Peer-review started: December 15, 2021
First decision: March 16, 2022
Revised: March 29, 2022
Accepted: April 24, 2022
Article in press: April 24, 2022
Published online: June 2, 2022
Processing time: 166 Days and 13.9 Hours
There are 422 million diabetic people in the world. 25% of these individuals are diagnosed with diabetic foot ulcer (DFU). 20% of patients with DFU will suffer amputation of the lower limbs. Following amputation procedures, the mortality rate of patients is over 70% in 5 years. Diabetes has no cure and, therefore, treatment aims to prevent and treat its complications. Autologous platelet-rich plasma (PRP) has been shown to be a therapeutic tool for many types of disorders, including the treatment of DFU. This manuscript aims to carry out a review to provide more knowledge about the efficacy and safety of autologous PRP for wound closure in patients with DFU. The majority of studies included in this review state that PRP promotes improvement of DFU lesions by accelerating tissue healing processes. However, many studies have a small sample size and thus require larger sample range in order to improve robustness of data in the literature.
Core Tip: Platelet-rich plasma (PRP) can be produced by the centrifugation of a patient's peripheral blood, separating the mixture into distinct layers containing plasma, platelets, leukocytes and erythrocytes. An elevated concentration of platelets above the basal value enables accelerated growth of bone and soft tissues with minimal side effects. Autologous PRP administration is a relatively new biotechnology undergoing expansion which continues to reveal optimistic results in the stimulation and enhanced healing of various sorts of tissue injuries.
- Citation: Simão VP, Cury CS, Tavares GMZ, Ortega GC, Ribeiro AC, Santos GS, Lana JFSD. Platelet-rich plasma application in diabetic ulcers: A review. World J Dermatol 2022; 10(1): 1-9
- URL: https://www.wjgnet.com/2218-6190/full/v10/i1/1.htm
- DOI: https://dx.doi.org/10.5314/wjd.v10.i1.1
There are approximately 422 million diabetic people in the world, comprising 8.5% of the adult population[1]. According to the World Health Organization, the number of people with diabetes mellitus increased significantly over the last decades due to the growth of the global population, ageing and prevalence of diabetes in each age range as well as the exposure of individuals to risk factors of such chronic disease[2].
A common consequence of diabetes mellitus is the development of a wound that takes a great amount of time to heal. It arises from the combination of peripheral neuropathy, which results in the loss of peripheral sensibility as well as the changes in hemostatic and vascular systems. Thus, diabetic foot ulcer (DFU) occurs and are often characterized by a series of physiological alterations that may occur on the foot of a patient with non-treated diabetes. Infections or vasculopathies of the lower limbs are among the most common complications, promoting the development of persistent wounds and additional pedal infections, which may lead to extensive tissue necrosis[3].
In the United States, for instance, there are an estimated one million to 3.5 million adults with a history of DFU. Approximately 25% of diabetic adults will develop DFU, of which 20% end up amputated. The recurrence rate of such wounds is 40% in 1 year and 65% in 5 years. In addition, patients with DFU have 2.5 times higher risk of mortality in 5 years than diabetic patients without diabetic foot injuries, and in the presence of amputation, mortality is greater than 70%[4,5].
As there is still no actual cure for diabetes, the interventions aim at a greater control of glucose levels and reduction of the most diverse detrimental risks, offering the patient a better quality of life[6]. The treatment of DFU can comprise the antibiotic therapy, neuropathic drugs, anti-inflammatory drugs, debridement techniques, compressive therapy, hyperbaric oxygen therapy, topical oxygen therapy, negative pressure therapy, placenta-derived products, platelet and leukocyte-rich fibrin, recombinant growth factors and platelet-rich plasma (PRP). Since the disease presents multiple physiological and biochemical variations, there is no “gold standard” treatment[5,7].
PRP is an orthobiologic product defined by a high concentration of platelets, clotting factors and hematological components. These are transformed into a small volume of plasma with a concentration greater than the basal value. PRP has several bioactive proteins, including growth factors, cytokines and peptides, capable of eliciting regenerative properties. Thus, PRP is applied in many fields associated with regenerative medicine, envisioning the enhanced healing process[8].
The preparation of PRP can be achieved via manual or automatic means. The process is given in three stages: blood collection, centrifugation and platelet concentration. It is important to note that during the collection stage, the type of anticoagulant used may influence the final PRP product. In the manual method, blood is subjected to a centrifugation step, which creates a layer of plasma at the top, an intermediate portion referred to as the “buffy coat”, and a dense layer of erythrocytes at the bottom. Plasma and buffy coat can be collected and submitted to a second centrifugation round, achieving greater concentration from platelet sedimentation, thus giving rise to a product rich in both platelets and leukocytes, in this case. Due to the existence of differences in protocols and centrifugation parameters (varying according to G force and time), great variance among PRP products is seen in the literature. In the automatic method, however, there are commercial kits which, although time-saving, can be much more expensive than manual methods and do not always yield great quantities of platelets. Furthermore, PRP varies significantly according to individual hematological characteristics on a per-patient basis. The fact that there is a lot of heterogeneity and variance of PRP products in the literature makes the evaluation of its efficacy far more challenging[8-10].
The preparation of PRP can also have additional steps such as platelet activation, characterizing the final product as PRP gel. Platelet activation can be commonly achieved via the addition of thrombin or calcium to PRP, promoting the formation of a fibrin network and fast liberation of growth factors and cytokines. Different products and concentrations used for platelet activation also contribute to the heterogeneity of PRP. There is no consensus regarding the best platelet activator or even the most appropriate circumstances where PRP would benefit from the addition or exclusion of platelet activation[10,11].
The aim of this study is to prove the efficacy and safety of PRP and its use for healing of wounds in patients with diabetic foot ulcers.
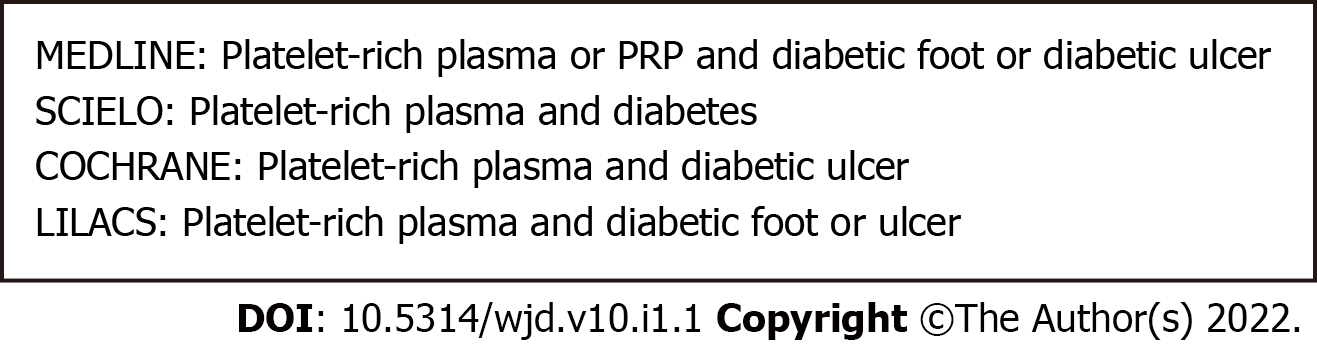
In the present study, we used search strategies that are described on Figure 1, which were conducted in the following databases: MEDLINE, COCHRANE, SCIELO and LILACS. The research was concluded in April 2021.
Prospective Cohort Studies and Randomized Clinical Trials were included. Restrictions were made considering the year of publication; choosing articles with, at most, 21 years of publication. In regards to the language, we considered only articles in English, Spanish and Portuguese. Studies without access to the full text were excluded. A review was made aiming the evaluation of PRP application, analyzing if it is related to healing or an effective improvement of diabetic foot ulcers.
The studies of this review added a total of 296 patients with diabetic ulcers. The interventions include 149 patients subjected to the PRP treatment and, in comparison, 119 patients were subjected to standard treatments such as wound dressing and bandaging 119. Follow-up times vary from four to 20 wk. Characteristics of the selected studies are described in Table 1.
| Ref. | Study design | Intervention | Control | Follow-up | Outcome |
| Driver et al[33], 2006 | RCT | PRP | Saline gel | 12 wk | UHT; ARE; AE |
| Li et al[30], 2015 | RCT | PRP | Gauze with Vaseline | 12 wk | UHT; ARE; R |
| Ahmed et al[31], 2017 | PC | PRP | AD + SS + IP | 12 wk | UHT; ARE; PI; LLA |
| Singh et al[32], 2018 | PC | PRP | ST | 28 d | UHT; CH; AAE |
| Tsai et al[34], 2019 | RCT | PRP | Advanced dressings | 12 wk | UHT; ARE; PI; LLA |
Although complex, diabetic foot injuries appear to be attributed to nerve dysfunction and cell death mainly by means of oxidative stress and inflammation[12]. Insulin resistance and other key components of metabolic syndrome can significantly contribute to dysregulation of metabolic pathways[13]. Metabolic stress promotes an imbalance in mitochondrial redox, culminating in accumulation of mitochondrial and cytosolic reactive oxygen species[14]. Mitochondriopathies are generally responsible for damage and loss of energy in axonal structures, paving the way for neuropathy and subsequent foot ulcers[15]. Additionally, the polyol pathway hyperactivity is also another major contributor as it increases the turnover of cofactors NADPH and NAD+. This brings a significant decrease in the redox potency and regeneration of glutathione, elevated levels of advanced glycation end products and activation of diacylglycerol and protein kinase C isoforms[16]. Depletion of intracellular concentrations of glutathione is the principal cause of oxidative stress and accumulation of toxic by-products, being a major culprit in the development of many pathogenic processes[17].
Many authors believe that the main mechanism responsible for diabetic foot injuries is linked to damaged nerve endings. Irregular action potentials are produced by damaged nerve endings and may be incorrectly translated by the brain as pain or dysesthesia signals[16]. Altered ion channel expression in peripheral nerve fibers is also related to pedal nerve injury, hyperexcitability and neuropathic pain[18]. One study[19] found that calcium ion channels are also disrupted in diabetic conditions, increasing calcium influx in sensory neurons which promotes the rapid stimulation of substance P and glutamate release[19].
Microglial activation is another feature involved in the pathogenic progression of diabetes-mediated neurological disorders. Microglial cells are primarily associated with homeostasis, myelin sheath formation, protection and neuron support from both the peripheral and central nervous systems[20]. Microglial activation occurs after peripheral nerve injury and can last up to 3 mo. This triggers the secretion of many inflammatory mediators including chemokines, cytokines, and cytotoxic substances such as nitric oxide (NO) and free radicals, which shifts homeostasis towards a pro-inflammatory and catabolic microenvironment[19,21]. In patients with metabolic syndrome and diabetic complications, the state of chronic inflammation impedes the standard healing process and aggravates the inflammatory cascade[22-24].
The local release of growth factors and cytokines present in the platelet alpha granules accelerates and improves tissue repair, mimicking and aiding in the lesion restoration pattern. This effect is enhanced when associated with the fibrinolytic system. Fibrinolytic reactions fine-tune cell recruitment of certain cell populations, such as mesenchymal stem cells and other immunomodulatory agents. Such reactions also control proteolytic activity in the areas of healing and regenerative process of mesenchymal tissues such as bone, cartilage and muscle. The regeneration cascade is divided into 4 phases: hemostasis, inflammation, cell and matrix proliferation and lesion remodeling[25].
Capillary leakage allows the recruitment of hemostatic factors and inflammatory mediators. Platelets adhere to exposed collagen and temporary extracellular matrix proteins, triggering the release of bioactive molecules present in alpha granules. Orban et al[26], to help platelets’ adherence, debrided the top of wounds and callosities, turning a chronic ulcer into an acute wound. This process transformed the ulcer into a fertile environment for the application of PRP and the development of an adequate inflammatory cascade. Platelets contain a wide variety of bioactive molecules, including growth factors, chemokines and cytokines, as well as pro-inflammatory mediators such as prostaglandins, prostacyclins, histamine, thromboxane, serotonin and bradykinin[25]. The exposed collagen connects and activates glycoprotein VI, which is present on platelets and megakaryocytes membrane. Another pathway is through G-protein-coupled receptors, activated by adenosine 5′-diphosphate, thromboxane A2, and thrombin[25-27].
Recruitment of neutrophils into the lesion occurs within one to two hours. Afterwards, approximately 48 to 72 h, macrophages reach the lesion and begin debridement and regulation of inflammation. These also participate in the recruitment of fibroblasts and endothelial cells. Lymphocytes are the last cells to reach the site of injury[25].
Cellular activity is predominant, being derived from pluripotent progenitor cells from adjacent tissues. During this phase, there is the occurrence of key events including the formation of an epithelial barrier, angiogenesis and strengthening of injured tissue. Fibroblasts and epithelial cells are affected by some variables such as macrophage activity as well as the secretion of chemotactic, mitogenic and angiogenic growth factors. These events allow cells to infiltrate the injury site, where fibroblasts then synthesize collagen and differentiate into myofibroblasts, specialized cells that promote and facilitate contraction, assisting in wound closure[25].
In this phase, maturation and remodeling occurs, with a balance between anabolic and catabolic reactions. Platelet-derived growth factor, transforming growth factor beta (TGF-β) and fibronectin stimulate fibroblast proliferation and migration in order to synthesize components of the temporary cell matrix. The maturation time at this stage depends on the size of the lesion, individual characteristics and specific regeneration characteristics of the injured tissue. Some health conditions such as ischemia, hypoxia, infection, etc. can interfere with regenerative processes and aggravate DFU[25].
PRP is much more than a mere source of growth factors. This therapeutic tool holds the capacity to effectively modulate the deleterious effects of prolonged tissue inflammation by controlling the exacerbated inflammatory state and establishing a pro-anabolic stimulus. PRP has the potential to regulate tissue turnover thanks to the release of growth factors located in platelet alpha granules, which also promotes pain relief. Thus, its main function is to interrupt the predominant inflammatory and catabolic state in the wound microenvironment, restoring equilibrium and a shift towards a more anti-inflammatory state[25].
Evidence suggests that activation of PRP by thrombin increases the release of many biomolecules such as hepatocyte growth factor, tumor necrosis factor-alpha, TGF-β1, vascular endothelial growth factor and epidermal growth factor. Some studies show that PRP does not only promote an increase in mRNA levels of collagen type II and aggrecan but also reduces their inhibition by the pro-inflammatory cytokine interleukin-1beta[25].
Another biological feature of PRP is the reduction of high levels of NO. According to some authors[25], NO can, in many circumstances, cause inhibitory effects on collagen synthesis and induce chondrocyte apoptosis. There also seems to be an increase in the synthesis of matrix metalloproteinases, which promotes a shift towards catabolic reactions.
Parrish and Roides[28] previously described an interaction between platelets and neutrophils in great detail. In their investigation, the researchers explained that arachidonic acid released by activated platelets is absorbed by neutrophils and converted into leukotrienes and prostaglandins, which are both inflammatory molecules. Interestingly, the interaction between platelets and neutrophils allows the conversion of leukotriene into lipoxin, a potent anti-inflammatory protein capable of limiting neutrophil activation, which prevents diapedesis and improves the responses of the last stages of the inflammatory cascade. The cytokines and growth factors present in PRP contribute to anabolic reactions by modulating the inflammatory state in injured tissues[25,28].
The fibrinolytic system, which is regulated by plasmin, has a fair share of relevance in the healing cascade due. It controls many key components of the cascade including cell migration, bioavailability of growth factors and regulation of other protease systems present in inflammation and tissue regeneration. PRP nevertheless became a feasible therapeutic tool for regenerative medicine and even aesthetics due to its low cost, rapidity and uncomplicated isolation. This orthobiologic material does not trigger major side effects and has high healing potential due to its robust immunomodulatory and paracrine effects. Furthermore, PRP allows the reduction of inflammation via cytokine secretion, increasing the healing potential, regeneration, reepithelization and angiogenic activity of injured tissues and reduces the possibility of infection by eliciting defensive mechanisms against bacteria, which are often major aggressors of DFU[8]. Considering all the properties of platelets and PRP as a whole, the latter stimulates a wide set of natural biologic responses for healing and regeneration of injured tissues[29].
In the current review, the majority of studies aimed to evaluate the efficacy, safety and healing potential of PRP in the treatment of DFU. The studies consider outcomes such as wound healing, ulcer healing time, reepithelization rate and presence of adverse effects. It was observed that many authors used different terms to refer to PRP throughout the work; as an example, in the study led by Li et al[30], the authors used the nomenclature “autologous platelet-rich gel” but described it, in their preparation, as obtaining PRP. Thus, such variability in terms has generated confusion[30].
The results obtained by Ahmed et al[31] are consistent with the statement that PRP has the property of reducing the possibility of infection[8]. All of the included studies state that PRP improves DFU or accelerates the healing process of such lesions, being consistent with the high healing power described by Samadi et al[8].
Ahmed et al[31] demonstrated that PRP is easy and safe to utilize in DFU, as well as Singh et al[32] and Li et al[30], who did not observe any adverse effects associated with the administration of PRP gel. Driver et al[33] found a minimum number of adverse effects and none of them serious. Tsai et al[34] mentioned neither the presence nor the absence of adverse reactions. Such statements are endorsed by the assertion that PRP is safe and easy[8,30-32].
Ahmed et al[31] observed a significantly slower rate of healing using PRP at the end of the 8th wk. The authors reported that this can be explained by the extremely high concentration of growth factors that lead to negative regulation of receptors due to biphasic effects. However, further studies including a larger group of patients are needed to support this observation. In addition, the authors suggested that PRP shall be used for 8 wk to accelerate the rate of healing, and then use the conventional dressing until complete healing is achieved. Moreover, the infection rate was lower in the group that received PRP, which may indicate that PRP also plays additional antimicrobial roles, as previously mentioned[31].
In their meta-analysis, Villela and Santos[35] concluded that evidence indicates favorable outcomes with the use of PRP in DFU. However, the authors stated that such conclusion depends on the association with a multidisciplinary treatment program, since this was present in all of the studies analyzed, indicating that future studies must evaluate the quality of life and cost-benefit outcomes of the treatment. Such relationship with multidisciplinary treatment was only reported by Driver et al[33], implicating the possible prevention of amputations, which directly influences the patient's quality of life. Furthermore, it must be emphasized that there is less accessibility to PRP compared to other conventional therapies, which was also stated in this review[35].
For Pino-Sedeño et al[36], PRP therapy positively impacts wound healing and is a safe option for the treatment of chronic ulcers in diabetic foot. In addition, the authors indicated the need for an interdisciplinary approach for the proper management of DFU; they cited the need for care such as the use of appropriate footwear to prevent recurrence of ulcers[36].
The conclusion of the systematic review by Hirase et al[37] was also consistent with the one obtained in this study, since it was found that the application of PRP in DFU resulted in higher cure rates and complication rates lower than those found in patients under conventional treatment[37].
Ahmed et al[31] and Li et al[30] described fewer complications in the group using PRP than in the control group. Driver et al[33], Singh et al[32] and Tsai et al[34] did not observe significant complications in the intervention group. As for the recurrence of ulcers, Driver et al[33] reported one recurrence in the intervention group and none in the control group, and Li et al[30] reported six recurrences in each group; the other authors did not report recurrence of ulcers during the study period. Hu et al[38] concluded that PRP can be an effective therapy for the treatment of DFU and is not associated with a significant increase in risk for adverse effects[30,32,33].
Among the biases and limitations of the use of PRP, there is its preparation. In all studies analyzed in this review, autologous PRP products were used. The type of anticoagulant used was dextrose citrate by Singh et al[32], while Li et al[30] decided to use an anticoagulant with a pH at a value of 8. The other studies reported no specifications regarding which anticoagulant was used. In terms of centrifugation, in the studies led by Tsai et al[34] and Driver et al[33], a single centrifugation was performed, whilst Singh et al[32], Li et al[30] and Ahmed et al[31] resorted to double centrifugation, all varying in the type of centrifuge as well as time and centrifugation force. Finally, concerning activation, studies used thrombin and/or calcium, varying the origin of thrombin (bovine or homologous) and the presentation of calcium (calcium chloride or gluconate)[30-34].
Another bias found is the way in which PRP is applied, patient follow-up, and decision of association with other therapies, which varied between studies. As for the preparation of the wound, in Singh et al[32], debridement was described; in Ahmed et al[31], the wound was cleaned; in Li et al[30] , topical washing, cleaning, drainage and debridement of callous and necrotic tissue were performed; in Tsai et al[34], cleaning and debridement of the ulcer was described; finally, in Driver et al[33], initial excision/debridement, measurements (culture and vascular tests) and assessment of the wound baseline and application of saline control gel on the wound were described. As for the application of PRP, in Singh et al[32], the use was injectable, once a week; in Ahmed et al[31], use was topical, twice a week; in Li et al[30] , the use was topical; in Tsai et al[34], the use was injectable; finally, in Driver et al[33], the use was topical, twice a week, with intervals between 3 d and 4 d, for 12 wk. Singh et al[32] combined PRP with antibiotic therapy and diabetes control with an oral hypoglycemic agent; Ahmed et al[31] combined glycemic control; in Li et al[30], insulin therapy, anti-infection, nerve-trophic therapies and improvement of the circulation were associated with PRP, and in addition to nutritional support and anti-symptomatic treatments, antihypertensive drugs and lipid regulators were also administered to patients with hypertension and dyslipidemia, respectively, finalizing with dressing changes. In the investigation led by Tsai et al[34], platelet-poor plasma, fibrin-rich plasma, negative pressure treatment to control excessive tissue exudate and hyperbaric oxygen therapy were also included in order to keep the wound infection-free; lastly, Driver et al[33] used a foam dressing in combination with PRP, with the non-absorptive layer on the contact dressing (on the PRP gel) and the external absorptive layer to drain the excessive exudate. A cream was placed on the intact skin around the wound to form a barrier[29-33,37].
The low number of controlled studies included in the review and the variability of study samples also pose a limitation. Most of the studies had a small sample size, requiring larger sample coverage in order to generate more robust data. In the study led by Singh et al[32], the sample consisted of 55 patients of various ages, accounting for variables such as average age of 53.76 (± 10.38); sex, with 34 male and 21 female patients; and place of residence, with 31 patients residing in the rural area and 24 from the urban district. Ahmed et al[31] recruited 56 patients, 38 men and 18 women with an average age of 49.8 years in the control group and 43.2 years in the intervention group; risk factors included were hypertension, previous acute myocardial infection, hyperlipidemia and tobacco consumption. Li et al[30] set the sample size at 117 patients, the largest one in this review. It included patients with a mean age of 63.8 years, with 48 patients having foot ulcers, six in the leg, four in the hip, two in the hand, one on the neck and one on the popliteal fossa. Tsai et al[34] had a sample size of 28 patients, with the average age of the diabetic control group being 64.8 (± 10.7) years, while in the intervention group, the average age was 62.9 (± 10.5) years. Finally, in Driver et al[33], the sample consisted of 72 patients, including patients with type 1 and type 2 diabetes, aged between 18 and 95, with ulcers lasting at least 4 wk[30-32,34,36].
PRP has been shown to be an effective and safe option for DFU, as observed in the results of the studies analyzed, making it an attractive therapy. However, in Brazil, the Federal Council of Medicine (CFM) allowed the use of PRP only on an experimental basis until the present moment. For these reasons, the practical applicability of PRP has yet to be fully elucidated. Nevertheless, the regulatory process was accepted by The Brazilian Health Regulatory Agency due to the clinical indications suggested in the various medical areas listed in the literature. Another important point is the lack of standardization in the preparation, administration and follow-up of PRP. Stipulating a standard is necessary in order to facilitate reproducibility and comparison of studies. Thus, standardized studies concerning the effectiveness and safety of PRP are of utmost importance for reliability in the results so that this tool becomes part of the therapeutic arsenal of complicated disorders, especially DFU.
Since the use of PRP in Brazil is only allowed by the CFM on an experimental basis, the practical applicability of this therapy becomes limited at this time. In this review, PRP demonstrated efficacy and safety in the treatment of diabetic foot ulcers. To increase the reliability of the results obtained and stimulate the regulation of PRP, the production of new studies is highly encouraged, with larger sample size, standardization in the preparation and application of PRP as well as in the patient follow-up and exclusion criteria in order to reduce the risk of bias.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: Brazil
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bugaj AM, Poland; Ng HY, China; Papazafiropoulou A, Greece; Zhang Q, China S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Gong ZM
| 1. | Monteiro-Soares M, Russell D, Boyko EJ, Jeffcoate W, Mills JL, Morbach S, Game F; International Working Group on the Diabetic Foot (IWGDF). Guidelines on the classification of diabetic foot ulcers (IWGDF 2019). Diabetes Metab Res Rev. 2020;36 Suppl 1:e3273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 111] [Article Influence: 22.2] [Reference Citation Analysis (1)] |
| 2. | Kakkar R. Rising burden of Diabetes-Public Health Challenges and way out. Nepal J Epidemiol. 2016;6:557-559. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Naidoo P, Liu VJ, Mautone M, Bergin S. Lower limb complications of diabetes mellitus: a comprehensive review with clinicopathological insights from a dedicated high-risk diabetic foot multidisciplinary team. Br J Radiol. 2015;88:20150135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Hicks CW, Canner JK, Mathioudakis N, Lippincott C, Sherman RL, Abularrage CJ. Incidence and Risk Factors Associated With Ulcer Recurrence Among Patients With Diabetic Foot Ulcers Treated in a Multidisciplinary Setting. J Surg Res. 2020;246:243-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 50] [Article Influence: 10.0] [Reference Citation Analysis (1)] |
| 5. | Rayman G, Vas P, Dhatariya K, Driver V, Hartemann A, Londahl M, Piaggesi A, Apelqvist J, Attinger C, Game F; International Working Group on the Diabetic Foot (IWGDF). Guidelines on use of interventions to enhance healing of chronic foot ulcers in diabetes (IWGDF 2019 update). Diabetes Metab Res Rev. 2020;36 Suppl 1:e3283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 104] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 6. | Wexler DJ. Initial management of hyperglycemia in adults with type 2 diabetes mellitus. UpToDate 2021.. Available from: https://www.uptodate.com/contents/initial management. |
| 7. | Didangelos T, Koliakos G, Kouzi K, Arsos G, Kotzampassi K, Tziomalos K, Karamanos D, Hatzitolios AI. Accelerated healing of a diabetic foot ulcer using autologous stromal vascular fraction suspended in platelet-rich plasma. Regen Med. 2018;13:277-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Samadi P, Sheykhhasan M, Khoshinani HM. The Use of Platelet-Rich Plasma in Aesthetic and Regenerative Medicine: A Comprehensive Review. Aesthetic Plast Surg. 2019;43:803-814. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 155] [Article Influence: 25.8] [Reference Citation Analysis (0)] |
| 9. | Acebes-Huerta A, Arias-Fernández T, Bernardo Á, Muñoz-Turrillas MC, Fernández-Fuertes J, Seghatchian J, Gutiérrez L. Platelet-derived bio-products: Classification update, applications, concerns and new perspectives. Transfus Apher Sci. 2020;59:102716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 27] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Lana JFSD, Andrade Santana MH, Dias Belangero W, Malheiros Luzo AC (eds). Platelet-Rich Plasma: Regenerative Medicine: Sports Medicine, Orthopedic, and Recovery of Musculoskeletal Injuries. Berlin, Heidelberg: Springer Berlin Heidelberg 2014: 1-59. [DOI] [Full Text] |
| 11. | Huber SC, Cunha Júnior JL, Montalvão S, da Silva LQ, Paffaro AU, da Silva FA, Rodrigues BL, Lana JF, Annichino-Bizzacchi JM. In vitro study of the role of thrombin in platelet rich plasma (PRP) preparation: utility for gel formation and impact in growth factors release. J Stem Cells Regen Med. 2016;12:2-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Hicks CW, Selvin E. Epidemiology of Peripheral Neuropathy and Lower Extremity Disease in Diabetes. Curr Diab Rep. 2019;19:86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 351] [Cited by in RCA: 419] [Article Influence: 69.8] [Reference Citation Analysis (0)] |
| 13. | Azzini GOM, Santos GS, Visoni SBC, Azzini VOM, Santos RGD, Huber SC, Lana JF. Metabolic syndrome and subchondral bone alterations: The rise of osteoarthritis - A review. J Clin Orthop Trauma. 2020;11:S849-S855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 14. | Sajic M. Mitochondrial dynamics in peripheral neuropathies. Antioxid Redox Signal. 2014;21:601-620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 15. | Feldman EL, Nave KA, Jensen TS, Bennett DLH. New Horizons in Diabetic Neuropathy: Mechanisms, Bioenergetics, and Pain. Neuron. 2017;93:1296-1313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 572] [Cited by in RCA: 617] [Article Influence: 77.1] [Reference Citation Analysis (0)] |
| 16. | Schreiber AK, Nones CF, Reis RC, Chichorro JG, Cunha JM. Diabetic neuropathic pain: Physiopathology and treatment. World J Diabetes. 2015;6:432-444. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 241] [Cited by in RCA: 286] [Article Influence: 28.6] [Reference Citation Analysis (9)] |
| 17. | Setti T, Arab MGL, Santos GS, Alkass N, Andrade MAP, Lana JFSD. The protective role of glutathione in osteoarthritis. J Clin Orthop Trauma. 2021;15:145-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 18. | Dickenson AH, Matthews EA, Suzuki R. Neurobiology of neuropathic pain: mode of action of anticonvulsants. Eur J Pain. 2002;6 Suppl A:51-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 78] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 19. | Hall KE, Liu J, Sima AA, Wiley JW. Impaired inhibitory G-protein function contributes to increased calcium currents in rats with diabetic neuropathy. J Neurophysiol. 2001;86:760-770. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 71] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 20. | Mika J, Zychowska M, Popiolek-Barczyk K, Rojewska E, Przewlocka B. Importance of glial activation in neuropathic pain. Eur J Pharmacol. 2013;716:106-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 292] [Cited by in RCA: 355] [Article Influence: 29.6] [Reference Citation Analysis (0)] |
| 21. | Vydyanathan A, Wu ZZ, Chen SR, Pan HL. A-type voltage-gated K+ currents influence firing properties of isolectin B4-positive but not isolectin B4-negative primary sensory neurons. J Neurophysiol. 2005;93:3401-3409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 101] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 22. | Greenhalgh DG. Wound healing and diabetes mellitus. Clin Plast Surg. 2003;30:37-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 252] [Cited by in RCA: 293] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 23. | Khamaisi M, Balanson S. Dysregulation of wound healing mechanisms in diabetes and the importance of negative pressure wound therapy (NPWT). Diabetes Metab Res Rev. 2017;33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Tsalamandris S, Antonopoulos AS, Oikonomou E, Papamikroulis GA, Vogiatzi G, Papaioannou S, Deftereos S, Tousoulis D. The Role of Inflammation in Diabetes: Current Concepts and Future Perspectives. Eur Cardiol. 2019;14:50-59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 952] [Cited by in RCA: 834] [Article Influence: 139.0] [Reference Citation Analysis (0)] |
| 25. | Dos Santos RG, Santos GS, Alkass N, Chiesa TL, Azzini GO, da Fonseca LF, Dos Santos AF, Rodrigues BL, Mosaner T, Lana JF. The regenerative mechanisms of platelet-rich plasma: A review. Cytokine. 2021;144:155560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 69] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 26. | Orban YA, Soliman MA, Hegab YH, Alkilany MM. Autologous platelet-rich plasma vs conventional dressing in the management of chronic diabetic foot ulcers. Wounds. 2022;33:36-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 27. | Akbarzadeh S, McKenzie MB, Rahman MM, Cleland H. Allogeneic Platelet-Rich Plasma: Is It Safe and Effective for Wound Repair? Eur Surg Res. 2021;62:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 28. | Parrish W, Roides B. Platelet rich plasma in osteoarthritis: More than a growth factor therapy. Musculoskel Regen. 2017;3:e1518. [DOI] [Full Text] |
| 29. | Babaei V, Afradi H, Gohardani HZ, Nasseri F, Azarafza M, Teimourian S. Management of chronic diabetic foot ulcers using platelet-rich plasma. J Wound Care. 2017;26:784-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 30. | Li L, Chen D, Wang C, Yuan N, Wang Y, He L, Yang Y, Chen L, Liu G, Li X, Ran X. Autologous platelet-rich gel for treatment of diabetic chronic refractory cutaneous ulcers: A prospective, randomized clinical trial. Wound Repair Regen. 2015;23:495-505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 74] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 31. | Ahmed M, Reffat SA, Hassan A, Eskander F. Platelet-Rich Plasma for the Treatment of Clean Diabetic Foot Ulcers. Ann Vasc Surg. 2017;38:206-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 124] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 32. | Singh SP, Kumar V, Pandey A, Pandey P, Gupta V, Verma R. Role of platelet-rich plasma in healing diabetic foot ulcers: a prospective study. J Wound Care. 2018;27:550-556. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 33. | Driver VR, Hanft J, Fylling CP, Beriou JM; Autologel Diabetic Foot Ulcer Study Group. A prospective, randomized, controlled trial of autologous platelet-rich plasma gel for the treatment of diabetic foot ulcers. Ostomy Wound Manage. 2006;52:68-70, 72, 74 passim. [PubMed] |
| 34. | Tsai HC, Lehman CW, Chen CM. Use of platelet-rich plasma and platelet-derived patches to treat chronic wounds. J Wound Care. 2019;28:15-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 35. | Villela DL, Santos VL. Evidence on the use of platelet-rich plasma for diabetic ulcer: a systematic review. Growth Factors. 2010;28:111-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 82] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 36. | Del Pino-Sedeño T, Trujillo-Martín MM, Andia I, Aragón-Sánchez J, Herrera-Ramos E, Iruzubieta Barragán FJ, Serrano-Aguilar P. Platelet-rich plasma for the treatment of diabetic foot ulcers: A meta-analysis. Wound Repair Regen. 2019;27:170-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 61] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 37. | Hirase T, Ruff E, Surani S, Ratnani I. Topical application of platelet-rich plasma for diabetic foot ulcers: A systematic review. World J Diabetes. 2018;9:172-179. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 42] [Cited by in RCA: 42] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 38. | Hu Z, Qu S, Zhang J, Cao X, Wang P, Huang S, Shi F, Dong Y, Wu J, Tang B, Zhu J. Efficacy and Safety of Platelet-Rich Plasma for Patients with Diabetic Ulcers: A Systematic Review and Meta-analysis. Adv Wound Care (New Rochelle). 2019;8:298-308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 32] [Article Influence: 5.3] [Reference Citation Analysis (0)] |