Copyright
©The Author(s) 2021.
World J Psychiatr. Nov 19, 2021; 11(11): 1053-1064
Published online Nov 19, 2021. doi: 10.5498/wjp.v11.i11.1053
Published online Nov 19, 2021. doi: 10.5498/wjp.v11.i11.1053
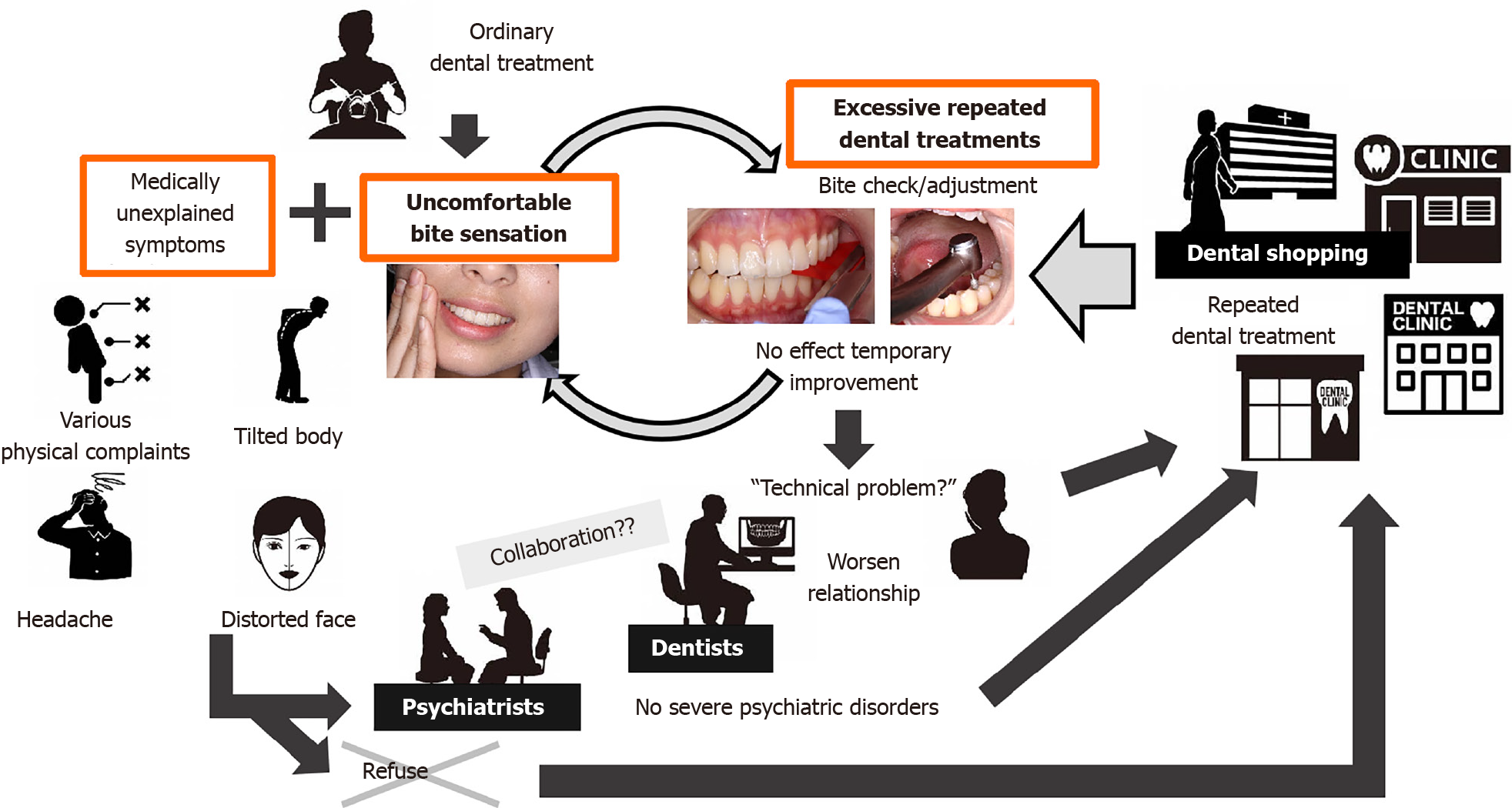
Figure 1 A typical course of phantom bite syndrome.
Those nomadic patients usually travel from one dentist to another, desperately seeking an “ideal bite correction”. They normally refuse to see psychiatrists if being referred.
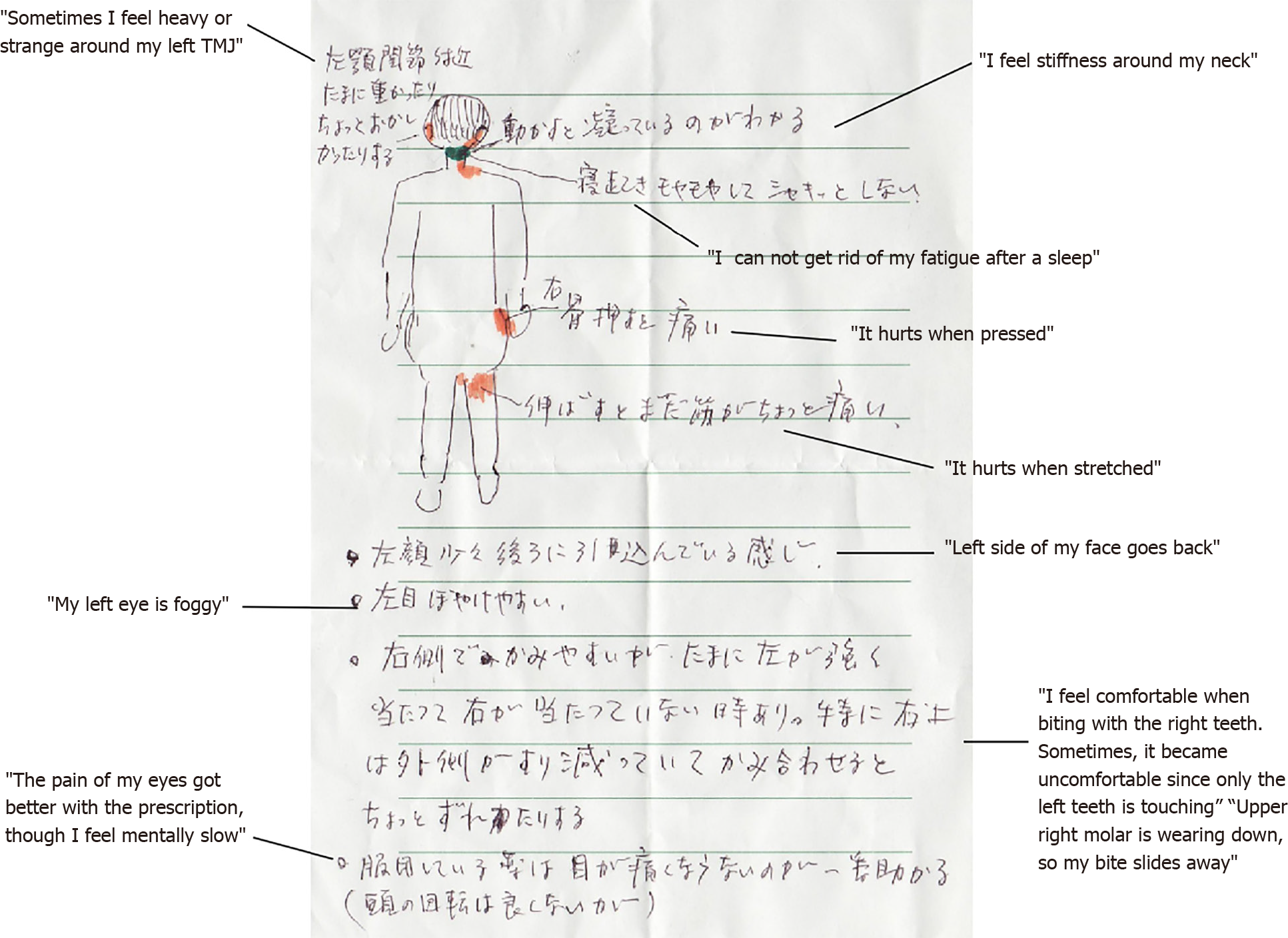
Figure 2 A written self-report of patient’s multiple comorbidities of medically unexplained symptoms (e.
g., headache, dizziness, neck and back pain, ambulatory impairment, numbness of hands and legs) associated with occlusal symptoms.
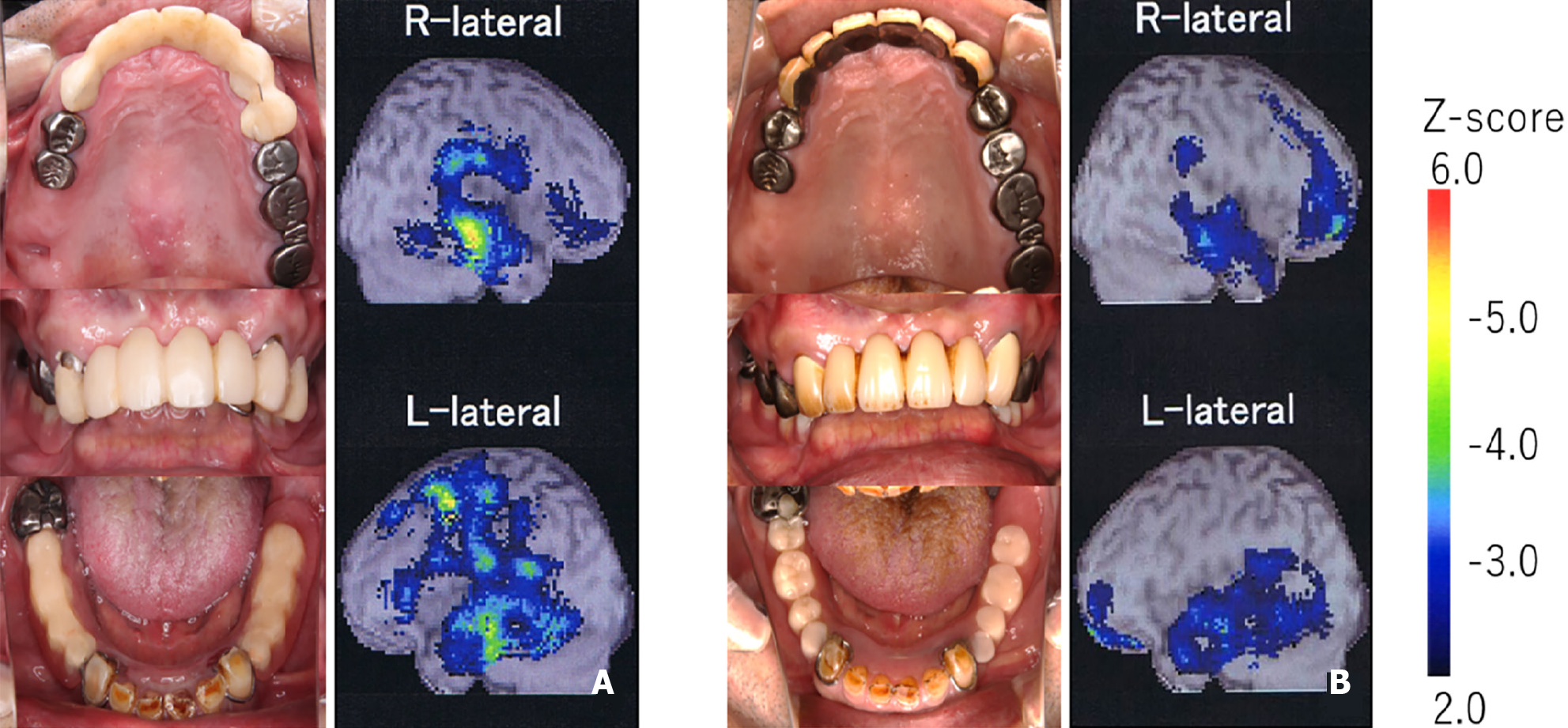
Figure 3 Occlusal view of mandibular arch in a 60-yr-old female phantom bite syndrome patient.
Clinical examination revealed unnatural restorations for dentition owing to the fullest effort of dentists.
Figure 4 Intra-oral photography and regional cerebral blood flow increasing map before and after phantom bite syndrome psychopharmacotherapy.
The color bar indicates the Z-score comparing normal controls. A and B: The before (A) and after (B) pharmacotherapy. As the phantom bite symptom decreased, the asymmetrical regional cerebral blood flow pattern attenuated, and dental treatment was finally completed. Citation: Umezaki Y, Watanabe M, Takenoshita M, Yoshikawa T, Sakuma T, Sako E, Katagiri A, Sato Y, Toyofuku A. A case of phantom bite syndrome ameliorated with the attenuation of the asymmetrical pattern of regional cerebral blood flow. Jpn J Psychosom Dent 2013; 28: 30-34. Copyright ©The Japanese Society of Psychosomatic Dentistry 2013. Published by The Japanese Society of Psychosomatic Dentistry[16].
- Citation: Tu TTH, Watanabe M, Nayanar GK, Umezaki Y, Motomura H, Sato Y, Toyofuku A. Phantom bite syndrome: Revelation from clinically focused review. World J Psychiatr 2021; 11(11): 1053-1064
- URL: https://www.wjgnet.com/2220-3206/full/v11/i11/1053.htm
- DOI: https://dx.doi.org/10.5498/wjp.v11.i11.1053