Published online Sep 18, 2017. doi: 10.5312/wjo.v8.i9.741
Peer-review started: January 29, 2017
First decision: May 11, 2017
Revised: May 18, 2017
Accepted: June 12, 2017
Article in press: June 13, 2017
Published online: September 18, 2017
Processing time: 232 Days and 6.4 Hours
Giant cell tumor (GCT) remains as major health problem. GCT which located at the lower end of the radius tends to be more aggressive. Wide excision and reconstruction of the wrist in stage 3 of distal radius GCT lesion is an optimal modality to prevent tumor recurrence. However, dislocation often occurs as its complication. We are reporting patient with GCT of distal radius treated with wide excision and reconstruction using nonvascularized fibular graft and the addition of hernia mesh. Circumferential non-absorbable polypropylene hernia mesh was applied, covered radioulnar joint and volar aspect of radius, and served as additional support to prevent dislocation. During five years and two months of follow-up, we found no dislocation in our patient. Furthermore, good functional outcome was obtained. Our finding suggests that the addition of hernia mesh after wide excision and reconstruction with nonvascularized fibular graft may benefit to prevent dislocation and provides an excellent functional outcome.
Core tip: Dislocation after wide excision and reconstruction with nonvascularized fibular graft on giant cell tumor (GCT) distal radius often occur and becomes a problem for the patient. This case report presented the outcome of a patient with GCT of distal radius and treated with wide excision and nonvascularized fibular graft with the addition of non-absorbable polypropylene hernia mesh. Circumferential non-absorbable polypropylene hernia mesh may prevent the occurrence of dislocation and provides an excellent functional outcome.
- Citation: Wiratnaya IGE, Budiartha IGBAM, Setiawan IGNY, Sindhughosa DA, Kawiyana IKS, Astawa P. Hernia mesh prevent dislocation after wide excision and reconstruction of giant cell tumor distal radius. World J Orthop 2017; 8(9): 741-746
- URL: https://www.wjgnet.com/2218-5836/full/v8/i9/741.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i9.741
Giant cell tumor (GCT) is an aggressive lesion with a high rate of recurrence[1]. Most GCTs are located in the epiphyseal regions of long bones, however studies reported that GCT in the lower end of the radius more aggressive and possess higher tendency for local recurrence[2,3]. Treatments for GCT of distal radius include curettage followed by bone graft or cementing, en-bloc excision and reconstruction either with nonvascular or vascular fibular autograft, ulnar translocation, endoprosthesis, or amputation[4-6].
Wide excision is the optimal surgical treatment modality to prevent tumor recurrence in stage 3 of distal radius GCT lesion. However, reconstruction of wrist after wide excision of distal radius remains a challenging task. Most patients are active young adults who demand cosmetically acceptable and functionally adequate wrist. Nonvascularized proximal fibular graft without arthrodesis still used for reconstruction with excellence function, but dislocation of radiocarpal joint often occur as its complication after surgery[7]. Here we try to prevent dislocation of radiocarpal joint by using hernia mesh.
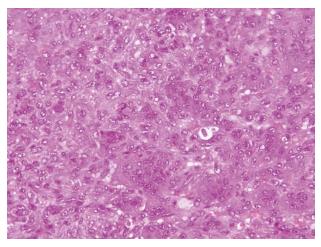
A 28-year-old female presented with lump and pain on the left wrist since one year. The lump was getting bigger, and the pain was felt while flexing the wrist. On examination, the lump was observed on the distal end of the radius with tissue exposure on the dorsal side (Figure 1). The skin was shiny, tense, tenderness with ill-defined margins. The wrist’s range of movements was restricted with intact neurovascular status. Left wrist anteroposterior and lateral radiograph revealed extensive local bony destruction along with significant soft-tissue expansion (campanaci grade 3) (Figure 2). She was suspected with GCT of the left distal radius. However, she refused open biopsy and went to bone setter. She came back to the outpatient clinic and then an open biopsy was performed. Histopathology examination revealed GCT of bone (Figure 3).
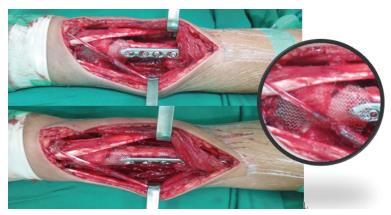
We did wide excision (Figure 4) with a posterior approach along with intracapsular resection (Figure 5) and osteotomy 9 cm proximal from styloid of radius (Figure 6). Flexor, extensor tendon, radial, ulnar artery, median and ulnar nerve were able to preserve. Subsequently, the lateral approach was used for harvesting entire proximal fibula including the head of fibula and bicep tendon with a length of 4 cm. The common peroneal nerve was identified and osteotomy 10 cm from the head of fibula was done (Figure 7).
The harvested fibula was fixed to the radius with 3.5 locking plate. The tip of fibula should lie for the radial styloid and its articular surface articulated with scaphoid. The dorsal radiocarpal capsule was sutured with bicep tendon, and the transplanted fibula stabilized to ulnar with 1.6 K wire. To prevent dislocation of the radioulnar and radiocarpal joint, circumferential non-absorbable polypropylene hernia mesh was applied circularly. At the distal part, the mesh was sutured to the remain of the capsule and the ligament of os carpalia at the volar, while at the proximal part the mesh was sutured to the periosteum and the surrounding soft tissue, attached to fibular graft. The mesh covered the radioulnar joint (Figure 8). This hernia mesh is used to provide additional support to weakened or damaged tissue in this area. Afterward, X-ray examination was performed (Figure 9). A short arm splint in 30° wrist extension was applied. Splint and pins were removed six weeks post operation and gentle range of motion was advised.
Four months post operation we evaluate her functional outcome by using Mayo Wrist Score and obtained a good result. Evaluation with quick dash score also obtained a good result. The total disabilities involving the arm, shoulder and hand (DASH) score was 9.2. During five years and two months of follow-up, no subluxation was observed in our patient (Figure 10). The total Mayo Wrist Score was 90. The patient did not feel any pain, returned to regular employment, range of motion of 75%-99% of normal side, and grip strength of 100% compared with normal hand (Figure 11).
En bloc excision method leaving a large defect in excision area, thus reconstruction on this site is necessary. Various techniques have been described for reconstruction, including iliac crest graft, centralization of ulna, distal radial allograft, vascularized or non-vascularized fibular graft, and prosthesis. Non-vascularized fibular autograft is one reconstruction technique to fill the defect caused by the wide excision. It was first used in 1945 for congenital absence of radius. The fibula was chosen since its size and shape are similar with distal radius[8]. Later, fibular transplant was used by various authors for tumors of the lower end of radius.
Nonvascularized fibular autograft possesses more advantages compared with other procedures. It has low morbidity of the donor site, satisfactory functional result, and free of major complications although some minor complications exist[7,9,10]. A study by Saini et al[11] in twelve patients with GCT of distal radius treated with wide excision of tumor and ipsilateral nonvascularized fibular autograft obtained the average of grip strength was 70% (24%-86%) compared with normal contralateral side and well preserved of forearm supination and pronation movement. However, a complication in term of subluxation occurs in 3 cases.
Subluxation is a commonly-occurring complication in defect reconstruction with nonvascularized fibular autograft method. With the addition of hernia mesh, the patient in our case did not develop any dislocation or subluxation, but the incidences reported in the literature are quite high. A study by Saikia et al[7] (2010) obtained 10 cases of subluxation from the total of 24 GCT of distal radius cases treated with en bloc resection and arthroplasty reconstruction of autogenous non-vascularized ipsilateral fibular graft. Seven of them occur 3-12 mo after surgery. A study by Dhammi et al[12] in 16 patient with GCT of lower end radius treated with similar method reported 10 cases suffered from wrist subluxation out of 16 patients, with follow-up duration ranges from two to five years. Saraf et al[13] reported subluxation on 2 patients from 15 patients which caused significant pain, deformity, and loss of function.
Fibular graft with appropriate length is a method to prevent subluxation of wrist joint after the reconstruction was performed. Saikia et al[7] ensure the appropriate length obtained with the addition of 2-3 mm longer than the required length, which is the resection tumor and safe margin, so that the compression at the host-graft junction during fixation with DCP was achieved and subluxation could be prevented. K-wire fixation used to stabilized wrist joint. However, this method did not ensure the prevention of subluxation.
We perform modification with a different approach than previous technique that is the addition of hernia mesh to prevent subluxation or dislocation. Circumferential hernia mesh which covered radioulnar joint and volar aspect of the radius was applied to stabilize the graft. Furthermore, the tensile strength of the mesh may withstand the local pressure forces, hence prevent the occurrence of dislocation or subluxation. During five years and two months of follow-up, no subluxation was observed in our patient. The total Mayo Wrist Score was 90. The patient did not feel any pain, returned to regular employment, the range of motion of 75%-99% of normal side, and grip strength of 100% compared with normal hand.
In conclusion, the complication in the form of subluxation did not occur in our case. Reconstruction method with the addition of hernia mesh to prevent subluxation provides an excellent functional outcome.
A 28-year-old female with lump which getting bigger in the last one year and pain on left wrist, aggravated by flexion of the wrist.
Swelling on the distal end of radius, the skin condition was shiny, tense, tenderness with ill-defined margins, and tissue exposure on the dorsal side.
Aneurysmal bone cyst and tuberculosis of bone.
All labs were within normal limits.
Anteroposterior and lateral radiograph of the left wrist showed extensive local bony destruction along with significant soft-tissue expansion (campanaci grade 3).
Multinucleated giant cells with a background of mononuclear cells, appropriate for giant cell tumor (GCT).
Wide excision and reconstruction using non vascularized fibular graft with the addition of hernia mesh.
GCT located in the lower end of the radius tend to be more aggressive and has a higher tendency for local recurrence. The optimal surgical treatment to prevent tumor recurrence in stage 3 of GCT distal radius is wide excision along with non-vascularized fibular autograft to repair the large defect in excision area. Subluxation is a commonly-occurring complication in defect reconstruction with nonvascularized fibular autograft method. The addition of hernia mesh may advantageous to prevent the subluxation, affecting the functional outcome of the patient.
GCTs are benign tumors which have a tendency for aggressive characteristics and ability to metastasize. The disabilities of the arm, shoulder and hand (DASH) score is an outcome instrument for measuring upper-extremity disability and symptoms.
The addition of hernia mesh after wide excision and reconstruction using nonvascularized fibular graft of GCT of distal radius prevent the complication in term of subluxation and offer excellent functional outcome.
The authors present a very interesting paper on the reconstruction of the wrist after radius bone excision for a GCT.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Indonesia
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Guerado E S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Malu RG, Jaju CR, Goyal V, Mali S, Nagoba B. Giant cell tumor of distal radius treated by en-bloc resection and reconstruction by non vascularized fibular graft. Eur J gen Med. 2015;12:183-186. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Gupta V, Kumar V. Recurrent giant cell tumor of the distal end radius: a case report and surgical treatment with wide resection and reconstruction with non-vascularized autologous proximal fibular graft. Open Journal of Orthopedics. 2014;4:285-291. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Cheng CY, Shih HN, Hsu KY, Hsu RW. Treatment of giant cell tumor of the distal radius. Clin Orthop Relat Res. 2001;383:221-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 92] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Khalil el SA, Younis A, Aziz SA, El Shahawy M. Surgical management for giant cell tumor of bones. J Egypt Natl Canc Inst. 2004;16:145-152. [PubMed] |
| 5. | Chalidis BE, Dimitriou CG. Modified ulnar translocation technique for the reconstruction of giant cell tumor of the distal radius. Orthopedics. 2008;31:608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Rastogi S, Prashanth I, Khan SA, Trikha V, Mittal R. Giant cell tumor of bone: Is curettage the answer? Indian J Orthop. 2007;41:109-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Saikia KC, Borgohain M, Bhuyan SK, Goswami S, Bora A, Ahmed F. Resection-reconstruction arthroplasty for giant cell tumor of distal radius. Indian J Orthop. 2010;44:327-332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Rabitsch K, Maurer-Ertl W, Pirker-Frühauf U, Wibmer C, Leithner A. Intercalary reconstructions with vascularised fibula and allograft after tumour resection in the lower limb. Sarcoma. 2013;2013:160295. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Chadha M, Arora SS, Singh AP, Gulati D, Singh AP. Autogenous non-vascularized fibula for treatment of giant cell tumor of distal end radius. Arch Orthop Trauma Surg. 2010;130:1467-1473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Asavamongkolkul A, Waikakul S, Phimolsarnti R, Kiatisevi P. Functional outcome following excision of a tumour and reconstruction of the distal radius. Int Orthop. 2009;33:203-209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Saini R, Bali K, Bachhal V, Mootha AK, Dhillon MS, Gill SS. En bloc excision and autogenous fibular reconstruction for aggressive giant cell tumor of distal radius: a report of 12 cases and review of literature. J Orthop Surg Res. 2011;6:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 12. | Dhammi IK, Jain AK, Maheshwari AV, Singh MP. Giant cell tumors of lower end of the radius: problems and solutions. Indian J Orthop. 2005;39:201-205. [DOI] [Full Text] |
| 13. | Saraf SK, Goel SC. Complications of resection and reconstruction in giant cell tumour of distal end of radius-An analysis. Ind J Orthop. 2005;39:206-211. [RCA] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |