Published online Nov 18, 2018. doi: 10.5312/wjo.v9.i11.262
Peer-review started: July 2, 2018
First decision: July 18, 2018
Revised: September 9, 2018
Accepted: October 23, 2018
Article in press: October 23, 2018
Published online: November 18, 2018
Processing time: 138 Days and 10.8 Hours
To explore the current evidence surrounding the administration of prophylactic antibiotics for arthroscopic knee surgery.
Databases were searched from inception through May of 2018 for studies examining prophylactic antibiotic use and efficacy in knee arthroscopy. Studies with patient data were further assessed for types of arthroscopic procedures performed, number of patients in the study, use of antibiotics, and outcomes with the intention of performing a pooled analysis. Data pertaining to “deep tissue infection” or “septic arthritis” were included in our analysis. Reported data on superficial infection were not included in our data analysis. For the pooled analysis, a relative risk ratio was calculated and χ2 tests were used to assess for statistical significance between rates of infection amongst the various patient groups. Post hoc power analyses were performed to compute the statistical power obtained from our sample sizes. Number needed to treat analyses were performed for statistically significant differences by dividing 1 by the difference between the infection rates of the antibiotic and no antibiotic groups. An alpha value of 0.05 was used for our analysis. Study heterogeneity was assessed by Cochrane’s Q test as well as calculation of the I2 value.
A total of 49682 patients who underwent knee arthroscopy for a diverse set of procedures across 19 studies met inclusion critera for pooled analysis. For those not undergoing graft procedures, there were 27 cases of post-operative septic arthritis in 34487 patients (0.08%) who received prophylactic antibiotics and 16 cases in 10911 (0.15%) who received none [risk ratio (RR) = 0.53, 95% confidence interval (CI): 0.29-0.99, P = 0.05]. A sub-group analysis in which bony procedures were excluded was performed which found no significant difference in infection rates between patients that received prophylactic antibiotics and patients that did not (P > 0.05). All anterior cruciate ligament reconstruction studies used prophylactic antibiotics, but two studies investigating the effect of soaking the graft in vancomycin in addition to standard intravenous (IV) prophylaxis were combined for analysis. There were 19 cases in 1095 patients (1.74%) who received IV antibioitics alone and no infections in 2034 patients who received IV antibiotics and had a vancomycin soaked graft (RR = 0.01, 95%CI: 0.001-0.229, P < 0.01).
Prophylactic antibiotics are effective in preventing septic arthritis following simple knee arthroscopy. In procedures involving graft implantation, graft soaking reduces the rate of infection.
Core tip: Our study is the first to demonstrate prophylactic antibiotics are effective in preventing septic arthritis following simple arthroscopic procedures of the knee, though given the large number needed to treat, the clinical significance of this finding is unclear. There is little to no debate that antibiotics should be used prophylactically for arthroscopic surgeries involving graft implantation. However, our findings indicate that the addition of graft soaking further reduces the rate of infection. Further study is warranted to identify patient populations and arthroscopic procedures in which the use of prophylactic antibiotics may not be necessary.
- Citation: Carney J, Heckmann N, Mayer EN, Alluri RK, Jr. CTV, III GFH, Weber AE. Should antibiotics be administered before arthroscopic knee surgery? A systematic review of the literature. World J Orthop 2018; 9(11): 262-270
- URL: https://www.wjgnet.com/2218-5836/full/v9/i11/262.htm
- DOI: https://dx.doi.org/10.5312/wjo.v9.i11.262
Antibiotics have been administered prophylactically in major orthopaedic surgeries for decades[1]. Their use has been shown to reduce rates of local and systemic infection, which leads to better patient outcomes when used in combination with proper sterile surgical technique[2]. Failure to provide adequate infection prophylaxis prior to elective knee arthroscopy may result in septic arthritis, a devastating complication which has been shown to delay recovery time and diminish functional outcomes[3]. The most common pathogen responsible for septic arthritis is Staphylococcus aureus; though other pathogens have been identified as well[4,5]. It is accepted within the orthopaedic community that prophylactic antibiotics, typically cephalosporins or vancomycin, should be administered prior to major orthopaedic surgeries[6]. However, the use of routine prophylactic antibiotics prior to less invasive surgeries such as hand procedures and elective arthroscopic surgeries has not been established. The wide range of rates of antibiotic administration in the published literature, ranging from as low as 5% to as high as 80.5%, highlights the lack of understanding of the role of antibiotic prophylaxis[7-13]. The use of prophylactic antibiotics is not without risk; allergic reaction, development of resistant organisms, and side effects specific to the chosen antibiotic can be a burden to patients and health care providers alike.
There is published data that demonstrate that prophylactic antibiotics may be unnecessary for minimally invasive non-bony procedures such as carpal tunnel release[14]. As of 2009, the American Acadamy of Orthopedic Surgeons published guidelines on carpal tunnel release that did not mandate the use of prophylactic antibiotics, but rather stated their use was an option for physicians to consider[14]. There is evidence to suggest that, like carpal tunnel release, patients undergoing knee arthroscopy may recieve little to no benefit from receiving prophylactic antibiotics. A recent study by Wyatt et al[8] found no significant difference in cases of deep infection between patients that received prophylactic antibioitics prior to knee arthroscopy and those who did not in a study that included 40810 patients. This study is in agreement with other studies on this topic, which similarly found no difference in infection rates if prophylactic antibiotics are used or withheld[7,12,15-17]. Although the study by Wyatt et al[8] contained large cohort of patients, other studies are relatively small and may be too underpowered to draw meaningful conclusions.
The purpose of this systematic review is to summarize current literature with regards to the efficacy of antibiotic prophylaxis in arthroscopic knee surgery and to pool available studies to better determine the true infection risk in knee arthroscopy. This study is the first to our knowledge that attempts to combine data from published studies to better understand the role of antibiotic prophylaxis in knee arthroscopy. We hypothesize that there is no evidence to support the routine administration of prophylactic antibiotics in arthroscopic knee surgery.
Two reviewers completed a comprehensive search of PubMed, MEDLINE, and Web of Science to identify studies pertaining to the use of antibiotic prophylaxis in knee arthroscopy from inception to May of 2018. Search strategies were customized for each database to produce the highest yield of possible results (Appendix A). Randomized control trials, prospective and retrospective studies, case-control studies, and systematic reviews were included. Review articles and surveys discussing the use of prophylactic antibiotics in arthroscopy were excluded from use in a pooled analysis, but were included for discussion purposes. Case reports, animal studies, and cadaveric studies were also excluded. The references of each study were also assessed for eligibility for our review. Studies with patient data were further assessed for types of arthroscopic procedures performed, number of patients in the study, use of antibiotics, and outcomes with the intention of performing a pooled analysis. Data pertaining to “deep tissue infection” or “septic arthritis” were included in our analysis. Reported data on superficial infection were not included in our data analysis.
For the pooled analysis, a relative risk ratio was calculated and χ2 tests were used to assess for statistical significance between rates of infection amongst the various patient groups. Post hoc power analyses were performed to compute the statistical power obtained from our sample sizes. Number needed to treat analyses were performed for statistically significant differences by dividing 1 by the difference between the infection rates of the antibiotic and no antibiotic groups. An alpha value of 0.05 was used for our analysis. Study heterogeneity was assessed by Cochrane’s Q test as well as calculation of the I2 value.
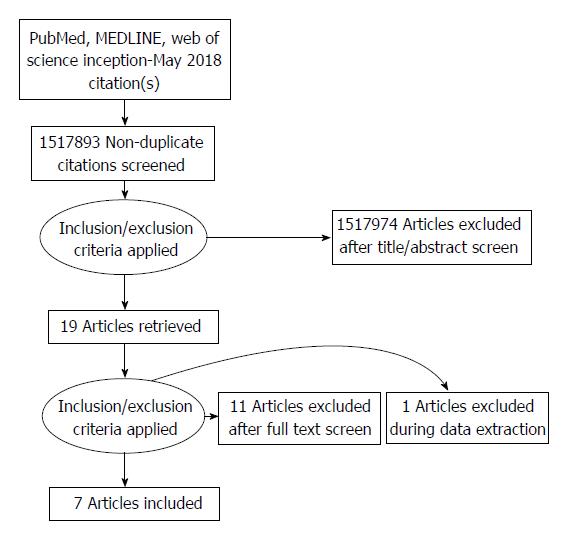
Our initial search yielded 1517893 studies. Nineteen studies satisfied inclusion criteria: 3 randomized control trials, 7 retrospective case control studies, 4 retrospective case series studies, 2 surveys, and 4 review articles (Table 1). These studies were further analyzed to determine if their data could be pooled for further analysis. Studies with data comparing infectious outcomes in knee arthroscopy procedures between groups that received prophylaxis and those that did not were included in our grouped analysis while studies with data not specific to the knee joint or not limited to arthroscopy were excluded.
