Published online Jun 18, 2025. doi: 10.5318/wjo.v9.i1.105857
Revised: April 1, 2025
Accepted: May 18, 2025
Published online: June 18, 2025
Processing time: 129 Days and 13.9 Hours
Pediatric cataract is a public health concern, and it causes long-term functional impairment and impacts the quality of life of the child with cataract. Visual impairment in children due to cataract has devastating consequences on their health, social life, and academic performance and places a socio-economic burden on the child’s family and society as a whole. Globally, pediatric cataract is a significant contributor to ocular morbidity and blindness. Findings from this study will help quantify the visual benefits of pediatric cataract surgical inter
To evaluate the visual acuity outcomes of children after cataract surgery.
The study employed a retrospective electronic review of pediatric cataract surgeries from January 2019 to July 2021 at the pediatric unit of the eye depart
163 children (257 eyes) underwent cataract surgery at KATH. The overall mean age was 3.81 ± 3.56 years. Congenital cataract was commonly observed (56.4%). All children underwent keratometry and phacoemulsification procedures. A few children (9.8%) experienced postoperative complications while 90.8% did not require further intervention after the surgery. After the surgery 27.0% of the children had refraction and the majority were corrected for myopia and near addition (12.9%). An analysis of the association of postoperative visual acuity and the type of cataract was statistically significant (P value < 0.05). There was a significant improvement in the visual outcomes following cataract surgery.
Timely pediatric cataract surgery improves postoperative visual outcomes. Creating awareness and implementing screening programs is important to ensure that the prevalence of childhood blindness is reduced to the barest minimum.
Core Tip: This study examines visual outcomes after pediatric cataract surgery at Komfo Anokye Teaching Hospital in Ghana, revealing significant insights into post-operative recovery. Our findings indicate a substantial improvement in visual acuity among children, with early intervention and tailored rehabilitation playing critical roles. Additionally, we identified key factors influencing visual outcomes, such as age at surgery, type of cataract, the cause and duration of cataract, complications after the surgery, follow-up visits and adherence to post-operative care. This study highlights the importance of creating awareness and implementing screening programs to reduce the prevalence of childhood cataract.
- Citation: Amematekpor LD, Amankwaa-Frempong D, Owusu E. Visual outcomes following pediatric cataract surgery at Komfo Anokye Teaching Hospital in Ghana. World J Ophthalmol 2025; 9(1): 105857
- URL: https://www.wjgnet.com/2218-6239/full/v9/i1/105857.htm
- DOI: https://dx.doi.org/10.5318/wjo.v9.i1.105857
Pediatric cataract is a public health concern, not only because it is relatively common, but also due to its potentially profound lifelong impacts on visual health, and the quality of life of the child[1]. The causes of cataract formation are complex and could result from several factors that influence the metabolism of the crystalline lens. Cataract occurs when there is a loss of transparency in the crystalline lens located in the eye[2]. Risk factors associated with cataract in children include heredity, certain systemic diseases, dysfunctional body metabolism, diet, medications and trauma[2,3]. Untreated cataract causes visual and functional impairment, blindness and a significant decline in a child’s quality of life. Visual impairment in children undoubtedly has negative effects on their academic performance, social life and future job prospects[1,4]. Hansen et al[5] and Wang et al[6] also corroborate that the socioeconomic burden of the families is wor
Pediatric cataract is a major cause of ocular morbidity and blindness in both developed and developing countries. The World Health Organization (2019) declared pediatric cataract the leading cause of addressable blindness in young children in many low-income countries. Approximately 200000 children are blind due to cataract, among which an estimated 10%-20% are born with the condition[7]. Ilechie et al[8] studied congenital eye anomalies in a pediatric clinic in Ghana and found that cataract had the highest prevalence, present in 16.8% of children. The standard treatment for cataract is surgery[9]. Over the years, advancement in surgical procedures has led to many successful visual outcomes[10]. Although vision can be restored by surgical intervention, visual outcomes following cataract surgery vary depending on several reasons: The cause and duration of cataract, complications after the surgery, follow-up visits and adherence to post-operative care[11,12]. Therefore, Self et al[13] state that the success of pediatric cataract surgery depends on both the surgeon and the child’s parents.
Unlike in high-income countries, where early diagnosis and timely surgical intervention are the norm, many children in Ghana[14] and similar low and middle-income countries (LMICs) such as Nigeria[15], Zambia[16], Madagascar[17], Democratic Republic of the Congo[18], Ethiopia[4], amongst others experience delays in diagnosis and treatment. These delays stem from multiple factors, including limited awareness among parents, late detection, lack of trained pediatric ophthalmologists, lack of healthcare infrastructure and financial constraints. Studies conducted in these LICs have shown comparably low attendance to follow-up visits and access to post-surgical visual rehabilitation, including spectacle correction and low vision services, which remain significant concerns[15-17].
In Ghana, the prevalence of childhood cataract is not well-documented at the national level, but studies conducted suggest that it is one of the leading causes of pediatric visual impairment[8,19]. There are 16 regions in Ghana, namely Greater Accra, Northern, Upper East, Upper West, Ashanti, Oti, Volta, Bono East, Ahafo, Northern East, Savannah, Western North, Western, Eastern, Central and Bono Region[20]. There are only four trained pediatric ophthalmologists in Ghana; three at Korle Bu Teaching Hospital in the Greater Accra Region and one at Komfo Anokye Teaching Hospital (KATH) in the Ashanti Region[21,22]. KATH, as a tertiary referral hospital, manages a large number of pediatric cataract cases from across the country, especially Northern, Upper East, Upper West, Oti, Bono East, Ahafo, Northern East, Savannah, Western North, Western, Eastern, Central, Bono and parts of the Volta Region[22].
There is a critical need for an evaluation of pediatric cataract surgeries to help assess the visual benefits of pediatric cataract surgical interventions and to identify opportunities for improving pediatric cataract services. This will help combat pediatric visual impairment and blindness in Ghana.
The study employed a hospital-based retrospective case study design.
KATH is one of a few tertiary hospitals in Ghana, located in Kumasi, the regional capital of the Ashanti region, the second most populous in the country. The eye centre is a modern 27000 square - foot well-equipped facility and receives referrals from all hospitals in the Ashanti Region and about seven other neighbouring regions. The pediatric unit of the eye department at KATH is the only hospital unit with a pediatric ophthalmologist in the upper part of Ghana.
This hospital-based retrospective study was conducted using the patient clinical records from the pediatric eye unit of KATH, Ghana, from January 2019 to July 2021. The medical records of pediatric patients who underwent cataract surgery within this timeframe were retrieved from the hospital’s electronic medical record system and paper-based surgical logs.
Inclusion criteria comprised pediatric patients aged 15 years and below who underwent cataract surgery and had documented postoperative follow-up. Exclusion criteria included patients with incomplete medical records.
The key data variables collected included demographic information, clinical presentation of cataract, laterality of cataract, pre-operative visual acuity, post-operative visual acuity, surgical procedure performed, postoperative complications, postoperative complication interventions and refraction.
To ensure accuracy, extracted data were cross-checked by a second reviewer to minimize transcription errors and ensure consistency. In cases where missing data points were identified, efforts were made to retrieve the missing information from related records, outpatient follow-up notes or surgical team documentation. If data remained incomplete after these efforts, the records were excluded. Any discrepancies were resolved through verification with the original patient records to confirm reliability.
The data was entered into a Microsoft Excel spreadsheet for organization and cleaning, then exported into statistical package and service solution (SPSS) (IBM SPSS Inc., Chicago, Illinois, United States) version 25. Descriptive statistics were used to determine frequencies and percentages of demographic characteristics. Pearson's χ2 test of independence was used to assess the association between various variables. P values below 0.05 were deemed statistically significant.
163 children underwent cataract surgery at KATH within the study period. The majority (58.1%, n = 96) were males. The mean age of all the children was 3.81 ± 3.56 years, ranging from 3 months to 14 years. In total, 257 eyes of the 163 children were operated on from January 1, 2019 to July 31, 2021. In 2019, 53 eyes were operated on, while 83 and 121 eyes were operated on in 2020 and 2021 respectively (Table 1).
| Affected eye | Year of surgery | Total | ||
| 2019 | 2020 | 2021 | ||
| Both eyes | 36 (19.1) | 64 (34.0) | 88 (46.8) | 188 (100.0) |
| Left eyes | 8 (27.6) | 7 (24.1) | 14 (48.3) | 29 (100.0) |
| Right eye | 9 (22.5) | 12 (23.5) | 19 (24.7) | 40 (100.0) |
| Total | 53 (21.5) | 83 (31.5) | 121 (47.2) | 257 (100.0) |
The records of 163 children who underwent cataract surgery were used in this study. The majority, 58.1% of the children were males and this is similar to findings in other published studies in Africa[18,15]. In African culture, male children are often given higher priority in healthcare, leading to more frequent hospital visits when they are unwell. Furthermore, male children tend to be more active than female children and are thus more prone to trauma[23]. In terms of age distribution, the minimum and maximum ages of children who had cataract surgery were 3 months and 14 years respectively. The majority of children were aged 2 to 10 years, constituting 52.8%. The mean age of presentation of cataract was 3.81 ± 3.56 years, this is suggestive of early presentation of cataract among the children. The possible reasons for the early presentation of the condition may be attributable to increased awareness among mothers, early detection of the condition and proximity of health facilities. An association between the age distribution and the final postoperative visual acuity was not found in the right eyes while found in the left eyes operated (Table 2).
| Visual impairment categories | ||||
| Variables | P value | |||
| Right eye | Left eye | |||
| Pre-op VA unaided | Post-op VA aided, 1 year | Pre-op VA unaided | Post-op VA aided, 1 year | |
| Gender | 0.413 | 0.253 | 0.468 | 0.07 |
| Age | 0.00 | 0.213 | 0.00 | 0.00 |
| Type of cataract | 0.00 | 0.001 | 0.00 | 0.00 |
| State of cataract (morphology) | 0.00 | 0.04 | 0.46 | 0.00 |
| Postoperative complications | 0.00 | 0.03 | 0.00 | 0.77 |
| Postoperative complication intervention | 0.00 | 0.25 | 0.001 | 0.98 |
| Refraction (corrected) | 0.00 | 0.00 | 0.00 | 0.00 |
We also found congenital cataract to be the most commonly observed in 92 children (56.4%), followed by developmental cataract in 31 children (19.0%), traumatic cataract in 26 children (16.0%) and 14 cases (8.6%) were not specified. Most children presented with congenital cataract, likely because bilateral cases have a rapid onset, leading to more profound visual impairment[17] (Table 3).
| Variable | Total | Females | Males |
| N = 163 (100%) | N = 67 (41.1%) | N = 96 (58.1%) | |
| Age group (years) | |||
| < 2 | 62 (38.0) | 23 (34.3) | 39 (40.6) |
| 2 ≤ 10 | 86 (52.8) | 31 (46.3) | 50 (52.0) |
| 10-15 | 15 (9.20) | 13 (19.4) | 7 (7.3) |
| Year of surgery | |||
| 2019 | 35 (21.5) | 14 (20.9) | 21 (21.9) |
| 2020 | 51 (31.3) | 21 (31.3) | 30 (31.3) |
| 2021 | 77 (47.2) | 32 (47.8) | 45 (46.9) |
| Type of cataract | |||
| Congenital | 92 (56.4) | 30 (44.8) | 62 (64.6) |
| Developmental | 31 (19.0) | 17 (25.4) | 14 (14.6) |
| Traumatic | 26 (16.0) | 13 (19.4) | 13 (13.5) |
| Not specified | 14 (8.6) | 7 (10.4) | 7 (7.3) |
| State of cataract (morphology) | |||
| Cortical | 3 (1.8) | 2 (3.0) | 1 (1.0) |
| Dense | 14 (8.6) | 6 (9.0) | 8 (8.3) |
| Nuclear | 2 (1.2) | 1 (1.5) | 1 (1.0) |
| Polar | 2 (1.2) | 0 (0.0) | 2 (2.1) |
| Not specified | 142 (87.1) | 58 (86.6) | 84 (87.5) |
| Laterality | |||
| Bilateral | 94 (57.7) | 35 (52.2) | 59 (61.5) |
| Unilateral | 69 (42.3) | 32 (47.8) | 37 (38.5) |
| Affected eye | |||
| Both eyes | 94 (57.7) | 35 (52.2) | 59 (61.5) |
| Left eye | 29 (17.8) | 13 (19.4) | 16 (16.7) |
| Right eye | 40 (24.5) | 19 (28.4) | 21 (21.9) |
| Presenting ocular co-morbidity | |||
| Yes | 14 (8.60) | 5 (7.5) | 9 (9.4) |
| No | 149 (91.4) | 62 (92.5) | 87 (90.6) |
| Strabismus | |||
| Right eye | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Left eye | 1 (0.6) | 0 (0.0) | 1 (1.0) |
| Both eyes | 1 (0.6) | 1 (1.5) | 0 (0.0) |
| Nystagmus | |||
| Right eye | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Left eye | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Both eyes | 7 (4.3) | 2 (3.0) | 5 (5.2) |
| Glaucoma | |||
| Right eye | 1 (0.6) | 1 (1.5) | 0 (0.0) |
| Left eye | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Both eyes | 2 (1.2) | 1 (1.5) | 1 (1.0) |
| Corneal opacity | |||
| Right eye | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Left eye | 1 (0.6) | 0 (0.0) | 1 (1.0) |
| Both eyes | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Leukocoria | |||
| Right eye | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Left eye | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Both eyes | 1 (0.6) | 1 (1.0) | 0 (0.0) |
| Keratometry | |||
| Yes | 163 (100.0) | 67 (41.1) | 96 (58.9) |
| No | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Type of surgical procedure | |||
| Small incision | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Phacoemulsification | 163 (100.0) | 67 (41.1) | 96 (58.9) |
| IOL inserted | 163 (100.0) | 67 (41.1) | 96 (58.9) |
| Postoperative surgical results | |||
| Postoperative complications | |||
| Yes | 16 (9.8) | 7 (10.4) | 9 (9.4) |
| No | 147 (90.2) | 60 (89.6) | 87 (90.6) |
| Glaucoma | |||
| Right eye | 1 (0.6) | 0 (0.0) | 1 (0.6) |
| Left eye | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Both eyes | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Decentered IOL | |||
| Right eye | 3 (1.8) | 1 (1.5) | 2 (2.1) |
| Left eye | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| Both eyes | 2 (1.2) | 0 (0.0) | 2 (3.0) |
| Posterior capsular opacification | |||
| Right eye | 5 (3.1) | 3 (4.5) | 2 (2.1) |
| Left eye | 1 (0.6) | 1 (1.5) | 0 (0.0) |
| Both eyes | 4 (2.5) | 1 (1.5) | 3 (3.3) |
| Postoperative complication intervention | |||
| Centering IOL | 4 (2.5) | 2 (3.0) | 2 (2.1) |
| Centering IOL and YAG laser | 2 (1.2) | 1 (1.5) | 1 (1.0) |
| No intervention needed | 148 (90.8) | 60 (89.6) | 88 (91.7) |
| Patching | 1 (0.6) | 1 (1.5) | 0 (0.0) |
| YAG laser | 8 (4.9) | 3 (4.5) | 5 (5.2) |
| Refraction | |||
| Yes | 44 (27.0) | 17 (25.5) | 27 (28.1) |
| No | 119 (73.0) | 50 (74.6) | 69 (71.9) |
| Refraction (corrected) | |||
| Myopia, add | 21 (12.9) | 11 (16.4) | 10 (10.4) |
| Mixed (Myopia & Astigmatism) | 3 (1.8) | 3 (3.1) | 0 (0.0) |
| Mixed (Myopia & Astigmatism), add | 3 (1.8) | 2 (3.0) | 1 (1.0) |
| Myopia | 17 (10.4) | 4 (6.0) | 13 (13.5) |
For congenital cataract, it is presented at birth due to genetic mutation resulting in the disruption of the microarchitecture of the crystalline lens[24]. Developmental cataract occurs during the developmental stages in children due to trauma, systemic conditions and acquired infections[2]. Günaydın et al[25] explain that a traumatic cataract occurs when there is a blunt or penetrating injury to the eye.
An analysis of the association of postoperative visual acuity and the type of cataract showed that the postoperative visual outcomes and the presented cataract were statistically significant. Owing to the fact that the duration of cataract and the timing of the surgery can affect the postoperative visual outcomes among children. The optimal time for cataract surgery in children is critical to prevent further complications. Some schools of thought have established that children with unilateral cataract should have cataract surgery six weeks after birth to achieve good visual outcomes[26]. For surgeries performed after four weeks, there is a high likelihood of the prevalence of strabismus and nystagmus[27]. On the contrary, Zhang et al[28] indicated that cataract surgery performed during the four weeks could lead to complications like glaucoma and secondary membrane formation. Nevertheless, for bilateral cataract, early cataract surgery is reco
We noticed no postoperative complications in 147 children (90.2%) after cataract surgery while 16 children (9.8%) had postoperative complications, and the necessary interventions were given. A postoperative complication rate of 9.8% means 9 out of 100 children after cataract surgery will have complications, which is a good rate outcome. All eyes operated on in this study were done using phacoemulsification and intraocular lens (IOL) implants. Our surgical technique was the ultimate since studies have shown phacoemulsification leads to good visual outcomes[26] and our postoperative complicate rate (9.8%) is proof. In addition, the implantation of an IOL during cataract surgery helps with visual rehabilitation and results in better visual outcomes than the eyes left aphakic to be corrected with spectacles[30].
The assessment of vision in infants and children can be quite challenging since they are normally uncooperative and unaware of their surroundings. The categorisation of vision in children is quite different from adults due to the methods and type of charts used. Our study focused on the visual outcomes following pediatric cataract surgery. There is a critical need for an evaluation of visual outcomes to help quantify the visual benefits after pediatric cataract surgical intervention. We used the World Health Organization (WHO) classification of vision impairment based on visual acuity to quantify visual outcomes following the cataract surgery[31].
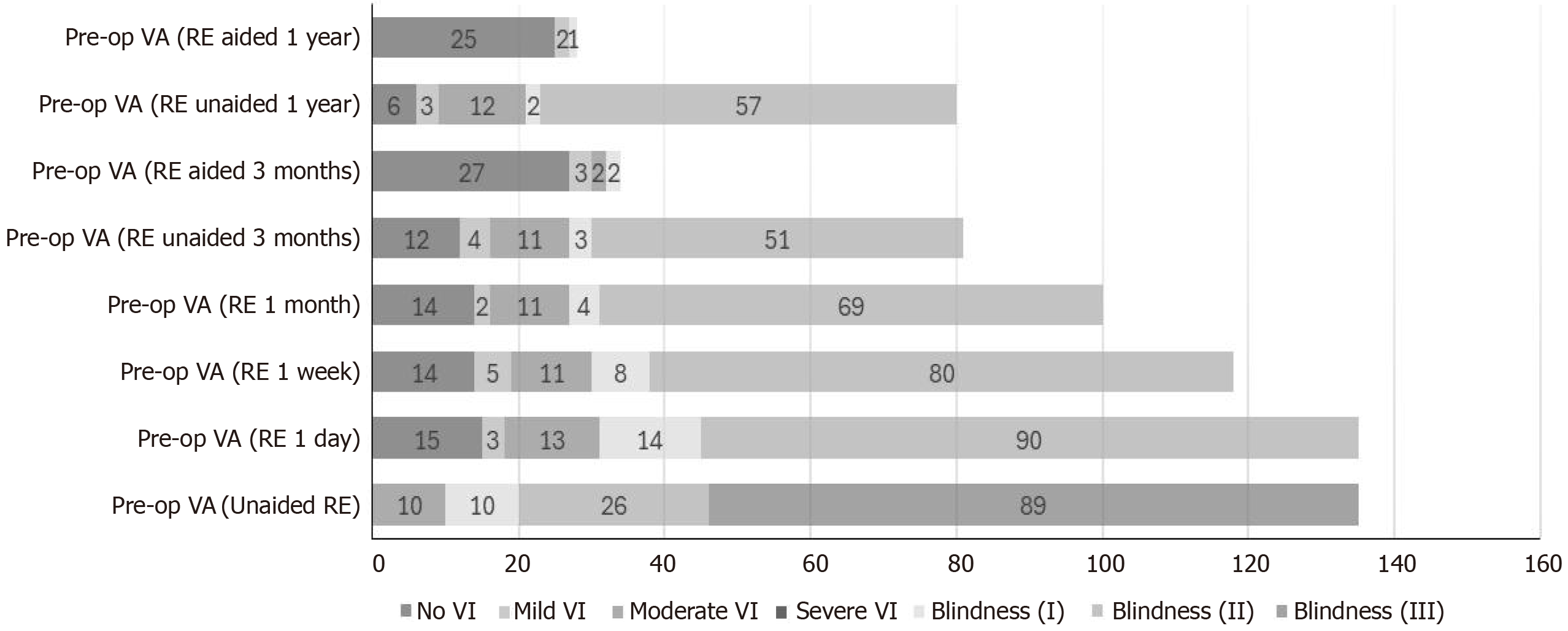
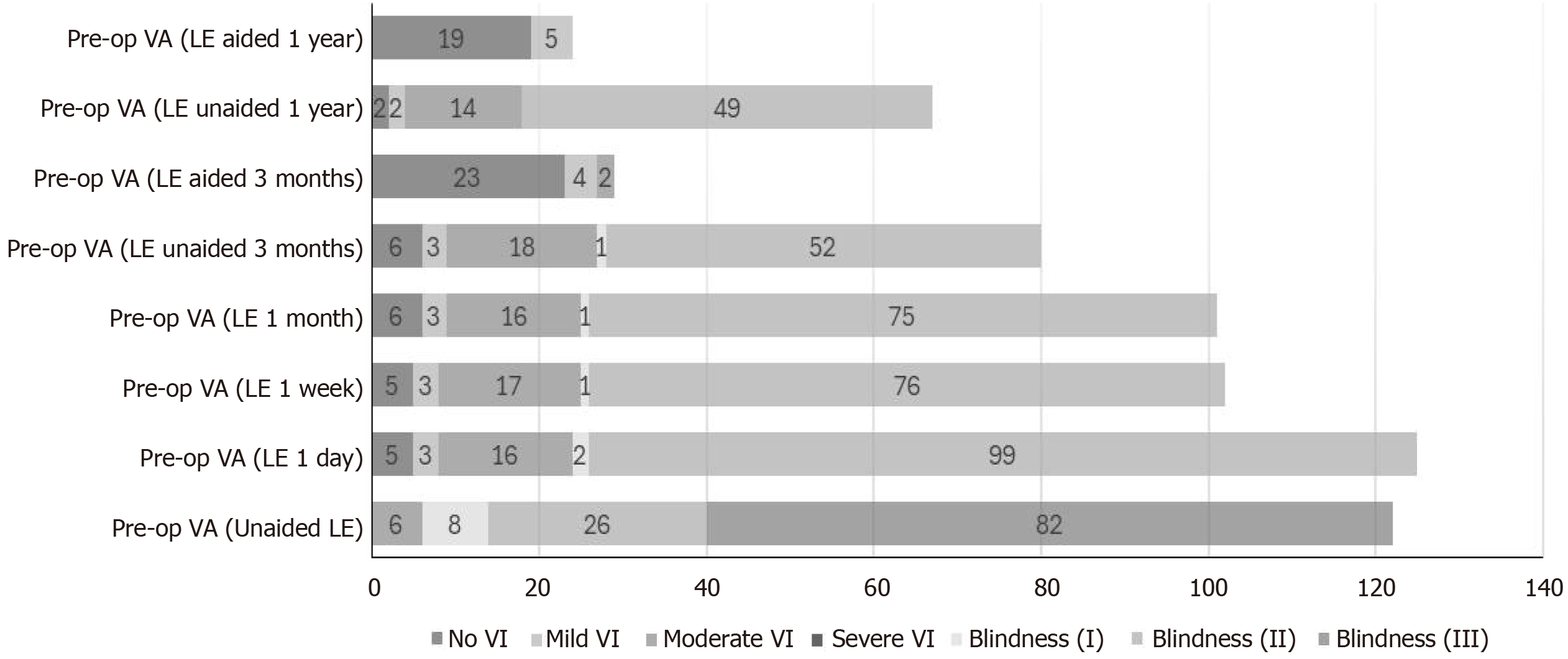
According to WHO, blindness is a visual acuity of less than 3/60 with the best correction and low vision is a visual acuity less than 6/18 but equal to or better than 3/60 with best correction. Furthermore, the Organization classified visual impairment based on visual acuity into No visual impairment (visual acuity > 6/12), Mild visual impairment (visual acuity > 6/12 - 6/18), Moderate visual impairment (visual acuity < 6/18 - 6/60), Severe visual impairment (visual acuity < 6/60 - 3/60), Blindness I (visual acuity < 3/60 - 1/60), Blindness II (Visual acuity < 1/60) and Blindness III (no perception of light). From the above definitions of the WHO, we will compare the unaided pre-operative and aided postoperative visual acuity to evaluate the visual outcomes (Table 4).
| Visual impairment category | Visual acuity worse equal to than or better | Right eye, pre VA unaided | Post VA aided 1 year | P value | Left eye, pre VA unaided | Post VA aided 1 year | P value |
| No VI | 6/12 | 0 (0.0) | 25 (15.2) | 0.00 | 0 (0.0) | 19 (11.6) | 0.00 |
| Mild VI | 6/12; 6/18 | 0 (0.0) | 2 (1.2) | 0.00 | 0 (0.0) | 5 (3.0) | 0.00 |
| Moderate VI | 6/18; 6/60 | 10 (6.1) | 0 (0.0) | 0.00 | 6 (3.7) | 0 (0.0) | 0.00 |
| Severe VI | 6/60; 3/60 | 0 (0.0) | 0 (0.0) | 0.00 | 0 (0.0) | 0 (0.0) | 0.00 |
| Blindness (I) | 3/60; 1/60 | 10 (6.1) | 0 (0.0) | 0.00 | 8 (4.9) | 0 (0.0) | 0.00 |
| Blindness (I) | PL; CF | ||||||
| Blindness (II) | 1/60; PL | 26 (15.9) | 0 (0.0) | 0.00 | 26 (15.9) | 0 (0.0) | 0.00 |
| Blindness (III) | NPL; NFO | 89 (54.6) | 0 (0.0) | 0.00 | 82 (50.0) | 0 (0.0) | 0.00 |
Figures 1 and 2 show the pattern of the pre-operative and post-operative visual acuity of the operated right eye and left eye respectively. 135 children had cataract extracted from their right eye. The post-operative visual acuity unaided recorded was as follows 89 children were in Blindness III (no perception of light), 26 children in Blindness II (Visual acuity < 1/60), 10 eyes in Blindness I (visual acuity < 3/60 - 1/60) and 10 children in Moderate visual impairment (visual acuity < 6/18 - 6/60) whiles Post-operative aided visual acuity had 1 child in Blindness I (visual acuity < 3/60 - 1/60), 2 children in Mild visual impairment (visual acuity > 6/12 - 6/18) and 25 children in No visual impairment (visual acuity > 6/12). For the left eye, 122 children had cataract extracted. Their postoperative visual acuity unaided had 82 children in Blindness III (no perception of light), 26 children in Blindness II (Visual acuity < 1/60), 8 children in Blindness I (visual acuity < 3/60 - 1/60) and 6 children in Moderate visual impairment (visual acuity < 6/18 - 6/60). Aided post-operative visual acuity included 19 children with No visual impairment (visual acuity > 6/12) and 5 children with Mild visual impairment (visual acuity > 6/12 - 6/18). There was a significant improvement in the visual outcomes following cataract surgery. We could attribute this to the low rate of postoperative complications following the cataract surgery, phacoemulsification surgical intervention with IOL implants and refraction conducted in this study (Table 5).
| Variables | Multivariate regression | P value | ||
| B | SE | 95%CI | ||
| Postoperative VA RE unaided (1 year) | ||||
| Age | 0.30 | 0.028 | -0.024 to 0.085 | 0.275 |
| Gender | -0.807 | 0.341 | -1.482 to -0.133 | 0.019 |
| Type of cataract | 0.383 | 0.162 | 0.063 to 0.703 | 0.019 |
| State of cataract (morphology) | -0.302 | 0.365 | -1.022 to -0.418 | 0.409 |
| Presenting ocular comorbidity | -0.544 | 0.607 | -1.743 to 0.655 | 0.371 |
| Postoperative complications | 0.314 | 0.584 | -0.839 to 1.467 | 0.591 |
| Postoperative complication intervention | 0.377 | 0.426 | -0.464 to 1.218 | 0.377 |
| Refraction (corrected) | 0.597 | 0.398 | -0.189 to 1.383 | 0.136 |
| Postoperative VA LE unaided (1 year) | ||||
| Age | 0.050 | 0.028 | -0.006 to 0.105 | 0.078 |
| Gender | -1.162 | 0.344 | -1.841 to -0.484 | < 0.001 |
| Type of cataract | 0.325 | 0.163 | 0.002 to 0.647 | 0.048 |
| State of cataract (morphology) | -0.017 | 0.367 | -0.741 to 0.708 | 0.963 |
| Presenting ocular comorbidity | -1.172 | 0.611 | -2.378 to 0.034 | 0.057 |
| Postoperative complications | 0.583 | 0.587 | -0.577 to 1.743 | 0.322 |
| Postoperative complication intervention | -0.012 | 0429 | -0.859 to 0.834 | 0.977 |
| Refraction (corrected) | -1.316 | 0.400 | -2.107 to -0.525 | 0.001 |
| Postoperative VA RE aided (1 year) | ||||
| Age | 0.006 | 0.005 | -0.005 to 0.016 | 0.298 |
| Gender | -0.045 | 0.066 | -0.176 to 0.086 | 0.499 |
| Type of cataract | -0.014 | 0.032 | -0.076 to 0.048 | 0.6659 |
| State of cataract (morphology) | -0.123 | 0.071 | -0.263 to 0.017 | 0.086 |
| Presenting ocular comorbidity | -0.073 | 0.118 | -0.306 to 0.161 | 0.539 |
| Postoperative complications | 0.093 | 0.114 | -0.132 to 0.317 | 0.416 |
| Postoperative complication intervention | 0.128 | 0.083 | -0.036 to 0.292 | 0.125 |
| Refraction (corrected) | -0.680 | 0.077 | -0.833 to -0.527 | < 0.001 |
| Postoperative VA LE aided (1 year) | ||||
| Age | 0.002 | 0.005 | -0.008 to 0.013 | 0.666 |
| Gender | -0.150 | 0.065 | -0.279 to -0.021 | 0.023 |
| Type of cataract | -0.013 | 0.031 | -0.074 to 0.048 | 0.678 |
| State of cataract (morphology) | -0.220 | 0.070 | -0.357 to -0.082 | 0.002 |
| Presenting ocular comorbidity | -0.111 | 0.116 | -0.340 to 0.118 | 0.339 |
| Postoperative complications | 0.181 | 0.112 | -0.039 to 0.401 | 0.107 |
| Postoperative complication intervention | 0.00 | 0.081 | -0.161 to 0.161 | 0.997 |
| Refraction (corrected) | -0.545 | 0.076 | -0.696 to 0.395 | < 0.001 |
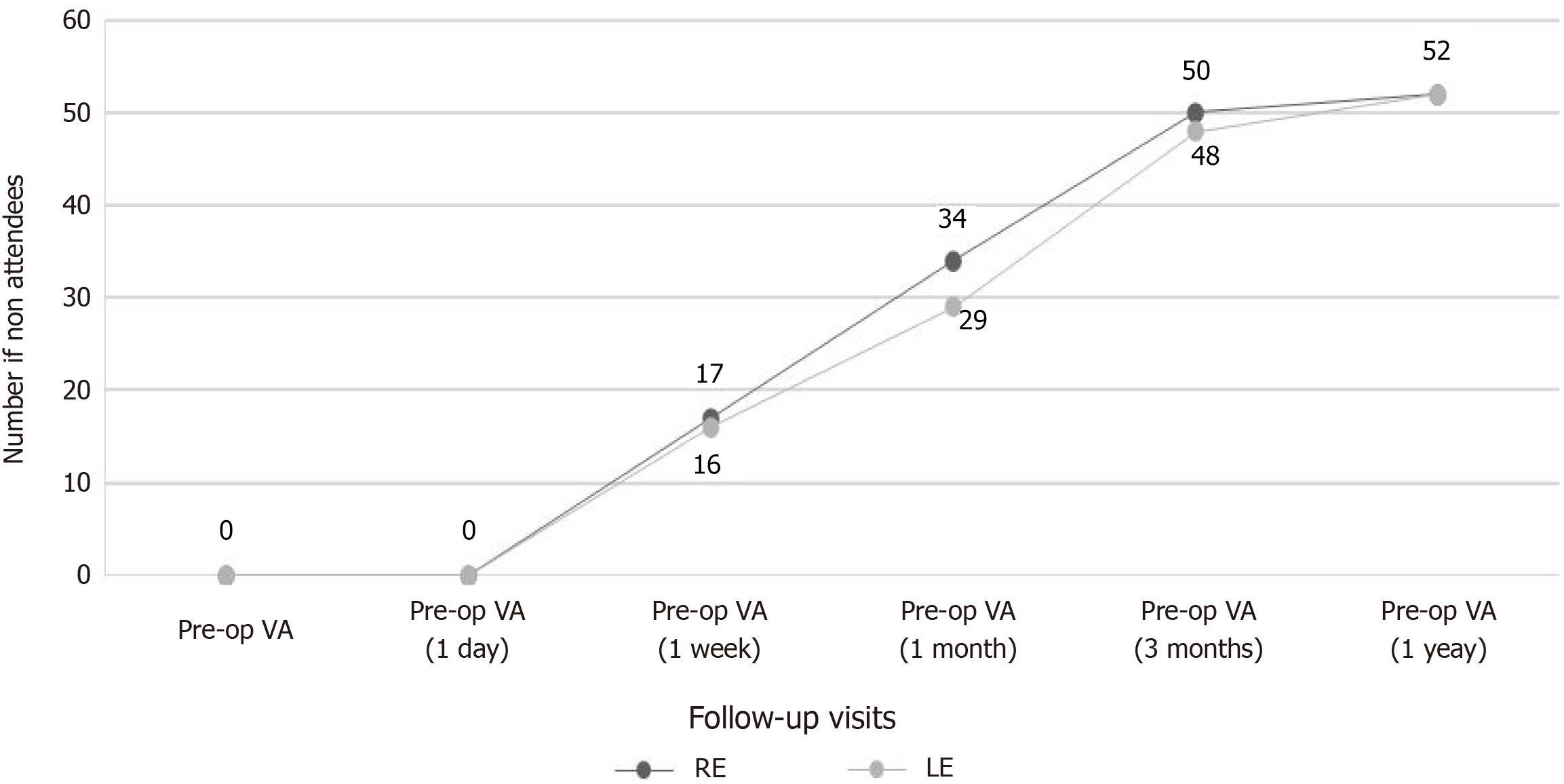
Observing the visual outcome pattern in Figure 3 shows a reduction in the follow-up rate post-operatively. Although vision can be restored by surgical intervention, visual outcomes following cataract surgery vary depending on several reasons. However, follow-up visits and adherence to post-operative care play a major role. The coronavirus disease 2019 (COVID-19) pandemic and post-pandemic consequences affected follow-up visits in our study. Generally, findings widely reported by studies revealed that financial constraints, lack of awareness of follow-up visits, lack of eyecare facilities, poor roads, and long distances to eyecare facilities were barriers resulting in poor follow-up visits[14,15,17]. Despite COVID-19 playing a major role in the reduction of follow-up visits, attention needs to be paid to how to encourage follow-up visits which will improve visual outcomes in children.
Our findings underscore the critical importance of early screening programs which facilitate the timely identification of congenital and developmental cataracts. Integrating vision screening into routine child health services, including neonatal and preschool check-ups, could aid in early detection. Postoperative care remains a challenge, with significant pro
From a policy-making perspective, pediatric eye care should be integrated into national health strategies to ensure sustainability and accessibility. Expanding specialized pediatric ophthalmology services across regional hospitals and incorporating pediatric cataract surgery into Ghana’s National Health Insurance Scheme could alleviate the financial burden on families and improve surgical uptake. Public awareness campaigns targeting parents, caregivers, and educators can further enhance early recognition and timely referral of affected children.
Our findings highlight the urgent need for targeted interventions to improve visual outcomes following pediatric cataract surgery in Ghana and other LMICs facing similar healthcare challenges.
Timely pediatric cataract surgery significantly improves postoperative visual outcomes. This study suggested that parents of three-quarters of children did not visit the hospital early enough and follow-up rates were poor. Based on the findings, it can be inferred that there will be a backlog of cases across the country.
Below are some recommendations: (1) The quality of life of children who have undergone cataract extraction in Ghana needs to be investigated; (2) Training more pediatric ophthalmologists since they are understaffed in Ghana as well as community health workers on recognizing pediatric cataracts for timely referrals; and (3) The Ministry of Health in partnership with the Ministry of Education should strengthen primary eye care services, by integrating pediatric eye screening into routine child health services, and school-based and community vision screening programs to detect cataracts earlier.
This study suggests that the Government should incorporate pediatric cataract surgery into Ghana's National Health Insurance Scheme to alleviate the financial burden on families and improve surgical uptake.
We extend our profound gratitude to Mr. Francis Essieh (Head, Eye Centre Biostatistics Unit), the authorities at KATH and the Head, Eye, Ear, Nose and Throat Directorate, for their support throughout the project.
| 1. | Chadha RK, Subramanian A. The effect of visual impairment on quality of life of children aged 3-16 years. Br J Ophthalmol. 2011;95:642-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 83] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 2. | Khokhar SK, Pillay G, Dhull C, Agarwal E, Mahabir M, Aggarwal P. Pediatric cataract. Indian J Ophthalmol. 2017;65:1340-1349. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 64] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 3. | Reis LM, Semina EV. Genetic landscape of isolated pediatric cataracts: extreme heterogeneity and variable inheritance patterns within genes. Hum Genet. 2019;138:847-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 35] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 4. | Tomkins O, Ben-Zion I, Moore DB, Helveston EE. Outcomes of pediatric cataract surgery at a tertiary care center in rural southern Ethiopia. Arch Ophthalmol. 2011;129:1293-1297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Hansen MM, Bach-Holm D, Kessel L. Visual outcomes after surgery for childhood cataracts. Acta Ophthalmol. 2020;98:579-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Wang W, Yan W, Fotis K, Prasad NM, Lansingh VC, Taylor HR, Finger RP, Facciolo D, He M. Cataract Surgical Rate and Socioeconomics: A Global Study. Invest Ophthalmol Vis Sci. 2016;57:5872-5881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 181] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 7. | World Health Organization. World report on vision. 2019. [January 23, 2025]. Available from: https://www.who.int/docs/default-source/documents/publications/world-vision-report accessible.pdf?sfvrsn=223f9bf7_2. |
| 8. | Ilechie AA, Essuman VA, Enyionam S. Prevalence of congenital eye anomalies in a paediatric clinic in Ghana. East Mediterr Health J. 2014;19 Suppl 3:S76-S80. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Day AC, Gore DM, Bunce C, Evans JR. Laser-assisted cataract surgery versus standard ultrasound phacoemulsification cataract surgery. Cochrane Database Syst Rev. 2016;7:CD010735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 63] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 11. | Chan E, Mahroo OA, Spalton DJ. Complications of cataract surgery. Clin Exp Optom. 2010;93:379-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 102] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 12. | Gollogly HE, Hodge DO, St Sauver JL, Erie JC. Increasing incidence of cataract surgery: population-based study. J Cataract Refract Surg. 2013;39:1383-1389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 153] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 13. | Self JE, Taylor R, Solebo AL, Biswas S, Parulekar M, Dev Borman A, Ashworth J, McClenaghan R, Abbott J, O'Flynn E, Hildebrand D, Lloyd IC. Cataract management in children: a review of the literature and current practice across five large UK centres. Eye (Lond). 2020;34:2197-2218. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 34] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 14. | Ramai D, Elliott R, Goldin S, Pulisetty T. A cross-sectional study of pediatric eye care perceptions in Ghana, Honduras, and India. J Epidemiol Glob Health. 2015;5:133-142. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Umar MM, Abubakar A, Achi I, Alhassan MB, Hassan A. Pediatric cataract surgery in National Eye Centre Kaduna, Nigeria: outcome and challenges. Middle East Afr J Ophthalmol. 2015;22:92-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Mboni C, Gogate PM, Phiri A, Seneadza A, Ramson P, Manolakos-Tsehisi H, Musonda L, Benjamin L, Øverland L. Outcomes of Pediatric Cataract Surgery in the Copperbelt Province of Zambia. J Pediatr Ophthalmol Strabismus. 2016;53:311-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Randrianotahina HC, Nkumbe HE. Pediatric cataract surgery in Madagascar. Niger J Clin Pract. 2014;17:14-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Ngoy JK, Stahnke T, Dinkulu S, Makwanga E, Moanda A, Ngweme G, Mukwanseke E, Kundt G, Thiesen F, Hopkins A, Guthoff RF. Bilateral paediatric cataract surgery - outcomes of 298 children from Kinshasa, the Democratic Republic of the Congo. Afr Health Sci. 2020;20:1817-1827. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Huh GJ, Simon J, Grace Prakalapakorn S. Causes of childhood blindness in Ghana: results from a blind school survey in Upper West Region, Ghana, and review of the literature. Int Ophthalmol. 2018;38:1415-1423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | World Maps. Ghana Maps. 2025. [Cited March 25, 2025]. Available from: https://ontheworldmap.com/ghana/. |
| 21. | Ministry of Health Ghana. Korle Bu Teaching Hospital. 2025. [Cited March 25, 2025]. Available from: https://kbth.gov.gh/departments-centres/eye-centre/. |
| 22. | Ministry of Health Ghana. Komfo Anokye Teaching Hospital. 2025. [Cited March 25, 2025]. Available from: https://www.moh.gov.gh/komfo-anokye-teaching-hospital/. |
| 23. | Jinagal J, Gupta G, Gupta PC, Yangzes S, Singh R, Gupta R, Ram J. Visual outcomes of pediatric traumatic cataracts. Eur J Ophthalmol. 2019;29:23-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 24. | Bremond-Gignac D, Daruich A, Robert MP, Valleix S. Recent developments in the management of congenital cataract. Ann Transl Med. 2020;8:1545. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 25. | Günaydın NT, Oral AYA. Pediatric traumatic cataracts: 10-year experience of a tertiary referral center. BMC Ophthalmol. 2022;22:199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 26. | Mohammadpour M, Shaabani A, Sahraian A, Momenaei B, Tayebi F, Bayat R, Mirshahi R. Updates on managements of pediatric cataract. J Curr Ophthalmol. 2019;31:118-126. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 27. | Kim KH, Ahn K, Chung ES, Chung TY. Clinical outcomes of surgical techniques in congenital cataracts. Korean J Ophthalmol. 2008;22:87-91. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Zhang S, Wang J, Li Y, Liu Y, He L, Xia X. The role of primary intraocular lens implantation in the risk of secondary glaucoma following congenital cataract surgery: A systematic review and meta-analysis. PLoS One. 2019;14:e0214684. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 29. | Birch EE, Cheng C, Stager DR Jr, Weakley DR Jr, Stager DR Sr. The critical period for surgical treatment of dense congenital bilateral cataracts. J AAPOS. 2009;13:67-71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 136] [Cited by in RCA: 111] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 30. | Marcos S, Martinez-Enriquez E, Vinas M, de Castro A, Dorronsoro C, Bang SP, Yoon G, Artal P. Simulating Outcomes of Cataract Surgery: Important Advances in Ophthalmology. Annu Rev Biomed Eng. 2021;23:277-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 31. | World Health Organization. WHO updates fact sheet on Blindness and Visual Impairment. 2018. [Cited February 22, 2025]. Available from: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment. |