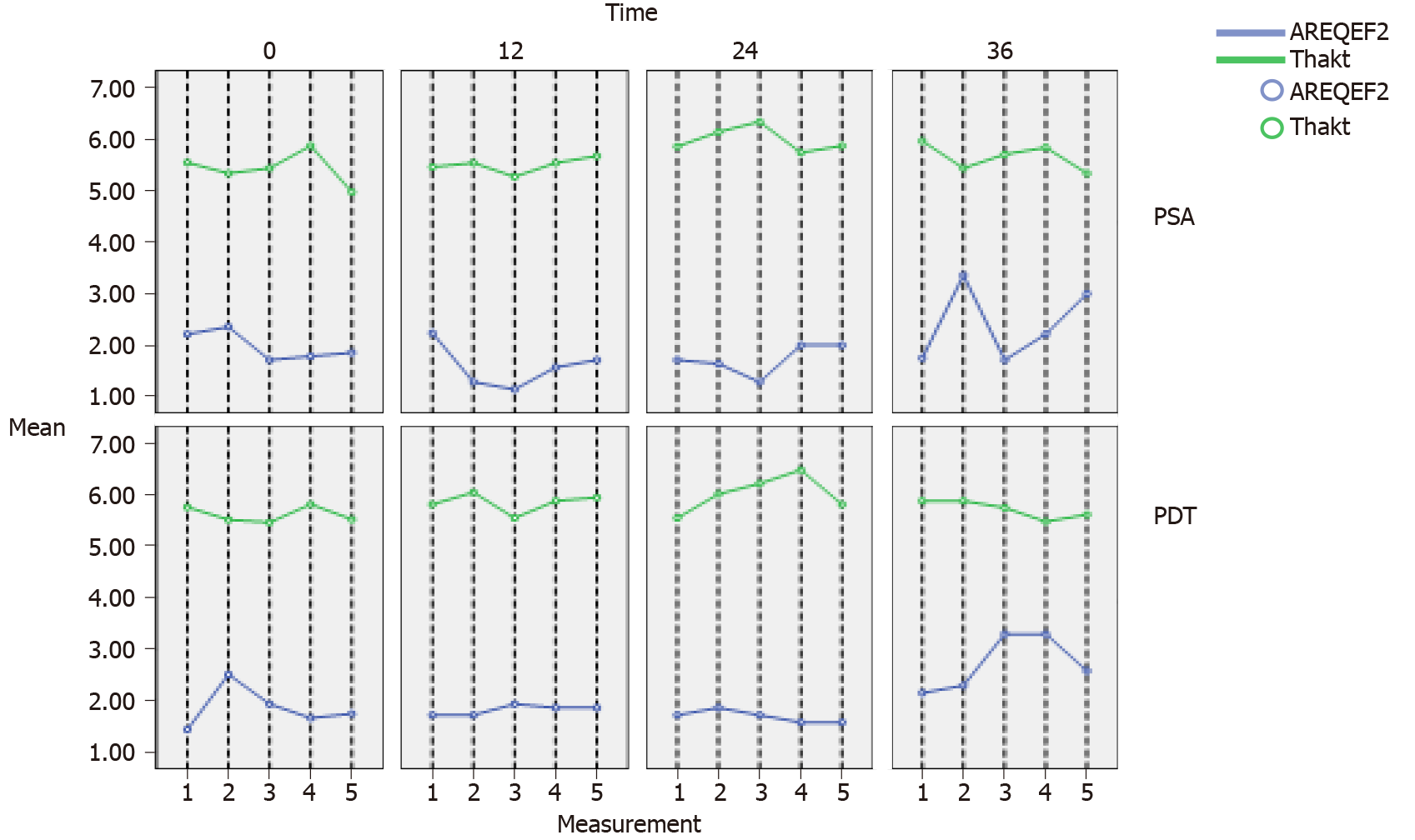
"Repetitive interaction structures," which are defined as responses of the patient towards therapeutic action with an increase in positive effects, are depicted in Figure 2. The graph illustrates a sequence of five consecutive sessions measured on a semi-annual basis. However, it is essential to mention that Figure 2 is merely a graphic presentation of the data since therapeutic action had no significant influence on the variable "SWAP Borderline". The main finding is depicted in Figure 2: The time-lag of the repetitive "interaction structures" in PSA is shorter (approximately two/three sessions) than the time-lag observed during PDT (about five sessions). Thus, the descriptive analysis showed patterns quite distinct for each method.
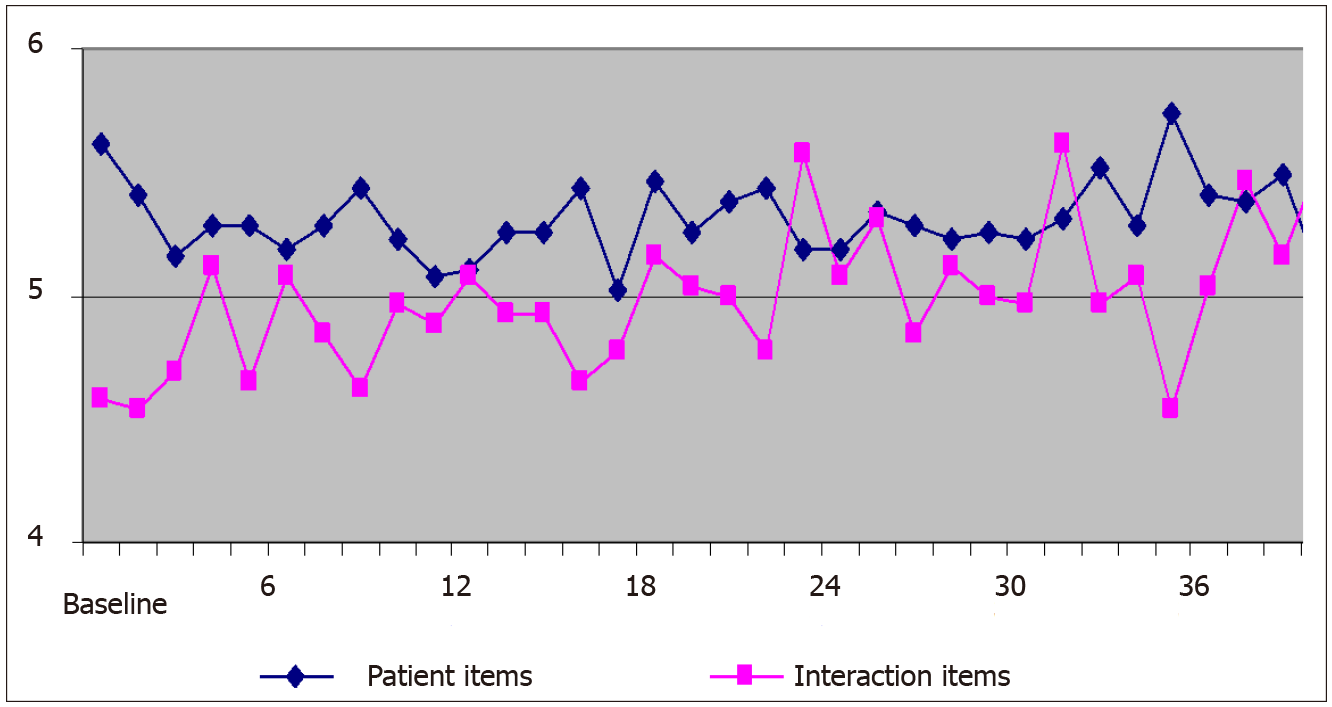
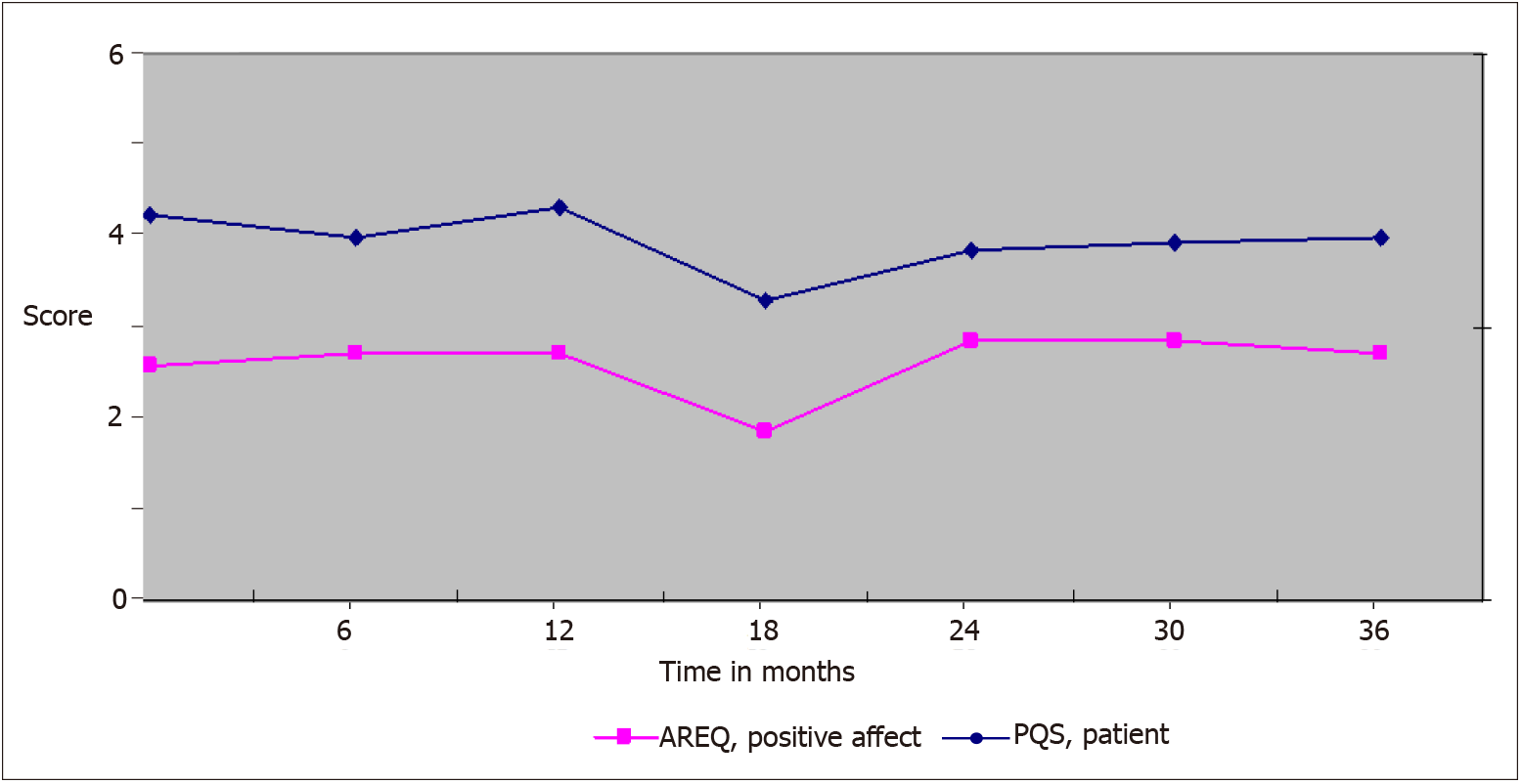
With respect to PSA, a qualitative analysis of character traits with the SWAP showed repetitive patterns of trait fluctuations over the course of three years. The interpretation of the object-relationship dyad in transference with patient-, therapist-, and interaction-variables carried out with the PQS showed repetitive patterns of interaction when treatment was successful. PQS patient items and interaction items showed a rise in patient items when "interaction structure" items were rated as low and vice versa (Figure 3). In unsuccessful therapy attempts, in neither the SWAP nor in the PQS/AREQ ratings did similar patterns manifest, with a relatively constant course over time (not shown). When looking at a set of five consecutive sessions, positive affective response (measured with the AREQ) increased following therapeutic interventions, with a time-lag phenomenon manifestly present (Figure 4). Qualitative analysis revealed shorter time-lag for the positive affective response of the patient towards the therapists' interaction in PSA in contrast to PDT (Figure 2; PSA two/three sessions, PDT five sessions).
The combined analyses of repetitive patient-therapist interaction structures (AREQ, PQS) and patient characteristics (SWAP-200, AREQ, QORS) performed in this study have met the demands for therapy concomitant evaluations, which were briefly mentioned in the introduction and have also been described in the literature[10]. By means of such therapy concomitant evaluations, where the assessment of therapeutic techniques and changes in patient characteristics are combined, the possibility of specifying specific therapeutic methods is opened up.
Our results have shown that patients, who were treated with PDT in the same time frame as patients treated with psychoanalysis proper, showed similar changes in the quality of object relations and affect parameters, albeit, however, with considerably distinct changes in personality pathology.
The increase in borderline pathology at the beginning of the PSA treatment is quite noticeable (mean change in SWAP borderline: PSA +6.71, PDT -3.18) with a higher variance of observed changes in the PSA group especially in the first year of therapy (Table 4). However, after one and after three years of therapy, mean “SWAP borderline” score was lower in the PSA group, while in the PDT group this score was even slightly increased.
These results indicate that indications for the two different methods must be assigned wisely, as they are not interchangeable.
Although all patients were diagnosed with BPD at the beginning of treatment, the two groups differed in the first six months of therapy. Considerably more patients in the PDT group were affected by social inhibitions (avoidant/self-conscious traits) and discomfort in social (schizoid traits) and close relationships (schizotypal traits). Borderline patients with schizoid personality pathology, treated with PDT, showed improvements, especially after the first year of therapy, while corresponding patients in the parallel group, treated with PSA, showed positive changes right from the start. Similar results have been reported in the Anna Freud Center study[44], where the psychoanalytic treatment of young patients with borderline and narcissistic personality disorders was performed at different frequencies (five times vs once per week) and then ultimately compared. The problems encountered with narcissistic personalities of not being able to accept interpretations[45] or creating transference configurations, where the analyst becomes a shut-out observer[46], are more likely to be solved during PSA.
In the descriptive analysis of the secondary moderating and mediating variables, it appeared that in higher-frequency therapeutic methods, such as PDT, therapeutic action increased during the first year of therapy. This observation could possibly be related to the therapists' more vigorous focus on the working alliance (see an increase in a positive working relationship). But, one can only speculate here, since the secondary variables did not show any statistically significant differences between the two therapeutic methods. The therapeutic dose, interestingly, also did not show any statistical significance, by which closer observation of the interaction process becomes more relevant.
Psychoanalyses, with quick interactions (meaning that a therapeutic action is followed by an increase in positive affects in the patient within the next two to three sessions,
Clarification and confrontation, as well as the interpretation and working through of the external reality of the patient, play a large role in higher-frequency therapeutic methods such as PDT[50]. Patterns in social interaction and ways of problem-solving are enacted in the patient-therapist setting, a thorough observation of such enactments (manifesting in language, gesture, facial expression, and micro-expression) is crucial for the detection of unconscious and preconscious material. This interactivity in the learning environment provided by the therapeutic setting leads to improved problem-solving and achievement of new perspectives.
The interaction styles in the PDT group of our study were slower; therapeutic actions and respective positive affective reactions of the patients were often observed to extend over three or four sessions (i.e., two weeks). This difference, observed in the descriptive analysis, could possibly be due to different session frequencies, setting, or therapeutic techniques. Meltzer[12] and Etechegoyen[51] have pointed out, that at the beginning of treatment mostly externalizing, projective mechanisms can be observed[12,51]. If these projective mechanisms are not understood and treated promptly and sufficiently, unsatisfactory therapy outcomes will be then more likely. The worsening of the borderline pathology could hypothetically be associated with the therapists' focus mainly on external reality and working alliance, without employing transference (optionally analyst-centered) interpretations.
While assigning patients to the two therapy groups, PSA and PDT, despite the known heterogeneity of BPD patients[52], we attempted to match patients who were comparable to one another, as far as their personality structure was concerned; however, differences in the patients' personality traits were found in both therapy groups. The fact that the assigning of patients to therapy groups depended on the availability of a therapist may be seen as a legitimate point of criticism. These differences, however, were only found to be significant in patients with avoidant traits and may therefore be seen as having an only minor influence on the total outcome. As for the "therapeutic dosage", it would be of further scientific interest, to systematically research the relationship between the number of treatment sessions and therapy outcome. This study showed no significant differences in this matter.
Treatment of patients with the borderline disorder has traditionally been limited due to high drop- out rates already within the first months of treatment in outpatient settings (by the six-month point only 34% to 57% of BPD outpatients remain in treatment[53,54]). Although BPD has a known positive trajectory over time, comorbidities[55] are frequent and long-term functional recovery is difficult, with short-term therapies often not addressing the underlying problematic personality traits[56]. Thus, in our clinical understanding, the analysis of the characteristics of early patient-therapist interactions is essential due to known difficulties in collaboration with BPD[53,54]. One strength of this study is that complete long-term follow-up data (three years) were available for a majority of the participants (i.e., PSA: 70%, PDT: 50%). Future research should investigate the specific drop-out process in BPD and further investigate factors that may improve long-term outcome, like repairing alliance ruptures.
Our research was carried out in a naturalistic manner, conducting on-site assessments. Thus, the observed phenomena resemble the 'real world'. Hypothesis-generating clinical research does not replace hypothesis-testing, but it can facilitate the development of a specific hypothesis that can be tested by the application of an experiment. The retrospective design limits the level of evidence. Our findings have descriptive value and contributed to the foundation of clinical-relevant hypotheses that might be further investigated in an experimental study design. Emotional reactivity in patients with borderline personality disorder (BPD) due to dysfunctional processes is still a concept being developed[52,57]. We agree that a larger sample size would have been favorable. With a small sample we are limited to detecting big differences or big "effects" and our data need replication[58]. Further research should choose a larger sample size, to ensure sufficient power for extrapolating the results of any statistical analysis to the overall patient population. Of course, the design of an observational study with hot-spot recruitment should be replicated, which is currently under progress in our department. Replication seems not only necessary, but interesting, as other centers had found similar findings[59] especially concerning the dose-efficacy question and differences in high- and low-frequent settings: The more sessions took place with psychoanalytic technique, the better psycho-structural change could be achieved[59].
Very restricted resources often limit availability of psychotherapy in outpatient settings, despite the relevance of mental health problems. However, psychotherapy should be available for everyone with psychological strains and in need of treatment. In the outpatient clinic where this study took place, therapy places for borderline patients also with limited resources were available. Unfortunately, this might not be the usual terms.
Exploring the changes in patient characteristics and linking these changes to specific treatment strategies is of clinical importance not only when starting treatment but also for its long-term progress. The quality and accurate timing of patient-therapist interactions seem to be essential to change processes than the number of such interactions. During psychoanalytic treatments, therapy concomitant evaluations should be used to identify aspects of the therapy, that can either be promising for or preventive to a positive outcome and so that the therapist can accordingly adjust his/her intervention techniques. In therapy concomitant evaluations, the observation of repetitive interaction structures in connection to changes in patient characteristics should be a focus. By assessing the capability of therapists to interpret transferences appropriately, this instrument of a treatment concomitant evaluation could be used to assure the quality of psychoanalytic treatments. However, high-level evidence from meta-analysis regarding effects of psychological therapies for people with borderline personalities is still scant but benefits over TAU have been shown[60-63].
Emotional reactivity in patients with borderline personality disorder (BPD) due to dysfunctional processes is still a concept being developed. Specifically designed psychotherapies for BPD have significant, modest benefits over TAU. The effects of psychotherapy on BPD are still insufficiently understood. Substantial heterogeneity of processes and populations studied contributes to varying research results when investigating the effects of different treatment methods, and whether they differ from each other.
The question was whether similarities and differences between psychoanalysis (PSA) and psychodynamic psychotherapy (PDT) in BPD would be detectable, especially in terms of emotional reactivity in the patient-therapist interaction.
We aimed to study repetitive interaction patterns in patients with BPD undergoing either psychoanalysis or psychodynamic therapy.
Within a retrospective study framework, we compared matched PSA (n = 10) and PDT (n = 10) BPD patients’ treatment sessions. Five consecutive sessions were recorded and analyzed, with evaluation of effects compared to baseline over three years. Patient characteristics (including affect regulation and personality traits), quality of object relations, as well as related therapeutic actions, were analyzed (micro-process analysis).
Differences between PSA and PDT were significant when analyzing the “mean change” in the Shedler-Westen Assessment Procedure Borderline variable after one year of therapy (P = 0.024). Variance of observed change was higher in PSA than in PDT (SDPSA ± 9.29 vs SDPDT ± 7.94). Transference interpretations are followed closely by affective changes in the patient, and were useful modes of interaction.
PSA and PDT were both effective in BPD. Interactional aspects differed between the two treatments.
As BPD patients are a very heterogeneous population, further research should focus on investigating optimal matching of BPD patients to specific modes of affect regulation, as well as which specific level of personality functioning would benefit from a given therapy modality.
The authors wish to express particular thanks to John Clarkin and Peter Fonagy for their help in initiating the study, Drew Westen and Enrico Jones for providing the rating instruments. We thank the external raters Katharina Hämmerle, Nora Frossard, Marion Swaton, Armina Hrusto-Lemes, Golda Schlaff and Simon Madanoglu. We also thank Hemma Rössler-Schülein for her help in gathering the data. The authors want to appreciate the contribution of Medical University of Vienna/General Hospital of Vienna and NÖ Landesgesundheitsagentur, legal entity of University Hospitals in Lower Austria, for providing the organizational framework to conduct this research.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Psychiatry
Country/Territory of origin: Austria
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Koo BH S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Sandell R, Blomberg J, Lazar A, Carlsson J, Broberg J, Schubert J. Varieties of long-term outcome among patients in psychoanalysis and long-term psychotherapy. A review of findings in the Stockholm Outcome of Psychoanalysis and Psychotherapy Project (STOPP). Int J Psychoanal. 2000;81 (Pt 5):921-942. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 140] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 2. | Levy KN, Meehan KB, Kelly KM, Reynoso JS, Weber M, Clarkin JF, Kernberg OF. Change in attachment patterns and reflective function in a randomized control trial of transference-focused psychotherapy for borderline personality disorder. J Consult Clin Psychol. 2006;74:1027-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 483] [Cited by in RCA: 396] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 3. | Leuzinger-Bohleber M, Stuhr U, Rüger B, Beutel M. How to study the 'quality of psychoanalytic treatments' and their long-term effects on patients' well-being: a representative, multi-perspective follow-up study. Int J Psychoanal. 2003;84:263-290. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Kantrowitz JL. A different perspective on the therapeutic process: the impact of the patient on the analyst. J Am Psychoanal Assoc. 1997;45:127-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Høglend P, Bøgwald KP, Amlo S, Marble A, Ulberg R, Sjaastad MC, Sørbye O, Heyerdahl O, Johansson P. Transference interpretations in dynamic psychotherapy: do they really yield sustained effects? Am J Psychiatry. 2008;165:763-771. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 112] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 6. | Bucci W. The challenge of diversity in modern psychoanalysis. Psychoan Psychol. 2002;19:216-226. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Whelton WJ. Emotional processes in psychotherapy: evidence across therapeutic modalities. Clin Psychol Psychother. 2004;11:58-71. [RCA] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 86] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 8. | Hull JW, Clarkin JF, Kakuma T. Treatment response of borderline inpatients. A growth curve analysis. J Nerv Ment Dis. 1993;181:503-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 21] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Piper WE, Ogrodniczuk JS, McCallum M, Joyce AS, Rosie JS. Expression of affect as a mediator of the relationship between quality of object relations and group therapy outcome for patients with complicated grief. J Consult Clin Psychol. 2003;71:664-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Clarkin JF, Levy KN. Psychotherapy for patients with borderline personality disorder: focusing on the mechanisms of change. J Clin Psychol. 2006;62:405-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | Bion WR. Clinical seminars and other works (first published 1987). 1st ed. Bion F, editor. London: Routledge, 2018. |
| 12. | Meltzer D. The psychoanalytical process (The Harris Meltzer Trust Series). United Kingdom: Harris Meltzer Trust, 1967: 1-120. |
| 13. | Etchegoyen RH. The fundamentals of psychoanalytic technique, (trans. Pitchon, P); United Kingdom: Routledge, 1991: 1-912. |
| 14. | Clarkin JF, Yeomans FE, Kernberg O. Psychotherapy for Borderline personality: Focusing on object relations. Washington: American Psychiatric Publishing, 2007: 1-411. |
| 15. | Blass RB, Carmeli Z. The case against neuropsychoanalysis. On fallacies underlying psychoanalysis' latest scientific trend and its negative impact on psychoanalytic discourse. Int J Psychoanal. 2007;88:19-40. [RCA] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 67] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 16. | Fonagy P, Roth A, Higgitt A. The outcome of psychodynamic psychotherapy for psychological disorders. Clin Neurosci Res. 2005;4:367-377. [RCA] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Jones EE, Ablon JS. On Analytic Process. Int J Psychoanal. 1997;78:1135-1150. [RCA] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 38] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 18. | Jones EE. Modes of therapeutic action. Int J Psychoanal. 1997;78 (Pt 6):1135-1150. [PubMed] |
| 19. | Blatt SJ, Zuroff DC. Empirical evaluation of the assumptions in identifying evidence based treatments in mental health. Clin Psychol Rev. 2005;25:459-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 100] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 20. | Löffler-Stastka H, Rössler-Schülein H, Skale E. [Predictors of dropout during psychoanalytic treatments of patients with personality disorders]. Z Psychosom Med Psychother. 2008;54:63-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Bronstein C. Kleinian theory: a contemporary perspective. London: Whurr Publishers, 2001: 1-236. |
| 22. | Schafer RE. The contemporary Kleinians of London. Inc, Madison CT: International Universities Press, 1997: 1-441. |
| 23. | Hoffer A. Toward a definition of psychoanalytic neutrality. J Am Psychoanal Assoc. 1985;33:771-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 55] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Luborsky L, Barrett MS. The history and empirical status of key psychoanalytic concepts. Annu Rev Clin Psychol. 2006;2:1-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 25. | Burian W, Grossmann-Garger B. [Psychanalytically oriented psychotherapy]. Wien, Berlin: Mandelbaum Verlag, 2018: 1-1023. |
| 26. | Rössler-Schülein H, Löffler-Stastka H. [Psychoanalysis and psychoanalytic oriented psychotherapy: differences and similarities]. Neuropsychiatr. 2013;27:180-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV-TR. Washington DC: American Psychiatric Pub, 2000. |
| 28. | Westen D, Shedler J. Revising and assessing axis II, Part I: developing a clinically and empirically valid assessment method. Am J Psychiatry. 1999;156:258-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 82] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 29. | Kernberg O. Severe Personality Disorders (Psychotherapeutic strategies). New Haven: Yale University Press, 1984: 1-396. |
| 30. | Blagov PS, Bi W, Shedler J, Westen D. The Shedler-Westen assessment procedure (SWAP): evaluating psychometric questions about its reliability, validity, and impact of its fixed score distribution. Assessment. 2012;19:370-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 31. | Höflich A, Rasting M, Mach J, Pless S, Danckworth S, Reimer C, Beutel ME. A German version of the Shedler-Westen Assessment Procedure (SWAP-200) for the dimensional assessment of personality disorders. Psychosoc Med. 2007;4:Doc02. [PubMed] |
| 32. | Westen D, Muderrisoglu S, Fowler C, Shedler J, Koren D. Affect regulation and affective experience: individual differences, group differences, and measurement using a Q-sort procedure. J Consult Clin Psychol. 1997;65:429-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 26] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 33. | ZPID. Zentrum für Psychologische Information und Dokumentation. Elektronisches Testarchiv. Trier. [cited 6 August 2010]. Available from: http://www.zpid.de/index.php?wahl=products&uwahl=frei&uuwahl=testarchiveintro. |
| 34. | Azim HF, Piper WE, Segal PM, Nixon GW, Duncan SC. The Quality of Object Relations Scale. Bull Menninger Clin. 1991;55:323-343. [PubMed] |
| 35. | Lindfors O, Knekt P, Virtala E, Haaramo P. Concurrent validity of the Quality of Object Relations Scale (QORS) in relation to proxy assessment of the theoretical scale constituents. Psychopathology. 2013;46:111-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 36. | Löffler-Stastka H. German version of the Psychotherapy Relationship Questionnaire (Westen, D. 2005); 2006. Available from: Löffler-Stastka H. Unpublished. |
| 37. | Bradley R, Heim AK, Westen D. Transference patterns in the psychotherapy of personality disorders: empirical investigation. Br J Psychiatry. 2005;186:342-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 38. | Tanzilli A, Colli A, Gualco I, Lingiardi V. Patient Personality and Relational Patterns in Psychotherapy: Factor Structure, Reliability, and Validity of the Psychotherapy Relationship Questionnaire. J Pers Assess. 2018;100:96-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 39. | Horvath AO, Symonds BD. Relation between working alliance and outcome in psychotherapy: A meta-analysis. J Couns Psychol. 1991;38:139-149. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1292] [Cited by in RCA: 1306] [Article Influence: 38.4] [Reference Citation Analysis (0)] |
| 40. | Jones EE, Windholz M. The psychoanalytic case study: toward a method for systematic inquiry. J Am Psychoanal Assoc. 1990;38:985-1015. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 42] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 41. | Albani C, Blaser G, Jacobs U, Jones E, Geyer M, Kachele H. Die Methode des, Psychotherapie-Prezess Q-Sort. Z Klein Psychol Psychopathol Psychother. 2000;48:151-171. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 42. | Astor J. Is transference the 'total situation'? J Anal Psychol. 2001;46:415-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 43. | Hornik K. The R FAQ. [cited 6 August 2020]. Available from: https://cran.r-project.org/doc/FAQ/R-FAQ.html. |
| 44. | Fonagy P, Target M. Predictors of outcome in child psychoanalysis: a retrospective study of 763 cases at the Anna Freud Centre. J Am Psychoanal Assoc. 1996;44:27-77. [RCA] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 75] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 45. | Steiner J. Seeing and being seen: narcissistic pride and narcissistic humiliation. Int J Psychoanal. 2006;87:939-951. [RCA] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 43] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 46. | Steiner J. Transference to the analyst as an excluded observer. Int J Psychoanal. 2008;89:39-54. [RCA] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 47. | Joseph B. Psychic change and the psychoanalytic process. In: Schafer RE. The contemporary Kleinians of London. Madison: International Universities Press, 1997: 395–409. |
| 48. | Strachey J. The nature of the therapeutic action of psycho-analysis. 1934. J Psychother Pract Res. 1999;8:66-82; discussion 64. [PubMed] |
| 49. | Schafer RE, Steiner J. Problems of psychoanalytic technique: patient-centered and analyst-centered interpretations. In: Schafer RE. The contemporary Kleinians of London. Madison: International Universities Press, 1997: 372–392. |
| 50. | Levy KN, Clarkin JF, Yeomans FE, Scott LN, Wasserman RH, Kernberg OF. The mechanisms of change in the treatment of borderline personality disorder with transference focused psychotherapy. J Clin Psychol. 2006;62:481-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 119] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 51. | Etechegoyen RH. Fundamentals of psychoanalytic technique. London: Karnac, 1991: 1-912. |
| 52. | Bortolla R, Cavicchioli M, Fossati A, Maffei C. Emotional Reactivity in Borderline Personality Disorder: Theoretical Considerations Based on a Meta-Analytic Review of Laboratory Studies. J Pers Disord. 2020;34:64-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 53. | Yeomans FE, Gutfreund J, Selzer MA, Clarkin JF, Hull JW, Smith TE. Factors Related to Drop-outs by Borderline Patients: Treatment Contract and Therapeutic Alliance. J Psychother Pract Res. 1994;3:16-24. [PubMed] |
| 54. | Loffler-Stastka H, Blueml V, Boes C. Exploration of personality factors and their predictive impact on therapy utilization: the externalizing mode of functioning. Psychother Res. 2010;20:295-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 55. | Shea MT, Elkin I, Imber SD, Sotsky SM, Watkins JT, Collins JF, Pilkonis PA, Beckham E, Glass DR, Dolan RT. Course of depressive symptoms over follow-up. Findings from the National Institute of Mental Health Treatment of Depression Collaborative Research Program. Arch Gen Psychiatry. 1992;49:782-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 342] [Cited by in RCA: 245] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 56. | Biskin RS. The Lifetime Course of Borderline Personality Disorder. Can J Psychiatry. 2015;60:303-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 80] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 57. | Degasperi G, Cristea IA, Di Rosa E, Costa C, Gentili C. Parsing variability in borderline personality disorder: a meta-analysis of neuroimaging studies. Transl Psychiatry. 2021;11:314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 58. | Jenkins DG, Quintana-Ascencio PF. A solution to minimum sample size for regressions. PLoS One. 2020;15:e0229345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 148] [Cited by in RCA: 234] [Article Influence: 46.8] [Reference Citation Analysis (1)] |
| 59. | Zimmermann J, Löffler-Stastka H, Huber D, Klug G, Alhabbo S, Bock A, Benecke C. Is It All about the Higher Dose? Clin Psychol Psychother. 2015;22:469-487. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 60. | Storebø OJ, Stoffers-Winterling JM, Völlm BA, Kongerslev MT, Mattivi JT, Jørgensen MS, Faltinsen E, Todorovac A, Sales CP, Callesen HE, Lieb K, Simonsen E. Psychological therapies for people with borderline personality disorder. Cochrane Database Syst Rev. 2020;5:CD012955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 145] [Article Influence: 29.0] [Reference Citation Analysis (0)] |
| 61. | Finch EF, Iliakis EA, Masland SR, Choi-Kain LW. A meta-analysis of treatment as usual for borderline personality disorder. Personal Disord. 2019;10:491-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 62. | Zahediabghari S, Boursiquot P, Links P. Impact of Psychotherapy on Psychosocial Functioning in Borderline Personality Disorder Patients. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 63. | Cristea IA, Gentili C, Cotet CD, Palomba D, Barbui C, Cuijpers P. Efficacy of Psychotherapies for Borderline Personality Disorder: A Systematic Review and Meta-analysis. JAMA Psychiatry. 2017;74:319-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 336] [Cited by in RCA: 381] [Article Influence: 47.6] [Reference Citation Analysis (0)] |