Peer-review started: November 4, 2017
First decision: December 27, 2017
Revised: January 4, 2018
Accepted: February 4, 2018
Article in press: February 5, 2018
Published online: March 18, 2018
Processing time: 132 Days and 12.4 Hours
To determine if ketamine sedation is a safe and cost effective way of treating displaced paediatric radial and ulna fractures in the emergency department.
Following an agreed interdepartmental protocol, fractures of the radius and ulna (moderately to severely displaced) in children between the age of 2 and 16 years old, presenting within a specified 4 mo period, were manipulated in our paediatric emergency department. Verbal and written consent was obtained prior to procedural sedation to ensure parents were informed and satisfied to have ketamine. A single attempt at manipulation was performed. Pre and post manipulation radiographs were requested and assessed to ensure adequacy of reduction. Parental satisfaction surveys were collected after the procedure to assess the perceived quality of treatment. After closed reduction and cast immobilisation, patients were then followed-up in the paediatric outpatient fracture clinic and functional outcomes measured prospectively. A cost analysis compared to more formal manipulation under a general anaesthetic was also undertaken.
During the 4 mo period of study, 10 closed, moderate to severely displaced fractures were identified and treated in the paediatric emergency department using our ketamine sedation protocol. These included fractures of the growth plate (3), fractures of both radius and ulna (6) and a single isolated proximal radius fracture. The mean time from administration of ketamine until completion of the moulded plaster was 20 min. The mean time interval from sedation to full recovery was 74 min. We had no cases of unacceptable fracture reduction and no patients required any further manipulation, either in fracture clinic or under a more formal general anaesthetic. There were no serious adverse events in relation to the use of ketamine. Parents, patients and clinicians reported extremely favourable outcomes using this technique. Furthermore, compared to using a manipulation under general anaesthesia, each case performed under ketamine sedation was associated with a saving of £1470, the overall study saving being £14700.
Ketamine procedural sedation in the paediatric population is a safe and cost effective method for the treatment of displaced fractures of the radius and ulna, with high parent satisfaction rates.
Core tip: Displaced paediatric forearm fractures can be safely and effectively treated in the emergency department with ketamine procedural sedation.
- Citation: Wiik AV, Patel P, Bovis J, Cowper A, Pastides PS, Hulme A, Evans S, Stewart C. Use of ketamine sedation for the management of displaced paediatric forearm fractures. World J Orthop 2018; 9(3): 50-57
- URL: https://www.wjgnet.com/2218-5836/full/v9/i3/50.htm
- DOI: https://dx.doi.org/10.5312/wjo.v9.i3.50
Fractures of the radius and ulna account for 18% to 40% of all fractures in children[1,2]. They are the most common childhood fracture presenting to the paediatric emergency department (ED), with population studies suggesting that the incidence is on the rise throughout the world[3,4]. The majority are treated in the ED with closed reduction and immobilisation in a cast or a splint[5,6]. An arc of rotation of 100 degrees, split evenly between pronation and supination is accepted as normal[7]. The goal of treatment is to restore appropriate length and alignment so normal forearm rotation can return after healing[8]. Simple closed reduction and temporary stable immobilisation is the standard of care sought for these fractures as they generally heal well and surgical fixation doesn’t come without risk[9]. The provision of closed reduction can be problematic as there are variations in treatment practice as result of hospital resources, local policy and experience[10,11]. Despite this, a safe and optimal level of analgesia should be achieved before manipulation to avoid unnecessary distress to the child and to ensure a favourable outcome[12]. Simple analgesia such as paracetamol and non-steroidal anti-inflammatory drugs, along with intra-nasal opiates and nitrous oxide may be sufficient and have been shown to be an effective treatment in the ED[13]. However formal ED procedural sedation is an attractive alternative as it offers a greater opportunity to deliver the optimal fracture reduction and cast application[11]. Sedation in the ED is particularly helpful if the fracture pattern is unstable and requires complex traction manoeuvres to achieve adequate correction[14]. Providing complete treatment in the ED and avoiding theatres would negate the economic and psychosocial impact on the child and family if they were admitted into hospital[15,16]. It also has been shown to be more cost-effective to society, which is important in times of economic austerity[17].
There are a variety of classes of procedural sedation drugs used in the United Kingdom[18]. The most popular include opiods, benzodiazapines, propofol and ketamine[18]. Ketamine is the only drug that does not routinely interfere with protective airway reflexes and spontaneous respiration[18]. Ketamine is also the most complete agent as it produces amnesia, anxiolysis and profound analgesia[19]. This drug was first used in humans in the 1960[20]. It was used extensively in the Vietnam war in the 1970s for surgical anaesthesia due to its good safety profile[21]. Its widespread application in paediatric procedural sedation was developed in the 1990s following the work of Green et al[22,23]. Over the last three decades it has become one of the most widely used sedative agents in the ED[24,25]. It acts as a dissociative agent that non-competitively blocks NDMA receptors[20]. Traditionally the dose required is 1-2 mg/kg, administered via slow intravenous infusion and can be combined with opiods and benzodiazepines[24].
The aim of this clinical practice study was to determine if ketamine is a safe and cost effective way of treating displaced fractures of the radius and ulna in children.
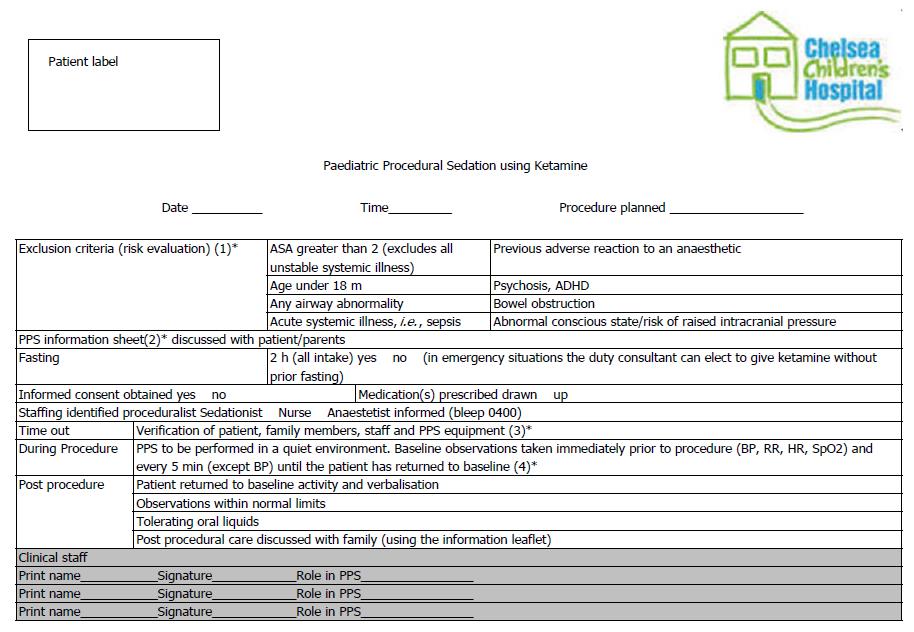
From May to September 2017, we prospectively evaluated a new ketamine protocol (Figure 1) for paediatric ED procedural sedation at Chelsea and Westminster Hospital (CWH). All eligible children with significantly displaced or unstable fractures of the radius and ulna who presented to CWH ED during daylight weekday hours that needed closed reduction and moulded casting were included. The service improvement project was registered locally (QIP# LA353) to follow good clinical governance practice guidelines.
Following triage all children presenting to CWH ED with a suspected fracture of the radius and ulna undergo orthogonal anterior-posterior and lateral radiography. The radiographs are then screened by an ED doctor or triage nurse; if significant malalignment is identified the on-call orthopaedic registrar is notified. If the fracture is deemed suitable for manipulation using sedation the orthopaedic registrar and paediatric ED specialist explain the procedure to the child and parent/legal guardian. Counselling is given prior to obtaining written consent to ensure that the family is happy with the proposed sedation plan. They are advised that other treatment options are available if they wish. The inclusion criteria is any child below the age of 16 years with a significantly displaced or unstable fracture of the radius and/or ulna. Plain radiographs are demonstrated as examples of the nature of these fractures. Exclusion criteria included open fractures, ASA greater than 2, under 18 mo of age, any airway abnormality, acute systemic illness, previous adverse anaesthetic reactions, raised intracranial pressure, and/or bowel obstruction.
Informed written consent is taken and final neurovascular assessment is documented. The weight of the child is measured before he or she is taken to a quiet room for ketamine sedation and closed reduction. The parent/legal guardian is given the option to stay with the child for support and comfort. The team consists of a paediatrician, a specialist ED trainee/consultant with ketamine sedation experience, and an orthopaedic registrar. Blood pressure, pulse, respiratory rate and oxygen saturation are monitored and recorded. An alert is sent to an anaesthetic consultant that the procedure is about to start in case of serious adverse event (SAE) occurs. A sedation checklist is completed.
To start 1 mg/kg of ketamine is given through a peripheral intravenous cannula normally in the antecubital fossa or dorsum of the hand of the contralateral upper limb. After a period of 3 min the child’s vitals are rechecked. If the child appears to be sedated a gentle manipulation is attempted. If they are not adequately sedated, a top-up of 0.5 mg/kg is administered. Manipulation is performed; when the position is deemed to be satisfactory a stockinette is placed over the arm followed by a thin layer of wool and a complete well moulded cast utilizing three point fixation. The level of the fracture determines the decision whether or not to extend the cast above the elbow.
Generally the child begins to wake after 20 min and is monitored until fully verbalising with normal observations. Radiographs are performed to ensure a satisfactory reduction and compared to the pre-injury images; these are presented at trauma meeting the following morning.
Patients are seen in a paediatric fracture clinic 1 and 2 wk after manipulation when further radiographs are performed. If alignment is maintained the child is reviewed 3-6 wk later for removal of cast and repeat radiographs. A comprehensive examination is performed at this stage particularly looking for any obvious deformity, range of motion and for clinical evidence of fracture union. If union is felt to be insufficient a cast may be re-applied or splint provided. The child is reviewed 4-6 wk later for a final check. At the point of cast removal advice is given to avoid contact sport for a period deemed appropriate to allow for the bone to strengthen in accordance to Wolff’s law[26].
All patient data was anonymised. All hospital medical record numbers were retained in the paediatric ED database. Patient demographics, site and nature of injury, time of procedure, sedation or reduction outcomes were documented. Consent forms were kept in the patient files. Pre and post reduction radiographs were taken from our departmental picture archiving and communication systems (PACS). Absolute angulation measurements were taken from the lateral radiographs using angle measuring tool (SECTRA) and measured by AW and PP. A repeated measure t-test was utilised to detect if a difference was made. A significance level was set to α = 0.005 due to small numbers. The results were then compared to the best available evidence regarding acceptable reduction parameters for different fracture levels of the forearm[7]. Parental satisfaction was assessed using a validated satisfaction score[27].
A total of 10 closed unilateral forearm fractures were included in the 4 mo time period. All ten were due to indirect trauma, the majority being due to a fall on an outstretched hand. There were 8 boys and 2 girls. The mean age was 8 years (range 2.2-14.5). There were 6 fractures on the left side and 4 fractures on the right side. There were no cases of compartment syndrome or neurovascular compromise. All children had successful procedural sedation. Two children required topping up to 1.5 mg/kg to achieve appropriate analgesia and sedation. There were no serious adverse events. Vomiting was the most common adverse event, seen in 3 children. All were treated definitively at time of injury and required no further manipulation. No patients were lost to follow-up and all patients reported excellent functional outcomes at discharge as guided by Price et al[28]. Figures 2-4 (A-D) demonstrate the variety of fracture types and fracture reduction result.
There were three Salter Harris II fractures of the distal radius, four fractures of the distal third of the radius and/or ulna, two fractures of the mid-shaft of the radius and/or ulna and one fracture of proximal third of the radius. The mean dorsal angulation prior to reduction was 45 degrees (range 17-80). The mean angulation after reduction was 6 degrees (0-15) an improvement that reached statistical significance (P < 0.001). Following reduction all fractures were within the parameters recommended by Noonan and Price as acceptable[7]. One patient had an over correction going from a 45 degrees dorsal angulation to 15 degrees of volar angulation, however there was no functional deficit at discharge.
The mean time from fracture diagnosis to sedation administration was 181 min (range 129-234). The mean time to completion of cast application was 20 min (range 7-35). The mean time from sedation to full recovery was 74 min (range 45-120). The mean interval between pre-reduction and post-reduction radiographs was 198 min (range 91-370 min). The mean length of stay in the ED department from arrival to discharge was 311 min (range 213-446).
In our trust the health resource group (HRG) code for general anaesthesia in paediatric theatres is £1620 per child. The cost for procedural sedation with ketamine in the paediatric ED was £150 per child. The cost of hospital inpatient admission was not calculated to give a fair comparison. The cost saving is £1470 per child without the addition of cost for admission and loss of earning to the parent/legal guardian if they had to stay with the child. The minimum total financial savings for these 10 children was £14700.
The validated sedation satisfaction score was out of 10, with 0 being not at all and 10 being very satisfied[27]. The mean satisfaction score for all questions was 9.6. The individual scores for each item is seen in Table 1. A score of 10 was the most common result for each questionnaire item.
| Questionnaire item | Mean | Range | Percent answering “10” |
| Preparation and instruction given | 9.86 | 9-10 | 85.7 |
| The care given by nurse pre-procedure | 9.43 | 8-10 | 71.4 |
| The care given by doctor pre-procedure | 9.86 | 9-10 | 85.7 |
| The suitability of environment | 9.57 | 8-10 | 71.4 |
| The experience of the child | 8.57 | 3-10 | 71.4 |
| The care given by the nurse post-procedure | 10 | 10 | 100 |
| The care given by doctor post-procedure | 9.86 | 9-10 | 85.7 |
| Overall parent satisfaction | 9.71 | 9-10 | 71.4 |
The use of ketamine for procedural sedation in the ED in the developed world is gaining popularity[19,24]. In the past few years there is a growing body of evidence supporting its use for successful procedural sedation with a good safety and efficacy profile[29,30]. Serious adverse events are low with the largest prospective cohort study to date reporting a 1.1% risk with no deaths in 6295 children. Vomiting (5.2%) and oxygen desaturation (5.6%) were the most common adverse event found in this multi-centre study[24]. With that risk being further reduced if no other sedatives, such as propofol or fentanyl, were used in conjunction. Earlier works by Green et al[31], support these findings as they found 3.9% of children having respiratory adverse events and 8.4% having vomiting. Furthermore they found that co-administering drugs (anticholinergics and benzodiazepines), which were to reduce the risk, in fact made them worse[31].
In our small study, we found no serious adverse events but three children had vomiting. High parental satisfaction scores in this pilot study demonstrate its acceptance amongst the families whose children had procedural sedation. All children had definitive reduction and stabilisation which resulted in an excellent functional outcome. This is contrary to a recent study comparing ketamine vs propofol for closed reduction of paediatric both bone forearm fractures which found 35% and 48% unacceptable alignment respectively at 4 wk[32]. However their institution used a splint unlike ours which used a completed moulded cast to maintain reduction. An explanation which they admittedly acknowledge[32]. This finding is supported by another recent study that found only 8.8% children had displaced to an unacceptable standard if a moulded cast was used[13]. An outcome which is impressive considering only Entonox and intra-nasal diamorphine was used for reduction analgesia[13]. Nevertheless our result reinforces the finding that ketamine can give effective pain relief and sedation to allow thorough manipulation that resulted in fractures that were reduced and immobilised appropriately. The only major disadvantage we found with ketamine in our paediatric ED was the length of stay which was longer than normal. It was 5 h and 11 min which is beyond our National Health Service 4-h target. A target which was met using Entonox and intranasal diamorphine with a mean time of 3 h and 51 min[13]. Still it is a parameter which can be improved as the greatest cause of lost time is administrative. Our mean result of 181 min to sedation from diagnosis of fracture could improve once this protocol becomes established as routine.
Like many studies, this study has limitations. Due to the range of forearm fracture types along with small numbers, we are unable to give clear fracture displacement cut-off guidelines to which should be safely managed in the ED. However a recent international multi-centre study survey sought to evaluate and establish the clinical practice of reducing paediatric forearm fractures[11]. The results of 111 paediatric ED physicians at 12 tertiary children hospitals found that ketamine was the most commonly (88%) and most frequently (55%) used procedural sedation agent followed by intranasal fentanyl and Entonox. The survey found that most ED physicians would tolerate a “no reduction required policy” for distal forearm fractures up to 20 degrees and 10 degrees for children less than 5 and 10 years old, respectively. It also indicated that majority of ED physicians would prefer fractures with obvious clinical deformity to be managed by the orthopaedic team in theatre due to lack of experience. The survey study also did not define a cut-off which was deemed unacceptable to be treated in the ED. However closely interpreting their survey results, the authors inferred from a clinical vignette with a 25 degree angulated fracture that 74% of physicians would treat that injury in the ED with procedural sedation. In our study we successfully treated fractures with a mean angulation of 45°. Another larger (100 children) study definitively treated 90% of forearm fractures with a mean of 28° of dorsal angulation in the ED with Entonox and intranasal diamorphine[13]. Our and the latter study, both utilised an interdepartmental protocol by which the ED physician gave the sedation and an orthopaedic doctor with fracture reduction experience managed the forearm. This may account for the success in both practical studies and the hesitancy found in the survey study of ED physicians to manipulate deformed fractures. Nonetheless the authors of this paper feel that most paediatric forearm fractures, irrespective of deformity angulation, can be treated in the ED as long as they feel that the fracture pattern is reducible and can be maintained for the duration of its healing.
Other weaknesses acknowledged include, the small number of patients and a lack of comparative procedural sedation agents, but as it was an audit of quality of improvement, the study had to be completed in a reasonable time for a single agent. However our prospective study design meant that we had good data uptake, capturing a variety of outcomes which validates its use in clinical practice. It also ensured a clear protocol, which meant that all children got the same method and delivery of care which makes analysis more robust in terms of reproducibility in everyday practice. Lastly our study demonstrated the success that can be achieved with a team effort using a variety of specialties and skillsets to deliver a service which at heart is at the benefit of the child and the family.
In conclusion, ketamine sedation for children is safe and cost-effective for treating displaced fractures of the radius and ulna, it is associated with a high level of satisfaction.
Children forearm fractures account for up to 40% of fractures that present to the emergency department (ED), majority which could be managed there.
This study improved the quality of care given to children with deformed forearm fractures in the ED.
The main aim of this quality improvement project was to determine if ketamine sedation is a safe and cost-effective way of treating deformed paediatric forearm fractures in the ED.
Over a set 4 mo period we prospectively evaluated a new ketamine protocol for paediatric ED procedural sedation. All eligible children with significantly displaced or unstable fractures of the radius and ulna that presented during daylight weekday hours that needed closed reduction and moulded casting were included.
A total of 10 forearm fractures with a mean 45° angulation deformity were definitively treated in the ED with ketamine procedural sedation. The cost saving was £1470 for each child compared if the patient was taken to theatre. Overall mean parental satisfaction was 9.6 out of 10.
Ketamine procedural sedation in the paediatric population is a safe and cost effective method for the treatment of displaced forearm fractures.
Majority of paediatric forearm fracture, irrespective of displacement, can be treated in the ED as long as the fracture pattern is reducible and can be maintained safely in a moulded cast for the duration of its healing.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Liu JY S- Editor: Wang JL L- Editor: A E- Editor: Li D
| 1. | Naranje SM, Erali RA, Warner WC Jr, Sawyer JR, Kelly DM. Epidemiology of Pediatric Fractures Presenting to Emergency Departments in the United States. J Pediatr Orthop. 2016;36:e45-e48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 246] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 2. | Rennie L, Court-Brown CM, Mok JY, Beattie TF. The epidemiology of fractures in children. Injury. 2007;38:913-922. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 336] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 3. | Mäyränpää MK, Mäkitie O, Kallio PE. Decreasing incidence and changing pattern of childhood fractures: A population-based study. J Bone Miner Res. 2010;25:2752-2759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 158] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 4. | Galano GJ, Vitale MA, Kessler MW, Hyman JE, Vitale MG. The most frequent traumatic orthopaedic injuries from a national pediatric inpatient population. J Pediatr Orthop. 2005;25:39-44. [PubMed] |
| 5. | Sinikumpu JJ, Victorzon S, Antila E, Pokka T, Serlo W. Nonoperatively treated forearm shaft fractures in children show good long-term recovery. Acta Orthop. 2014;85:620-625. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Jones K, Weiner DS. The management of forearm fractures in children: a plea for conservatism. J Pediatr Orthop. 1999;19:811-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 61] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Noonan KJ, Price CT. Forearm and distal radius fractures in children. J Am Acad Orthop Surg. 1998;6:146-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 178] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 8. | Pace JL. Pediatric and Adolescent Forearm Fractures: Current Controversies and Treatment Recommendations. J Am Acad Orthop Surg. 2016;24:780-788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 50] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 9. | Franklin CC, Robinson J, Noonan K, Flynn JM. Evidence-based medicine: management of pediatric forearm fractures. J Pediatr Orthop. 2012;32 Suppl 2:S131-S134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Meyer S, Grundmann U, Gottschling S, Kleinschmidt S, Gortner L. Sedation and analgesia for brief diagnostic and therapeutic procedures in children. Eur J Pediatr. 2007;166:291-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Schofield S, Schutz J, Babl FE; Paediatric Research in Emergency Departments International Collaborative (PREDICT). Procedural sedation and analgesia for reduction of distal forearm fractures in the paediatric emergency department: a clinical survey. Emerg Med Australas. 2013;25:241-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Drendel AL, Kelly BT, Ali S. Pain assessment for children: overcoming challenges and optimizing care. Pediatr Emerg Care. 2011;27:773-781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 121] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 13. | Kurien T, Price KR, Pearson RG, Dieppe C, Hunter JB. Manipulation and reduction of paediatric fractures of the distal radius and forearm using intranasal diamorphine and 50% oxygen and nitrous oxide in the emergency department: a 2.5-year study. Bone Joint J. 2016;98-B:131-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | McCarty EC, Mencio GA, Walker LA, Green NE. Ketamine sedation for the reduction of children’s fractures in the emergency department. J Bone Joint Surg Am. 2000;82-A:912-918. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 64] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Ben-Amitay G, Kosov I, Reiss A, Toren P, Yoran-Hegesh R, Kotler M, Mozes T. Is elective surgery traumatic for children and their parents? J Paediatr Child Health. 2006;42:618-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | Stargatt R, Davidson AJ, Huang GH, Czarnecki C, Gibson MA, Stewart SA, Jamsen K. A cohort study of the incidence and risk factors for negative behavior changes in children after general anesthesia. Paediatr Anaesth. 2006;16:846-859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Jordan RW, Aquilina A, Westacott DJ, Cooke S. A comparison of ketamine sedation and general anaesthesia for manipulation of paediatric forearm fractures. Acta Orthop Belg. 2016;82:836-842. [PubMed] |
| 18. | Atkinson P, French J, Nice CA. Procedural sedation and analgesia for adults in the emergency department. BMJ. 2014;348:g2965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Tobias JD, Leder M. Procedural sedation: A review of sedative agents, monitoring, and management of complications. Saudi J Anaesth. 2011;5:395-410. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 99] [Cited by in RCA: 127] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 20. | Kost S, Roy A. Procedural sedation and analgesia in the pediatric emergency department: A review of sedative pharmacology. Clinical Pediatric Emergency Medicine. 2010;11:233-243. [RCA] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Domino EF. Taming the ketamine tiger. 1965. Anesthesiology. 2010;113:678-684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 295] [Cited by in RCA: 356] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 22. | Green SM. The safety of ketamine for emergency department pediatric sedation. J Oral Maxillofac Surg. 1995;53:1232-1233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 23. | Green SM, Rothrock SG, Harris T, Hopkins GA, Garrett W, Sherwin T. Intravenous ketamine for pediatric sedation in the emergency department: safety profile with 156 cases. Acad Emerg Med. 1998;5:971-976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 131] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 24. | Bhatt M, Johnson DW, Chan J, Taljaard M, Barrowman N, Farion KJ, Ali S, Beno S, Dixon A, McTimoney CM, Dubrovsky AS, Sourial N, Roback MG; Sedation Safety Study Group of Pediatric Emergency Research Canada (PERC). Risk Factors for Adverse Events in Emergency Department Procedural Sedation for Children. JAMA Pediatr. 2017;171:957-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 97] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 25. | Sacchetti A, Stander E, Ferguson N, Maniar G, Valko P. Pediatric Procedural Sedation in the Community Emergency Department: results from the ProSCED registry. Pediatr Emerg Care. 2007;23:218-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 51] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 26. | Wolff J. The classic: on the inner architecture of bones and its importance for bone growth. 1870. Clin Orthop Relat Res. 2010;468:1056-1065. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 93] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 27. | Lew VK, Lalwani K, Palermo TM. Factors affecting parental satisfaction following pediatric procedural sedation. J Clin Anesth. 2010;22:29-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 28. | Price CT, Scott DS, Kurzner ME, Flynn JC. Malunited forearm fractures in children. J Pediatr Orthop. 1990;10:705-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 159] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 29. | Vardy JM, Dignon N, Mukherjee N, Sami DM, Balachandran G, Taylor S. Audit of the safety and effectiveness of ketamine for procedural sedation in the emergency department. Emerg Med J. 2008;25:579-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 30. | Kidd LR, Lyons SC, Lloyd G. Paediatric procedural sedation using ketamine in a UK emergency department: a 7 year review of practice. Br J Anaesth. 2016;116:518-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 31. | Green SM, Roback MG, Krauss B, Brown L, McGlone RG, Agrawal D, McKee M, Weiss M, Pitetti RD, Hostetler MA. Predictors of airway and respiratory adverse events with ketamine sedation in the emergency department: an individual-patient data meta-analysis of 8,282 children. Ann Emerg Med. 2009;54:158-168.e1-4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 168] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 32. | Morrison T, Carender C, Kilbane B, Liu RW. Procedural Sedation With Ketamine Versus Propofol for Closed Reduction of Pediatric Both Bone Forearm Fractures. Orthopedics. 2017;40:288-294. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |