Published online Sep 18, 2017. doi: 10.5312/wjo.v8.i9.705
Peer-review started: February 15, 2017
First decision: March 27, 2017
Revised: April 10, 2017
Accepted: June 6, 2017
Article in press: June 7, 2017
Published online: September 18, 2017
Processing time: 215 Days and 23.8 Hours
To compare the operation time, blood loss, and early outcomes of acetabular components with and without the screw.
Thirty patients who underwent cementless acetabular component with or without screw and whose follow-up exceeded one year period in total hip arthroplasty were evaluated. A posterior approach was used in all surgical procedures by one experienced surgeon. Demographic data, operation time, intra- and postoperative blood loss volume, follow-up clinical score, cup migration, and osteolysis were recorded. The Kolmogorov-Smirnov test was performed for testing the normality of study data. Mann-Whitney U test was used to analyze the inter-group differences. A P-value of ≤ 0.05 was considered statistically significant.
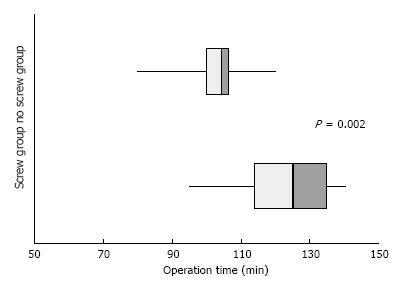
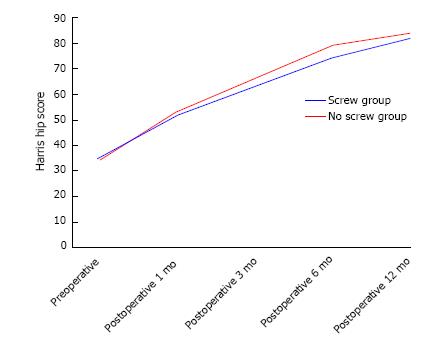
Acetabular components were used in 16 (53.3%) patients with screw and 14 (46.7%) without screw. After one year of follow-up, an osteolytic lesion of 3 mm was found in only one patient in the screw group. No cup migration was encountered. Intra-group mean Harris hip score significantly increased, but there was no significant inter-group difference. While the mean operation time of the screw group was 121.8 min (range; 95-140), it was 102.7 min (range; 80-120) in the no-screw group, and this difference was statistically significant (P = 0.002). The mean intraoperative/postoperative, and total blood loss were 556.6 mL (range: 350-800)/423.3 mL (range: 250-600), and 983.3 mL (range: 600-1350), respectively in the screw group; and 527 mL (range: 400-700)/456 mL (range: 230-600), and 983 mL (range: 630-1250), respectively in the no-screw group. The blood loss difference between the two groups was not significant. In the screw group, the operation time was 19.1 min longer than the no-screw group, and this difference was statistically significant.
Acetabular components with or without screw have similar results, but the use of screw increases the operation time significantly, while not changing the blood loss volume.
Core tip: This is a retrospective study comparing the perioperative data and early outcomes of the screw and no-screw acetabular components in total hip arthroplasty. There is no study comparing the screw and no-screw components for perioperative data in the literature. Both components were characterized with similar clinical outcomes in the early term. But additional screws significantly increase the mean operative time.
- Citation: Pepe M, Kocadal O, Erener T, Ceritoglu K, Aksahin E, Aktekin CN. Acetabular components with or without screws in total hip arthroplasty. World J Orthop 2017; 8(9): 705-709
- URL: https://www.wjgnet.com/2218-5836/full/v8/i9/705.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i9.705
Uncemented porous coated acetabular components have been preferred over cemented ones in primary total hip arthroplasty (THA) in the last 25 years[1]. Cementless acetabular cups can be implanted with or without screw[2]. While some studies have reported that the additional screw improves stability, others have mentioned that the press-fit implanted no-screw components have produced similar results with the screw fixation systems[3-6]. In addition, avoidance of screw reduces the risk of osteolysis of acetabular bone, neurovascular complications, and operational costs[7-9]. Screws could be responsible for an increased wear due to two phenomena. One is by contact with the insert, and the other one by corrosion between the screw and the cup. Screws can ensure stability in osteoporotic bones, acetabular defects, and when reliable implantation is not possible during surgery[10]. Studies comparing acetabular components with and without screws are of limited number, and the majority of them have focused on component migration, osteolysis, and clinical outcome[4,5,11]. According to our literature survey, no study has yet compared screw and no-screw fixation with respect to blood loss and operation time. In our study, we aimed to compare these two groups in terms of bleeding, surgery time, early clinical outcome, and cup migration.
Patients who underwent THA with cementless porous coated acetabular component with or without screw for primary hip osteoarthritis and who had at least 12 mo of follow-up were included in this study. Patients with previous hip surgery, revision cases, cemented components, Crowe type 3 and 4 patients, less than 1 year follow-up, tumor or constrained prosthesis, and any bleeding diathesis were excluded from the study. The amount of intraoperative bleeding was determined by a resident by adding the total gauze weight to the difference between the irrigation and vacuum volumes[12,13]. The postoperative blood loss was calculated by the volume of drainage. No pharmacological agent was used to affect the bleeding; monopolar cauterization was applied for hemostasis during surgery. The time from the beginning of the surgical incision to the closure of the subcutaneous tissue was recorded as the operation time. Harris hip scores (HHP) were recorded by a resident at preoperative period and at postoperative 1st, 3rd, 6th, and 12th months. On the first day after surgery, articular suction drain was removed and walking and strengthening exercises without full loading were started. Patients began to walk with full weight bearing at 6th week after surgery. Radiolucent lines, osteolytic lesions more than 3 mm in diameter[14] and bone loss were recorded on radiographs of the patients at 3 acetabular regions described by Delee and Charnley[15]. This study was approved by the ethical committee of our hospital.
All patients underwent unilateral THA. Preoperatively, pelvis and standing posteroanterior hip radiographs were obtained. Posterior approach was performed in all surgical procedures by one experienced surgeon. A cementless proximal 1/3 porous plasma spray coated Bi-Metric femoral component was used in all patients. A cementless Exceed ABT taper fit acetabular cup with C2A ceramic liner and head was used in patients under 65 years old. A cementless Exceed ABT Ringloc X acetabular cup and E1 10° polyethylene liner and M2A CoCrMo head was used in patients over 65 years old (Biomet, Warsaw, IN). Acetabular socket preparation was similar in both groups and the region was reamed concentrically. When the maximum medial depth was reached, the acetabular cup was implanted. After the surgeon implanted the component, he attempted to move the cup bar antero-posteriorly and supero-inferiorly for the stability control, and two additional screws were used if the stabilization was suspicious. Otherwise it was implanted without screws.
SPSS Mac OS X 20.0 (SPSS, Chicago, IL) program was used for statistical analysis. The Kolmogorov–Smirnov test was used to test the normality of study data. Mann-Whitney U test was used for the analysis of operation time, bleeding volumes, and clinical scores between the groups. The Wilcoxon test was used to analyze the changes in intra-group clinical scores before and after the operation. A P-value below 0.05 was considered statistically significant.
Ten (33.3%) patients were male and 20 (66.7%) were female. Acetabular cups were used with screw in 16 (53.3%) patients and without screw in 14 (46.7%) patients. Table 1 shows the demographic data of the patients. While the mean operation time was 121.8 min (range; 95-140), in the screw group, it was 102.7 min (range; 80-120) in the no-screw group, and this difference was statistically significant (P = 0.002) (Figure 1). The mean intraoperative bleeding volume was 556.6 mL (range; 350-800)/527 mL (range; 400-700), the postoperative drainage volume was 423.3 mL (range; 250-600)/456 mL (range; 230-600), and the mean total bleeding volume was 983.3 mL (range; 600-1350)/983 mL (range; 630-1250) in the screw/no-screw group, respectively. The bleeding amount was not statistically significant between the groups (P > 0.05). Harris hip scores significantly increased within the groups, but no significant difference was found between the groups (Figure 2). Hip dislocation occurred in two patients. One of them occurred in the screw group 15 d after surgery and was relocated by sedation in the operating room; the other one was noticed in no-screw group at the early postoperative period and relocated on patient bed. No-screw group had a trochanteric fracture during femoral stem implantation. Plate fixation was performed and callus tissue formed at 6th month. None of the patients had acetabular component migration and revision surgery. One patient in screw group (6.2%) had osteolytic lesions around the screw (Table 1).
| Screw group | No-screw group | |
| No. of patients | 16 (53.3) | 14 (46.7) |
| Age (yr) | 56.5 (36-82) | 54.0 (35-68) |
| Sex | ||
| Male | 4 (25) | 6 (42.9) |
| Female | 12 (75) | 8 (57.1) |
| Diagnosis | ||
| Osteoarthritis/posttraumatic | 12 | 9 |
| Inflammatory | 2 | 3 |
| Osteonecrosis | 2 | 2 |
| Head size | ||
| 28 | 1 | 0 |
| 32 | 15 | 14 |
Transacetabular screw is used by surgeons to improve stability in total hip arthroplasty[10,16]. It has been shown to improve initial stability in cadaveric studies[10,17]. However, it is known that additional screws increase neurovascular complications[8], although there is no consensus whether they increase osteolytic lesions[11,18,19]. Some authors have attributed the increase in osteolytic lesions to a reaction to the debris escaping from the screw holes to the acetabular bone[6,20]. In contrast, Schmalzried et al[19] reported in their retrospective study that pelvic osteolysis is associated with significantly greater head size and longer follow-up than screw use. In our study, only one case of osteolysis was identified, which was in the screw group. We attributed the low number of osteolysis cases to a short follow-up period.
Cup migration can be evaluated not only by conventional radiography but also by radiostereometry[20]. Studies comparing middle- and long-term cup migration have yielded no significant differences between the screw and no-screw groups[11,20]. In our study, cup migration did not occur in either group at one-year follow up.
Thanner et al[4] reported a comparative study and found a mean HHP of 99 in the screw group and 98 in the no-screw group at the end of 2 years. In our study, at the end of one year, the mean HHP was 81.6 in the screw group and 84 in the no-screw group. Similar to the literature findings, our study did not reveal any significant differences between the two groups in terms of clinical outcomes and cup migration. Short-term follow-up and limited case series were the weak points of our study.
The strength of our study is that it compared perioperative data. A review of the literature indicated that no study has yet compared the screw and no-screw groups with regard to volume of blood loss and operation time. Studies have reported that blood loss in THA ranges between 600 and 1800 mL[21,22]. The mean blood loss in our study was 983.3 mL in the screw group and 983 mL in the no-screw group, with the difference being statistically non-significant. The mean volume of intraoperative bleeding was greater by 29.6 mL in the screw group. We attributed this difference to a bleeding from screw holes, but it was not statistically significant. An analysis of the postoperative drain volumes revealed that the mean volume was greater by 32.7 mL in the no-screw group, which contributed to a slight difference of 0.3 mL between the two groups in the total amount of bleeding.
Duchman et al[23] reported that an operative time greater than 120 min was associated with increased short-term morbidity and risk of complications in THA. We found a mean operative time of 121.8 min in the screw group but no complication such as wound infection was encountered. We compared the screw and no-screw groups for the operation time and found that the mean time was 19.1 min greater in the screw group, and this difference was statistically significant. We attribute this difference to preparation of holes, sterile unpacking, and screwing.
Similar to the literature data, our study showed no difference between clinical outcome and cup migration between the screw and no-screw groups in the short term, whereas not using a screw provided a significant advantage in terms of operation time.
Cementless acetabular components in total hip arthroplasty can be implanted with or without screws. It is known that using screws increases neurovascular complications. However, its effects on osteolysis, component stability, and migration are still being debated. No study has compared the perioperative data of screw and no-screw components in the literature. In this study, the authors compared the acetabular components with and without screws in terms of bleeding, operation time, early clinical outcomes, and cup migration.
The results of this study contribute to clarifying the effect of the screws used in the fixation of the acetabular component in total hip arthroplasty on the operation time, surgical bleeding, and early clinical outcomes.
Using screw did not affect clinical outcome and cup migration at the early postoperative period. Screw and no-screw groups showed similar results in respect to surgical bleeding. However, the use of the screw significantly increased the operation time.
This study showed that the implantation of the acetabular component without screw would have a significant advantage in the operation time.
Osteolysis: Bone matrix resorption by osteoclast cells.
The sample size and the follow up is short of course but interesting.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Turkey
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Prudhon JL S- Editor: Kong JX L- Editor: A E- Editor: Lu YJ
| 1. | Yamada H, Yoshihara Y, Henmi O, Morita M, Shiromoto Y, Kawano T, Kanaji A, Ando K, Nakagawa M, Kosaki N. Cementless total hip replacement: past, present, and future. J Orthop Sci. 2009;14:228-241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 75] [Cited by in RCA: 69] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 2. | Engh CA, Hopper RH, Engh CA. Long-term porous-coated cup survivorship using spikes, screws, and press-fitting for initial fixation. J Arthroplasty. 2004;19:54-60. [PubMed] |
| 3. | Roth A, Winzer T, Sander K, Anders JO, Venbrocks RA. Press fit fixation of cementless cups: how much stability do we need indeed? Arch Orthop Trauma Surg. 2006;126:77-81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 29] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Thanner J, Kärrholm J, Herberts P, Malchau H. Hydroxyapatite and tricalcium phosphate-coated cups with and without screw fixation: a randomized study of 64 hips. J Arthroplasty. 2000;15:405-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 48] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Iorio R, Puskas B, Healy WL, Tilzey JF, Specht LM, Thompson MS. Cementless acetabular fixation with and without screws: analysis of stability and migration. J Arthroplasty. 2010;25:309-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Udomkiat P, Dorr LD, Wan Z. Cementless hemispheric porous-coated sockets implanted with press-fit technique without screws: average ten-year follow-up. J Bone Joint Surg Am. 2002;84-A:1195-1200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 93] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 7. | Valle AG, Zoppi A, Peterson MG, Salvati EA. Clinical and radiographic results associated with a modern, cementless modular cup design in total hip arthroplasty. J Bone Joint Surg Am. 2004;86-A:1998-2004. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 75] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Wasielewski RC, Cooperstein LA, Kruger MP, Rubash HE. Acetabular anatomy and the transacetabular fixation of screws in total hip arthroplasty. J Bone Joint Surg Am. 1990;72:501-508. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 174] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Healy WL, Iorio R, Lemos MJ, Patch DA, Pfeifer BA, Smiley PM, Wilk RM. Single Price/Case Price Purchasing in orthopaedic surgery: experience at the Lahey Clinic. J Bone Joint Surg Am. 2000;82:607-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Hsu JT, Chang CH, Huang HL, Zobitz ME, Chen WP, Lai KA, An KN. The number of screws, bone quality, and friction coefficient affect acetabular cup stability. Med Eng Phys. 2007;29:1089-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 88] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 11. | Ni SH, Guo L, Jiang TL, Zhao J, Zhao YG. Press-fit cementless acetabular fixation with and without screws. Int Orthop. 2014;38:7-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Nadler SB, Hidalgo JH, Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962;51:224-232. [PubMed] |
| 13. | Li J, Zhao J, He C, Tong W, Zou Y, Xu W. Comparison of Blood Loss After Total Hip Arthroplasty Between Ankylosing Spondylitis and Osteoarthritis. J Arthroplasty. 2016;31:1504-1509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Claus AM, Sychterz CJ, Hopper RH, Engh CA. Pattern of osteolysis around two different cementless metal-backed cups: retrospective, radiographic analysis at minimum 10-year follow-up. J Arthroplasty. 2001;16:177-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20-32. [PubMed] |
| 16. | Lachiewicz PF, Suh PB, Gilbert JA. In vitro initial fixation of porous-coated acetabular total hip components. A biomechanical comparative study. J Arthroplasty. 1989;4:201-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 47] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Perona PG, Lawrence J, Paprosky WG, Patwardhan AG, Sartori M. Acetabular micromotion as a measure of initial implant stability in primary hip arthroplasty. An in vitro comparison of different methods of initial acetabular component fixation. J Arthroplasty. 1992;7:537-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 76] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Schmalzried TP, Akizuki KH, Fedenko AN, Mirra J. The role of access of joint fluid to bone in periarticular osteolysis. A report of four cases. J Bone Joint Surg Am. 1997;79:447-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 100] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 19. | Schmalzried TP, Brown IC, Amstutz HC, Engh CA, Harris WH. The role of acetabular component screw holes and/or screws in the development of pelvic osteolysis. Proc Inst Mech Eng H. 1999;213:147-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Röhrl SM, Nivbrant B, Ström H, Nilsson KG. Effect of augmented cup fixation on stability, wear, and osteolysis: a 5-year follow-up of total hip arthroplasty with RSA. J Arthroplasty. 2004;19:962-971. [PubMed] |
| 21. | Smith LK, Williams DH, Langkamer VG. Post-operative blood salvage with autologous retransfusion in primary total hip replacement. J Bone Joint Surg Br. 2007;89:1092-1097. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Hochreiter J, Hejkrlik W, Emmanuel K, Hitzl W, Ortmaier R. Blood loss and transfusion rate in short stem hip arthroplasty. A comparative study. Int Orthop. 2016; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 23. | Duchman KR, Pugely AJ, Martin CT, Gao Y, Bedard NA, Callaghan JJ. Operative Time Affects Short-Term Complications in Total Joint Arthroplasty. J Arthroplasty. 2017;32:1285-1291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 118] [Article Influence: 14.8] [Reference Citation Analysis (0)] |