Published online Feb 20, 2015. doi: 10.5321/wjs.v4.i1.29
Peer-review started: September 30, 2014
First decision: October 21, 2014
Revised: November 14, 2014
Accepted: December 3, 2014
Article in press: January 12, 2015
Published online: February 20, 2015
Processing time: 138 Days and 16.3 Hours
Central giant cell granuloma (CGCG) is found exclusively in jaws. Its etiopathogenesis is unclear; however it is suggested that it can arise as a reactive response to trauma. This report describes an aggressive variety of CGCG which raises a question; can extraction of tooth modify the behavior of CGCG? A 46 years old male had reported with a rapidly increasing intraoral and extraoral swelling of lower jaw following tooth extraction. Radiographic examination revealed a large multilocular lesion involving the body and ramus of mandible which had been proved to be aggressive CGCG on histopathological examination. The importance of radiographic examination prior to extraction of teeth and importance of inclusion of CGCG in jaw swellings associated with mobility of teeth or failure of healing sockets is emphasized.
Core tip: This report describes an aggressive variety of central giant cell granuloma (CGCG) after extraction which raises a question; can extraction of tooth modify the behavior of CGCG? The importance of radiographic examination prior to extraction of teeth and importance of inclusion of CGCG in jaw swellings associated with mobility of teeth or failure of healing sockets is emphasized. Literature about clarity in clinical behavior, radiographic features and various treatment modalities of this one of the bony lesion of jaws are reviewed.
- Citation: Dangore-Khasbage S, Degwekar SS, Bhowate RR, Hande AH, Lohe VK. Unusual aggressive behavior of central giant cell granuloma following tooth extraction. World J Stomatol 2015; 4(1): 29-34
- URL: https://www.wjgnet.com/2218-6263/full/v4/i1/29.htm
- DOI: https://dx.doi.org/10.5321/wjs.v4.i1.29
Central giant cell granuloma (CGCG) has unpredictable biologic behavior, non-specific radiographic features and is amenable to a plethora of treatment alternatives. A reactive response to trauma is the most accepted etiopathogenesis of CGCG[1-3]. This report describes a case of an aggressive variety of CGCG which was augmented following extraction of teeth. This is a rare presentation of CGCG and it suggests two important things, as delay in diagnosis has an important implication on morbidity and mortality of the patient. (1) The necessity of radiographic examination prior to extraction of teeth; and (2) importance of early histopathological examination, if extraction socket fails to heal should not be underestimated. Though abundant literature is available regarding this well known entity, case reports are still considered to be the source of information.
A 46 years old male reported to the Department of Oral Diagnosis and Medicine at Sharad Pawar Dental College and Hospital, Wardha, India, with a chief complaint of progressive extraoral and intraoral swelling on lower right back region of the jaw since 2 mo. History of present illness revealed that approximately three months ago patient had noticed mobility of the teeth in same region and all his molars were extracted from that quadrant. This had resulted in failure of healing of the extraction socket and development of rapidly enlarging extraoral and intraoral swelling 1 mo post-extraction. There was associated pain too. As a result of intraoral swelling the patient had difficulty in chewing, swallowing and speaking as these processes were aggravating the pain. There was no history of discharge from the swelling. The patient was of moderate build and healthy weight. The general systemic examination did not reveal any major illness.
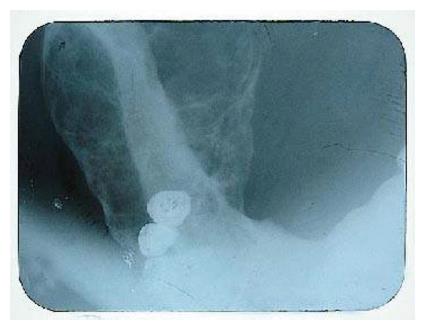
On extraoral examination, there was diffuse swelling on lower right side of face resulting in marked facial asymmetry as shown in Figure 1. Palpation elicited that the swelling was bony hard, non-tender, fixed to the underlying structures and with no pulsations. Local Temperature was not raised. There were no signs of loss of sensory function.
Intraoral examination revealed missing lower right molars with an exophytic soft tissue growth from the residual socket and well-circumscribed ovoid swelling of approximately 4 cm × 6 cm in posterior region of right side of the mandible causing bucco-lingual expansion of the jaw with marks of indentation on overlying mucosa. (Figure 2). The swelling was firm in consistency, slightly tender and was fixed to underlying structures. On the basis of history and clinical features, provisional diagnosis was malignant tumor. Investigations were carried out to evaluate the case.
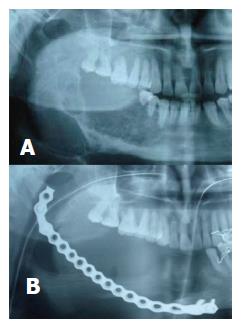
Lateral mandibular occlusal view showed single large multilocular radiolucent lesion having well defined periphery with predominant buccal and lingual expansion and thinned-out of cortical plates (Figure 3). A panoramic radiograph revealed a single large mutilocular radiolucent lesion involving the body (honey comb appearance) and ramus (soap bubble appearance) on right side of mandible extending anteroposteriorly from the canine to posterior border of ramus and superoinferiorly from sigmoid notch to inferior border of mandible in ramus region and from alveolar crest to inferior border of mandible in body region as illustrated in Figure 4A. The periphery of the lesion was well defined and scalloped. There was resorption and thinning of superior and inferior cortices, roots resorption as well as expansion at the inferior border of mandible.
On the basis of radiographic findings, probability of ameloblastoma was considered while various benign tumors and multilocular cysts were considered in differential diagnosis. The lesion was subjected to fine needle aspiration biopsy which was non productive. Then an incisional biopsy of the lesion was performed. Results of the biopsy showed the features suggestive of CGCG. An attempt was made to exclude the brown tumor of the hyperparathyroidism by undergoing biochemical tests (serum calcium, phosphorus, alkaline phosphates, and parathyroid hormone) which were within normal limits.
As surgery is the most accepted and traditional form of treatment for CGCG especially in the aggressive type and as there was absence of any systemic disease which could complicate the surgical treatment, surgery was chosen as a treatment of choice in this case.
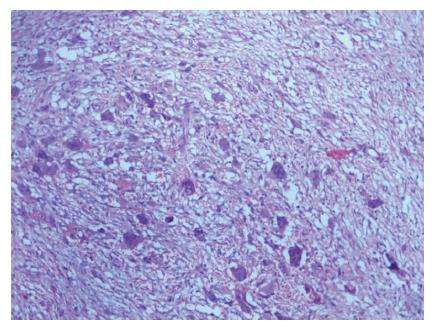
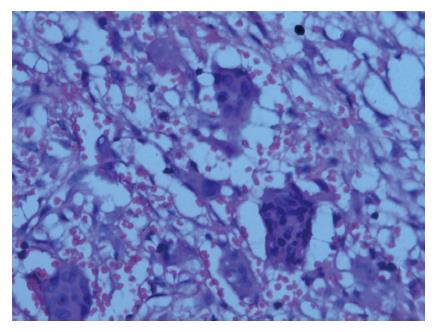
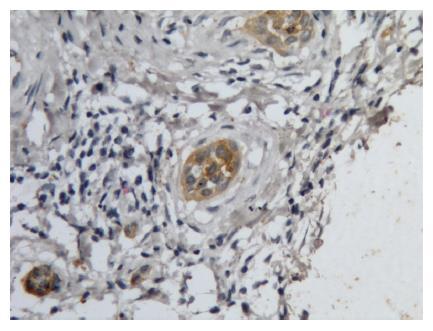
Under general anesthesia the surgical excision of the lesion was performed by hemimandibulectomy and a reconstruction plate was inserted to repair the defect (Figure 4B). Post-operative healing was uneventful. The specimen was sent for histopathological examination. Hematoxylin and Eosin stained section showed highly cellular fibrous connective tissue stroma, which consisted of many plump fibroblasts, extravagated blood elements and numerous multinucleated giant cells, containing nuclei ranging from 5-20 in numbers and uniformly scattered throughout the lesion (Figures 5 and 6). The clinic-pathological diagnosis was compatible with aggressive CGCG. To confirm the origin of giant cells, the tissue was analyzed by immunohistochemistry by cytokeratin expression and giant cells were found to be positive for cytokeratin which confirmed the diagnosis (Figure 7). Clinical and radiographic examination after six months following surgery revealed uncomplicated recovery and no recurrence.
CGCG is an intra-osseous destructive lesion of jaws which has definite predilection for mandibular anterior region and has a tendency to cross the midline though controversial results also exist[4-7]. It rarely occurs in areas elsewhere other than the jaws like maxillary sinus, temporal bone, cranial vault and other bones of the craniofacial complex[4].
The etiopathogenesis of CGCG can be an exacerbated reparative process related to previous trauma and intraosseous hemorrhage that triggers the reactive granulomatous process[8,9]. In the present case, we can assume that trauma due to extraction might be responsible for change in behavior (rapid progress) of the lesion since the lesion grew rapidly and perforated intraorally after molar extractions. Similar such cases are rarely reported in the literature[9,10]. However, this type of clinical presentation is commonly observed in oral malignancy which was ruled out by radiographic examination in the present case.
Basically CGCG is a benign entity but based on its clinical behavior and radiographic features, it has been classified into non-aggressive and aggressive variety[1,11]. Aggressive CGCG is found in younger patients while in this regards, the present case was distinct showing features of aggressive variety at advanced age.
Although aggressive lesion is expansive and invasive, paresthesia is usually not observed in these patients. However, Whitaker et al[5] reported paresthesia in 6% of their cases. Bataineh et al[12] have suggested the remedy to avoid distressing paresthesia or painful dysesthesia.
Amongst aggressive and non-aggressive types of CGCG, the controversial reports are observed in histologic differences. Few authors stated that there are no histologic differences between aggressive and non aggressive varieties[1,11]. Ahuja et al[13] reported high cellularity and a vesiculated fibroblastic population in aggressive CGCG while a minimal-moderate cellularity and a non vesiculated fibroblast population in non-aggressive cases[13]. Shetty et al[14] explained that the number of giant cells and number of nuclei within alone does not determine aggressive nature and recurrence of CGCG.
CGCG can present different radiological features, from small unilocular radiolucent lesions to extensive multilocular radiolucent areas. Wood et al[6] reported that the lesion may initially occur as a solitary-cyst like radiolucency and as it grows larger it may develop architecture of a soap bubble or honeycomb type of mutilocular radiolucency. Presence of wispy trabeculae within the lesion is the most significant radiographic sign associated with CGCG[2,5,6]. Though radiolucent is the commonest radiographic internal structure of CGCG (87.5%), Kaffe et al[7] have observed mixed (10%) and radiopaque (2.5) appearances too. Generally the periphery of CGCG is well defined but many times it presents with ill defined, diffused borders[7,15]. There may be a cortical radiopaque halo and dental displacement or root resorption[1,2]. Stavropoulos et al[16] and Jose et al[15] have found radicular resorption in 37% and 15.4% of cases respectively.
Overall above description suggests that the clinical and radiographic features of CGCG are non pathognomic and are often confused with several other lesions of the jaws that pose challenge to oral diagnostician. In this case also the provisional diagnosis considered was oral malignancy and radiological diagnosis was ameloblastoma. The present case justify radiographic examination before extraction of molars as failure of which resulted in an extensive lesion involving the body and ramus entirely due to modification in behavior of lesion following extractions. It also suggests inclusion of CGCG in jaw swellings associated with mobility of teeth and failure of healing sockets.
It is equally important to exclude brown tumors associated with hyperparathyroidism from CGCG as they share identical clinical and radiological features[15]. This differentiation depends on laboratory tests for investigating serum levels of calcium, phosphorus and alkaline phosphatase which, in cases of hyperparathyroidism, present alterations[2]. Ahuja et al[13] presented difficulty in diagnosing aggressive CGCG from Giant cell tumors with which they share similar histopathology, behavior and prognosis. Histologically, CGCG is indistinguishable from other giant cell lesions of the bone like cherubism and aneurysmal bone cyst too. But, in the present case immunohistochemcal expression of cytokeratin in giant cells helped to confirm the diagnosis. In multiregional cases of CGCG, cherubism, neurofibromatosis type 1 and Noonan syndrome must be considered in differential diagnosis[6,17]. A combination of CGCG with some other lesions like fibro osseous lesions called as hybrid lesions is also reported in the literature[18,19].
Traditionally the most accepted treatment of CGCG of the jaws is surgical while successful medicinal treatment modalities are also reported in the literature; each has got its own advantages and disadvantages[20-22]. Surgical approach may result in loss of teeth, disfigurement and loss of dental germs (in younger patients)[12,23]. Whitaker et al[5] have mentioned the recurrence rate of CGCG as 4% to 20% and the reasons were larger lesion and incomplete removal of the tumor. Radiation therapy is contraindicated in CGCG[3].
An alternative nonsurgical approaches are intralesional corticosteroid injections, calcitonin injections and subcutaneous interferon injections[20,23,24]. Weekly intralesional injections of corticosteroids are believed to inhibit the bone resorption by controlling proliferation and differentiation of osteoclasts. However, this is contraindicated in certain conditions like diabetes mellitus, peptic ulcer and immunocompromised state[21,23,24]. Calcitonin act by inhibiting the calcitonin receptors that are present on giant cells thereby inhibiting osteoclastogenesis[17,25]. Interferons have anti-angiogenic effect and inhibition of bone resorption[1]. Nalan et al[26] have used the combination of surgical and medicinal treatment in their patient. Non surgical treatment options are simple, inexpensive, save vital structures and avoid facial deformity[2,23].
In conclusion, though the classic presentation of CGCG is a slow growing benign lesion in mandibular anterior region in a young patient, variable clinical appearances exist. Thus, it is still a topic of keen interest to study about clarity in clinical behavior, radiographic features and various treatment modalities of this one of the bony lesion of jaws.
A 46 years old male had reported with a rapidly increasing intraoral and extraoral swelling of lower jaw following tooth extraction.
Extraorally bony hard, non-tender swelling on lower right side of face and exophytic soft tissue growth from the residual socket intraorally.
Provisional diagnosis was malignant tumor.
Serum calcium, phosphorus, alkaline phosphates, and parathyroid hormone which were within normal limits. Thus, exclude the brown tumor of the hyperparathyroidism.
Lateral mandibular occlusal view and a panoramic radiograph showed single large multilocular radiolucent lesion having well defined periphery with predominant buccal and lingual expansion and thinned-out of cortical plates suggested benign tumor like ameloblastoma.
Biopsy showed highly cellular fibrous connective tissue stroma, which consisted of many plump fibroblasts, extravagated blood elements and numerous multinucleated giant cells. These features were diagnostic of central giant cell granuloma (CGCG).
Surgery was chosen as a treatment of choice.
Immunohistochemistry by cytokeratin expression and giant cells were found to be positive for cytokeratin which confirmed the diagnosis of CGCG.
An aggressive variety of CGCG which was augmented following extraction of teeth is described.
The necessity of radiographic examination prior to extraction of teeth, and the importance of early histopathological examination, if extraction socket fails to heal should not be underestimated.
The case report shows some valuable information to understand the diagnosis and treatment for this disease in future. The manuscript is written well and organized reasonable.
P- Reviewer: Guo X, Kawano K, Vieth M S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK
| 1. | Chi AC. Bone pathology. Oral and Maxillofacial Pathology. New York: WB Saunders 2009; 626-629. |
| 2. | White SC, Pharoah MJ. Diseases of bone manifested in jaws. Oral radiology: principles and interpretation. St. Louis: MO- CV Mosby 2004; 501-503. |
| 3. | Rajendran R, Sivapatha SB. Shafer‘s Textbook of Oral Pathology. 5th ed. Elsevier. 2007;187-188. |
| 4. | Nandimath KR, Naikmasur VG, Babshet MP. Central Giant Cell Granuloma - A rare presentation. Webmed Central Oral Medicine. 2011;2:WMC001466. [DOI] [Full Text] |
| 5. | Whitaker SB, Waldron CA. Central giant cell lesions of the jaws. A clinical, radiologic, and histopathologic study. Oral Surg Oral Med Oral Pathol. 1993;75:199-208. [PubMed] [DOI] [Full Text] |
| 6. | Wood NK, Goaz PW, Kallal RH. Multilocular radiolucencies. Differential diagnosis of oral and maxillofacial lesions. St Louis: MO, Mosby-Year Book 2005; 340, 341, 353. |
| 7. | Kaffe I, Ardekian L, Taicher S, Littner MM, Buchner A. Radiologic features of central giant cell granuloma of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81:720-726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 92] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 8. | Ustündağ E, Iseri M, Keskin G, Müezzinoğlu B. Central giant cell granuloma. Int J Pediatr Otorhinolaryngol. 2002;65:143-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Unal M, Karabacak T, Vayisoğlu Y, Bağiş HE, Pata YS, Akbaş Y. Central giant cell reparative granuloma of the mandible caused by a molar tooth extraction: special reference to the maneuver of drilling the surgical field. Int J Pediatr Otorhinolaryngol. 2006;70:745-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Donoff RB, Rosenberg AE. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 20-1993. A 23-year-old woman with a rapidly enlarging intraoral mass after a tooth extraction. N Engl J Med. 1993;328:1478-1483. [PubMed] |
| 11. | Chuong R, Kaban LB, Kozakewich H, Perez-Atayde A. Central giant cell lesions of the jaws: a clinicopathologic study. J Oral Maxillofac Surg. 1986;44:708-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 295] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 12. | Bataineh AB, Al-Khateeb T, Rawashdeh MA. The surgical treatment of central giant cell granuloma of the mandible. J Oral Maxillofac Surg. 2002;60:756-761. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 82] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Ahuja P, Rathore AS, Chhina S, Manchanda A. Aggressive central giant cell granuloma mimicking giant cell tumor. IJCRI. 2011;2:5-10. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 14. | Shetty DC, Aadithya B, Rai HC, Singh A, Kumar A and Manchanda A. Multiple soft tissue recurrences in a case of central giant cell granuloma – true tumor‘ behavior? Clinical Reviews and Opinions. 2011;3:1-5 Available from: http: //www.academicjournals.org/article/article1379666096_Shetty et al.pdf. |
| 15. | Jose WN, Edson M, Renato KS, Klaus L. Irion, Felipe BC. Radiological and epidemiologicalaspects of central giant cell granuloma. Radiol Bras. 2007;40:167–171. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 16. | Stavropoulos F, Katz J. Central giant cell granulomas: a systematic review of the radiographic characteristics with the addition of 20 new cases. Dentomaxillofac Radiol. 2002;31:213-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 52] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | De Lange J, Van den Akker HP. Clinical and radiological features of central giant-cell lesions of the jaw. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:464-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 121] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 18. | Shetty K, Giannini P and Leigh J. A hybrid giant cell granuloma and fibro-osseous lesion of the mandible. Oral Oncology Extra. 2004;40:81-84. [DOI] [Full Text] |
| 19. | Farzaneh AH, Pardis PM. Central giant cell granuloma and fibrous dysplasia occurring in the same jaw. Med Oral Patol Oral Cir Bucal. 2005;10 Suppl 2:E130-E132. [PubMed] |
| 20. | Mohanty S, Jhamb A. Central giant cell lesion of mandible managed by intralesional triamcinolone injections. A report of two cases and literature review. Med Oral Patol Oral Cir Bucal. 2009;14:E98-102. [PubMed] |
| 21. | Cawson RA, Odell EW. Cawson‘s Essentials of Oral Medicine and Pathology. 7th ed.. 2002;135-136. |
| 22. | Infante Cossío P, Martínez de Fuentes R, Carranza Carranza A, Torres Lagares D, Gutiérrez Pérez JL. Recurrent central giant cell granuloma in the mandible: surgical treatment and dental implant restoration. Med Oral Patol Oral Cir Bucal. 2007;12:E229-E232. [PubMed] |
| 23. | Rajeevan NS, Soumithran CS. Intralesional corticosteroid injection for central giant cell granuloma. A case report. Int J Oral Maxillofac Surg. 1998;27:303-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 24. | Sezer B, Koyuncu B, Gomel M, Günbay T. Intralesional corticosteroid injection for central giant cell granuloma: a case report and review of the literature. Turk J Pediatr. 2005;47:75-81. [PubMed] |
| 25. | Pogrel MA. Calcitonin therapy for central giant cell granuloma. J Oral Maxillofac Surg. 2003;61:649-653; discussion 53-54. [PubMed] |
| 26. | Nalan Y, Bilgehan Y, Taner Y, Canan A, Kader K, Arzu S, Munevver B, kpamukc U. Surgeryand calcitonin therapy in childhood central giant cell granuloma. Int J of PediatricOtorhinolaryngol Extra. 2006;1:297-303. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |