Copyright
©2013 Baishideng Publishing Group Co.
World J Clin Pediatr. Nov 8, 2013; 2(4): 54-64
Published online Nov 8, 2013. doi: 10.5409/wjcp.v2.i4.54
Published online Nov 8, 2013. doi: 10.5409/wjcp.v2.i4.54
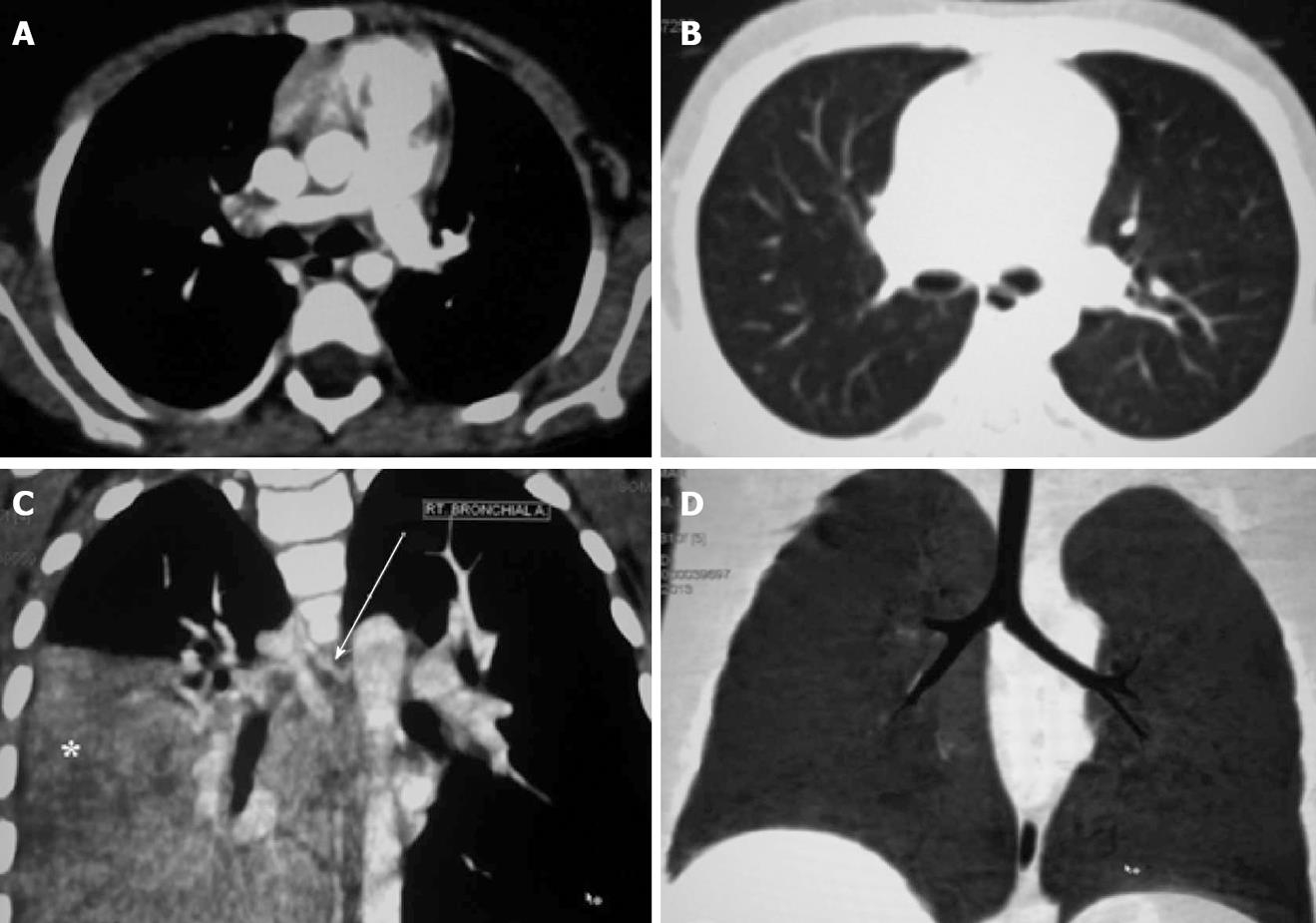
Figure 1 Multi-detector computed tomography image interpretation.
Axial computed tomography image showing mediastinal window (A) and lung window (B). Coronal maximum intensity projection image (C) demonstrating the origin and proximal portion of the right bronchial artery (arrow). There is consolidation in the right lower lobe (asterisk). Coronal Minimum Intensity Projection image (D) delineating the central airways.
Figure 2 Chest radiograph (A) and axial computed tomography image (B) showing consolidation with cavitation in the left upper lobe.
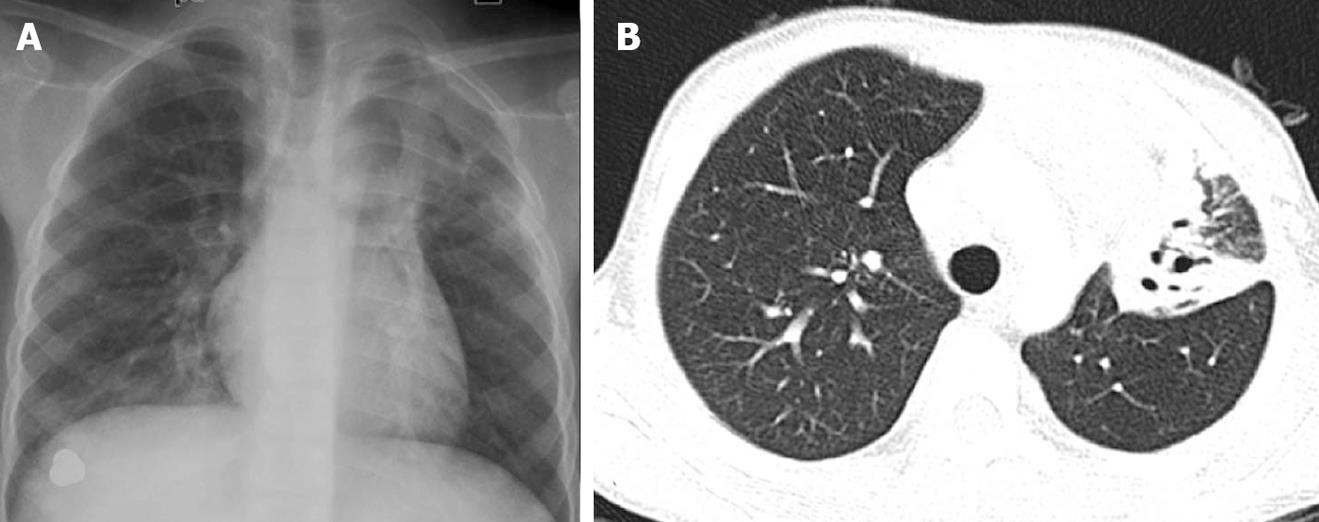
Figure 3 A seven-year-old girl with ruptured pulmonary hydatid cyst.
Axial computed tomography image (A) showing the ruptured cyst with air (asterisk) in the right upper lobe along with surrounding consolidation. Axial section of the abdomen (B) shows an unruptured cyst in the segment VI of the liver.
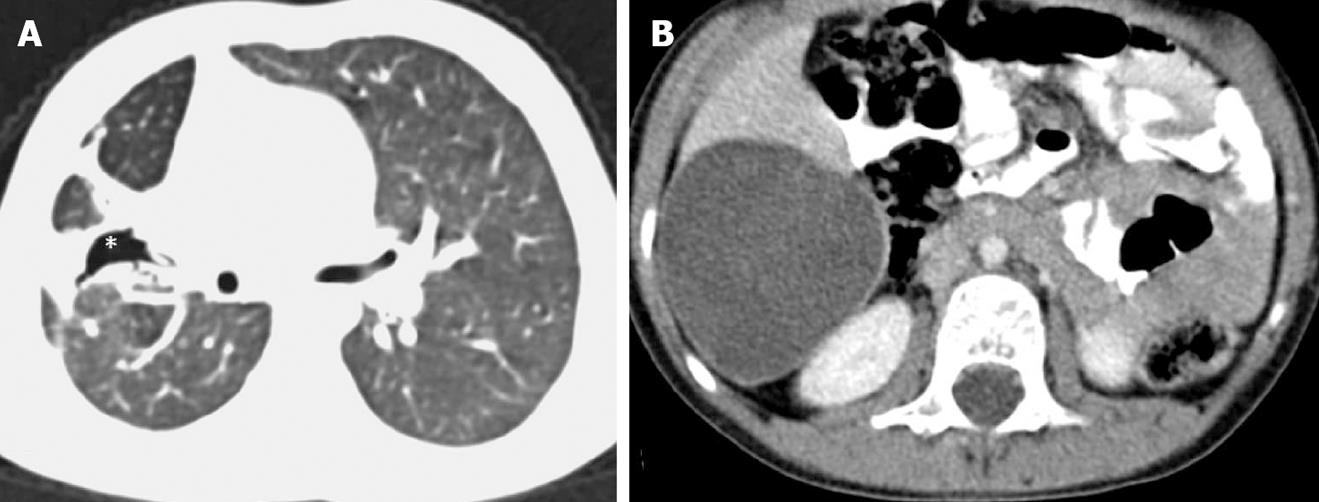
Figure 4 A 12-year-old girl with allergic bronchopulmonary aspergillosis.
Frontal chest radiograph (A) and axial computed tomography (CT) image (B) showing tubular opacities with consolidation in the right lung suggestive of mucoceles along with cystic bronchiectasis in bilateral lungs. Coronal CT image (C) of the patient showing evidence of bilateral allergic fungal rhinosinusitis.
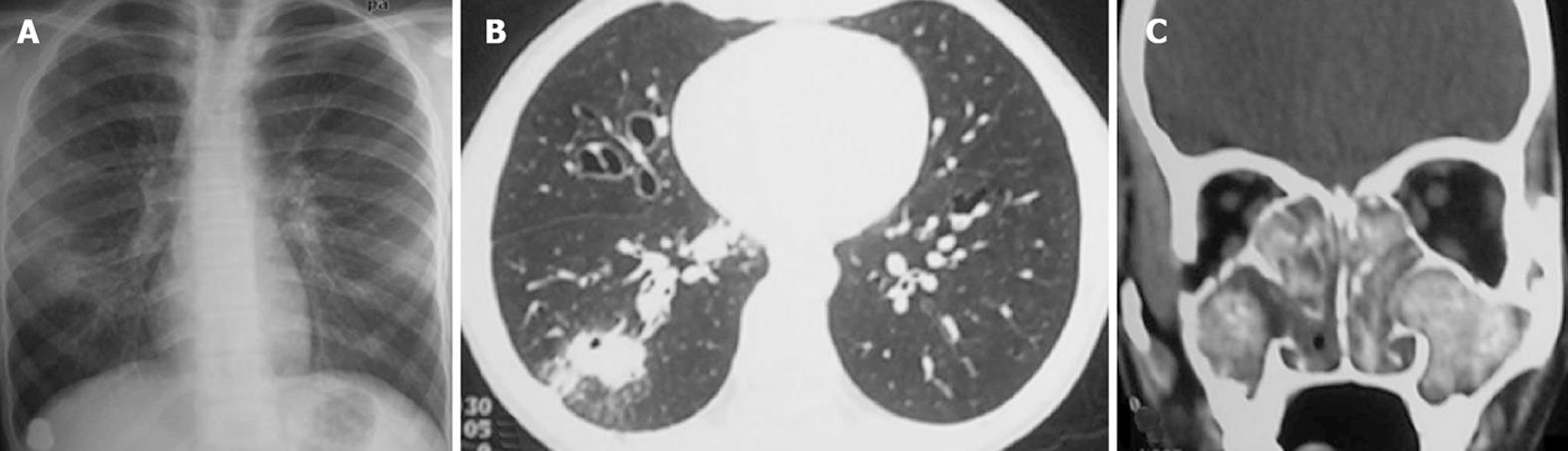
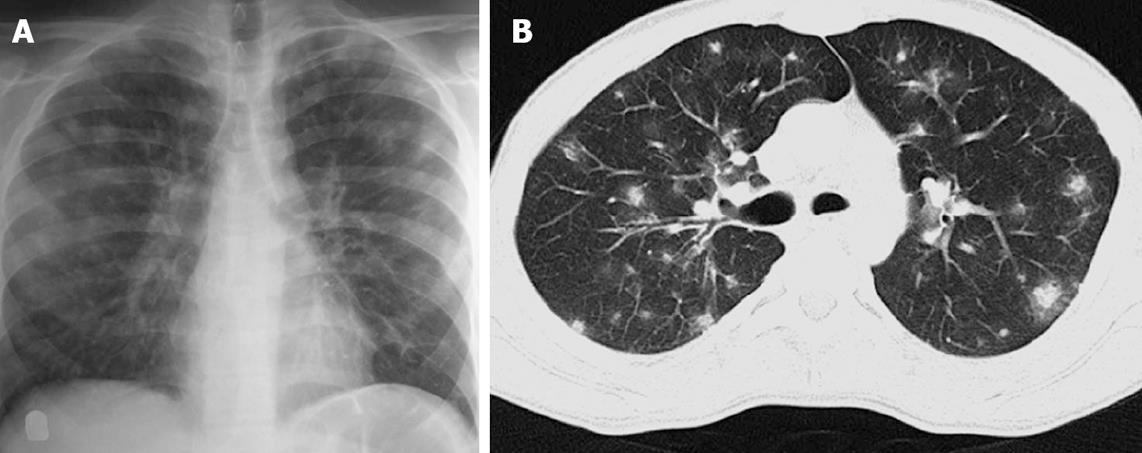
Figure 5 A 17-year-old boy with acute lymphocytic leukemia along with angioinvasive aspergillosis.
Chest radiograph (A) showing multiple fluffy nodules in bilateral lung fields. High resolution CT image (B) of the same patient shows multiple nodules with surrounding ground glass opacity (halo sign).
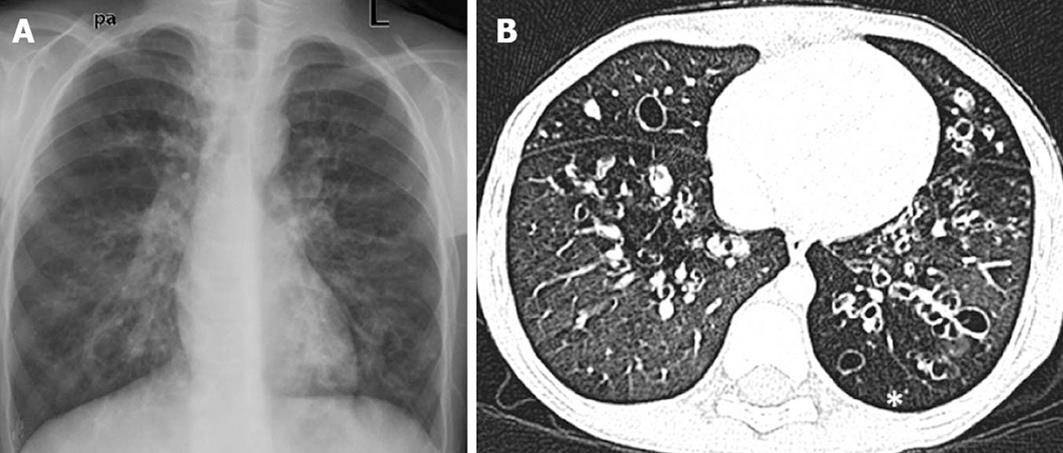
Figure 6 A 10-year-old boy with post-infectious bronchiectasis.
Frontal chest radiograph (A) showing multiple cystic lucencies and tubular opacities in both lungs. Chest high resolution CT image (B) shows multiple areas of cystic bronchiectasis with associated air trapping (asterisk).
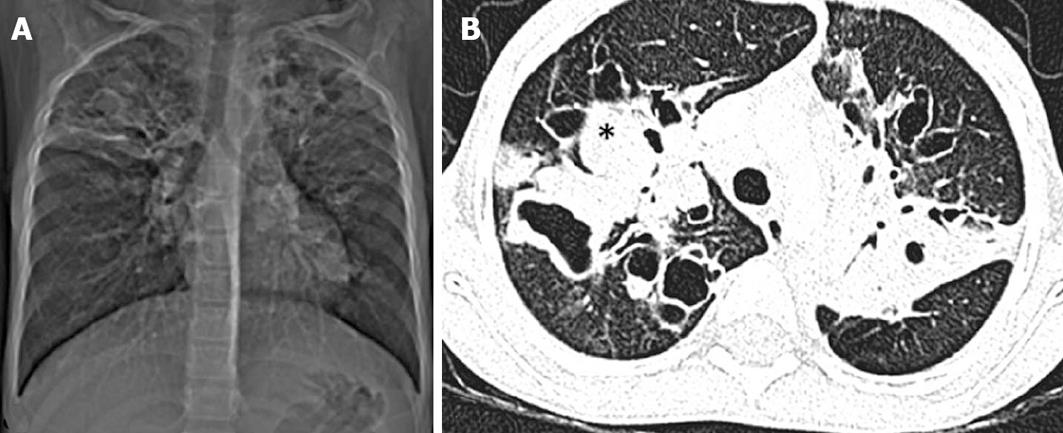
Figure 7 A 7-year-old boy with cystic fibrosis.
Computed tomography (CT) scout image (A) and axial CT chest image (B) showing bilateral upper lobe bronchiectasis with bronchocele formation (asterisk) due to mucous plugging and sparing of lower zones.
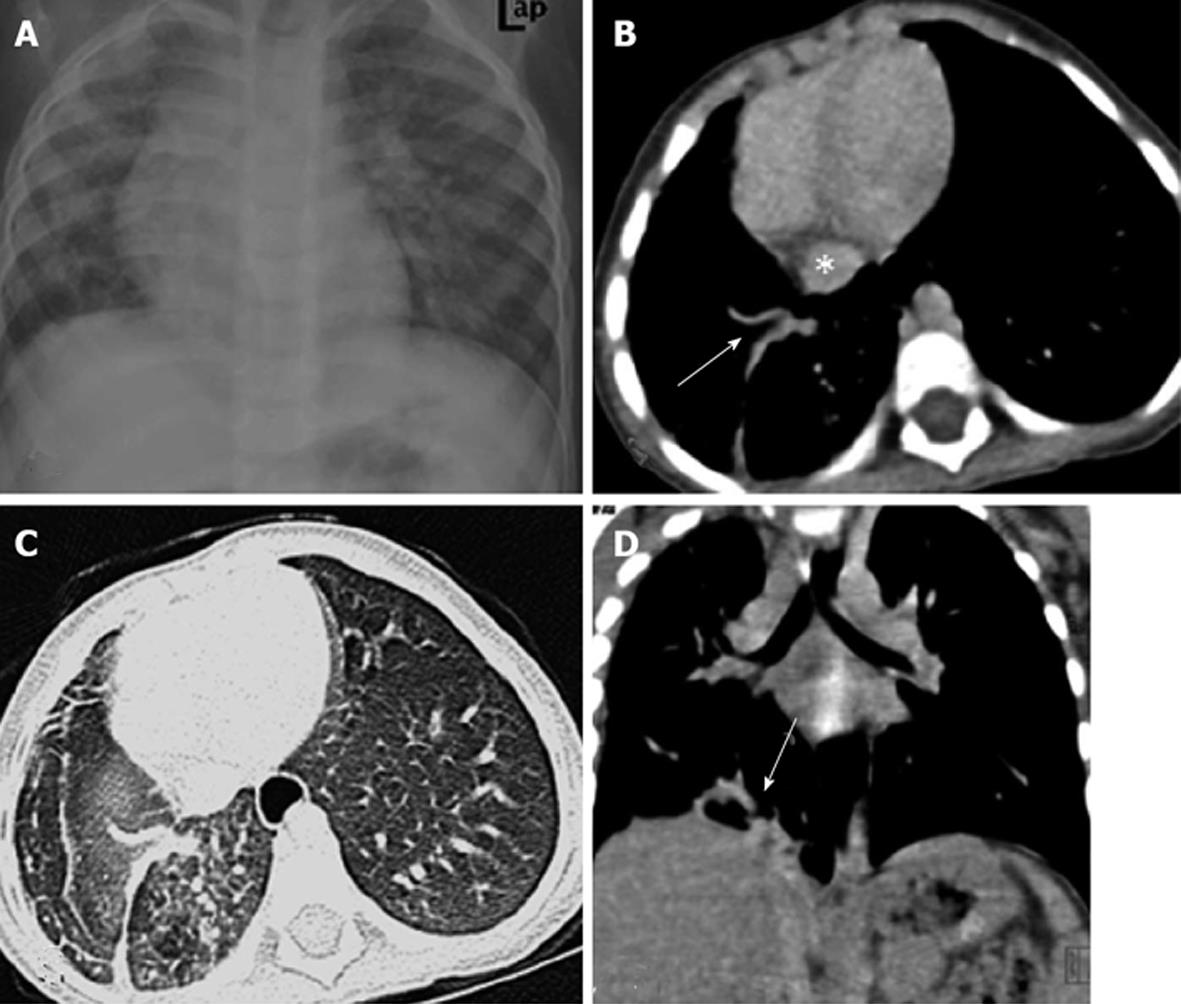
Figure 8 Pulmonary venolobar hypoplasia.
Chest radiograph (A) shows volume loss of the right hemithorax with ipsilateral mediastinal shift. Contrast-enhanced computed tomography images (B-D) showing anomalous right inferior pulmonary vein (arrows) coursing inferiorly towards the inferior vena cava (asterisk).
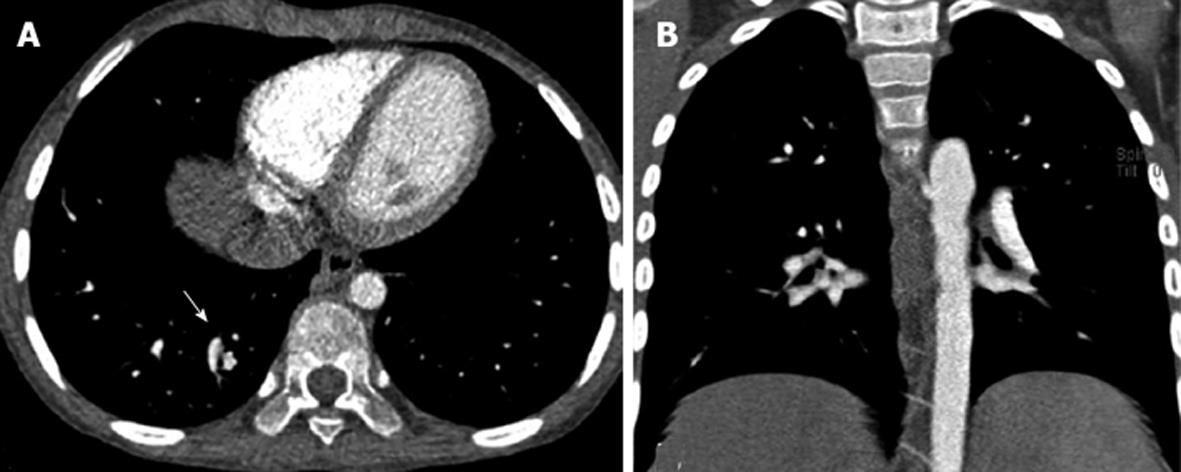
Figure 9 Pulmonary arteriovenous malformation.
Axial (A) and coronal (B) computed tomography images showing abnormal communication between branches of the pulmonary artery and vein in right lower lobe (arrows).
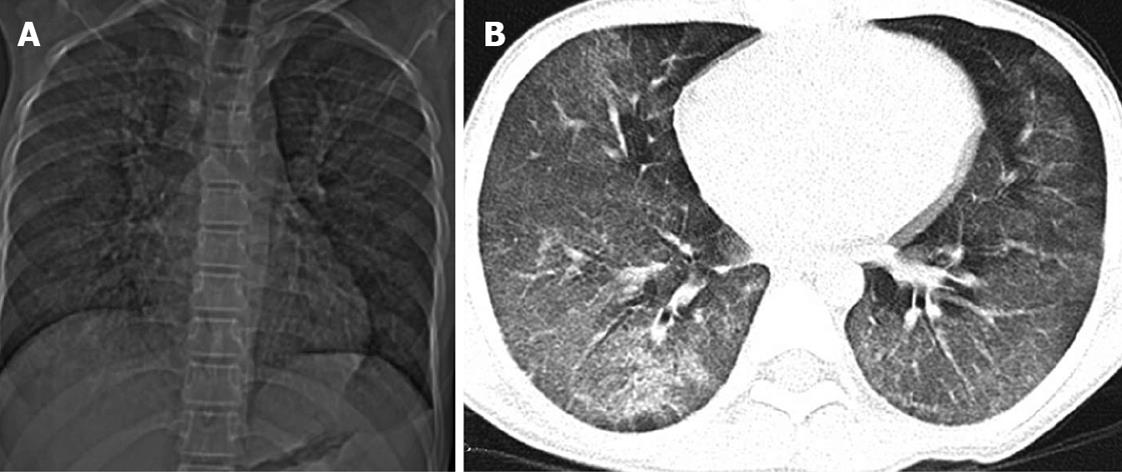
Figure 10 A 15-year-old boy with idiopathic pulmonary hemosiderosis.
Scout computed tomography (CT) image (A) and axial CT image (B) showing diffuse ground glass opacity in bilateral lungs.
Figure 11 Foreign body aspiration.
Chest radiograph (A) shows a radio-opaque foreign body in the left main bronchus (arrow) with hyperinflation of the left lung. Axial computed tomography images (B, C) delineate the morphology of the foreign body in the left main bronchus causing luminal compromise. There is associated air trapping in the left lung with patchy consolidation in the apical segment of the lower lobe.
Figure 12 Bronchial carcinoid.
Scout computed tomography (CT) image (A) revealing non-visualization of the right main bronchus with volume loss and opacification of the right hemithorax along with bronchiectasis in right lower zone. Axial CT image (B) shows a mass in the right lung with mediastinal infiltration. Coronal Minimum Intensity Projection image (C) shows the outline of the mass projecting in the right main bronchus along with bronchiectasis in the right lower lobe.
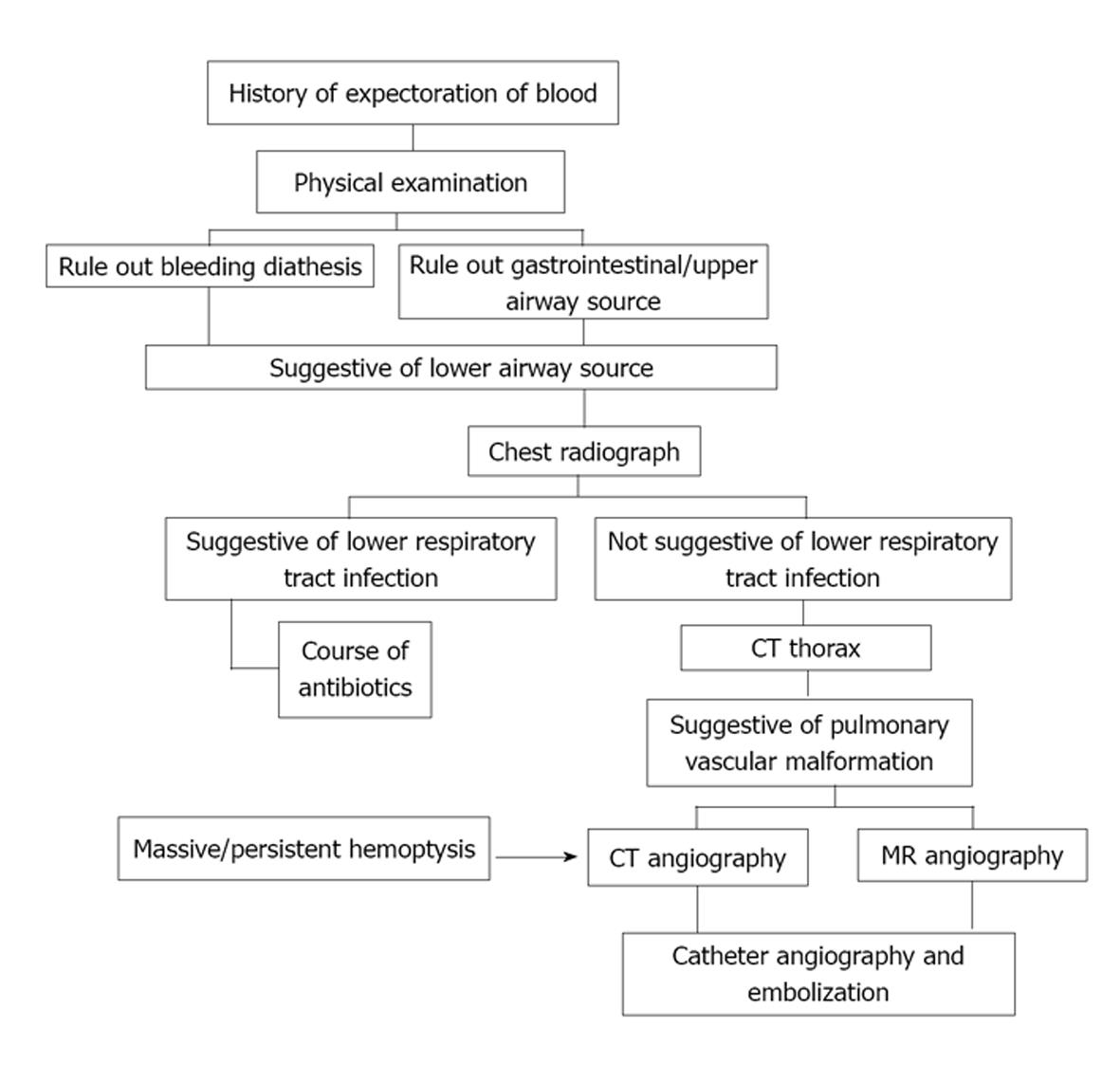
Figure 13 Flowchart depicting approach to a child presenting with hemoptysis.
MR: Magnetic resonance; CT: Computed tomography.
- Citation: Singh D, Bhalla AS, Veedu PT, Arora A. Imaging evaluation of hemoptysis in children. World J Clin Pediatr 2013; 2(4): 54-64
- URL: https://www.wjgnet.com/2219-2808/full/v2/i4/54.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v2.i4.54