Peer-review started: September 16, 2015
First decision: October 27, 2015
Revised: March 16, 2016
Accepted: April 7, 2016
Article in press: April 11, 2016
Published online: May 2, 2016
Processing time: 224 Days and 11.2 Hours
Vitiligo is a common, acquired pigmentary disorder of unknown etiology with great impact on patient’s appearance and quality of life. It presents a therapeutic challenge to many dermatologists. Photochemotherapy using psoralen and ultraviolet A (UVA) therapy, topical and oral immunosuppresants, as well as cosmetic camouflage are also commonly employed with varying clinical efficacy. Phototherapy is a popular treatment option, which includes both of the generalized ultraviolet B (UVB) therapies, broadband UVB and narrowband UVB (NB-UVB). It has been used favorably, both alone as well as in combination with other agents like topical calcineurin inhibitors, vitamin-D analogs. Combination therapies are useful and may provide quicker regimentation and treat vitiligo with an additive mechanism of action than UVB phototherapy. Advances in technology may lead to the continuing use of UVB phototherapy as a treatment for vitiligo through the development of sophisticated devices and delivery systems as well as innovative application methods. These will provide increased therapeutic options for all vitiligo patients, particularly those with refractory disease. In this article, I have reviewed the available data pertaining to efficacy and safety issues for NB-UVB as monotherapy, its comparison with psoralen plus UVA and other modes of phototherapy, combination regimens that have been tried and future prospects of NB-UVB in vitiligo.
Core tip: Vitiligo is a procured depigmentation issue with great effect on patient’s appearance and his satisfaction. Till date, the etiology of vitiligo remains elusive, which makes it difficult to have curative therapies. Narrowband ultraviolet B (UVB) phototherapy is generally utilized and delivers great clinical results. In this manuscript, I review the excursion of narrowband UVB from its prior days of advancement until this time as monotherapy, its comparison with psoralen and ultraviolet A and other modes of phototherapy and in combination with other therapies in the management of vitiligo.
- Citation: Attwa E. Review of narrowband ultraviolet B radiation in vitiligo. World J Dermatol 2016; 5(2): 93-108
- URL: https://www.wjgnet.com/2218-6190/full/v5/i2/93.htm
- DOI: https://dx.doi.org/10.5314/wjd.v5.i2.93
The principal investigation of the use of light in the therapy of dermatologic issue dates from 1400 BC when patients with vitiligo were taken sure concentrates of the plants Psoralea corylifolia in India and Ammi majus linnaeus in Egypt as topical application or ingestion, trailed by introduction to the sun[1]. The genuine enthusiasm for the utilization of ultraviolet (UV) light in the remediation of different cutaneous illnesses began in the nineteenth century when Niels Finsen got the Nobel Prize in 1903 for his helpful outcomes with UV illumination in lupus vulgaris[2].
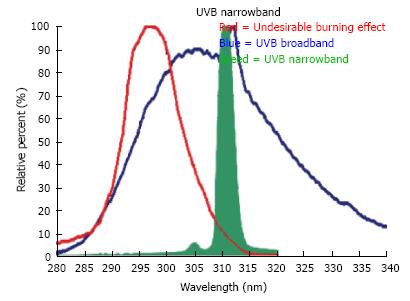
In 1977, Fischer[3] observed that light at a wavelength of 313 nm was viable in clearing psoriatic plaques. Diffey and Farr[4] in the wake of concentrating on the impacts of UV radiation (UVA, UVB and UVC), recommended that more drawn out wavelengths added nothing to the helpful event, that shorter wavelengths really cheapened the adequacy of remediation, and that UVB was practically viable at 311 nm.
A couple of years after the fact it was resolved that the best wavelengths were somewhere around 295 and 313 nm; inside of that range, the proportion of the most reduced viable every day dosage to the negligible erythema measurement was littlest for 313 nm, demonstrating that this wavelength might have the ideal “phototherapy index” for clearing psoriasis[5]. These ponders prompted the advancement of the Phillips TL-01 fluorescent light, which radiates a slender crest around 311-312 nm (Figure 1)[6].
Narrowband UVB (NB-UVB) is a subset of the UVB wideband or broadband range. The UVB band includes the scope of wavelengths between 290 nm and 320 nm while UVB narrowband has a restricted range of emanation (310-315 nm) wavelengths with a crest at 311 nm[7].
NB-UVB phototherapy lodges comprise fluorescent TL-01 (100 W) tubes as the wellspring of light. The expense of a chamber and lights show extensive varieties in the middle of nations and wholesalers. NB-UVB lodges accessible industrially either join TL-01 alone or in blend with UVA tubes. Blend chambers take more time to control a medication measurements. Along these lines, in spite of the fact that they give adaptability, they might speak to an unacceptable tradeoff for a bustling phototherapy unit[8].
Smaller containers of NB-UVB have additionally gotten to be accessible in little range treatment types of gear (hand and foot unit, NB-UVB brush) for the treatment of restricted body sites[9].
NB-UVB calendars can be customized by skin sort and neighborhood experience. Two methods are most generally utilized; one includes definition of the person’s minimum erythema dose (MED) by method for a different bank of TL-01 tubes[10]. Another approach, as commonly practiced is the tight band skin sort convention. It involves standard initial dose according to Fitzpatrick skin phototype (Table 1) with stepwise increments (typically 20%) contingent upon patient’s erythema response. This plan has demonstrated colossally compelling and has been generally circulated and utilized as a part of an expansive choice of phototherapy practices[8].
| Phototype | Sunburn and tanning history (defines the photo type) | Immediate pigment darkening | Delayed tanning | Constitutitve color(unexposed) buttock skin | UVA MED(mJ/cm2) | UVB MED (mJ/cm2) |
| I | Burns easily, never tans | None | None | Ivory White | 20-35 | 15-30 |
| II | Burns easily, tans minimally with difficulty | Weak | Minimal to weak | White | 30-45 | 35-40 |
| III | Burns moderately, tans moderately and uniformly | Definite | Low | White | 40-55 | 30-50 |
| IV | Burns minimally, tans moderately and easily | Moderate | Moderate | Beige-olive, lightly tanned | 50-80 | 40-60 |
| V | Rarely burns, tans profusely | Intense brown | Strong, intense brown | Moderate brown or tanned | 70-100 | 60-90 |
| VI | Never burns, tans profusely | Intense (dark brown) | Strong, intense brown | Dark brown or black | 100 | 90-150 |
Minimum erythema dose determination includes uncovering little characterized ranges of sun-ensured, clinically unaffected skin to expanding dosages of UV light, the measurements to every zone normally being 1.4 times the past measurement. A layout of UV-hazy, glue plastic with eight 2.3 cm2 gaps (ports), fastened to the lower back of the patient might be utilized, with every port presented to an alternate illumination dose from a board of TL-01 fluorescent tubes. Whatever remains of the patient’s skin is secured amid these UV exposures[11].
The dose for each port for NB-UVB photo-testing is reliant on the subject Fitzpatrick skin type. For skin types I-III, initial doses of 400, 600, 800, 1000, 1200, 1400 mJ/cm2 are utilized while for skin sorts IV-VI, 800, 1000, 1200, 1400, 1600 and 1800 mJ/cm2 are utilized. The patients are instructed not to receive any natural or artificial UV light to this region of the skin during the next 24 h and asked to return to the phototherapy center in 24 h. The area of the photo-testing should be identified by ink marking at the different dosage sites. A positive perusing is believed as recognizable erythema inside of the edges of the photo-testing port. If bright red erythema develops or blistering occurs at the site of any of the phototesting sites, topical corticosteroids can be used to treat the area[12].
When MED has been detected, the treatment convention is typically “percent based”. Regularly 70% of the MED worth is utilized for the first treatment; from there on treatment is given three times or all the more week by week with 40%, 20% or 10% increases relying upon neighborhood experience, erythema response and skin sort resistant[13,14].
A semi-automated small hand-held MED tester (Durham MED tester) has gotten to be accessible which produces a settled arrangement of UV dosages, taking into account constricting foils. The Durham MED analyzer lessening arrangement approximates a geometric arrangement with a variable of 1.26. Beginning from the open gap (100%), each consequent gap is lessened by a variable of around 1.26[15].
NB-UVB phototherapy has been observed to be powerful and alright for vitiligo[16]. The consequences of monotherapy with NB-UVB have been exceptional in Asian skin. Roughly 75% of cases in a previous study accomplished more prominent than 75% to finish repigmentation after NB-UVB therapy for a greatest time of 12 mo[17]. The average length of time of sickness was fundamentally shorter in the individuals who had stamped to finish pigmentation contrasted and the individuals who had weaker reaction. Likewise with any treatment methodology for vitiligo, the best results were seen in lesions on the face and neck, trailed by the proximal limbs and trunk. Pigmentation around the hair follicles was the more widely recognized kind of starting repigmentation that was seen in around seventy five percent of cases.
It was focused on impact of NB-UVB and the impact of influenced destinations, individual’s age and duration of illness on the response[18]. Full pigmentation was all the most ordinarily seen in facial sores and sores situated on the neck and trunk in diminishing request of recurrence (68, 57.9, half, individually). Age did not impact the reaction to treatment for facial sores, while in different extents aggregate pigmentation was significantly more ordinarily seen in more youthful patients (under a twenty years). Injuries over the neck and extremities (arms and legs) demonstrated a high percent of total pigmentation (83.3%, 33.3% and 28.5%, separately) in those with illness of late onset (less than two years).
Likewise as the time span of the lesion is prolonged, the sores over the face reacted better. Creators suggest early therapy, as the excellent outcomes were accomplished by youthful patients with late onset vitiligo.
In a randomized, controlled, side-to-side correlation survey, the average change in the NB-UVB was 42.9% contrasted and 3.3% in the untreated side, with the seriousness of malady having been surveyed by VASI[19]. The response changed extraordinarily between distinctive body areas, with the excellent reaction occured over the lower furthest points and most exceedingly terrible reaction on the foot. While all cases did not get therapy for their face, 37.5% of the individuals who decided on therapy of this area had more than seventy five percent repigmentation.
In India, an extensive, open, forthcoming study, just around a quarter of patients could accomplish more than seventy-five percent repigmentation[20]. This poor response can be credited to bring down initial estimation and twice-week after week therapy. In those patients who had huge pigmentation, it was ascribed to great consistence, a more prominent number of medicines and expanding total measurements. Albeit introductory repigmentation was darker, great shading coordinating could be accomplished with proceeded with treatment (Table 2).
| Ref. | Study component | Study design | Patient's No. | Mode of each treatment | Dosimetry | Degree of pigmentation | Incidence of side effects |
| Njoo et al[134] | NB-UVB | Prospective, open, uncontrolled | 51 | Twice a week | 0.25 J/cm2 followed by 20% increments until minimal erythema | After a maximum of 1-yr treatment: > 75% repigmentation in 53% | Pruritus: 8% Xerosis: 4% |
| Scherschun et al[16] | NB-UVB | Retrospective | 7 | Three-times a week | 280 mJ/cm2; followed by 15% increments until mild erythema or pruritus | 70% patients achieved > 75% repigmentation after a mean 19 treatments | Mild asymptomatic erythema: 58% Pruritus: 14% |
| Hamzavi et al[19] | NB-UVB | Randomized, controlled side to side | 22 | Three-times a week | 70% of MED on depigmented skin followed by 10% increments until onset of repigmentation | Mean improvement after 6 mo or 80 exposures: 42.9% (treatment side) vs 3.3% (control side) | |
| Kanwar et al[17] | NB-UVB | Open uncontrolled | 14 | Three-times a week | 280 mJ/cm2 followed by 20% increments | After 1 yr: > 75% repigmentation in 71.4% | Burning and pruritus: 28.6% Xerosis 3nd thickening of lesional skin: 21.4% |
| Kanwar and Dogra[27] | NB-UVB | Prospective, open, uncontrolled | 20 | Three-times a week | 280 mJ/cm2 followed by 20% increments | After a maximum of 1 yr treatment: > 75% repigmentation in 75% patients | Lesional burning and pruritus: 20%. Xerosis 3nd thickening of skin: 15% |
| Brazzelli et al[18] | NB-UVB | Open, uncontrolled | 60 | Twice or three times a week | 180-200 mJ/cm2 followed by 50 mJ/cm2 increments until mild erythema | Complete repigmentation or up to maximum 2 yr: 68% (face) 57.9% (neck). 50% (trunk), limbs poorer results | |
| Kishan Kumar et al[20] | NB-UVB | Prospective, open, non-randomized | 150 | Twice a week | 250 mJ/cm2 (150 mJ/cm2 for children) followed by 20% increments until perceptible erythema | > 75% repigmentation after maximum 1 yr treatment: 17.4% | Erythema, burning, pruritus: 7%. Xerosis: 6% |
In a previous study contrasting twice-week after week, local psoralen and UVA (PUVA) against NB-UVB, authors reported return of pigmentation in 67% of cases in the NB-UVB bunch contrasted and 46% in the local PUVA bunch following four months of therapy[21]. Following three months of NB-UVB therapy, 8% of cases indicated more than 75% repigmentation, though following 1 year of NB-UVB usage, 63% had such repigmentation. In another review, permanent pigmentation following 12 mo of therapy consummation was seen in 78.5% of patients in the NB-UVB bunch and 60% in the PUVA bunch[22].
In the initially randomized, twofold visually impaired, fake treatment controlled study, change in body area territory influenced by vitiligo was more noteworthy with NB-UVB than fake treatment after 48 sittings[23]. Following 1 year of end of treatment, predominance as far as adequacy for NB-UVB was kept up, in spite of the fact that it was not measurably huge. No relationship between length of time of malady and accomplishment of treatment was watched. Albeit some levels of repigmentations were seen in the total series of the NB-UVB bunch and 92% of those in the PUVA bunch, shading match was astounding in whole patients in NB-UVB, however it was so weaker with PUVA. The cosmetic prohibited shading planning had a tendency to bear notwithstanding taking after 12 mo of phototherapy discontinuance.
In a side-to-side examination work, a precisely break even with number of patients accomplished 0%-40%, 40%-60% and 60%-75% repigmentation following 60 sittings[24]. The distinction in the frequency of symptoms, for example, erythema and rankling was not significant between the gatherings.
In a little review investigation, 70% of patients accomplished > 75% repigmentation following an average of 19 remedy sittings. Authors watched that more drawn out ailment length of time associated contrarily with reaction to therapy[16]. In the same sitting, NB-UVB gave higher response contrasted and PUVA in bestowing strength in vitiligo and in pigmentation in both dynamic and permanent illness[25].
Vitiligo for the most part starts in youth with half of the affected persons having ailment onset before the age of twenty years[26]. Be that as it may, experience of NB-UVB in youth vitiligo is constrained. In a planned work, enlisted twenty six youngsters, of whom twenty finished the search. Following therapy for a most extreme of 12 mo, three quarters of the studied group had more than 75% repigmentation. After an average introduction of 34 times, half repigmentation was accomplished. Median length of time of illness before treatment start was less for patients who had stamped to finish repigmentation contrasted and the individuals who had negligible or mild change. Excellent reaction was seen on the face and neck, trailed by the upper arms, thighs and trunk. In spite of the way that the makers assumed that NB-UVB is convincing and all around persevered in youngsters with vitiligo, the whole deal result for dermatologic issues when in doubt is unknown[27].
NB-UVB offers significant points of interest over PUVA which might be essential in picking treatment for patient. It is less tedious, less demanding to perform, and does not require the associative organization of a photograph sensitizer that might bring about queasiness, waterfalls, phototoxic responses, and undesirable medication reactions[25]. Different points of interest additionally incorporate the sheltered use in pregnant ladies and youngsters and truant medication expenses[28,29].
However, short remission rate is one of the best disservices of NB-UVB contrasted and PUVA, regarding infirmities on palms and soles does not react to NB-UVB albeit such sickness can now and again react in youthful youngsters. In correlation, PUVA treatment is regularly viable at these locales as NB-UVB is less infiltrating than UVA radiation[30,31].
NB-UVB has a moderately monochromatic range of emission when contrasted and broadband-UVB (BB-UVB)[32]. Erythema is more usually delivered by BB-UVB than NB-UVB, as NB-UVB is compelling at negligible erythema dosages considerably less than those utilized as a part of BB-UVB treatment[33]. The TL01 light is around 5-10 overlay less strong than BB-UVB for erythema incitement, hyperplasia, edema, sunburn cell arrangement and langerhans cell exhaustion from the skin[34].
NB-UVB is viewed as more powerful with fewer side effects contrasted and BB-UVB in treating a few ceaseless incendiary skin infections as psoriasis and vitiligo. Recently it has been ended up being better than BB-UVB in treatment of HIV-related eosinophilic pustular folliculitis with impressive achievement, particularly against the extreme tingle[35].
Targeted phototherapy implies delivering light to localized diseased areas of skin involving less than 10% body surface area (BSA) and it can be combined with systemic treatments if needed[36]. Since only the affected area is presented to radiation, more doses of radiation can be utilized to achieve better and faster results with lower total cumulative dose and hazards of phototoxicity. Also, it can be used to treat difficult to reach areas like skin folds.
Recent UV devices that discharge light successful for the improvement of vitiliginous patches in a targeted fashion are becoming popular. Among targeted phototherapy devices currently available, excimer laser has been shown to induce the most rapid onset of repigmentation in vitiligo. In addition to excimer laser a monochromatic excimer lamp has also been utilized in the treatment of vitiligo with almost comparable results[37,38].
As far as the targeted UVB devices are concerned, the UV spectrum delivered varies from one machine to another. These devices include “BClear” that delivers BB-UVB, “multiclear” or “dualight” providing UVA and UVB combination and lastly “Bioskin”, which gives a NB-UVB waveband peaking at 311 nm[39].
Xenon chloride laser, popularly known as an excimer laser (EL), is a 308 nm laser that was initially used for treating psoriasis[40]. Be that as it may, as its operational wavelength is near that utilized as a part of NB-UVB, it is utilized to regard vitiligo too. This laser offers the benefit of conveying high measurements of light to limited areas[41,42].
It was initially utilized effectively in vitiligo by Baltás et al[43] in 2001. In 2002 Spencer et al[42] presumed that the level of repigmentation in a time of 2-4 wk is much higher than that accomplished with whatever other current vitiligo treatment. Taneja et al[44] and Choi et al[36] likewise demonstrated helpful results with excimer laser with non acral lesions reacting the best. Two reports contrasted the viability of excimer laser with NB-UVB, and found that the former brought about more huge and faster repigmentation[45,46]. However, neither of these two studies was controlled nor used a standardized scoring method.
The monochromatic excimer light (308 nm MEL) might introduce a few preferences over the laser. Firstly, it gives a bigger illumination field that empowers to treat bigger ranges at once. Secondly, bring down force thickness prompts diminished danger of mishaps because of overexposure, recommending a superior wellbeing profile. The excimer light was found to give proportional pigmentation as contrasted and an excimer laser. In 2003, Leone et al[38] reported that 35/37 (95%) patients hinted at repigmentation inside of initial eight sittings of MEL and excellent and good repigmentation in 18 and 16 patients, respectively. They likewise demonstrated that 3 of their series who were resistant to NB-UVB phototherapy, indicated astounding repigmentation after 308 nm MEL treatment. They suggested this may be conceivable because of the distinction in the method of activity of these two sources, with 308 nm MEL gadget conveying higher vitality fluences to the objective tissue in less time when contrasted with NB-UVB devices.
The repigmentation rate was somewhere around 25% and half over the whole body, and somewhere around half and 75% for vitiligo injuries not situated at hard prominences or extremities[47]. Interestingly, agents additionally noticed that MEL impelled more erythema than EL recommending that regardless of indistinguishable 308 nm crest wavelength, EL and MEL may have diverse photobiological properties.
Additionally, Shi et al[48] likewise found that the repigmentation rates with excimer light were same as those with laser (79% vs 87.5%, P > 0.05). A review investigation of 80 patients with segmental vitiligo (SV) treated with EL demonstrated that 75%-99% repigmentation was accomplished in 23.8% of cases and 50%-74% repigmentation in 20% of cases[49]. This report shows that other than surgical systems, EL may be a possibility for SV patients, with the level of repigmentation absolutely connecting with treatment span, combined measurements, and shorter malady duration[49].
A recent study was conducted in 40 patients of “stable” vitiligo including under 5% BSA who were resistant to conventional oral/topical treatment options. They were treated with a focused on NB-UVB gadget twice-week by week for a most extreme of 30 sessions or until 100% repigmentation, whichever was come to first. Seventy-seven point five percent of cases accomplished pigmentation at a rate from half to hundred percent. Pigmentation started as ahead of schedule as the 3rd dosage now and again and by the 10th measurements in all responders. Best reaction was seen on the face and neck with 20 of the 31 injuries accomplishing 90%-100% repigmentation around there. There was not a correlation between the Length of time of the disease and the repigmentation accomplished. Focused on NB-UVB phototherapy is by all accounts a viable treatment choice in restricted lesion with a quick onset of repigmentation appeared as right on time as 2nd week of therapy[50].
Very few studies utilizing broadband UVB exist. Asawanonda et al[51] analyzed the repigmenting viability of targeted BB-UVB therapy with that of NB-UVB in an equi-erythemogenic manner. Twenty similar vitiliginous lesions from 10 patients were arbitrarily distributed to get either targeted BB-UVB or targeted NB-UVB treatment. Ultraviolet fluences were begun at half of the insignificant erythema measurements detected within the vitiliginous patches, then increased gradually, in the same manner, to ensure equi-erythemogenic comparison. Medicines were completed twice week after week for 12 wk. The outcomes demonstrate that review 1, i.e., 15%-25% repigmentation, to review 2, 26%-50% repigmentation, happened in 6 of 10 subjects. Responses in terms of repigmentation, de-pigmentation, or lack thereof, were similar between lesions receiving broadband and NB-UVB phototherapy. Beginning of repigmentation happened as ahead of schedule as 4 wk of treatment in many subjects. Medicines were all around endured, with just negligible erythema and hyperpigmentation. They concluded that targeted BB-UVB produces comparable clinical reactions to targeted NB-UVB in the treatment of the non-segmental kind of vitiligo.
The points of combination treatment are to lessen the reactions of phototherapy, by possibly encouraging a lower UVB combined measurements or number of medicines, and to enhance adequacy; this includes the simultaneous utilization of a specialists that might offer an added substance or synergistic effect[52]. Similarity between medicines must be considered, as topical operators might have UVB blocking impacts; thus, it is for the most part exhorted that if topical specialists are utilized, they ought to be connected post-UVB presentation[53].
The blend of vitamin D simple and NB-UVB was utilized first by Dogra and Parsad[54]. Decreased levels of vitamin D3 were observed in vitiligo patients and other co-morbid autoimmune conditions. A significant body of data suggests that vitamin D3 is strongly immunosuppressive and improves many Th1 triggered diseases, i.e., it inhibits the Th1 phenotype and potentiates the Th2 phenotype; and that low levels are associated with autoimmune conditions including vitiligo. However, the cause of low vitamin D3 in patients with autoimmune conditions remains unknown[55]. Some authors[56] watched considerably better reaction with the blend contrasted and NB-UVB alone (in spite of the fact that not critical) in a side-to-side examination study. Likewise, others reported the adequacy of mix treatment of NB-UVB with calcipotriol in vitiligo and they recommended that phototherapy with NB-UVB in blend with topical calcipotriol might prompt prior pigmentation with lower beginning aggregate NB-UVB radiation in subjects with vitiligo[57,58].
On the other hand, some authors couldn’t discover empowering contrasts in the rate of repigmentation[59].
Autoimmunity is most likely the major cause suggested for vitiligo. Its part in the disease is supported by discovery of organ-particular antibodies in the patients[60]. Topical immunomodulators are discovered valuable in the treatment of vitiligo alone, and in addition in mix with NB-UVB. It was proposed that cooperation in the middle of pimecrolimus and keratinocytes, making a positive environment for melanocyte development and movement[61].
Castanedo-Cazares et al[62] and Nordal et al[63] reported the viability of the combination in the treatment of vitiligo through the initiation of pathways impacting melanocyte movement and melanogenesis. They recommended that expansion of topical tacrolimus to NB-UVB ought to be further researched, considering its lower carcinogenic profile contrasted and systemic organization. Additionally, the utilization of tacrolimus might be valuable to counteract UVB-instigated erythema by restraining early-stage occasions of the provocative process[64]. Most of the reports consolidating local calcineurin inhibitors with NB-UVB proved that the blend might expand the adequacy, and likely rush the reaction, just for facial sores.
Afamelanotide, is a potent and longer-lasting synthetic analogue of naturally occurring α-MSH. Grimes et al[65] showed in 4 vitiligo patients that combined treatment of NB-UVB and afamelanotide is likely to promote melanoblast differentiation, proliferation and eumelanogenesis leading to faster and deeper repigmentation (at least > 50%) in each case within 2 d to 4 wk.
In another recent study, patients with skin phototypes, III through VI and an affirmed conclusion of NSV that included fifteen percent to half of aggregate body area range were subjected to combination treatment (n = 28) vs NB-UVB monotherapy (n = 27). Following 30 d of NB-UVB therapy, 16 mg of afamelanotide was directed subcutaneously to the blend treatment amass month to month for 4 mo while NB-UVB therapy proceeded with; the second gathering kept on getting NB-UVB monotherapy. A blend of afamelanotide insert and NB-UVB phototherapy brought about clinically obvious, measurably critical predominant and speedier repigmentation contrasted and NB-UVB alone. Reaction was highly discernible in patients with skin types IV to VI[66].
In a recent study, various sessions of intradermal 5-fluorouracil have likewise appeared to enhance NB-UVB adequacy, with 48% of patients accomplishing > 75% repigmentation contrasted with 7% of patients treated with NB-UVB alone[67].
The part of increased oxidative anxiety in the etiology of vitiligo has prompted the utilization of antioxidants orally and topically in the treatment of vitiligo[68,69]. Topical preparations containing catalase and superoxide dismutase have been concentrated on with NB-UVB in a few case arrangement. Topical utilization of pseudocatalase (Mn/ethylenediaminetetraacetic acid-bicarbonate complex) and calcium in mix with decreased-measurements BB-UVB brought about total repigmentation on the face and dorsum of the hands in ninety percent of cases[69]. Elgoweini and Nour El Din[70] concluded that mean number of medicines required to accomplish > half percent repigmentation was diminished (sixteen vs twenty sessions) by adding oral antioxidants to NBUVB. Dell’Anna et al[71] found that a tablet containing vitamins E and C, alpha-lipoic corrosive, polyunsaturated unsaturated fats and cysteine monohydrate brought about more subjects accomplishing > 75% repigmentation contrasted with NB-UVB alone (47% vs 18%, P < 0.05). In another report, NB-UVB was joined with oral organization of polypodium leucotomus separate, which is known not anti-oxidative and immune-modulating characters. In the blend therapy bunch, a pattern towards an expanded repigmentation in the head and neck zone was watched, that almost came to measurable significance[72].
A previous study contrasted four different treatment gatherings of vitiligo patients with progressive course: Steroid oral minipulse (OMP) alone, betamethasone in a dose of 0.1 mg/kg body weight twice weekly on two continuous days for three months took after by decreasing of the dosage by 1 mg consistently over the accompanying three months, OMP with PUVA, OMP with NB-UVB, and OMP with BB-UVB. The outcomes demonstrated that OMP was not helpful all alone but rather had some quality as an enhancer treatment for PUVA and NB-UVB[73].
Erbium laser dermabrasion has been speculated to bring about a more noteworthy profundity of radiation infiltration into the dermis, where it can animate melanocyte undifferentiated cells furthermore bring about conveyance of more prominent measurements of radiation[74]. This standard was demonstrated successfully when generally UV-safe destinations on the hands, feet and hard protuberance were treated with NB-UVB with former Erbium laser dermabrasion. Measurably critical results were acquired with 46% of sores accomplishing > 50% repigmentation with going before 2940-nm erbium:YAG laser contrasted with 4.2% of control sores (P < 0.0001). Furthermore, unfavorable impacts like postponed recuperating (up to 21 d in 1 patient), edema going on for two through fifteen days when limits were dealt with, and hypertrophic scarring hampered the general patient satisfaction[74].
This study proposes a need to investigate the synergistic part of lasers with NB-UVB in the therapy of vitiligo, particularly on generally UV-safe locales.
Recently, home based NB-UVB regimens, using instruments like SS-01 UV phototherapy instrument, Dermfix 1000™ NB-UVB and Waldmann™ NB-UVB 109, have been attempted effortlessly of use at home, along these lines, maintaining a strategic distance from incessant visits to a healing facility based phototherapy unit more than a while. This modality makes phototherapy available to individuals who cannot afford this treatment because of logistical reasons; however, it may not be financially affordable by patients in resource poor developing countries. It is a useful option for localized lesions and can be used to target new lesions at the earliest. Shan et al[75] reported excellent repigmentation in 27 of 36 cases with face and neck lesions, 16 of 43 cases with truncal vitiligo and 9 of 34 patients with limb lesions following treatment with SS-01 UV phototherapy. Lesions on the acral parts were, nonetheless, impervious to treatment.
Newer forms of unconventional phototherapy were endeavored in the management of vitiligo with changing outcomes. In a previous research, the authors[76] looked at the response of skin taking after illumination with UVA1 (340-400 nm) and broadband noticeable light in typical people with skin sorts IV-VI. Utilizing diffuse reflectance accessories, the examiners demonstrated that melanin esteem expanded in a measurements subordinate way taking after UVA1 or noticeable light introduction. Be that as it may, in a late study, El-Zawahry et al[77] contrasted UVA1 phototherapy and NB-UVB and reasoned that UVA1 was less effective than NB-UVB and along these lines had a constrained worth as a monotherapy in vitiligo.
A planned study utilizing a new multi-wavelength focused on Intense Pulse Light System UVA1-UVB in relationship with fluticasone cream was embraced. Eight of the ten patients who took an interest in the survey finished it. Four patients had grade 1 change (1%-25%); one had grade 3 (51%-75%); two had intensifying of the injuries after sun presentation; the last showed no response. The fundamental favorable circumstances of this strategy are that it is anything but difficult to do and it is focused to the skin lesions[78].
It was demonstrated that unmistakable light created by a helium-neon laser (633 nm) could actuate melanocyte relocation and expansion[79]. Few years later, Lan et al[80] utilized the same laser light source to bring about repigmentation in SV. It is trusted that the dermatomal dispersion of SV suggests a neural dysregulation, forcing it somewhat diverse to cure than NSV. The helium-neon laser has been found to adjust the adrenergic dysregulation of cutaneous blood stream seen in SV[81]. Taking after treatment with helium-neon laser, more than half repigmentation was noted in 60% of patients with head and neck SV, repigmentation starting after 16-17 medications[79,81].
Recently, Yu et al[82] utilized 635 nm low-vitality laser for treating SV with the principle objective to distinguish components anticipating therapy result. In this study, 7 of 14 patients reacted to the treatment (reaction was characterized as accomplishing no less than 25% of repigmentation) accordingly affirming the effectiveness, albeit constrained, of noticeable light in SV remediation. Imperatively, the creators inferred that assessment of noninvasive cutaneous blood stream with and without earlier unmistakable light illumination on frosty focused on SV sores might serve as a treatment reaction indicator[82].
Hartmann et al[83] as of late attempted UVB extreme heartbeat light source with top outflow at 311 nm (Relume-Mode, Lumenis) in a right-left similar study where phototherapy was given once week by week on left side and tacrolimus was connected twice every day on right side. They reasoned that long haul treatment with both of the two modalities turned out to be equivalently compelling.
NB-UVB may exert its effects in vitiligo in a two-step process. Both may occur simultaneously. The first being the stabilization of depigmentation process and the second, the stimulation of residual follicular melanocytes[84]. It is likely that NB-UVB, similar to PUVA therapy stimulates the dopa-negative, amelanotic melanocytes in the outer hair root sheaths, which are activated to proliferate, produce melanin, and migrates outward to adjacent depigmented skin resulting in perifollicular pigmentation[85].
The helpful activity includes a mix of impacts in cell cycle energy, modifications in cytokine expression, impact on melanocytes and immunomodulation[86,87].
NB-UVB has been appeared to impel isomerization of urocanic corrosive (UCA), “a cutaneous photoreceptor”, from trans to cis structure, which might be essential in the immunomodulatory impacts of TL-01[86]. Cis-UCA has been appeared to stifle human natural killer cell action in a measurements subordinate manner[56]. The safe concealment properties of cis-UCA might be because of tweak of cytokines, for example, tumor necrosis factor (TNF)-α, interleukin (IL)-10 and IL-12, and also LC depletion[88]. A furthermore effort in the system of activity of cis-UCA incorporates the incitement of prostaglandins E2 (PGE2) generation[89].
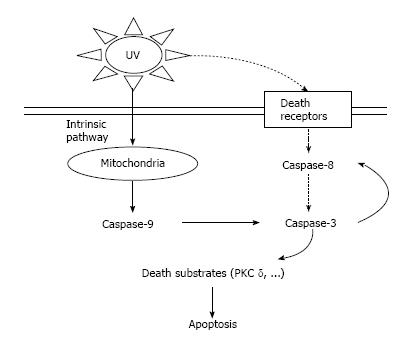
The progress in using NB-UVB for treatment of numerous provocative skin diseases is intellect to be through the inciting of apoptosis and incredible consumption of T cells. DNA harm is one of the real sub-atomic triggers for UVB-actuated apoptosis[90]. Caspases, which are apoptosis related serine proteases inside of the cell, are enacted and give rise to a course of occasions which stimulate atomic buildup, DNA fracture, and breaking down of the cell[87,91].
In caspase-dependent apoptosis, there are two primary pathways included: The natural pathway (mitochondrial/apoptosome pathway) in which cell passing happens through mitochondrial crumbling and the extraneous pathway (death-receptor pathway) in which coordinate enactment of death receptors by UVB is included in UV-prompted cell demise (Figure 2)[92].
Demise receptors have a place with a super group of receptors communicated on any cell and are described via conveying an intracellular passing domain[93]. This family involves CD95 (Fas), the TNF receptor and the TNF-related apoptosis-affecting ligand receptor[94].
Impelling of apoptosis by UVB, in any case, is not particular for keratinocytes but rather influences different cells also including lymphocytes and macrophages[95]. Little information has been created in regards to NB-UVB in keratinocytes. NB-UVB affects apoptosis in T lymphocytes more effectively than BB-UVB[91].
It is conceivable that UVB-prompted lesional T cell apoptosis is interceded by implication by CD95L expression on neighboring keratinocytes or by direct cytotoxic effect of UVB[96].
Antigen presenting cells: Janssens et al[97] showed that the impact of UVB on the capacity of epidermal langerhans cell (LCs) demonstrated a checked concealment of blended epidermal cell lymphocyte response (MECLR) which is utilized as a measure of insusceptible responsiveness. The decrease in MECLR was not paralleled by the progressions in LCs numbers or HLA class 2 expression. On the other hand, Aufiero et al[91] affirmed that different exposures of NB-UVB diminished the thickness of LCs by 20% however on introduction to BB-UVB, LCs morphology was unaffected. Thus, NB-UVB decreases the quantity of both T lymphocytes and LCs.
Natural killer cells: NB-UVB radiation causes a measurement subordinate hindrance of natural killer cell action, in relationship with a lessening in NK-associated cytokines[98-100].
Intense presentation to high measurements of NB-UVB appears to smother sort 1 (IFN-γ) and associatively incite sort 2 (IL-4) cytokine expression while incessant introduction to low dosages of NB-UVB comes about prevalently in the concealment of IFN-γ expression[101]. Piskin et al[102] also, confirmed that the declaration of IFN-γ actuating cytokines (IL-12, IL-18, IL-23 and IL-27) was diminished after chronic NB-UVB presentation.
UVB also fortifies keratinocytes to discharge the immunosuppressive solvent cytokines including IL-10 which repeals the capacity of LCs to present antigens to Th1 clones and even tolerizes them. Therefore, IL-10 moves the resistant reaction from a Th1 into a Th2 reaction[34].
Lebwohl and Ali[103] suggested that UVB-prompt concealment of Th2 chemokine creation proposes that UVB introduction to the skin smothers invasion of Th2 cells to the epidermis, along these lines, both BB-UVB and NB-UVB are thought to be viable for the treatment of different Th2-interceded or Th2-penetrating skin illnesses. What’s more, the impacts of NB-UVB on constituent cells of skin other than keratinocytes might take an interest in the aggregate restorative activity.
UVB radiation has been appeared to be an intense inducer of TNF-α quality expression which intervenes motioning by human keratinocytes[104]. It is recommended that NB-UVB modifies the creation of cytokines and chemokines as a joined consequence of its immediate and aberrant TNF-α-interceded effects[105].
NB-UVB phototherapy expands union of IL-1, TNF-α and LTC-4, which incite melanocyte proliferation and relocation and melanin formation[16]. Furthermore, the parts of IL-1 and TNF-α in synthesis of melanin are disputable and opposing, as reported in a few researches[104,106].
It was suggested that TNF-α hinders the appearance and movement of tyrosinase, the main chemical in melanin blend. It also provoke limitation of pigment formation which is optional to initiation of atomic variable κB. IL-1 animates combination of endothelin-1, which is mitogenic and melanogenic[107]. The disagreement is that IL-1β has been found to lessening expansion of melanocytes and melanogenesis, while IL-1β diminishes melanocyte tyrosinase movement with no impact on multiplication[108]. Imokawa et al[109] watched expanded articulation of endothelin-1, IL-1 and tyrosinase in human keratinocytes in vivo and in vitro after UVB illumination, recommending the conceivable component of repigmentation. Arrival of PGE2 and PGF2 is other system of activity of phototherapy[110]. PGE2 is incorporated in the skin and manages melanocyte and Langerhans cell work, and advances melanocyte proliferation[111].
Skiba et al[112] inspected the impact of UVB light on cytokines (TNF-α, IL-10, IL-1β, FasL) by illuminating the unconstrained changed human epidermal cell line HaCaT to UVA (2000 and 8000 J/cm2) or UVB (200-2000 J/cm2) irradiation. RNA was removed from cells at 0, 4, 8, 12, 16, 24, 48 h post light for consequent ongoing PCR enhancement. They found that, TNF-α mRNA amount were promptly up managed (0 h) next light ,with highest incitement at 8 h post 2000 J/m² UVA and 200 J/m² UVB illumination.
Hino et al[105] explored the impact of NB-UVB on creation of chemokines and proinflammatory cytokines by keratinocytes in examination with BB-UVB. They utilized the same method as that of Skiba et al[112] and affirmed the past consequences of the expanded generation of TNF-α after UVB light however the increased impact of NB-UVB was not as much as that of BB-UVB.
Immuno-histochemical examination was done, to evaluate the TNF-α expression in lesional and perilesional skin when contrasted with ordinary control skin, prior and then afterward NB-UVB treatment. At standard, there was a critical increment of TNF-α in vitiligo injuries contrasted and perilesional and solid skin which proposes a conceivable inclusion of this substance in the loss of pigmentation in vitiligo. The expansion in TNF-α expression after NB-UVB phototherapy recommends another part in repigmentation[106].
Introduction to UV light results in expansion in the quantity of dynamic melanocytes, the rate of melanin combination, and the exchange of shade granules to encompassing keratinocytes[113].
Sunlight exposure causes expanded levels of coursing MSH and ACTH with expanded skin darkening[114]. It was watched that UVB and MSH act synergistically to build melanin content in the skin[115].
UVB light causes lipid peroxidation took after by era of free radicals and consumption of the intracellular pool of diminished glutathione (GSH), bringing about oxidative anxiety. There is confirmation that the dynamic oxygen species created by UVB light might assume a part in melanogenesis and directs the epidermal melanin unit by expanded articulation of melanogenic α-MSH and ACTH peptides[116].
NB-UVB might apply its belongings in vitiligo in a two-stage process. Both might happen all the while. The primary being the adjustment of depigmentation procedure and the second, the incitement of leftover follicular melanocytes[84]. However, the molecular mechanisms of these processes remain unraveled[117].
In ordinary melanocytes, the coupling of development components, for example, bFGF HGF, and ET-1, to receptors on melanocyte results in the quick actuation of the mitogen-enacted protein kinase (MAPK) and ribosomal S6 kinases[118]. In melanocytes, a solitary development element is adequate to stimulate the MAPK course however is not ready to support melanocyte expansion or reasonability. No less than two distinctive development variables in mix are important to affect melanocyte expansion[118].
Wu et al[119] showed that NB-UVB irradiation stimulated the proliferation of melanocytes with a critical increment in the arrival of bFGF and ET-1 by keratinocytes. bFGF has been perceived as a characteristic mitogen for melanocytes, which improves the development and survival of them. ET-1 invigorates DNA union in melanocytes, and has a synergistically stimulatory impact on bFGF-animated DNA amalgamation of these cells.
Kawaguchi et al[120] reported that NB-UVB is viable in stimulation of proliferation and differentiation of functioning melanocytes in epidermis. The precursor melanocytes seem to proliferate into mature pigmented melanocytes after UV exposure. They differentiate into TRP-2 positive melanocytes by the activation of c-kit receptor then become TRP-1 positive melanocytes.
NB-UVB animates expanded articulation of the POMC quality which is joined by creation and arrival of α-MSH[119,121] .
Erythema: NB-UVB is moderately sheltered, and this is one of the fundamental purposes behind it being viewed as the first decision of treatment of summed up vitiligo in grown-ups, and also in youngsters. Erythema is the most critical intense symptom of NB-UVB, and the frequency differs somewhere around 10% and 94% according to the pharmaceutical style and meaning of erythema[120]. Be that as it may, asymptomatic powerless redness is relied upon to be basic, as this is the final stage for NB-UVB in vitiligo. A more noteworthy extent of cases create erythema as contrasted and PUVA, yet they are less inclined to pulsate therapy because of a smaller span of NB-UVB-prompted redness.
Blistering: Lesional blistering following NB-UVB treatment is extraordinary, depicted for the most part in psoriatic plaques, and amid treatment of pityriasis rubra pilaris. The instrument of rankling is misty. George and Ferguson[122] proposed that inside psoriatic plaques might be because of fast loss of scales, presenting lesional skin to a “phototoxic” measurements in connection to contiguous moderately photograph shielded skin causing rapid loss photoprotection from the lesions thus exposing them to a big dose of radiation.
Pruritus: Albeit additionally a typical symptoms of TL-01 treatment, it now and again mirrors the hidden infection forms[123]. Wallengren[124] explained this phenomenon by the possibility of the role of prostaglandin E2 which induces itch and potentiates itch induced by histamine release.
Infection: Reactivation of herpes simplex infection can happen with NB-UVB therapy and safety oriented procedures ought to be brought in those with a background marked by this condition[125]. The possible impacts of NB-UVB on the eyes, specifically presentation related conjunctivitis or keratitis; should be considered if treating patients with periocular skin inflammation, despite the fact that treatment can be performed deliberately with the eye close as opposed to with goggles in this circumstance[126].
Photoaging: Constant NB-UVB introduction is liable to increment photoaging. There is an expanded era of ROS in skin upon introduction to NB-UVB. These ROS are accepted to be basic go betweens of the photoaging process. ROS can adjust proteins in tissue to frame carbonyl subsidiaries, which aggregate in the papillary dermis of photodamaged skin[127].
Carcinogenesis: Actuation of the decay brought on by UVB is settled. This light is a completed disease bringing about specialists and TL-01 has been seemed to provoke DNA hurt in individual’s tissues and animal examples. In a final knockout mouse case, change of hurtful cutaneous neoplasms were essentially more noteworthy for NB-UVB than BB-UVB taking after similar dose presentation[128]. The development of cyclobutane pyrimidine dimers (CPD) was basically ascending with NB-UVB, however those of radiation inducing and 8-oxoguanine were on a very basic level more after BB-UVB. These discoveries recommended the nearby connection in the middle of CPD and the higher cancer-causing capability of NB-UVB. In any event in the setting of psoriasis, it is suggested this hindrance of NB-UVB opposite BB-UVB could be offset the way which the aggregate measurements wanted for leeway of psoriasis is less than that for BB-UVB. The main accessible creature information required perception for a long time[129].
However, there were conflicting data that NB-UVB has been appeared to be less[5] just as[130], and more cancer-causing than BB-UVB[6]. Likewise NB-UVB related skin tumor danger might be not as much as that with PUVA[22]. Rivard and Lim[131] reported that the danger of improvement of nonmelanoma skin growth has been assessed to be under 2% every year which is not as much as that of PUVA. Black and Gavin[132] have recommended that at present, NB-UVB has all the earmarks of being a moderately safe treatment methodology; in any case, consistent long haul follow-up is crucial.
The world writing was methodically explored to upgrade data on the skin tumor hazard with UVB phototherapy, and strategies suggested to reduce carcinogenicity during phototherapy[133].
Skin sparing strategy: Parts of the body where no sores are available (particularly the face) ought to be protected amid medications. Likewise, parts that have repigmented palatable ought to, if conceivable, be protected amid consequent medications (for instance by wearing trousers when in doubt, don’t react to phototherapy)[134]. Privates ought to be likewise protected in light of the fact that these regions, when in doubt, don’t react to phototherapy and genital tumors have been seen after PUVA treatment[22].
Prevention of pointless presentation to characteristic daylight on both treatment and non treatment days and the utilization of UV-blocking specialists on sun uncovered ranges. Also, the use of combined treatments with other modalities to reduce the cumulative dose[135].
Proper patient selection: And using protocols suitable to each patient with lower cumulative doses[132].
Chemoprevention: This term is used to minimize the risk of carcinogenesis to UV therapy by using non toxic diet with antitumour properties. For example, black teas extract which contains dimeric faranols, and polymeric polyphenols. These are effective in reducing UVB and UVA mediated DNA damage and expression of early response genes[136].
Light dose adjustment: This may be the best approach to obliging the carcinogenesis of NB-UVB. Close erythemogenic measurements of NB-UVB clear psoriasis quicker than lower dosages of NB-UVB, but the later regimen is similarly powerful with just somewhat more medicines[6].
Less frequent doses: Dawe et al[137] thought about thrice-weekly and five times week after week medications utilizing half body correlation study. Notwithstanding no critical contrast in extent of patients who indicated skin clearing and time to freedom were found between the two regimens. Besides, the five week by week bunches got higher aggregate measurements and had more scenes of very much delineated erythema.
From the advantages of NB-UVB phototherapy over other phototherapeutics: No topical or oral drug, tests, or unique glasses are needed[34]. Quicker reaction than expansive band UVB and like PUVA[138]. Number of medicines required for clearing is by and large not as much as wide band UVB and PUVA[22]. Safe for youngsters, pregnant ladies and lactating mothers[139]. Eliminating erythemogenic wavelengths underneath 311 nm grants higher intensities and more presentation times bringing about most extreme advantage from phototherapy and a shorter course of treatment[22,32].
Longer reduction periods after treatment like those with PUVA treatment and particularly better than BB-UVB treatment[33]. Studies show 38%-40% of NB-UVB treated patients requires no extra treatment for no less than one year[140].
Because of the diminished force of tight band contrasted with expansive band, more lights are expected to give auspicious treatment. Standard wide band frameworks have 8 to 16 lights, though limit band frameworks need 24 to 48 lamps[141]. Additionally NB-UVB lights seem to have a shorter future than expansive band and subsequently, require more continuous substitution. NB-UVB light lodges costs including the lights are a great deal more expensive[34]. Erythema is less unsurprising than with expansive band UVB, however it might be more extraordinary and steady. Frequently lesional just[8].
Vitiligo is an illness with significant restorative and ensuing psychological sway, instead of physical inability. Most of the researches carried out yet have evaluated the viability of NB-UVB in the change of restorative distortion - that is, a diminishing in the range of depigmentation. In spite of the fact that it is normal to trust that repigmentation taking after NB-UVB would enhance the personal satisfaction in vitiligo patients, there is insignificant target appraisal to such an impact. In an investigation of review configuration, Tjioe et al[142] surveyed the personal satisfaction in vitiligo individuals after therapy with NB-UVB. Despite the fact that the patients evaluated their wellbeing to be by and large great to fantastic, phototherapy represented just a little change in a minority of patients as a rule prosperity. The principle issue of phototherapy in reasonable cleaned people is conspicuousness of the vitiligo injuries resulting in pigmentation of the encompassing typical skin demanding a more noteworthy level of disguising unto total repigmentation is accomplished in the sores. In a report in youngsters, personal satisfaction evaluated by the Children’s Dermatology Life Quality Index (CDLQI) did not lessen altogether in kids having under 25% repigmentation, whereas the diminishment was noteworthy in the individuals who had more than 25% pigmentation with a corresponding abatement in CDLQI with change evaluation of repigmentation[133].
Albeit various administration alternatives exist for vitiligo, UVB phototherapy is for the most part the treatment of decision as it is compelling as well as has a great danger to-advantage proportion. Ordinary BB- and NB-UVB is generally accessible and helpful especially in far reaching illness, despite the fact that NB-UVB has been all the more broadly concentrated on with demonstrated viability. Combined treatments are likewise helpful and might give faster regimentation and treat vitiligo with an added substance system of activity than UVB phototherapy. Progresses in innovation might prompt the proceeding with utilization of UVB phototherapy as a remedy for vitiligo through the improvement of complex gadgets and conveyance frameworks and in addition creative application strategies. These will give expanded helpful choices to all vitiligo patients, especially those with recalcitrant disease.
P- Reviewer: Aksoy B, Gonzalez-Lopez MA, Hu SCS, Kaliyadan F, Lee T, Vasconcellos C S- Editor: Gong XM L- Editor: A E- Editor: Lu YJ
| 1. | Fitzpatrick TB, Pathak MA. Historical aspects of methoxsalen and other furocoumarins. J Invest Dermatol. 1959;32:229-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 94] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 2. | Roelandts R. The history of phototherapy: something new under the sun? J Am Acad Dermatol. 2002;46:926-930. [PubMed] |
| 3. | Fischer T. Comparative treatment of psoriasis with UV-light, trioxsalen plus UV-light, and coal tar plus UV-light. Acta Derm Venereol. 1977;57:345-350. [PubMed] |
| 4. | Diffey BL, Farr PM. An appraisal of ultraviolet lamps used for the phototherapy of psoriasis. Br J Dermatol. 1987;117:49-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Van Weelden H, Baart de la Faille H, Young E, van der Leun JC. Comparison of narrow-band UV-B phototherapy and PUVA photochemotherapy in the treatment of psoriasis. Acta Derm Venereol. 1990;70:212-215. [PubMed] |
| 6. | Bandow GD, Koo JY. Narrow-band ultraviolet B radiation: a review of the current literature. Int J Dermatol. 2004;43:555-561. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Nicolaidou E, Antoniou C, Stratigos AJ, Stefanaki C, Katsambas AD. Efficacy, predictors of response, and long-term follow-up in patients with vitiligo treated with narrowband UVB phototherapy. J Am Acad Dermatol. 2007;56:274-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 85] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Shelk J, Morgan P. Narrow-band UVB: a practical approach. Dermatol Nurs. 2000;12:407-411. [PubMed] |
| 9. | Dogra S, Kanwar AJ. Narrow band UVB phototherapy in dermatology. Indian J Dermatol Venereol Leprol. 2004;70:205-209. [PubMed] |
| 10. | el-Ghorr AA, Norval M. Biological effects of narrow-band (311 nm TL01) UVB irradiation: a review. J Photochem Photobiol B. 1997;38:99-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 99] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 11. | Youn JI, Park JY, Jo SJ, Rim JH, Choe YB. Assessment of the usefulness of skin phototype and skin color as the parameter of cutaneous narrow band UVB sensitivity in psoriasis patients. Photodermatol Photoimmunol Photomed. 2003;19:261-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Waterston K, Naysmith L, Rees JL. Physiological variation in the erythemal response to ultraviolet radiation and photoadaptation. J Invest Dermatol. 2004;123:958-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 38] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Wainwright NJ, Dawe RS, Ferguson J. Narrowband ultraviolet B (TL-01) phototherapy for psoriasis: which incremental regimen? Br J Dermatol. 1998;139:410-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 41] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Leslie KS, Lodge E, Garioch JJ. A comparison of narrowband (TL-01) UVB-induced erythemal response at different body sites. Clin Exp Dermatol. 2005;30:337-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Otman SG, Edwards C, Gambles B, Anstey AV. Validation of a semiautomated method of minimal erythema dose testing for narrowband ultraviolet B phototherapy. Br J Dermatol. 2006;155:416-421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Scherschun L, Kim JJ, Lim HW. Narrow-band ultraviolet B is a useful and well-tolerated treatment for vitiligo. J Am Acad Dermatol. 2001;44:999-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 170] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 17. | Kanwar AJ, Dogra S, Parsad D, Kumar B. Narrow-band UVB for the treatment of vitiligo: an emerging effective and well-tolerated therapy. Int J Dermatol. 2005;44:57-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 60] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 18. | Brazzelli V, Antoninetti M, Palazzini S, Barbagallo T, De Silvestri A, Borroni G. Critical evaluation of the variants influencing the clinical response of vitiligo: study of 60 cases treated with ultraviolet B narrow-band phototherapy. J Eur Acad Dermatol Venereol. 2007;21:1369-1374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Hamzavi I, Jain H, McLean D, Shapiro J, Zeng H, Lui H. Parametric modeling of narrowband UV-B phototherapy for vitiligo using a novel quantitative tool: the Vitiligo Area Scoring Index. Arch Dermatol. 2004;140:677-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 231] [Cited by in RCA: 256] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 20. | Kishan Kumar YH, Rao GR, Gopal KV, Shanti G, Rao KV. Evaluation of narrow-band UVB phototherapy in 150 patients with vitiligo. Indian J Dermatol Venereol Leprol. 2009;75:162-166. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 21. | Westerhof W, Nieuweboer-Krobotova L. Treatment of vitiligo with UV-B radiation vs topical psoralen plus UV-A. Arch Dermatol. 1997;133:1525-1528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 149] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 22. | Parsad D, Kanwar AJ, Kumar B. Psoralen-ultraviolet A vs. narrow-band ultraviolet B phototherapy for the treatment of vitiligo. J Eur Acad Dermatol Venereol. 2006;20:175-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 61] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 23. | Yones SS, Palmer RA, Garibaldinos TM, Hawk JL. Randomized double-blind trial of treatment of vitiligo: efficacy of psoralen-UV-A therapy vs Narrowband-UV-B therapy. Arch Dermatol. 2007;143:578-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 113] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 24. | El Mofty M, Mostafa W, Esmat S, Youssef R, Azzam O, Hunter N, El Hanafi G, Fawzi M. Narrow band Ultraviolet B 311 nm in the treatment of vitiligo: two right-left comparison studies. Photodermatol Photoimmunol Photomed. 2006;22:6-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 36] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 25. | Bhatnagar A, Kanwar AJ, Parsad D, De D. Psoralen and ultraviolet A and narrow-band ultraviolet B in inducing stability in vitiligo, assessed by vitiligo disease activity score: an open prospective comparative study. J Eur Acad Dermatol Venereol. 2007;21:1381-1385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 53] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 26. | Jaisankar TJ, Baruah MC, Garg BR. Vitiligo in children. Int J Dermatol. 1992;31:621-623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 50] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 27. | Kanwar AJ, Dogra S. Narrow-band UVB for the treatment of generalized vitiligo in children. Clin Exp Dermatol. 2005;30:332-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 59] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 28. | Brazzelli V, Prestinari F, Castello M, Bellani E, Roveda E, Barbagallo T, Borroni G. Useful treatment of vitiligo in 10 children with UV-B narrowband (311 nm). Pediatr Dermatol. 2005;22:257-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 28] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 29. | Kural Y, Onsun N, Aygin S, Demirkesen C, Büyükbabani N. Efficacy of narrowband UVB phototherapy in early stage of mycosis fungoides. J Eur Acad Dermatol Venereol. 2006;20:104-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 30. | Morison WL. Psoralen ultraviolet A therapy in 2004. Photodermatol Photoimmunol Photomed. 2004;20:315-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 31. | Engin B, Oguz O. Evaluation of time-dependent response to psoralen plus UVA (PUVA) treatment with topical 8-methoxypsoralen (8-MOP) gel in palmoplantar dermatoses. Int J Dermatol. 2005;44:337-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 32. | Zanolli M. Phototherapy arsenal in the treatment of psoriasis. Dermatol Clin. 2004;22:397-406, viii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 23] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 33. | Berneburg M, Brod C, Benedix F, Röcken M. [New and established indications for phototherapy with narrowband UVB]. J Dtsch Dermatol Ges. 2005;3:874-882. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 34. | Weichenthal M, Schwarz T. Phototherapy: how does UV work? Photodermatol Photoimmunol Photomed. 2005;21:260-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 71] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 35. | Kuwano Y, Watanabe R, Fujimoto M, Komine M, Asahina A, Tsukada N, Tamaki K. Treatment of HIV-associated eosinophilic pustular folliculitis with narrow-band UVB. Int J Dermatol. 2006;45:1265-1267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 36. | Choi KH, Park JH, Ro YS. Treatment of Vitiligo with 308-nm xenon-chloride excimer laser: therapeutic efficacy of different initial doses according to treatment areas. J Dermatol. 2004;31:284-292. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 25] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 37. | Park KK, Liao W, Murase JE. A review of monochromatic excimer light in vitiligo. Br J Dermatol. 2012;167:468-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 38. | Leone G, Iacovelli P, Paro Vidolin A, Picardo M. Monochromatic excimer light 308 nm in the treatment of vitiligo: a pilot study. J Eur Acad Dermatol Venereol. 2003;17:531-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 69] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 39. | Asawanonda P, Charoenlap M, Korkij W. Treatment of localized vitiligo with targeted broadband UVB phototherapy: a pilot study. Photodermatol Photoimmunol Photomed. 2006;22:133-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 40. | Kemény L, Bónis B, Dobozy A, Bor Z, Szabó G, Ignácz F. 308-nm excimer laser therapy for psoriasis. Arch Dermatol. 2001;137:95-96. [PubMed] |
| 41. | Spann CT, Barbagallo J, Weinberg JM. A review of the 308-nm excimer laser in the treatment of psoriasis. Cutis. 2001;68:351-352. [PubMed] |
| 42. | Spencer JM, Nossa R, Ajmeri J. Treatment of vitiligo with the 308-nm excimer laser: a pilot study. J Am Acad Dermatol. 2002;46:727-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 109] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 43. | Baltás E, Nagy P, Bónis B, Novák Z, Ignácz F, Szabó G, Bor Z, Dobozy A, Kemény L. Repigmentation of localized vitiligo with the xenon chloride laser. Br J Dermatol. 2001;144:1266-1267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 63] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 44. | Taneja A, Trehan M, Taylor CR. 308-nm excimer laser for the treatment of localized vitiligo. Int J Dermatol. 2003;42:658-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 58] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 45. | Casacci M, Thomas P, Pacifico A, Bonnevalle A, Paro Vidolin A, Leone G. Comparison between 308-nm monochromatic excimer light and narrowband UVB phototherapy (311-313 nm) in the treatment of vitiligo--a multicentre controlled study. J Eur Acad Dermatol Venereol. 2007;21:956-963. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 68] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 46. | Hong SB, Park HH, Lee MH. Short-term effects of 308-nm xenon-chloride excimer laser and narrow-band ultraviolet B in the treatment of vitiligo: a comparative study. J Korean Med Sci. 2005;20:273-278. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 57] [Cited by in RCA: 44] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 47. | Le Duff F, Fontas E, Giacchero D, Sillard L, Lacour JP, Ortonne JP, Passeron T. 308-nm excimer lamp vs. 308-nm excimer laser for treating vitiligo: a randomized study. Br J Dermatol. 2010;163:188-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 48. | Shi Q, Li K, Fu J, Wang Y, Ma C, Li Q, Li C, Gao T. Comparison of the 308-nm excimer laser with the 308-nm excimer lamp in the treatment of vitiligo--a randomized bilateral comparison study. Photodermatol Photoimmunol Photomed. 2013;29:27-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 49. | Do JE, Shin JY, Kim DY, Hann SK, Oh SH. The effect of 308nm excimer laser on segmental vitiligo: a retrospective study of 80 patients with segmental vitiligo. Photodermatol Photoimmunol Photomed. 2011;27:147-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 50. | Majid I. Efficacy of targeted narrowband ultraviolet B therapy in vitiligo. Indian J Dermatol. 2014;59:485-489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 51. | Asawanonda P, Kijluakiat J, Korkij W, Sindhupak W. Targeted broadband ultraviolet b phototherapy produces similar responses to targeted narrowband ultraviolet B phototherapy for vitiligo: a randomized, double-blind study. Acta Derm Venereol. 2008;88:376-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 52. | Goktas EO, Aydin F, Senturk N, Canturk MT, Turanli AY. Combination of narrow band UVB and topical calcipotriol for the treatment of vitiligo. J Eur Acad Dermatol Venereol. 2006;20:553-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 53. | Kircik L, Bagel J, Korman N, Menter A, Elmets CA, Koo J, Yang YC, Chiou CF, Dann F, Stevens SR. Utilization of narrow-band ultraviolet light B therapy and etanercept for the treatment of psoriasis (UNITE): efficacy, safety, and patient-reported outcomes. J Drugs Dermatol. 2008;7:245-253. [PubMed] |
| 54. | Dogra S, Parsad D. Combination of narrowband UV-B and topical calcipotriene in vitiligo. Arch Dermatol. 2003;139:393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 55. | Ersoy-Evans S. Commentary: Vitamin D and autoimmunity: is there an association? J Am Acad Dermatol. 2010;62:942-944. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 56. | Kullavanijaya P, Lim HW. Topical calcipotriene and narrowband ultraviolet B in the treatment of vitiligo. Photodermatol Photoimmunol Photomed. 2004;20:248-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 57. | Leone G, Pacifico A, Iacovelli P, Paro Vidolin A, Picardo M. Tacalcitol and narrow-band phototherapy in patients with vitiligo. Clin Exp Dermatol. 2006;31:200-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 42] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 58. | Gamil H, Attwa E, Ghonemy S. Narrowband ultraviolet B as monotherapy and in combination with topical calcipotriol in the treatment of generalized vitiligo. Clin Exp Dermatol. 2010;35:919-921. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 59. | Arca E, Taştan HB, Erbil AH, Sezer E, Koç E, Kurumlu Z. Narrow-band ultraviolet B as monotherapy and in combination with topical calcipotriol in the treatment of vitiligo. J Dermatol. 2006;33:338-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 48] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 60. | Ongenae K, Dierckxsens L, Brochez L, van Geel N, Naeyaert JM. Quality of life and stigmatization profile in a cohort of vitiligo patients and effect of the use of camouflage. Dermatology. 2005;210:279-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 125] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 61. | Mayoral FA, Gonzalez C, Shah NS, Arciniegas C. Repigmentation of vitiligo with pimecrolimus cream: a case report. Dermatology. 2003;207:322-323. [PubMed] |
| 62. | Castanedo-Cazares JP, Lepe V, Moncada B. Repigmentation of chronic vitiligo lesions by following tacrolimus plus ultraviolet-B-narrow-band. Photodermatol Photoimmunol Photomed. 2003;19:35-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 63. | Nordal EJ, Guleng GE, Rönnevig JR. Treatment of vitiligo with narrowband-UVB (TL01) combined with tacrolimus ointment (0.1%) vs. placebo ointment, a randomized right/left double-blind comparative study. J Eur Acad Dermatol Venereol. 2011;25:1440-1443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 64. | Fai D, Cassano N, Vena GA. Narrow-band UVB phototherapy combined with tacrolimus ointment in vitiligo: a review of 110 patients. J Eur Acad Dermatol Venereol. 2007;21:916-920. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 65. | Grimes PE, Hamzavi I, Lebwohl M, Ortonne JP, Lim HW. The efficacy of afamelanotide and narrowband UV-B phototherapy for repigmentation of vitiligo. JAMA Dermatol. 2013;149:68-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 66. | Lim HW, Grimes PE, Agbai O, Hamzavi I, Henderson M, Haddican M, Linkner RV, Lebwohl M. Afamelanotide and narrowband UV-B phototherapy for the treatment of vitiligo: a randomized multicenter trial. JAMA Dermatol. 2015;151:42-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 106] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 67. | Abd El-Samad Z, Shaaban D. Treatment of localized non-segmental vitiligo with intradermal 5-flurouracil injection combined with narrow-band ultraviolet B: a preliminary study. J Dermatolog Treat. 2012;23:443-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 25] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 68. | Westerhof W, d’Ischia M. Vitiligo puzzle: the pieces fall in place. Pigment Cell Res. 2007;20:345-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 42] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 69. | Schallreuter KU, Moore J, Wood JM, Beazley WD, Gaze DC, Tobin DJ, Marshall HS, Panske A, Panzig E, Hibberts NA. In vivo and in vitro evidence for hydrogen peroxide (H2O2) accumulation in the epidermis of patients with vitiligo and its successful removal by a UVB-activated pseudocatalase. J Investig Dermatol Symp Proc. 1999;4:91-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 306] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 70. | Elgoweini M, Nour El Din N. Response of vitiligo to narrowband ultraviolet B and oral antioxidants. J Clin Pharmacol. 2009;49:852-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 56] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 71. | Dell’Anna ML, Mastrofrancesco A, Sala R, Venturini M, Ottaviani M, Vidolin AP, Leone G, Calzavara PG, Westerhof W, Picardo M. Antioxidants and narrow band-UVB in the treatment of vitiligo: a double-blind placebo controlled trial. Clin Exp Dermatol. 2007;32:631-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 108] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 72. | Middelkamp-Hup MA, Bos JD, Rius-Diaz F, Gonzalez S, Westerhof W. Treatment of vitiligo vulgaris with narrow-band UVB and oral Polypodium leucotomos extract: a randomized double-blind placebo-controlled study. J Eur Acad Dermatol Venereol. 2007;21:942-950. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 104] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 73. | Rath N, Kar HK, Sabhnani S. An open labeled, comparative clinical study on efficacy and tolerability of oral minipulse of steroid (OMP) alone, OMP with PUVA and broad / narrow band UVB phototherapy in progressive vitiligo. Indian J Dermatol Venereol Leprol. 2008;74:357-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 42] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 74. | Bayoumi W, Fontas E, Sillard L, Le Duff F, Ortonne JP, Bahadoran P, Lacour JP, Passeron T. Effect of a preceding laser dermabrasion on the outcome of combined therapy with narrowband ultraviolet B and potent topical steroids for treating nonsegmental vitiligo in resistant localizations. Br J Dermatol. 2012;166:208-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 52] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 75. | Shan X, Wang C, Tian H, Yang B, Zhang F. Narrow-band ultraviolet B home phototherapy in vitiligo. Indian J Dermatol Venereol Leprol. 2014;80:336-338. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 76. | Mahmoud BH, Ruvolo E, Hexsel CL, Liu Y, Owen MR, Kollias N, Lim HW, Hamzavi IH. Impact of long-wavelength UVA and visible light on melanocompetent skin. J Invest Dermatol. 2010;130:2092-2097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 226] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 77. | El-Zawahry BM, Bassiouny DA, Sobhi RM, Abdel-Aziz E, Zaki NS, Habib DF, Shahin DM. A comparative study on efficacy of UVA1 vs. narrow-band UVB phototherapy in the treatment of vitiligo. Photodermatol Photoimmunol Photomed. 2012;28:84-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 78. | Coelho JD, Ferreira A. Letter: Association of targeted intense pulse light system UVA1-UVB and fluticasone in the treatment of vitiligo: Prospective study of 10 patients. Dermatol Online J. 2010;16:15. [PubMed] |
| 79. | Yu HS, Wu CS, Yu CL, Kao YH, Chiou MH. Helium-neon laser irradiation stimulates migration and proliferation in melanocytes and induces repigmentation in segmental-type vitiligo. J Invest Dermatol. 2003;120:56-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 106] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 80. | Lan CC, Wu CS, Chiou MH, Chiang TY, Yu HS. Low-energy helium-neon laser induces melanocyte proliferation via interaction with type IV collagen: visible light as a therapeutic option for vitiligo. Br J Dermatol. 2009;161:273-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 81. | Wu CS, Hu SC, Lan CC, Chen GS, Chuo WH, Yu HS. Low-energy helium-neon laser therapy induces repigmentation and improves the abnormalities of cutaneous microcirculation in segmental-type vitiligo lesions. Kaohsiung J Med Sci. 2008;24:180-189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 82. | Yu WT, Yu HS, Wu CS, Lee CH, Cheng YC, Lin WT, Chen GS, Lan CC. Noninvasive cutaneous blood flow as a response predictor for visible light therapy on segmental vitiligo: a prospective pilot study. Br J Dermatol. 2011;164:759-764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 83. | Hartmann A, Löhberg L, Keikavoussi P, Eichner S, Schuler G. Treatment of generalised vitiligo with tacrolimus 0.1% ointment vs. UVB intense pulsed light phototherapy: a pilot study. Acta Derm Venereol. 2014;94:585-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 84. | Norris DA, Horikawa T, Morelli JG. Melanocyte destruction and repopulation in vitiligo. Pigment Cell Res. 1994;7:193-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 54] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 85. | Cui J, Shen LY, Wang GC. Role of hair follicles in the repigmentation of vitiligo. J Invest Dermatol. 1991;97:410-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 232] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 86. | Ibbotson SH, Bilsland D, Cox NH, Dawe RS, Diffey B, Edwards C, Farr PM, Ferguson J, Hart G, Hawk J. An update and guidance on narrowband ultraviolet B phototherapy: a British Photodermatology Group Workshop Report. Br J Dermatol. 2004;151:283-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 165] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 87. | Shintani Y, Yasuda Y, Kobayashi K, Maeda A, Morita A. Narrowband ultraviolet B radiation suppresses contact hypersensitivity. Photodermatol Photoimmunol Photomed. 2008;24:32-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 88. | Norval M. The mechanisms and consequences of ultraviolet-induced immunosuppression. Prog Biophys Mol Biol. 2006;92:108-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 72] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 89. | Di Nuzzo S, Sylva-Steenland RM, Koomen CW, de Rie MA, Das PK, Bos JD, Teunissen MB. Exposure to UVB induces accumulation of LFA-1+ T cells and enhanced expression of the chemokine psoriasin in normal human skin. Photochem Photobiol. 2000;72:374-382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 90. | Kulms D, Zeise E, Pöppelmann B, Schwarz T. DNA damage, death receptor activation and reactive oxygen species contribute to ultraviolet radiation-induced apoptosis in an essential and independent way. Oncogene. 2002;21:5844-5851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 196] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 91. | Aufiero BM, Talwar H, Young C, Krishnan M, Hatfield JS, Lee HK, Wong HK, Hamzavi I, Murakawa GJ. Narrow-band UVB induces apoptosis in human keratinocytes. J Photochem Photobiol B. 2006;82:132-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 92. | Sitailo LA, Tibudan SS, Denning MF. Activation of caspase-9 is required for UV-induced apoptosis of human keratinocytes. J Biol Chem. 2002;277:19346-19352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 124] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 93. | van Oosten M, Rebel H, Friedberg EC, van Steeg H, van der Horst GT, van Kranen HJ, Westerman A, van Zeeland AA, Mullenders LH, de Gruijl FR. Differential role of transcription-coupled repair in UVB-induced G2 arrest and apoptosis in mouse epidermis. Proc Natl Acad Sci USA. 2000;97:11268-11273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 70] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 94. | Mak TW, Yeh WC. Signaling for survival and apoptosis in the immune system. Arthritis Res. 2002;4 Suppl 3:S243-S252. [PubMed] |
| 95. | Petit-Frère C, Capulas E, Lyon DA, Norbury CJ, Lowe JE, Clingen PH, Riballo E, Green MH, Arlett CF. Apoptosis and cytokine release induced by ionizing or ultraviolet B radiation in primary and immortalized human keratinocytes. Carcinogenesis. 2000;21:1087-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 63] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 96. | Smith KJ, Diwan H, Skelton H. Death receptors and their role in dermatology, with particular focus on tumor necrosis factor-related apoptosis-inducing ligand receptors. Int J Dermatol. 2003;42:3-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 97. | Janssens AS, Pavel S, Out-Luiting JJ, Willemze R, de Gruijl FR. Normalized ultraviolet (UV) induction of Langerhans cell depletion and neutrophil infiltrates after artificial UVB hardening of patients with polymorphic light eruption. Br J Dermatol. 2005;152:1268-1274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 39] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 98. | Kammeyer A, Teunissen MB, Pavel S, de Rie MA, Bos JD. Photoisomerization spectrum of urocanic acid in human skin and in vitro: effects of simulated solar and artificial ultraviolet radiation. Br J Dermatol. 1995;132:884-891. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 44] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 99. | Weiss E, Mamelak AJ, La Morgia S, Wang B, Feliciani C, Tulli A, Sauder DN. The role of interleukin 10 in the pathogenesis and potential treatment of skin diseases. J Am Acad Dermatol. 2004;50:657-675; quiz 676-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 57] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 100. | Phan TA, Halliday GM, Barnetson RS, Damian DL. Spectral and dose dependence of ultraviolet radiation-induced immunosuppression. Front Biosci. 2006;11:394-411. [PubMed] |
| 101. | Piskin G, Sylva-Steenland RM, Bos JD, Teunissen MB. T cells in psoriatic lesional skin that survive conventional therapy with NB-UVB radiation display reduced IFN-gamma expression. Arch Dermatol Res. 2004;295:509-516. [PubMed] |
| 102. | Piskin G, Tursen U, Sylva-Steenland RM, Bos JD, Teunissen MB. Clinical improvement in chronic plaque-type psoriasis lesions after narrow-band UVB therapy is accompanied by a decrease in the expression of IFN-gamma inducers -- IL-12, IL-18 and IL-23. Exp Dermatol. 2004;13:764-772. [PubMed] |
| 103. | Lebwohl M, Ali S. Treatment of psoriasis. Part 1. Topical therapy and phototherapy. J Am Acad Dermatol. 2001;45:487-498; quiz 499-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 132] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 104. | Schwarz T. Photoimmunosuppression. Photodermatol Photoimmunol Photomed. 2002;18:141-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 62] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 105. | Hino R, Kobayashi M, Mori T, Orimo H, Shimauchi T, Kabashima K, Tokura Y. Inhibition of T helper 2 chemokine production by narrowband ultraviolet B in cultured keratinocytes. Br J Dermatol. 2007;156:830-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 106. | Attwa E, Gamil H, Assaf M, Ghonemy S. Over-expression of tumor necrosis factor-α in vitiligo lesions after narrow-band UVB therapy: an immunohistochemical study. Arch Dermatol Res. 2012;304:823-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 107. | Englaro W, Bahadoran P, Bertolotto C, Buscà R, Dérijard B, Livolsi A, Peyron JF, Ortonne JP, Ballotti R. Tumor necrosis factor alpha-mediated inhibition of melanogenesis is dependent on nuclear factor kappa B activation. Oncogene. 1999;18:1553-1559. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 54] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 108. | Swope VB, Sauder DN, McKenzie RC, Sramkoski RM, Krug KA, Babcock GF, Nordlund JJ, Abdel-Malek ZA. Synthesis of interleukin-1 alpha and beta by normal human melanocytes. J Invest Dermatol. 1994;102:749-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 42] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 109. | Imokawa G, Miyagishi M, Yada Y. Endothelin-1 as a new melanogen: coordinated expression of its gene and the tyrosinase gene in UVB-exposed human epidermis. J Invest Dermatol. 1995;105:32-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 182] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 110. | Pentland AP, Mahoney MG. Keratinocyte prostaglandin synthesis is enhanced by IL-1. J Invest Dermatol. 1990;94:43-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 64] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 111. | Parsad D, Pandhi R, Dogra S, Kumar B. Topical prostaglandin analog (PGE2) in vitiligo--a preliminary study. Int J Dermatol. 2002;41:942-945. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 112. | Skiba B, Neill B, Piva TJ. Gene expression profiles of TNF-alpha, TACE, furin, IL-1beta and matrilysin in UVA- and UVB-irradiated HaCat cells. Photodermatol Photoimmunol Photomed. 2005;21:173-182. [PubMed] |
| 113. | Miyamura Y, Coelho SG, Wolber R, Miller SA, Wakamatsu K, Zmudzka BZ, Ito S, Smuda C, Passeron T, Choi W. Regulation of human skin pigmentation and responses to ultraviolet radiation. Pigment Cell Res. 2007;20:2-13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 170] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 114. | Levine N, Sheftel SN, Eytan T, Dorr RT, Hadley ME, Weinrach JC, Ertl GA, Toth K, McGee DL, Hruby VJ. Induction of skin tanning by subcutaneous administration of a potent synthetic melanotropin. JAMA. 1991;266:2730-2736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 104] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 115. | Sulaimon SS, Kitchell BE. The biology of melanocytes. Vet Dermatol. 2003;14:57-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 81] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 116. | Murahashi H, Azuma H, Zamzami N, Furuya KJ, Ikebuchi K, Yamaguchi M, Yamada Y, Sato N, Fujihara M, Kroemer G. Possible contribution of apoptosis-inducing factor (AIF) and reactive oxygen species (ROS) to UVB-induced caspase-independent cell death in the T cell line Jurkat. J Leukoc Biol. 2003;73:399-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 58] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 117. | Jo SJ, Yoon HS, Woo SM, Youn JI. Time course of tanning induced by narrow-band UVB phototherapy in Korean psoriasis patients. Photodermatol Photoimmunol Photomed. 2006;22:193-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 118. | Böhm M, Luger TA. Melanocortins in fibroblast biology--current update and future perspective for dermatology. Exp Dermatol. 2004;13 Suppl 4:16-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 119. | Wu CS, Yu CL, Wu CS, Lan CC, Yu HS. Narrow-band ultraviolet-B stimulates proliferation and migration of cultured melanocytes. Exp Dermatol. 2004;13:755-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 81] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 120. | Kawaguchi M, Mitsuhashi Y, Kondo S. Overexpression of tumour necrosis factor-alpha-converting enzyme in psoriasis. Br J Dermatol. 2005;152:915-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 49] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 121. | Hill RP, MacNeil S, Haycock JW. Melanocyte stimulating hormone peptides inhibit TNF-alpha signaling in human dermal fibroblast cells. Peptides. 2006;27:421-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 122. | George SA, Ferguson J. Lesional blistering following narrow-band (TL-01) UVB phototherapy for psoriasis: a report of four cases. Br J Dermatol. 1992;127:445-446. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 123. | Goodwin RG, Finlay AY, Anstey AV. Vitiligo following narrow-band TL-01 phototherapy for psoriasis. Br J Dermatol. 2001;144:1264-1266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 124. | Wallengren J. Neuroanatomy and neurophysiology of itch. Dermatol Ther. 2005;18:292-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 41] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 125. | Perna JJ, Mannix ML, Rooney JF, Notkins AL, Straus SE. Reactivation of latent herpes simplex virus infection by ultraviolet light: a human model. J Am Acad Dermatol. 1987;17:473-478. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 74] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 126. | Naldi L, Griffiths CE. Traditional therapies in the management of moderate to severe chronic plaque psoriasis: an assessment of the benefits and risks. Br J Dermatol. 2005;152:597-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 117] [Cited by in RCA: 109] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 127. | Afaq F, Mukhtar H. Botanical antioxidants in the prevention of photocarcinogenesis and photoaging. Exp Dermatol. 2006;15:678-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 171] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 128. | Kunisada M, Kumimoto H, Ishizaki K, Sakumi K, Nakabeppu Y, Nishigori C. Narrow-band UVB induces more carcinogenic skin tumors than broad-band UVB through the formation of cyclobutane pyrimidine dimer. J Invest Dermatol. 2007;127:2865-2871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 53] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 129. | Man I, Crombie IK, Dawe RS, Ibbotson SH, Ferguson J. The photocarcinogenic risk of narrowband UVB (TL-01) phototherapy: early follow-up data. Br J Dermatol. 2005;152:755-757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 79] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 130. | de Laat A, van der Leun JC, de Gruijl FR. Carcinogenesis induced by UVA (365-nm) radiation: the dose-time dependence of tumor formation in hairless mice. Carcinogenesis. 1997;18:1013-1020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 96] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 131. | Rivard J, Lim HW. Ultraviolet phototherapy for pruritus. Dermatol Ther. 2005;18:344-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 55] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 132. | Black RJ, Gavin AT. Photocarcinogenic risk of narrowband ultraviolet B (TL-01) phototherapy: early follow-up data. Br J Dermatol. 2006;154:566-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 133. | Lee AY, Kim NH, Choi WI, Youm YH. Less keratinocyte-derived factors related to more keratinocyte apoptosis in depigmented than normally pigmented suction-blistered epidermis may cause passive melanocyte death in vitiligo. J Invest Dermatol. 2005;124:976-983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 88] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 134. | Njoo MD, Bos JD, Westerhof W. Treatment of generalized vitiligo in children with narrow-band (TL-01) UVB radiation therapy. J Am Acad Dermatol. 2000;42:245-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 154] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 135. | Hartmann A, Lurz C, Hamm H, Bröcker EB, Hofmann UB. Narrow-band UVB311 nm vs. broad-band UVB therapy in combination with topical calcipotriol vs. placebo in vitiligo. Int J Dermatol. 2005;44:736-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 42] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 136. | Bickers DR, Athar M. Oxidative stress in the pathogenesis of skin disease. J Invest Dermatol. 2006;126:2565-2575. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 748] [Cited by in RCA: 770] [Article Influence: 40.5] [Reference Citation Analysis (0)] |
| 137. | Dawe RS, Wainwright NJ, Cameron H, Ferguson J. Narrow-band (TL-01) ultraviolet B phototherapy for chronic plaque psoriasis: three times or five times weekly treatment? Br J Dermatol. 1998;138:833-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 63] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 138. | Lahiri K, Malakar S, Sarma N, Banerjee U. Repigmentation of vitiligo with punch grafting and narrow-band UV-B (311 nm)--a prospective study. Int J Dermatol. 2006;45:649-655. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 46] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 139. | Jury CS, McHenry P, Burden AD, Lever R, Bilsland D. Narrowband ultraviolet B (UVB) phototherapy in children. Clin Exp Dermatol. 2006;31:196-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 83] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 140. | Holme SA, Anstey AV. Phototherapy and PUVA photochemotherapy in children. Photodermatol Photoimmunol Photomed. 2004;20:69-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 26] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 141. | Gibbs NK, Traynor NJ, MacKie RM, Campbell I, Johnson BE, Ferguson J. The phototumorigenic potential of broad-band (270-350 nm) and narrow-band (311-313 nm) phototherapy sources cannot be predicted by their edematogenic potential in hairless mouse skin. J Invest Dermatol. 1995;104:359-363. [PubMed] [DOI] [Full Text] |
| 142. | Tjioe M, Otero ME, van de Kerkhof PC, Gerritsen MJ. Quality of life in vitiligo patients after treatment with long-term narrowband ultraviolet B phototherapy. J Eur Acad Dermatol Venereol. 2005;19:56-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |