Published online Mar 27, 2018. doi: 10.5313/wja.v7.i1.1
Peer-review started: December 5, 2017
First decision: December 18, 2017
Revised: December 24, 2017
Accepted: January 16, 2018
Article in press: January 16, 2018
Published online: March 27, 2018
Processing time: 157 Days and 10.9 Hours
To determine if video laryngoscopy (VL) has significantly impacted management of difficult airways by decreasing the rate of awake fiberoptic intubation (FOI).
Anesthetic records of 3723 patients who underwent general anesthesia at Rush University Medical Center were reviewed over a 2-mo period prior to the introduction of VLs in 2009 (“pre-VL” group) and over the same 2-mo period after the introduction of VLs in 2012 (“post-VL” group). Patient records with predicted difficult airways based on pre-operative airway examination were analyzed. The primary outcome was rate of awake FOI.
To control for possible factors that may influence the FOI rate, a logistic regression was performed with these factors included as covariates. The rate of awake FOI was 13.1% in pre-VL group compared to 9.0% in post-VL group. Although this decrease was not statistically significant individually (P = 0.1768), it showed a trend toward significance when covariates were accounted for (P = 0.0910). Several factors predicting a higher likelihood of awake FOI were found to be statistically significant: Morbid obesity (larger BMI P = 0.0154, OR = 1.5 per 10 point BMI increase), male gender (P = 0.0026, OR = 3.0) and a higher el-Ganzouri airway score (P = 0.0007, OR = 1.5). Although VLs were seen to be used to intubate 51% of predicted difficult airways, the rate of awake FOI has not significantly changed.
Although VL may continue to grow in popularity, the most difficult airways are still managed using awake FOI.
Core tip: This study shows that the introduction of video laryngoscopes has not significantly impacted the management of predicted difficult airways in the operating room; specifically, that the rate of awake fiberoptic intubation (FOI), the previous gold standard for intubating a predicted difficult airway, has not decreased. Although video laryngoscopy (VL) has clear advantages compared to direct laryngocscopy and has been proven to have increased in popularity in the operating room for non-difficult airways, we postulate that the anesthesiologist’s assessment of the ability to mask ventilate is likely a key factor in the choice of awake FOI vs VL.
- Citation: Jarzebowski M, Rajagopal A, Austell B, Moric M, Buvanendran A. Change in management of predicted difficult airways following introduction of video laryngoscopes. World J Anesthesiol 2018; 7(1): 1-9
- URL: https://www.wjgnet.com/2218-6182/full/v7/i1/1.htm
- DOI: https://dx.doi.org/10.5313/wja.v7.i1.1
Tracheal intubation in patients with predicted difficult airways often requires advanced techniques and equipment, much of which is changing as technology advances. As anesthesiologists, we often turn to difficult airway algorithms such as those published by the American Society of Anesthesiologists to offer guidance[1]. One of the newest and most commonly used tools is the video laryngoscope (VL). Introduced into practice around 2001, VLs have gained widespread use in the operating room. Multiple studies have compared VL to direct laryngoscopy in patients with at least one predictor of a difficult airway and found increased success in first-attempt intubations[2-5], improved Cormack Lehane view obtained[4-7] and decreased time to intubation[4,5,7]. The data from these studies are difficult to compare, with wide variances in patient populations, level of experience and specialty of the physician performing the intubation, differences in location of airway management, and multiple different VLs available for use. Despite such encouraging outcomes, data on how anesthesiologists are using VL for predicted difficult intubations is lacking.
The previous gold standard technique for tracheal intubation in patients with predicted difficult airways has been flexible bronchoscopy. This is either done following induction of general anesthesia or awake, while maintaining spontaneous ventilation, in patients assessed to be difficult to mask ventilate or who require a neurological exam post intubation (awake fiberoptic intubation or FOI). By maintaining spontaneous ventilation, one eliminates the risk of the much feared “can’t intubate, can’t ventilate” scenario. The ASA difficult airway algorithm[1] recommends assessment of the merits of awake intubation and preservation of spontaneous ventilation in all patients. Although the success rate of awake FOI is reported to be high (ranging from 88%-100%[8-10]), this technique requires considerably more skill and time than direct laryngoscopy. There is also potentially more discomfort for the patient. At Rush University Medical Center, attending and resident physicians are encouraged and trained to adhere to the ASA difficult airway algorithm for securing difficult airways. If VL is deemed appropriate by an attending for a difficult airway then this method is employed by the attending and resident. With the logistical challenges of awake FOI and the advent of the newer, faster and simpler VL, we hypothesize that the number of awake FOI has decreased for predicted difficult airways.
Following institutional IRB approval, we collected data for a 2-mo period (November and December of 2009) before the introduction of VL at our hospital (the “pre-VL” group) and for a 2-mo period (November and December of 2012) after the introduction of VLs (the “post-VL” group). We reviewed anesthetic records of patients undergoing general anesthesia both before and after the introduction of VLs at a major academic medical center in order to assess any change in airway techniques used to intubate the trachea. VLs were first introduced at the institution in May, 2010. Given this information, we collected patient-level data for each surgical encounter 6 mo before and then three years after their introduction. The gap allows for familiarization of anesthesia personnel with the new VLs, as well as time for the equipment to become more readily available. Using electronic medical records, all patients over the age of 18 years who received general anesthesia during those time periods were identified and their anesthetic record for that encounter reviewed.
From the pre-anesthetic evaluation, we reviewed each patient’s modified el-Ganzouri airway score (Table 1)[11]. This validated score for predicting difficult airways includes the following criteria: interincisor gap, head and neck movement, ability to prognath, thyromental distance, body weight, history of difficult intubation and Mallampati classification. Based on this scale, patients with a score of 4 or greater have a significant likelihood of difficult intubation and alternative methods to direct laryngoscopy should be considered. Therefore, only patients with a modified el-Ganzouri score of 4 or greater were included in our study.
| Score | 0 | 1 | 2 |
| Interincisor gap | > 4 cm | < 4 cm | Cannot open mouth |
| Head/neck movement | > 90 degrees | 90 degrees | < 90 degrees |
| Buck teeth | Can prognath edentulous | Can approximate teeth only | Cannot approximate teeth |
| Thyromental distance | > 6.5 cm | 6.0-6.5 cm | < 6.5 cm |
| Body weight | < 90 kg | 90-110 kg | > 110 kg |
| Hx of difficult intubation | None | Questionable | Definite |
| Mallampati classification | I | II | III |
We excluded patients who underwent monitored anesthesia care (MAC) and regional or neuraxial anesthesia as their primary anesthetic. We also excluded patients undergoing cardiac surgery, as these patients are frequently left intubated post-operatively (one of our measured secondary outcomes). We excluded patients undergoing thoracic surgery, as their airway management is frequently different to accommodate single-lung ventilation. We also excluded obstetric patients from our data set as the vast majority of patients have neuraxial anesthesia. Patients who had been intubated prior to the operating room were also excluded.
Data collected included age, gender, American Society of Anesthesiologists (ASA) status, body mass index (BMI), and el-Ganzouri airway score with individual components (weight, Mallampati Score, thyromental distance, previous difficult intubation, neck range of motion and ability to prognath the teeth). Airway management data collected included awake FOI vs asleep endotracheal intubation (primary outcome), Cormack-Lehane view obtained, number of attempts at intubation prior to securing endotracheal intubation, method used to secure airway (direct laryngoscopy vs VL vs fiberoptic bronchoscope), if rapid sequence intubation (RSI) was used, if rescue laryngeal mask airway was used, and if the patient was left intubated after surgery.
Power analysis is based on the primary outcome of a reduction in rate of awake vs asleep intubations. Assuming a base rate of 15% awake intubations prior to introduction of the VL and a 50% reduction to 7.5% after introduction, at 80% power to detect a reduction, 219 subjects per group (438 total) are required, using standard parameters of 5% alpha for a one-sided test of proportions.
All patient data was de-identified prior to analysis and stored on password-protected laptops belonging to study personnel. In total, 3723 patient records were reviewed. 461 patients met the inclusion and exclusion criteria and were analyzed. Their characteristics can be seen in Table 2. The primary outcome was rate of awake FOI. To control for possible factors that may influence the FOI rate, a logistic regression was performed with these factors included as covariates. Various models including models with interaction terms were constructed and evaluated using fit indices. Differences between time periods were also compared using Student’s t-test (with appropriate adjustment for violations of homoscedasticity), Mantel-Haenszel, χ2 and Fisher’s exact tests. All analyses were performed using SAS version 9.2 (SAS Institute. Cary, NC, United States). Significance threshold was set at α = 0.05. Model based assumptions were evaluated for violations using descriptive methods.
| Pre-VL | Post-VL | ||
| Mean ± SD | Mean ± SD | P value | |
| Age | 55 ± 14 | 57 ± 14 | 0.2435 |
| Height (m) | 1.71 ± 0.11 | 1.69 ± 0.11 | 0.0658 |
| Weight (kg) | 108 ± 30 | 97 ± 26 | 0.00011 |
| BMI | 37 ± 10 | 34 ± 9 | 0.00141 |
| ASA Status | 2.67 ± 0.62 | 2.73 ± 0.67 | 0.3145 |
| Composite Airway Score | 4.83 ± 1.21 | 4.79 ± 1.22 | 0.7711 |
| Count (%) | Count (%) | ||
| Gender | 0.4546 | ||
| Female | 105 (51) | 139 (55) | |
| Male | 101 (49) | 116 (45) | |
| Mallampati score | 0.04811 | ||
| 1 | 5 (2) | 6 (2) | |
| 2 | 89 (43) | 85 (33) | |
| 3 | 112 (54) | 164 (64) | |
| Interincisor gap | 0.9033 | ||
| > 4 cm | 142 (69) | 180 (71) | |
| < 4 cm | 63 (31) | 73 (29) | |
| Cannot open mouth | 0 (0) | 2 (1) | |
| Neck range of motion | 0.00841 | ||
| > 90° | 149 (73) | 152 (60) | |
| 90° | 37 (18) | 69 (27) | |
| < 90° | 19 (9) | 34 (13) | |
| Ability to prognath | 0.3058 | ||
| Can prognath | 157 (77) | 187 (73) | |
| Can approximate teeth | 46 (22) | 62 (24) | |
| Cannot approximate teeth | 2 (1) | 6 (3) | |
| Thyromental distance (cm) | 0.6811 | ||
| > 6.5 | 60 (29) | 69 (27) | |
| 6.0 – 6.5 | 128 (62) | 162 (64) | |
| < 6.0 | 18 (8) | 24 (9) | |
| Known previous difficult intubation | 0.1740 | ||
| None | 162 (79) | 213 (84) | |
| Questionable | 24 (12) | 26 (10) | |
| Definite | 19 (9) | 16 (6) | |
| Surgery type | 0.00851 | ||
| General | 64 (31) | 55 (22) | |
| Gynecologic | 24 (12) | 27 (11) | |
| Neurosurgery | 20 (10) | 56 (22) | |
| Orthopedic | 15 (7) | 16 (6) | |
| Other | 37 (18) | 47 (19) | |
| Spine | 38 (18) | 36 (14) | |
| Vascular | 8 (4) | 16 (6) |
The statistical methods of this study were reviewed by Mario Moric, MS from Rush University Medical Center.
Most demographics were similar between both groups but several were found to have significant differences. BMI (and correspondingly weight) was significantly lower in the post-VL patient population. Additionally, the post-VL group had significantly more patients with higher Mallampati scores. Neck range of motion was also significantly less in the post-VL patient population. The final model included age, BMI, time period (pre-VL/post-VL), gender, ASA status, composite airway score, neck range of motion, Mallampati score and surgery type (based on significant univariates differences at baseline and need for control due to possible confounding).
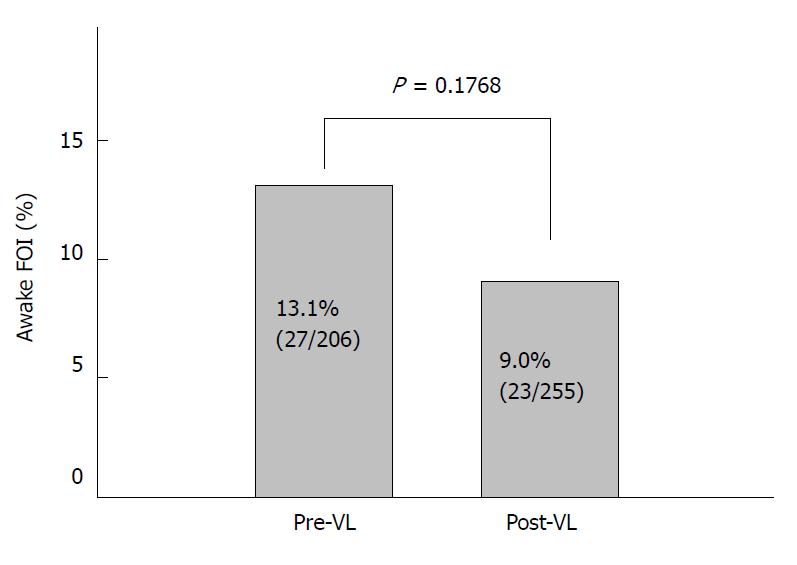
The rate of awake FOI was 13.1% in the pre-VL group compared to 9.0% in post-VL group (Figure 1), although this decrease was not statistically significant (P = 0.1768). Due to differences in demographics between the two time periods, we included these and other factors (listed above) that may impact the primary outcome in the logistic model, to account for these effects. Controlling for the covariates did not change the significance of the effect over time (P = 0.0910) but does indicate a trend toward significance.
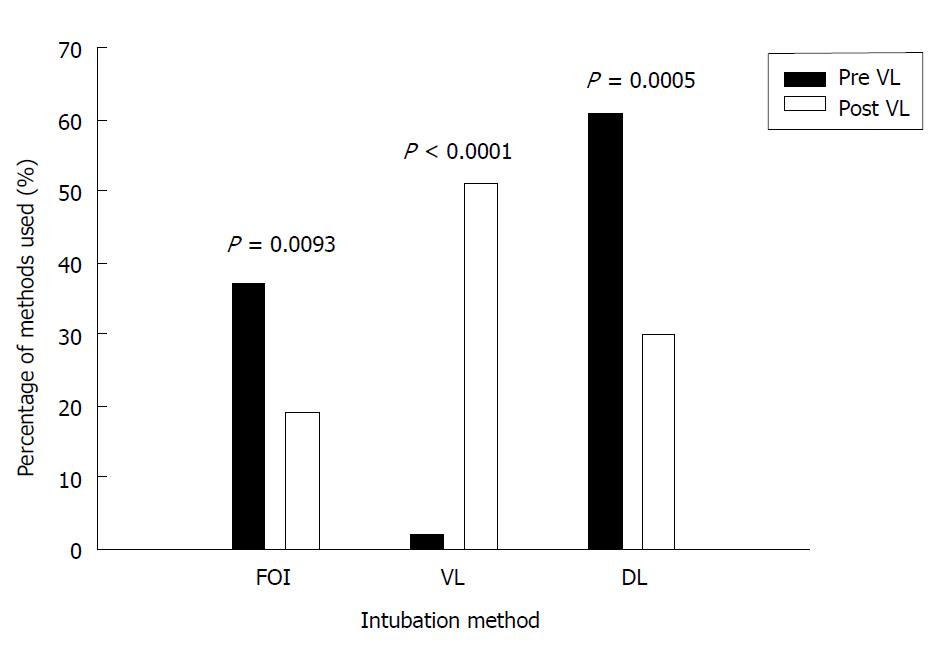
Method of intubation for patients with predicted difficult airways was significantly different after the introduction of VLs (Figure 2). In the post-VL group, VLs were used to intubate 51% of predicted difficult airways (P < 0.0001, Table 3). The overall rate of FOI (both awake and asleep) decreased from 37% to 19% (P = 0.0093) in patients with predicted difficult airways. The use of direct laryngoscopy decreased from 61% in the pre-VL group to 30% in the post-VL group (P = 0.0005).
| Pre-VL | Post-VL | ||
| Count (%) | Count (%) | P value | |
| Grade (Cormack-Lehane view obtained) | 0.0141 | ||
| 1 | 86 (57) | 149 (75) | |
| 2 | 43 (29) | 28 (14) | |
| 3 | 19 (13) | 16 (8) | |
| 4 | 2 (13) | 5 (3) | |
| Intubation method | < 0.00011 | ||
| FOI | 72 (37) | 44 (19) | 0.00931 |
| VL | 4 (2) | 119 (51) | < 0.00011 |
| DL | 118 (2) | 70 (30) | 0.00051 |
| Rapid sequence induction | 0.1489 | ||
| RSI | 30 (17) | 27 (12) | |
| Rescue LMA used | 0.7055 | ||
| Yes | 4 (17) | 3 (1) | |
| Patient left intubated | 0.5467 | ||
| Yes | 24 (12) | 25 (12) |
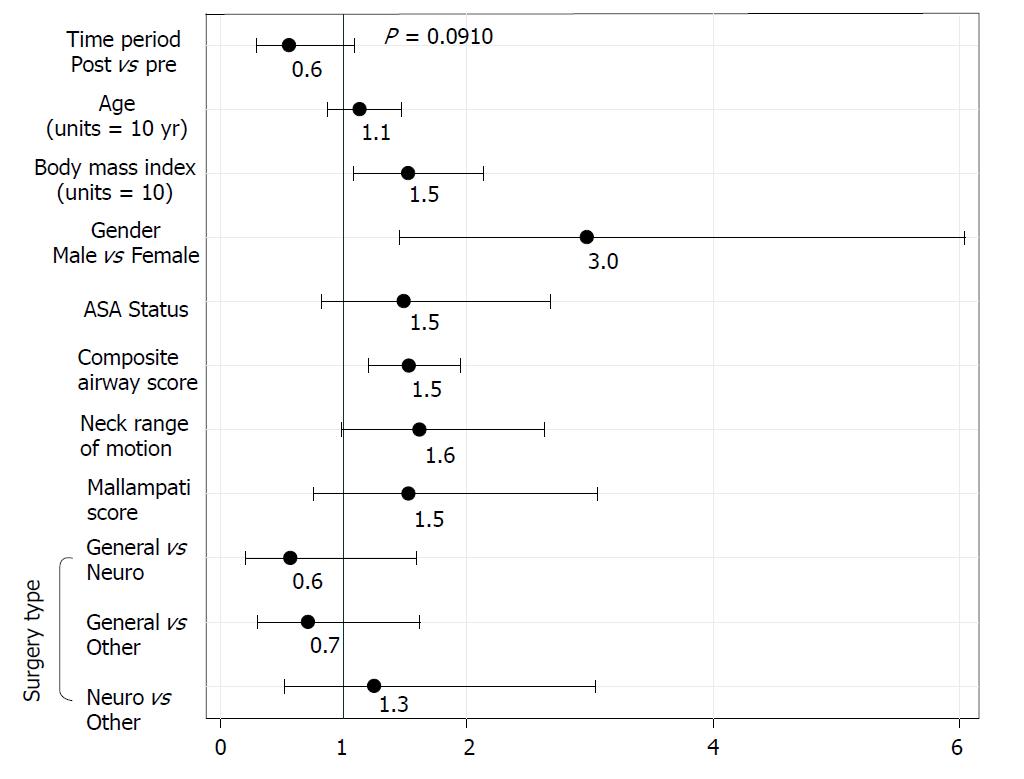
Potential risk factors, determined prior to study initiation, and significant demographic variables, were entered into the logistic regression predicting likelihood of awake FOI. After model fit and selection, the resulting odds ratios are shown in Figure 3. Several statistically significant factors predicting a higher likelihood of awake FOI were found: morbid obesity determined by BMI (P = 0.0154, OR = 1.5 per 10-point BMI increase), male gender (P = 0.0026, OR = 3.0) and a higher el-Ganzouri airway score (P = 0.0007, OR = 1.5 per point above 4). Neck range of motion (P = 0.0582, OR = 1.6) verged on significant but was not. Neither ASA status (P = 0.1869), Mallampati score (P = 0.2278), age (P = 0.3598) nor surgery type (P = 0.5437) was significantly predictive. The BMI and age variables were scaled so that the odds ratio refers to 10-point change instead of one-point changes. So, a 10-point increase in BMI is associated with 1.5 the odds of an awake FOI. Additionally, surgery type within three categories (general, neurologic, and other) was included in the model as a covariate, since the parameterization with the full seven categories was not estimable.
To evaluate the risk factors independent of the time period, another model with time period removed was run and produced similar results indicating that these risk factors are independent of the time period.
To evaluate possible relationships among the predictors/covariates models, the interactions among them were tested. There were no interactions that appreciably improved the fit of the model or the overall significance of the primary contrast. Although the primary outcome was not statistically significant it trended towards significance with a P-value of 0.0910. The decrease in awake FOI, from 13.1% to 9.0% represents a reduction of 4.1%. Our power analysis was based on the assumption of a larger effect size (7.5%), so if the true effect is smaller, we may be underpowered to test the hypothesis.
Our results suggest that the proportion of patients with predicted difficult airways who receive awake FOI has not changed significantly following the introduction of VLs at the magnitude we had postulated. However, there was a trend toward a reduction in the rate of awake FOI in patients with difficult airways. Overall, the method used to intubate patients with predicted difficult airways changed significantly, with significantly fewer FOI (awake and asleep) and direct laryngoscopies and significantly more VL. Similar results were obtained by Law et al[12], who noted a steady incidence of awake FOI each year from 2002 to 2013, despite a significant increase in the use of VL over the same time period. The trend toward a reduction in awake FOI (although not statistically seen in our data) has received commentary in recent publications[13,14], with attention drawn to lack of training in awake FOI, to advances in VL and supraglottic airway devices (SAD), and to pharmacologic advances in reversal of neuromuscular blockade as possible explanations.
Others disagree with the continued use of awake FOI. A recent editorial[13] suggests that the practice of awake FOI should be abandoned as our gold standard for airway management in predicted difficult airways. They cite a relative paucity of training in fiberoptic intubations with trainees prefering the latest technological advances in video laryngoscopy. One must also consider the array of SAD that now provides a useful rescue airway for the “can’t intubate, can’t ventilate” scenario when laryngoscopy fails. Many of these SAD’s provide a conduit for intubation. The introduction of sugammadex into clinical practice may also have influenced the management of difficult airways. A case report of its utility in a “can’t intubate, can’t ventilate” scenario was illustrated recently[14,15] in a patient who had failed previous attempts at awake FOI. With the continued advances in VL, SAD’s and emergency reversal of neuromuscular blockade, perhaps the need for awake FOI is further decreasing.
Patients with cervical myelopathy also warrant consideration. In the past, fear of exacerbating their myelopathy led most anesthesiologists to perform awake FOI with a confirmatory neurologic exam after intubation and before induction of general anesthesia. Studies looking at cervical spine motion during intubation with VLs show mixed results, with one reporting no difference in cervical spine movement between direct laryngoscopy and VL[16] and another showing significantly less cervical spine movement between direct laryngoscopy and VL[17]. However, when directly compared, asleep FOI yielded significantly less cervical spine motion than intubation by VL[18]. It seems reasonable, therefore, to conclude that fiberoptic bronchoscopy may be a safer technique for intubation in patients with critical cervical myelopathy; however, outcomes data remains lacking.
In its relative infancy as a technique, VL will also have its limitations. A retrospective analysis of intubations using VL found the most likely predictors of failed VL were the presence of a surgical scar in the oropharynx, history of neck irradiation, or presence of a neck mass[19]. Interestingly, these are also predictors of difficult mask ventilation, based on a retrospective analysis by Kheterpal et al[20]. It seems likely, therefore, that we are accepting a certain amount of risk by inducing general anesthesia and relying on VL without fully understanding who is most at risk of failed airway mangement with this technique.
Data from the National Audit Project (NAP4) of the Royal College of Anaesthetists looking into complications of airway management in the United Kingdom makes some pertinent points concerning the implications of difficult awake FOI[21]. The authors present data of unsuccessful awake FOI. Difficulties encountered were because of lack of patient cooperation, anatomical airway obstruction and obscuration of visualization by blood or secretions. However, the reviewers of the NAP4 data did caution that the failure to consider or employ awake FOI when clinically indicated provided the largest cohort of cases of failed airway management that they reviewed. Based on this, they recommend that “all anaesthetic departments should provide a service where the skills and equipment are available to deliver awake fiberoptic intubation whenever it is indicated”. Notably, they also recommend that “where FOI is considered the optimal method of securing the airway, an awake technique should be considered unless contraindicated”[21].
The strengths of our project lie in defining potential trends in airway management with the advent of new technology. There will likely always be a subset of patients who, despite advances in SAD’s, VL and pharmacologic reversal of neuromuscular blockade, cannot be intubated or ventilated. Therefore, we posit the need for awake FOI will remain for the future. Our commitment as a specialty to patient safety mandates approaching predicted difficult airways with the same caution as in the past, despite advances in technology, as the outcomes of failed airway management remain devastating. Our study also emphasizes the implications for training of future anesthesiologists to foster proficiency at awake FOI. Familiarity with awake FOI is necessary if we are to continue to consider it a viable option in patients with predicted difficult airways.
The limitations of our study are several. First, as it is retrospective data, the possibility of confounding variables is always present. Our two groups had some differing baseline characteristics, which we attempted to control for using logistic regression. However, prospective data would be more valuable. Second, our sample size was relatively small. With advances in electronic anesthetic records, a larger review of anesthetic data may hold more statistical power to observe these trends over time. In conclusion, our data demonstrate a trend, although not significant, toward a decrease in awake FOI in patients with predicted difficult airways, although at a smaller effect size than expected. This trend has been noted at other institutions and highlights potential risks to patient safety in patients with difficult airways. Our data also demonstrate a reduction in the use of asleep FOI and direct laryngoscopy for the intubation of predicted difficult airways, with > 50% of these patients receiving VL. We believe awake FOI continues to remain the gold standard for managing the predicted difficult airway, despite new technology. As such, we advocate for a specialty-wide commitment to train future physician anesthesiologists to be ready to manage the most difficult of airways safely.
Advanced techniques and equipment are often needed for tracheal intubation in patients with difficult airways. New technology has brought about video laryngoscopes (VLs). Multiple studies have compared VL to direct laryngoscopy and the effects on success rates and factors surrounding intubation. However, in this study we aim to investigate the influence of VL on fiberoptic intubation, the previous gold standard for difficult airways.
Management of the difficult airway has traditionally relied on the difficult airway algorithm published by the American Society of Anesthesiologists. Given the ever-increasing clinical use of VL, it is important to assess if their introduction has affected the clinical practice of managing difficult airways, specifically in regards to awake fiberoptic intubation, part of the difficult airway algorithm.
In light of the introduction of VL, this study investigates whether or not the rate of awake fiberoptic intubation has decreased in the management of difficult airway. It is important to recognize the trends surrounding VL given that the frequency of use and level of training that anesthetists have with fiberoptic intubation may be influenced. If this were the case it would be important to acknowledge and address in the future.
Anesthetic records were reviewed at Rush University Medical Center before and after the introduction of video laryngoscopes to analyze the effects on awake fiberoptic intubation (FOI).
Awake FOI decreased from 13.1% before VL to 9% after video laryngoscopy (P = 0.1768 but trended toward significance). Morbid obesity (larger BMI P = 0.0154, OR = 1.5 per 10-point BMI increase), male gender (P = 0.0026, OR = 3.0), and higher el-Ganzouri score (P = 0.0007, OR = 1.5) predicted higher rates of awake FOI. VL was used to intubate 51% of predicted difficult airways, while use of direct laryngoscopy significantly decreased.
In light of increasing use of VL, fiberoptic intubation remains the gold standard for difficult airway intubation. It is important for patient safety that our specialty commit to train on multiple modalities of tracheal intubation in order to be prepared for the most difficult of airways. Continued study is required to assess trends in regards to VL vs fiberoptic intubation in difficult airways.
While a retrospective study has shed light on the fact that the rate of VL is clearly increasing, a randomized clinical trial could provide greater data on the outcomes of difficult airways given varying tracheal intubation methods. In addition, continual readdressing of VL use in difficult airways will aid in assessing whether or not it should be introduced into the difficult airway algorithm.
The authors would like to acknowledge the Department of Anesthesiology at Rush University Medical Center for support in conducting this study.
Manuscript source: Invited manuscript
Specialty type: Anesthesiology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): A, A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): E
P- Reviewer: Afzal DM, Ajmal M, Higa K, Mentes O, Spasojevic SD S- Editor: Cui LJ L- Editor: A E- Editor: Tan WW
| 1. | Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, Hagberg CA, Caplan RA, Benumof JL, Berry FA. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118:251-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1327] [Cited by in RCA: 1202] [Article Influence: 100.2] [Reference Citation Analysis (0)] |
| 2. | Serocki G, Bein B, Scholz J, Dörges V. Management of the predicted difficult airway: a comparison of conventional blade laryngoscopy with video-assisted blade laryngoscopy and the GlideScope. Eur J Anaesthesiol. 2010;27:24-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 95] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 3. | Malik MA, Subramaniam R, Maharaj CH, Harte BH, Laffey JG. Randomized controlled trial of the Pentax AWS, Glidescope, and Macintosh laryngoscopes in predicted difficult intubation. Br J Anaesth. 2009;103:761-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 109] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 4. | Jungbauer A, Schumann M, Brunkhorst V, Börgers A, Groeben H. Expected difficult tracheal intubation: a prospective comparison of direct laryngoscopy and video laryngoscopy in 200 patients. Br J Anaesth. 2009;102:546-550. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 118] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 5. | Enomoto Y, Asai T, Arai T, Kamishima K, Okuda Y. Pentax-AWS, a new videolaryngoscope, is more effective than the Macintosh laryngoscope for tracheal intubation in patients with restricted neck movements: a randomized comparative study. Br J Anaesth. 2008;100:544-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 120] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 6. | Aziz MF, Dillman D, Fu R, Brambrink AM. Comparative effectiveness of the C-MAC video laryngoscope versus direct laryngoscopy in the setting of the predicted difficult airway. Anesthesiology. 2012;116:629-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 233] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 7. | Lim Y, Yeo SW. A comparison of the GlideScope with the Macintosh laryngoscope for tracheal intubation in patients with simulated difficult airway. Anaesth Intensive Care. 2005;33:243-247. [PubMed] |
| 8. | Cohn AI, Zornow MH. Awake endotracheal intubation in patients with cervical spine disease: a comparison of the Bullard laryngoscope and the fiberoptic bronchoscope. Anesth Analg. 1995;81:1283-1286. [PubMed] |
| 9. | Ovassapian A, Krejcie TC, Yelich SJ, Dykes MH. Awake fibreoptic intubation in the patient at high risk of aspiration. Br J Anaesth. 1989;62:13-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 114] [Article Influence: 3.2] [Reference Citation Analysis (2)] |
| 10. | Reasoner DK, Warner DS, Todd MM, Hunt SW, Kirchner J. A comparison of anesthetic techniques for awake intubation in neurosurgical patients. J Neurosurg Anesthesiol. 1995;7:94-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 50] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 11. | el-Ganzouri AR, McCarthy RJ, Tuman KJ, Tanck EN, Ivankovich AD. Preoperative airway assessment: predictive value of a multivariate risk index. Anesth Analg. 1996;82:1197-1204. [PubMed] |
| 12. | Law JA, Morris IR, Brousseau PA, de la Ronde S, Milne AD. The incidence, success rate, and complications of awake tracheal intubation in 1,554 patients over 12 years: an historical cohort study. Can J Anaesth. 2015;62:736-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 68] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 13. | Ahmad I, Bailey CR. Time to abandon awake fibreoptic intubation? Anaesthesia. 2016;71:12-16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 54] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 14. | Mueller L. A Case Report from the Anesthesia Incident Reporting System. ASA Monitor. 2016;80:36-37. |
| 15. | Paton L, Gupta S, Blacoe D. Successful use of sugammadex in a 'can't ventilate' scenario. Anaesthesia. 2013;68:861-864. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Robitaille A, Williams SR, Tremblay MH, Guilbert F, Thériault M, Drolet P. Cervical spine motion during tracheal intubation with manual in-line stabilization: direct laryngoscopy versus GlideScope videolaryngoscopy. Anesth Analg. 2008;106:935-941, table of contents. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 104] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 17. | Turkstra TP, Craen RA, Pelz DM, Gelb AW. Cervical spine motion: a fluoroscopic comparison during intubation with lighted stylet, GlideScope, and Macintosh laryngoscope. Anesth Analg. 2005;101:910-915, table of contents. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 139] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 18. | Wong DM, Prabhu A, Chakraborty S, Tan G, Massicotte EM, Cooper R. Cervical spine motion during flexible bronchoscopy compared with the Lo-Pro GlideScope. Br J Anaesth. 2009;102:424-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Aziz MF, Healy D, Kheterpal S, Fu RF, Dillman D, Brambrink AM. Routine clinical practice effectiveness of the Glidescope in difficult airway management: an analysis of 2,004 Glidescope intubations, complications, and failures from two institutions. Anesthesiology. 2011;114:34-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 268] [Cited by in RCA: 251] [Article Influence: 17.9] [Reference Citation Analysis (0)] |
| 20. | Kheterpal S, Healy D, Aziz MF, Shanks AM, Freundlich RE, Linton F, Martin LD, Linton J, Epps JL, Fernandez-Bustamante A, Jameson LC, Tremper T, Tremper KK; Multicenter Perioperative Outcomes Group (MPOG) Perioperative Clinical Research Committee. Incidence, predictors, and outcome of difficult mask ventilation combined with difficult laryngoscopy: a report from the multicenter perioperative outcomes group. Anesthesiology. 2013;119:1360-1369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 210] [Cited by in RCA: 215] [Article Influence: 19.5] [Reference Citation Analysis (0)] |
| 21. | Cook TM, Woodall N, Frerk C; Fourth National Audit Project. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth. 2011;106:617-631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1171] [Cited by in RCA: 1240] [Article Influence: 88.6] [Reference Citation Analysis (1)] |