| Study name | Study type | No. of Patients | Procedures done | Findings/results/conclusions |
| Wyatt et al[8] | Retrospective Review | 40810 | Diagnostic arthroscopy, joint debridement, synovectomy, partial or complete meniscectomy, meniscus repair, microfracture, and lateral retinacular release | No significant difference in infection rates between prophylaxis and non-prophylaxis groups |
| Bert et al[7] | Retrospective Review | 3231 | Arthroscopic meniscectomy, arthroscopic meniscal repair, loose body removal, lateral retinacular release, and arthroscopic debridement | No significant difference in infection rates between prophylaxis and non-prophylaxis groups |
| Qi et al[17] | Retrospective Review | 1326 | Arthroscopic diagnosis, debridement, partial or complete meniscectomy, arthroscopic shaving and microfracture, removal of loose bodies, synovectomy and lateral retinacular release | No significant difference in infection rates between prophylaxis and non-prophylaxis groups |
| Ghnmait et al[15] | Randomized control trial | 180 | Diagnostic arthroscopy, meniscus repair | No significant difference in infection rates between prophylaxis and non-prophylaxis groups |
| Rose et al[12] | Retrospective Review | 302 | Meniscectomies, arthroscopic debridement, arthroscopic meniscal repair, arthroscopic shaving and microfracture, removal of loose bodies, arthroscopic synovectomy, arthroscopic lateral retinacular release and diagnostic arthroscopic | No significant difference in infection rates between prophylaxis and non-prophylaxis groups |
| Wieck et al[16] | Randomized control trial | 437 | Unspecified arthroscopy | No significant difference in infection rates between prophylaxis and non-prophylaxis groups |
| Phegan et al[18] | Retrospective Review | 1585 | ACL reconstruction with graft | Vancomycin soaked grafts have a lower infection rate than non-soaked grafts |
| Vertullo et al[19] | Retrospective Review | 1135 | ACL reconstruction with graft | Vancomycin soaked grafts have a lower infection rate than non-soaked grafts |
| Pérez-Prieto et al[22] | Retrospective Review | 1544 | ACL reconstruction with graft | Vancomycin soaked grafts have a lower infection rate than non-soaked grafts |
| Yazdi et al[31] | Randomized control trial | 360 | ACL reconstruction with graft | Using gentamicin in irrigating solutions during arthroscopic ACL reconstruction surgery does not statistically decrease post-operation septic arthritis |
| Formaini et al[10] | Retrospective Review | 2330 | Unspecified arthroscopy | No significant difference in infection rates between prophylaxis and non-prophylaxis groups |
| Armstrong et al[11] | Retrospective Review | 4256 | Unspecified arthroscopy | Infection following knee arthroscopy was associated with prolonged operation time and corticosteroid use, not presence or absence of prophylactic antibiotics |
| D'Angelo and Ogilvie-Harris[26] | Retrospective Review | 9 | Unspecified arthroscopy | Antibiotic prophylaxis may reduce hospital costs by reducing spending on treating septic arthritis based on a 9 case review of patients with septic arthritis following arthroscopy |
| Babcock et al[23] | Retrospective Review | 27 | Unspecified arthroscopy | In a case series review of septic arthitis patients, shaving and corticosteriods were found to be significant risk factors, but not antibiotics |
| Lubowitz et al[25] | Review Article | NA | NA | There is not enough evidence to conclude whether or not antibiotics should be administered prophylactically in knee arthroscopy. However, the results of articles like Bert et al should be further examined and studied |
| Kurzweill[27] | Review Article | NA | NA | There is not enough evidence to conclude whether or not antibiotics should be administered prophylactically in knee arthroscopy. However, they should still be used as a measure to reduce the risk of post procedure infection |
| Onyema et al[24] | Review Article | NA | NA | Prophylactic antibiotics should not be used for knee arthroscopy |
| Prokuski[6] | Review Article | NA | NA | Cephalosporins are the drug of choice for most orthopedic surgeries. However, there is a lack of evidence supporting their efficacy in arthroscopic surgery |
| Müller-Rath et al [9] | Survey | 110 physicians | NA | 62 % of the surgeons reported the use of an antibiotic prophylaxis in every arthroscopic case, while 19 % administer antibiotics only occasionally |
| Mini et al [13] | Survey | 166 hospitals | NA | 57.1% of orthopedic surgeons routinely use antibiotic prophylaxis for arthroscopy |
Eight studies met inclusion criteria for pooled analysis. Upon closer review however, it was determined that two studies likely utilized the same patient database to achieve their results[18,19]. We established correspondence with one of the authors to confirm this finding. Upon confirmation the more recent and higher powered of the two was included while the other was excluded from data analysis, leaving 7 studies for pooled analysis (Figure 1). From these studies, there were a total of 49682 patients who underwent an arthroscopic procedure. Arthroscopic procedures included diagnostic arthroscopy, joint debridement, synovectomy, partial or complete meniscectomy, meniscus repair, microfracture repair, lateral retinacular release, loose body removal, and anterior cruciate ligament reconstruction.
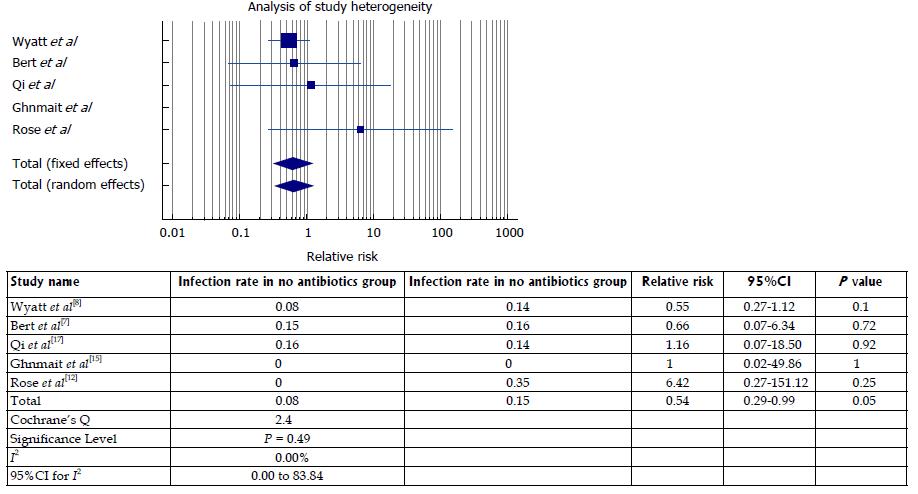
Five of the 7 studies had similar designs that allowed us to perform a pooled analysis of prophylactic antibiotic efficacy in arthroscopic procedures that do not involve the implantation of a graft (Table 2)[7,8,12,15,17]. Out of a total of 45398 patients, 34487 received prophylactic antibiotics prior to arthroscopy while 10991 did not. All authors used a first generation cephalosporin such as cefazolin for primary prophylaxis, except in cases of known drug allergy. The antibiotic group had a total of 27 cases of septic arthritis (0.08%) while the no antibiotic group had 16 cases of septic arthritis (0.15%). The differences in infection rates was found to be significant [risk ratio (RR) = 0.53, 95% confidence interval (CI): 0.29 to 0.99, P = 0.05, post hoc power = 53%]. Based on these findings, the number of patients needed to treat with IV antibiotics in order to prevent 1 infection is 1463.
| Study name | Total patients | Patients receiving antibiotics | Patients not receiving antibiotics | No. of septic arthritis cases: Antibiotic group | No. of septic arthritis cases: No antibiotic group | Septic arthritis: Antibiotic group (%) | Septic arthritis rate: No antibiotic group (%) | P valuea |
| Wyatt et al[8] | 40810 | 32836 | 7974 | 25 | 11 | 0.08 | 0.14 | |
| Bert et al[7] | 2780 | 933 | 1847 | 1 | 3 | 0.15 | 0.16 | |
| Qi et al[17] | 1326 | 614 | 712 | 1 | 1 | 0.16 | 0.14 | |
| Ghnmait et al[15] | 180 | 90 | 90 | 0 | 0 | 0 | 0 | |
| Rose et al[12] | 302 | 14 | 288 | 0 | 1 | 0 | 0.35 | |
| Total | 45398 | 34487 | 10911 | 27 | 16 | 0.08 | 0.15 | 0.05 |
Regarding study heterogeneity, the Cochrane Q value was calculated to be 2.40 (P = 0.49) while the I2 value was calculated to be 0% (95%CI: 0.00 to 83.11). Study heterogeneity is illustrated in Figure 2.
A subgroup analysis of this group was conducted and excluded studies that involved bony procedures (microfracture repair, procedures requiring bone tunnels, etc.), which have been demonstrated to have an increased risk of infection[20,21]. Two studies excluded bony procedures and were included in a separate analysis (Table 3)[7,15]. A study by Bert et al[7] examined 3231 patients undergoing various arthroscopic procedures, and analyzed meniscectomies separately, of which 933 (34%) received antibiotic prophylaxis and 1847 (66%) did not. A second study by Ghnaimat et al[15] randomized 180 patients undergoing either partial menisectomy, plica excision, synovial biopsy, or diagnostic arthroscopy into two groups, of which 90 (50%) received antibiotic prophylaxis and 90 (50%) did not. From a total of 2960 patients, 1023 (35%) receieved antibiotics and 1937 (65%) did not. There was 1 (0.10%) case of septic arthritis in the antibiotic group and 3 (0.15%) cases of septic arthritis in the group that did not recieve antibiotics, however this difference was not statistically significant (RR = 0.63, 95%CI: 0.07 to 6.06, P = 0.69, post hoc power = 5%).
| Study name | Total patients | Patients receiving antibiotics | Patients not receiving antibiotics | No. of septic arthritis cases: Antibiotic group | No. of septic arthritis cases: No antibiotic group | Septic arthritis rate: Antibiotic group (%) | Septic arthritis rate: No antibiotic group (%) | P valuea |
| Bert et al[7] | 2780 | 933 | 1847 | 1 | 3 | 0.11 | 0.16 | |
| Ghnmait et al[15] | 180 | 90 | 90 | 0 | 0 | 0 | 0 | |
| Total | 2960 | 1023 | 1937 | 1 | 3 | 0.1 | 0.15 | 0.69 |
Two of the 7 studies were pooled for data analysis to analyze arthroscopic anterior cruciate ligament (ACL) reconstruction (Table 4)[18,22]. Both studies investigated the role of soaking the ACL autograft in vancomycin prior to implantation. Of 3129 patients, 1095 received intravenous (IV) antibiotics alone prior to arthroscopic ACL reconstruction, while 2034 patients received IV antibiotics and had their ACL graft soaked in vancomycin. There were 19 cases of infection in the IV antibiotics alone group (1.74%) and 0 infections in the IV antibiotics with vancomycin soaked graft group (0%). The difference in rates was found to be significant (RR = 0.01, 95%CI: 0.001 to 0.229, P < 0.01, post hoc power = 99.8%). Given these infection rates, the number need to treat with vancomycin soaked grafts to prevent 1 infection is 57.0. Analysis of heterogeneity was not performed in this dataset given the rates of infection in treatment groups were equal at 0%.
| Study name | Total patients | IV prophylaxis alone | IV prophylaxis + vancomycin | Number infected IV alone | Number infected IV + vancomycin | Infection rate IV alone (%) | Infection rate IV + vancomycin (%) | P valuea |
| Phegan et al[18] | 1585 | 285 | 1300 | 4 | 0 | 1.4 | 0 | |
| Pérez-Prieto et al[22] | 1544 | 810 | 734 | 15 | 0 | 1.85 | 0 | |
| Total | 3129 | 1095 | 2034 | 19 | 0 | 1.74 | 0 | < 0.001 |
The results of our systematic review demonstrate that there is evidence supporting the use of prophylactic antibiotics in knee arthroscopic procedures to prevent postoperative infections (P = 0.05). The statistical significance may be attributed to knee arthroscopic procedures in which the subchondral bone is manipulated. Given the post hoc power analyses of our general population as well as our bone manipulation subgroup (53% and 5%, respectively), our findings should not be interpreted as a definitive answer to the question of whether antibiotic prophylaxis is appropriate in knee arthroscopy not involving a graft. However, in cases of graft implantation, particularly ACL autograft reconstruction, antibiotics appear to have a substantial protective effect particularly when antibiotics are used both locally (i.e., autograft soaked in vancomycin) and systemically. Furthermore, while our findings for the pooled group were statistically significant, the clinical utility of these differences is in question as reflected by the needed to treat of approximately 1400 patients.
The findings of this systematic review are in juxtaposition with current literature on this subject. A study by Babcock et al[23] investigated an outbreak of septic arthritis following arthroscopy at a community hospital from 1994 to 1996. The study concluded that preoperative skin shaving and intra-articular corticosteroid injection significantly increased risk of infection, but found no link between infection and use of prophylactic antibiotics. A review of 4256 knee arthroscopies with 15% receiving prophylactic antibiotics by Armstrong et al[11] similarly found that antibiotic use was not linked to a lower infection rate. Rather, corticosteroid use and prolonged operation time were the two greatest risk factors.
Our literature search found five studies of similar design that did not include the use of a graft and could be pooled for analysis. This pooled analysis demonstrated that there was a significant difference in infection rates between knee arthroscopy patients who received antibiotics and those who did not. Of these five studies, Wyatt et al[8] was substantially larger in size (n = 40810) than the others, and thus our results are largely dominated by the findings of this study. Although they concluded that there was no difference in infection rate, they reported a P value that approached statistical significance (P = 0.10). Pooling their cases with those of the other studies was able to tip the scale towards significance and show that there is a differencein infection rate between those that do and do not receive prophylactic antibiotics.
Regarding the rigour of these studies, we feel confident in the results as investigation of infection rates was the primary focus of each study. Furthermore, each study analyzed similar patient groups and used similar methods of antibiotic prophylaxis (cephalosporins) that are consistent with contemporary guidelines. Our analysis of study hetrogenity confirms that the findings amongst studies are consistent (I2: 0.00%). Thus, we believe the results of this systematic review to be both accurate and applicable to current orthopaedic practice.
There were other studies identified during our search that were excluded from our pooled analysis, but are worth mentioning in regards to our findings. Wieck et al[16] investigated the role of antibiotic prophylaxis in 437 patients who underwent an arthroscopic procedure, not limited to the knee, and found no cases of deep infection in either arm of their study. A retrospective study of pediatric patients undergoing minimally invasive orthopedic procedures, including arthroscopy, by Formaini et al[10] found no evidence to suggest that antibiotic prophylaxis reduced infection rates. Review articles by Onyema et al[24], Lubowitz et al[25], and Prokuski[6] all highlighted the lack of evidence with regards to prophylactic antibiotic administration in arthroscopy and noted that their use may not be necessary. Our review differs from the aforementioned articles in that we reviewed new literature as well as included our own data analysis, which provided a large enough population size to show significant differences in infection rates. Our study is the first to our knowledge to demonstrate the efficacy of prophylaxis at the alpha = 0.05 level. Thus, we emphasize the need for further study and confirmation of our findings before they can be translated into clinical practice.
There were two publications identified that recommended prophylactic antibiotics and thus are in agreement with our findings. One was a retrospective review of septic arthritis cases following arthroscopy by D’Angelo and Ogilvie-Harris[26] in which the authors recommended that prophylaxis be used to prevent deep tissue infections. However, the authors’ rationale for the efficacy of antibiotic prophylaxis in arthroscopy is based on a paper on general orthopedic surgeries, not arthroscopy[1]. A 2006 opinion article by Kurzweil[27] argued that although current evidence does not demonstrate the efficacy of antibiotic prophylaxis in knee arthroscopy, there is still not enough evidence to argue for its discontinuation. Kurzweil[27] stated that although a perfectly performed arthroscopic procedure on a healthy patient may not be affected by the use of antibiotics, they may serve as a safety net for physician errors or breaks in protocol as well as both known and unknown health-related risk factors of patients. Despite our significant findings, we agree that more evidence is needed to better understand the role of antibiotic prophylaxis in arthroscopy before a strong recommendation for or against their use can be made.
After a review of the literature, we determined that ACL reconstruction needed to be considered separate from other arthroscopic procedures, as our search did not yield any publications related to ACL reconstruction that did not use antibiotic prophylaxis. Rather, studies varied in the type of antibiotic prophylaxis utilized. In arthroscopic ACL reconstruction, the graft presents additional infection risk as it is inserted into the joint space from the outside environment. It has been demonstrated that the source of infection can come from direct contamination of the graft or from skin flora[28].
A 2013 study by Torres-Claramunt et al[29] found an infection rate of 1.8% following ACL reconstruction with prophylactic administration of either cefazolin or vancomycin. However, three retrospective reviews found significantly reduced rates of septic arthritis when ACL grafts were soaked in vancomycin prior to insertion into the joint space[18,19,22]. Our combined analysis of two of these studies strengthens these authors’ individual findings. It is particularly important to note that in all three of these studies the infection rate was reduced to 0%. This highlights the important role of local prophylactic antibiotics during ligament reconstruction, which has been demonstrated in other orthopaedic procedures[30]. An alternative method of irrigating knee joints with a solution containing gentamycin was tested in a randomized control trial by Yazdi et al[31], but found to have no significant impact on infection rates.
The main weakness of this systematic review was the small number of studies that directly compared patients receiving antibiotic prophylaxis in arthroscopy to controls. Also, even in simple arthroscopic procedures without grafts, there may be many variations that affect infection risk (e.g., type of meniscal repair, whether additional incisions were made as in for an inside-out approach, etc.). Furthermore, our findings with regards to simple arthroscopy are largely dominated by one study. Three of the four studies used in the pooled analysis were multi-surgeon retrospective cohort studies and critera for determining which patients received prophylactic antibiotics was left to individual surgeon discretion. The controlled trial performed by Ghnaimat et al[16] only semi-randomized antibiotic prophylaxis by allotting according to admission number (even admission numbers received antibiotics). Additional studies are needed to better understand the role antibiotic prophylaxis plays in the development of septic arthritis. Being able to identify procedures and patient groups that do not require antibiotic prophylaxis offers the potential to reduce hospital costs, reduce the risk of allergic reaction to medication, and slow the development of drug resistant organisms. Thus, further study of this topic is warranted.
Our study is the first to demonstrate prophylactic antibiotics are effective in preventing septic arthritis following simple arthroscopic procedures of the knee, though given the large number needed to treat, the clinical significance of this finding is unclear. Our findings regarding the addition of graft soaking indicate that further steps can be taken to reduce the rate of infection in procedures involving graft implantation. Further studies are needed to better understand when withholding prophylaxis may be appropriate.
The administration of prophylactis antibiotics prior to knee arthroscopy is a common practice in the orthopaedic community.
There are no studies to date that demonstrate that the use of antibiotic prophylaxis in arthroscopic surgery of the knee is effective.
The purpose of this study is to analyze the literature on the effect on antibioitic prophylaxis in knee arthroscopy on rates of septic arthritis.
We conducted a literature review of PubMed, MEDLINE, and Web of Science from inception to May of 2018. Data from studies meeting inclusion criteria were pooled for analysis. Risk-ratios were calculated to determine the effect of antibiotic prophylaxis on rates of septic arthritis in knee arthroscopy.
Nineteen studies met inclusion critera for pooled analysis. For those not undergoing graft procedures, there were 27 cases of post-operative septic arthritis in 34487 patients (0.08%) who received prophylactic antibiotics and 16 cases in 10911 (0.15%) who received none [risk ratio (RR) = 0.53, 95% confidence interval (CI): 0.29-0.99, P = 0.05]. A sub-group analysis in which bony procedures were excluded was performed which found no significant difference in infection rates between patients that received prophylactic antibiotics and patients that did not (P > 0.05). All ACL reconstruction studies used prophylactic antibiotics, but two studies investigating the effect of soaking the graft in vancomycin in addition to standard intravenous (IV) prophylaxis were combined for analysis. There were 19 cases in 1095 patients (1.74%) who received IV antibioitics alone and no infections in 2,034 patients who received IV antibiotics and had a vancomycin soaked graft (RR = 0.01, 95%CI: 0.001-0.229, P < 0.01).
Our study is the first to demonstrate prophylactic antibiotics are effective in preventing septic arthritis following simple arthroscopic procedures of the knee, though given the large number needed to treat, the clinical significance of this finding is unclear. Our literature search demonstrates that there is little to no debate that antibiotics should be used prophylactically for arthroscopic surgeries involving graft implantation. However, our findings indicate that the addition of graft soaking further reduces the rate of infection.
Further prospective studies on this topic will help further elucidate this conclusion.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Elfering A, Hernandez-Sanchez S, Li JM, Robertson GAJ S- Editor: Ji FF L- Editor: A E- Editor: Wu YXJ
| 1. | Elson RA. Clean Air Operating Environment and Superficial Infection. In: Uhthoff H.K., Stahl E (eds). Current Concepts of Infections in Orthopedic Surgery. Springer, Berlin, Heidelberg 1985; 33-37. [DOI] [Full Text] |
| 2. | Bryson DJ, Morris DL, Shivji FS, Rollins KR, Snape S, Ollivere BJ. Antibiotic prophylaxis in orthopaedic surgery: difficult decisions in an era of evolving antibiotic resistance. Bone Joint J. 2016;98-B:1014-1019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 66] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 3. | Boström Windhamre H, Mikkelsen C, Forssblad M, Willberg L. Postoperative septic arthritis after anterior cruciate ligament reconstruction: does it affect the outcome? A retrospective controlled study. Arthroscopy. 2014;30:1100-1109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 4. | Helito CP, Noffs GG, Pecora JR, Gobbi RG, Tirico LE, Lima AL, de Oliveira PR, Camanho GL. Epidemiology of septic arthritis of the knee at Hospital das Clínicas, Universidade de São Paulo. Braz J Infect Dis. 2014;18:28-33. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Lim SY, Pannikath D, Nugent K. A retrospective study of septic arthritis in a tertiary hospital in West Texas with high rates of methicillin-resistant Staphylococcus aureus infection. Rheumatol Int. 2015;35:1251-1256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Prokuski L. Prophylactic antibiotics in orthopaedic surgery. J Am Acad Orthop Surg. 2008;16:283-293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 175] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 7. | Bert JM, Giannini D, Nace L. Antibiotic prophylaxis for arthroscopy of the knee: is it necessary? Arthroscopy. 2007;23:4-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 41] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Wyatt RWB, Maletis GB, Lyon LL, Schwalbe J, Avins AL. Efficacy of Prophylactic Antibiotics in Simple Knee Arthroscopy. Arthroscopy. 2017;33:157-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Müller-Rath R, Ingenhoven E, Mumme T, Schumacher M, Miltner O. [Perioperative management in outpatient arthroscopy of the knee joint]. Z Orthop Unfall. 2010;148:282-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Formaini N, Jacob P, Willis L, Kean JR. Evaluating the use of preoperative antibiotics in pediatric orthopaedic surgery. J Pediatr Orthop. 2012;32:737-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Armstrong RW, Bolding F, Joseph R. Septic arthritis following arthroscopy: clinical syndromes and analysis of risk factors. Arthroscopy. 1992;8:213-223. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 146] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Uhl GR, Liu QR, Drgon T, Johnson C, Walther D, Rose JE. Molecular genetics of nicotine dependence and abstinence: whole genome association using 520,000 SNPs. BMC Genet. 2007;8:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 122] [Cited by in RCA: 117] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 13. | Mini E, Grassi F, Cherubino P, Nobili S, Periti P. Preliminary results of a survey of the use of antimicrobial agents as prophylaxis in orthopedic surgery. J Chemother. 2001;13 Spec No 1:73-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Keith MW, Masear V, Amadio PC, Andary M, Barth RW, Graham B, Chung K, Maupin K, Watters WC 3rd, Haralson RH 3rd, Turkelson CM, Wies JL, McGowan R. Treatment of carpal tunnel syndrome. J Am Acad Orthop Surg. 2009;17:397-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 79] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 15. | Ghnaimat MM, Shawabkeh JS, Hijazi AM, Alturk MM, Aldweri MK. Aldweri. Is Antibiotic Prophylaxis in Knee Arthroscopy Mandatory? J R Med Serv. 2009;16:39-41. |
| 16. | Wieck JA, Jackson JK, O’Brien TJ, Lurate RB, Russell JM, Dorchak JD. Efficacy of prophylactic antibiotics in arthroscopic surgery. Orthopedics. 1997;20:133-134. [PubMed] |
| 17. | Qi Y, Yang X, Pan Z, Wang H, Chen L. Value of antibiotic prophylaxis in routine knee arthroscopy : A retrospective study. Orthopade. 2018;47:246-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Phegan M, Grayson JE, Vertullo CJ. No infections in 1300 anterior cruciate ligament reconstructions with vancomycin pre-soaking of hamstring grafts. Knee Surg Sports Traumatol Arthrosc. 2016;24:2729-2735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 19. | Vertullo CJ, Quick M, Jones A, Grayson JE. A surgical technique using presoaked vancomycin hamstring grafts to decrease the risk of infection after anterior cruciate ligament reconstruction. Arthroscopy. 2012;28:337-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 89] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 20. | Sherman OH, Fox JM, Snyder SJ, Del Pizzo W, Friedman MJ, Ferkel RD, Lawley MJ. Arthroscopy-“no-problem surgery”. An analysis of complications in two thousand six hundred and forty cases. J Bone Joint Surg Am. 1986;68:256-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 281] [Cited by in RCA: 230] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 21. | Jebson PJ, Adams BD. Wrist arthrodesis: review of current techniques. J Am Acad Orthop Surg. 2001;9:53-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 40] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Pérez-Prieto D, Torres-Claramunt R, Gelber PE, Shehata TM, Pelfort X, Monllau JC. Autograft soaking in vancomycin reduces the risk of infection after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2016;24:2724-2728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 91] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 23. | Babcock HM, Carroll C, Matava M, L’ecuyer P, Fraser V. Surgical site infections after arthroscopy: Outbreak investigation and case control study. Arthroscopy. 2003;19:172-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 39] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 24. | Onyema C, Oragui E, White J, Khan WS. Evidence-based practice in arthroscopic knee surgery. J Perioper Pract. 2011;21:128-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Lubowitz JH, Poehling GG. Arthroscopy and antibiotics. Arthroscopy. 2007;23:1-3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 26. | D’Angelo GL, Ogilvie-Harris DJ. Septic arthritis following arthroscopy, with cost/benefit analysis of antibiotic prophylaxis. Arthroscopy. 1988;4:10-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 80] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 27. | Kurzweil PR. Antibiotic prophylaxis for arthroscopic surgery. Arthroscopy. 2006;22:452-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 28. | Nakayama H, Yagi M, Yoshiya S, Takesue Y. Micro-organism colonization and intraoperative contamination in patients undergoing arthroscopic anterior cruciate ligament reconstruction. Arthroscopy. 2012;28:667-671. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 29. | Torres-Claramunt R, Pelfort X, Erquicia J, Gil-González S, Gelber PE, Puig L, Monllau JC. Knee joint infection after ACL reconstruction: prevalence, management and functional outcomes. Knee Surg Sports Traumatol Arthrosc. 2013;21:2844-2849. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 66] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 30. | Edelstein AI, Weiner JA, Cook RW, Chun DS, Monroe E, Mitchell SM, Kannan A, Hsu WK, Stulberg SD, Hsu EL. Intra-Articular Vancomycin Powder Eliminates Methicillin-Resistant S. aureus in a Rat Model of a Contaminated Intra-Articular Implant. J Bone Joint Surg Am. 2017;99:232-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 45] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 31. | Yazdi H, Moradi A, Herbort M. The effect of gentamicin in irrigating solutions on articular infection prophylaxis during arthroscopic ACL reconstruction. Arch Orthop Trauma Surg. 2014;134:257-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |