Published online Sep 18, 2017. doi: 10.5312/wjo.v8.i9.697
Peer-review started: February 7, 2017
First decision: May 2, 2017
Revised: July 23, 2017
Accepted: August 2, 2017
Article in press: August 3, 2017
Published online: September 18, 2017
Processing time: 233 Days and 0.7 Hours
To analyze different terms used in literature to identify lumbar extradural cysts and propose a common scientific terminology; to elaborate a new morphological classification of this pathology, useful for clinical and surgical purposes; and to describe the best surgical approach to remove these cysts, in order to avoid iatrogenic instability or treat the pre-existing one.
We retrospectively reviewed 34 patients with symptomatic lumbar ganglion cysts treated with spinal canal decompression with or without spinal fixation. Microsurgical approach was the main procedure and spinal instrumentation was required only in case of evident pre-operative segmental instability.
The complete cystectomy with histological examination was performed in all cases. All patients presented an improvement of clinical conditions, evaluated by Visual Analogic Scale and Japanese Orthopaedic Association scoring.
Spinal ganglion cysts are generally found in the lumbar spine. The treatment of choice is the microsurgical cystectomy, which generally does not require stabilization. The need for fusion must be carefully evaluated: Pre-operative spondylolisthesis or a wide joint resection, during the operation, are the main indications for spinal instrumentation. We propose the terms “ganglion cyst” to finally identify this spinal pathology and for the first time its morphological classification, clinically useful for all specialists.
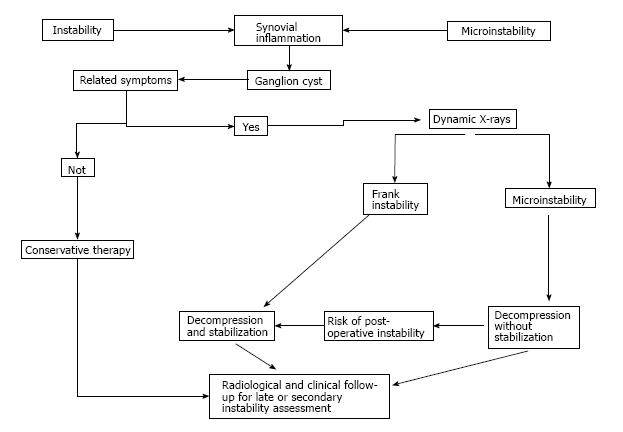
Core tip: This paper is an original study that analyzes for the first time the many words and acronyms used in literature to describe lumbar extradural cysts, suggesting the term “ganglion cyst” in clinical practice. It also propose a morphological classification of these cysts, which could be useful for clinicians and surgeons. Finally, a description of microsurgical approaches to resect the cyst and avoid spinal instability is reported: As a guide to a common therapeutical strategy, we report a flow-chart, evaluating clinical conditions, mechanical stability and the most suitable treatment.
- Citation: Domenicucci M, Ramieri A, Marruzzo D, Missori P, Miscusi M, Tarantino R, Delfini R. Lumbar ganglion cyst: Nosology, surgical management and proposal of a new classification based on 34 personal cases and literature review. World J Orthop 2017; 8(9): 697-704
- URL: https://www.wjgnet.com/2218-5836/full/v8/i9/697.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i9.697
Ganglion cysts, more common in the hands and wrists[1,2], have been described for more than 2 millennia[3]. The Greek term “ganglion” indicates a knot of the tissues.
Ganglion cysts of the minor and major joints, especially at the level of the wrist and back of the hand, have been known since ancient times and were described by Hippocrates[3] more than two millennia ago. These cysts have an high incidence: Burke et al[1], reviewing the period 1990-2000, found between 44 and 55 new cases per 100000 inhabitants each year.
In the past century, similar cysts were also described as originated from lumbar zygapophyseal joints and occupying the spinal canal, most frequently in the lumbar spine and occasionally, in the cervical and thoracic spine[4-6]. To define these spinal neoformations, many terms have been adopted in the literature, according to the site of development or to the supposed origin: Ganglion[6], juxtafacet[7], flavum[8], cyfmos[9] and synovial[7,8,10-14].
The etiology of the cyst, not fully clear, could be strongly related to inflammatory phenomena secondary to facet hypermobility, which would produce modifications of the articular synovial membrane leading to cyst formation[13] . Microsurgical cystectomy is today the treatment of choice[15], with or without arthrodesis: Generally, microsurgical approach does not produce vertebral instability and arthrodesis is required only in case of a clear pre-operative instability, such as spondylolisthesis.
Evaluating all etiological factors and all treatment options, we propose an original morphological classification of lumbar ganglion cysts, based on their relation with the other anatomical structures. Lastly, in order to clarify the confusing terminology that describes these particular cysts, we suggest “spinal ganglion cyst” (SGC) as definitive term to be applied in clinical practice.
Thirty-four cases of symptomatic lumbar SGCs surgically treated from 1995 to 2011 were enrolled ninths study. They include 18 previously published arthrodesis, with 3 hemorrhagic SGCs. All patients underwent preoperative magnetic resonance imaging (MRI) and computed tomography (CT) scan. To assess lumbar segmental instability, dynamic X-ray were also obtained in all patients but 4 cases, in which pain did not allow standing position.
Pain was evaluated by the Visual Analogic Scale (VAS score). Neurological examination was performed to assess signs of roots compression with any sensory and/or motor deficits.
All patients were operated through a microsurgical approach[15], to maintain articular congruence and not jeopardize vertebral stability. Cystectomy was achieved through laminotomy or hemilaminectomy. In presence of demonstrated pre-operative or iatrogenic intraoperative segmental instability (wide resection of the articular process), instrumented arthrodesis was also performed.
Histological examination of the cyst was performed in all cases to confirm the diagnosis.
Average follow-up was 28.5 mo (range 12-60). All patients underwent MRI, plain X-rays and were evaluated by VAS and modified Japanese Orthopaedic Association score (JOA score) for neurological improvement in the lower limbs.
The Wilcoxon signed rank test was used for statistical analysis, considering P value equal to or less than 0.05 as significant.
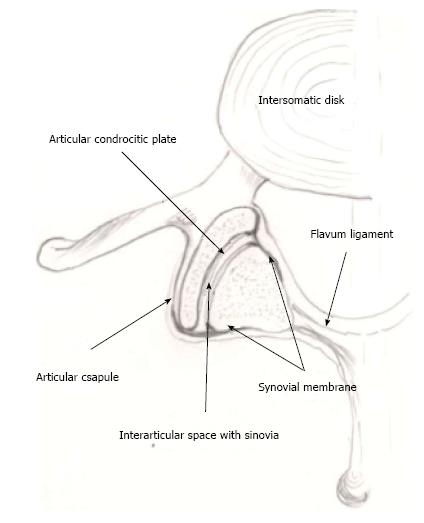
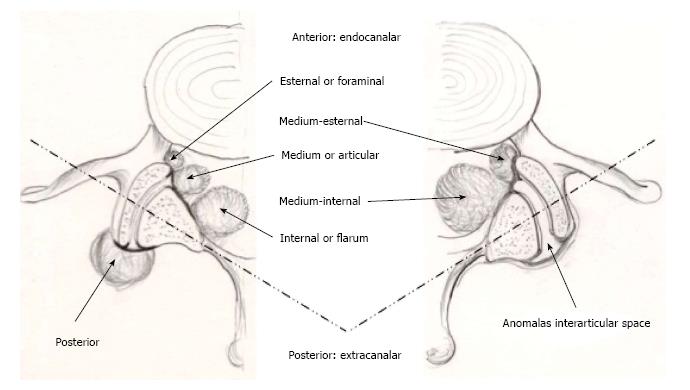
Based on our experience and literature review, we were able to construct a new and original classification of the ganglion cysts. By some drawings, performed by the first author (Maurizio D), we reported for the first time the main locations of these cysts, summarizing and comparing our radiological and surgical data with those from the pertinent literature.
The data regarding our 34 cases are summarized in Table 1. Average age was 63 (range 50-76 years): 13 (38%) patients were males and 21 (62%) females. All patients had radicular pain, generally associated with lumbago. In 7 cases (21%), neurological deficits were also present. No cauda equina syndrome was detected. Duration of symptoms prior to surgical treatment varied from 1 to 3 years in 10 cases, whereas in the others average duration was 142 d (range 10-300 d). An acute onset, with a brief preoperative symptomatology, occurred in 4 hemorrhagic cysts.
| Case | Age and sex | Location (side) | Instability | Treatment | Other data | ||
| Verified | Supposed | Type 1 | Type 2 | ||||
| 1 | 68 M | L5-S1 (left internal) | a | y | |||
| 2 | 75 M | L4-L5 (right medium) | a, b, c | y | Re | ||
| 3 | 50 F | L4-L5 (right medium-internal) | a, b | y | |||
| 4 | 63 F | L5-S1 (right medium) | b, c | y | |||
| 5 | 76 F | L4-L5 (left medium-internal) | a | y | |||
| 6 | 75 M | L5-S11 (right medium-lateral) | a, b, d | y | |||
| 7 | 75 F | L4-L5 (right medium-lateral) | y | b, c | y | ||
| 8 | 62 M | L4-L5 (right medium-internal) | y | a, b | y | ||
| 9 | 60 M | L4-L5 (right lateral) | a, b, c | y | |||
| 10 | 73 F | L5-S1 (right lateral) | a, b, d | y | |||
| 11 | 55 M | L2-L3 (left medium-lateral) | a | y | |||
| 12 | 55 M | L4-L5 (left medium) | y | a, b | y | ||
| 13 | 74 F | L3-L41 (right medium-lateral) | b, c | y | |||
| 14 | 56 F | L3-L4 (left medium-lateral) | y | a | y | ||
| 15 | 67 F | L4-L5 (left medium-lateral) | b | y | |||
| 16 | 56 F | L4-L5 (right medium-lateral) | b, c | y | |||
| 17 | 66 F | L4-L5 (left medium-internal) | b | y | IF | ||
| 18 | 68 M | L4-L51 (left medium-lateral) | a | y | |||
| 19 | 73 F | L5-S11 (left medium) | a, b | y | |||
| 20 | 53 F | L5-S1 (left medium-lateral) | a, b, c, d | y | |||
| 21 | 60 F | L4-L5 (right internal) | a, b, c, d | y | |||
| 22 | 52 M | L4-L5 (right medium-internal) | y | a | y | ||
| 23 | 64 F | L5-S1 (left internal) | y | a, b | y | ||
| 24 | 53 M | L5-S1 (left medium) | y | a, b | y | ||
| 25 | 73 F | L4-L5 (left medium-lateral) | a, b, c | y | IF | ||
| 26 | 54 F | L3-L4 (right medium-internal) | y | a, b | y | ||
| 27 | 61 M | L4-L5 (left medium) | a, b, c | y | |||
| 28 | 65 M | L5-S1 (left medium) | a, d | y | |||
| 29 | 71 M | L5-S1 (right medium-internal) | a | y | |||
| 30 | 52 F | L4-L5 (left medium-lateral) | a, b | y | |||
| 31 | 63 F | L4-L5 (right medium) | a, b | y | |||
| 32 | 72 F | L4-L5 (right lateral) | a, b, d | y | |||
| 33 | 56 F | L4-L5 (right lateral) | a | y | |||
| 34 | 62 F | L4-L5 (left medium-lateral) | a | y | |||
Preoperative dynamic X-rays showed a mobile olisthesis in 8 cases (23%) and a stable one in 6 (18%). In all cases, preoperative CT and MRI showed signs of microinstability consisting of a reduced disc space and black disc (28 cases, 82%), increased interfacet synovial fluid (24 cases, 70%) and/or signal hyperintensity of the interspinous ligament on STIR sequences (10 cases, 29%).
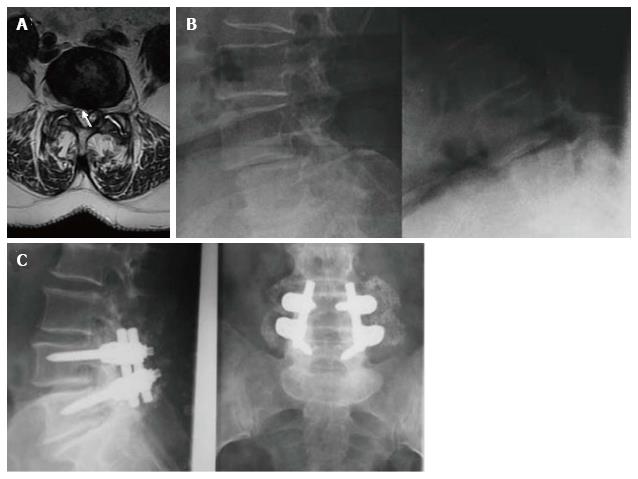
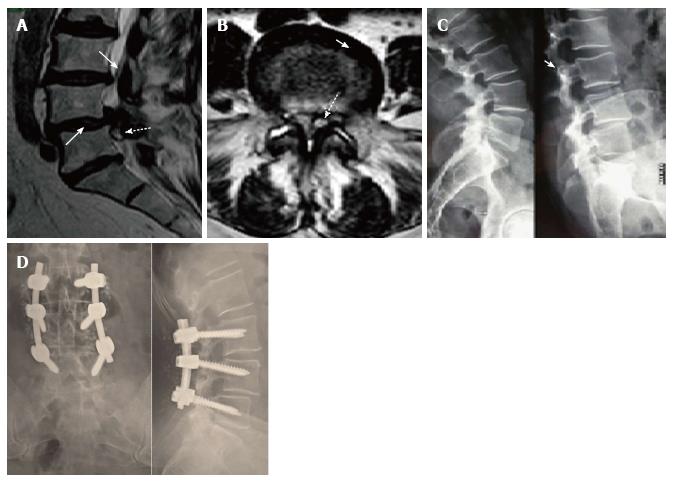
All 14 pre-operative spondylolisthesis were submitted to arthrodesis. Instrumented fusion was achieved at the level of the cyst in 10 cases (Figure 1), while, in the remaining 4, it was extended to the level above (Figure 2).
During surgery, we observed 2 dural laceration that were successfully repaired. Histology confirmed the nature of the lesions as ganglion or synovial cysts.
Based on neuroradiological investigations and operative findings, the lumbar SGCs were classified according to the scheme illustrated in Figures 3 and 4. Using this classification, 3 cysts were internal, 7 medium, 8 medium-internal, 12 medium-lateral and 4 lateral.
In the immediate post-operative period, all patients presented remission of pain, gradual recovery from radicular deficits or improvement of claudication. At 12-mo follow-up, one patient developed an olisthesis at the level of cystectomy with low back pain. Instability was correlated with an excessive demolition of the articular process. Therefore, stabilization and fusion achieved remission of pain and good long-term outcome. No recurrences or new contralateral or adjacent SGCs were observed.
At long-term follow-up, VAS reduced from 7.4 ± 1.5 (6-10) to 1.3 ± 0.9 (0-2) (P = 0.037). JOA score improved from 7.6 ± 1.3 (7-9) to 2.5 ± 0.3 (0-3) (P = 0.041).
During the second half of the last century, articular cysts of the spine, prevalently lumbar, were likened to those of the wrist, hand, knee and hip and called, in the Greek language, γαγγλιον (ganglion). Hippocrate (460-377 a.C.), translated by Foesio et al[3] in 1596, in the chapter “De Articulis” describes some cutaneous periarticular cysts as “…quae ganglia dominant, quaecunque fluida sunt, et mucosam carnem continent…” (… these so-called ganglion, that contains a fluid or a mucous substance…). In 1930, Elmslie[16], during a knee surgery, observed a communication between the cyst and the synovial membrane, and used for the first time the term “synovial cyst”. In 1968, Kao et al[6] described the first two cases of lumbar intraspinal extradural cyst, calling it “ganglion”. In 1973, Sypert et al[10] referred the possible origin from the synovial cells of the lumbar zygapophyseal joints. In 1974, Kao et al[7], trying to establish terminology and nosology, published a review on spinal ganglion and synovial cysts, grouping them under a single definition: “Juxtafacet synovial cysts”. This term was subsequently adopted by several authors[13,17-22], while others proposed other terms such as “flavum cyst”[8] or cyfmos[9], according respectively to the site of pathology or biomechanics of the mobile spine. They are all essentially correct, in relation to the tissue of origin[6,10], site[7-9] or etiology, but, in our hands, create some confusion. In order to identify this specific pathology in terms of pathogenesis, symptomatology and treatment, we reconsidered the ancient term of “ganglion”: Spinal ganglion cyst (SGC) may be the term of choice if the cyst originates from the articular process: The distinction between ganglion and synovial cyst is in fact purely histological. Psaila and Mansel[23] defined that a ganglion cyst “…mainly consists of sheets of collagen fibers arranged in multidirectional strata” and “the ganglion tissue may be produced by the multifunctional mesenchymal cells”. The main histological feature of the ganglion is the loss of continuity with the capsule of the facet joints, that makes it free inside and/or outside the spinal canal. On the contrary, the real and conserved synovial cyst is always in continuity with the capsule and recurrently presents synovial villi.
SGCs originate from the joint capsule, more precisely from the mesenchymal tissue[23] that constitutes the synovial membrane. This tissue covers the internal face of the capsule and also the external portion of the joint: This extension can explain the intra-articular or extra-articular development of SGCs. On the basis of these considerations, we propose an original classification that distinguishes the cysts between anterior or endocanalar and posterior or extra-canalar. The anterior variety can be subdivided into lateral or foraminal, medium or articular and internal or flavum.
To the best of the authors’ knowledge, a comprehensive classification of SGCs has never been reported. Papers from the literature distinguished between synovial, posterior longitudinal ligament or flavum ligament cysts based on their location, origin or histopathological features. Our paper suggests for the first time the distinction between endo-canalar and extra-canalar SGC: The last one is posterior, generally asymptomatic and do not require treatment[24]. On the contrary, endo-canalar SGC is frequently symptomatic and neurological impairment is closely related to its position within the spinal canal, explaining different disorders ranging from single radiculopathy to cauda equina syndrome.
Factor responsible for proliferation of the synovial cells seems to be repeated articular micro-trauma that induces chronic inflammation, increase of synovial fluid and development of the cyst. Different grades of instability up to olisthesis can favor the weakening of the capsule and ultimately the cystic formation.
We observed lumbar degenerative olisthesis and SGC in more than 40% of our cases. These associated pathologies are frequently reported in the literature, in varying percentages from 30%[13] to 50%[25] of cases. Recently, Boviatsis et al[18], reviewing 499 SGCs, have found disc degeneration, osteoarthritis and spondylolisthesis. Many authors[9,13,18,24-27] underlined that SGCs originate in the most mobile spinal segments, which are more susceptible to micro or macroinstability.
Cysts formation has been also presented in literature as consequence of an adjacent segment syndrome, due to the hypermobility of a segment just above or below other fixed vertebral segments; also in this case the mechanical stress would be the trigger necessary for mesenchimali tissue degeneration[28].
In our series and in the literature[9,13,18,24-26,29,30], SGCs were more frequent at L4-L5, which is notoriously the most mobile spinal level.
Clinical onset of SGCs is generally described as rapid and intense[14,18,19,21,31], characterized by radicular type disturbances, severe impairment of deambulation due to painful symptoms or, less frequently, motor deficits. Occasionally, onset may be extremely acute and intractable due to intracystic hemorrhage. In agreement with other authors[32-34], bleeding in such cysts is caused by neo-formed vessels following the repeated inflammations.
Radiological investigations mainly consist of MRI, which can visualize the SGC and relative degenerative phenomena, such as an increased quantity of “sinovia”, more commonly described as interfacetal fluid, or inflammatory processes involving the interspinous ligament, which appears “shiny” mainly on T2 and STIR sequences[35]. In our series these phenomena were present in all cases, either singly or, more often, in combination.
Conventional radiography can play an important role. Standard load-bearing and flexion-extension X-rays may identify hypermobility or instability otherwise unrecognized: However, the severe painful symptoms sometimes make it impossible to perform this type of pre-operative investigation.
Once a diagnosis of SGC has been made, treatment depends on clinical conditions and neurological symptoms. In the literature[21], outcomes of different conservative treatments are reported. Surgery is indicated in case of severe pain resistant to medical therapy or when neurological deficits are present.
Operative approach has to totally remove the neoformation, taking into account the degree of instability of the spinal level involved by the cyst. Only when one part of the capsule appears tenaciously adherent to the dura mater it is advisable to perform a subtotal excision, to avoid risks of a CSF fistula. Microsurgical cystectomy seems to be able to maintain vertebral stability: Only one case developed vertebral slippage at follow-up. Fusion can be planned on the basis of preoperative investigations in presence of clear instability, as spondylolisthesis, or can be decided during surgery, evaluating the degree of joint demolition in order to achieve nerve roots decompression and radical cystectomy.
We limited posterior instrumented fusion to about a third of our cases, all suffering from spondylolisthesis: In the literature, fusion varies from over 50% of patients[29] to a percentage similar or lower than ours[9,12,13,17,25], whereas in other series surgery was performed without fusion[15,22,30,36,37]. This variability in surgical strategy illustrates how the indication for fusion do not follow common guidelines. As a guide to a common therapeutical strategy, we have laid out a flow-chart (Figure 5), evaluating clinical conditions, mechanical stability and the most suitable treatment.
The long-term outcomes in patients surgically treated are usually good, with complete remission from pre-operative disturbances, in our series as in others[9,11,12,13,17,20,22,25,29,30,36,37]. Only one of our patients presented a symptomatic olisthesis about 1 year after treatment. This iatrogenic deformity, due to an excessive bone demolition, required posterior fusion to achieve resolution of symptoms. In the literature[11,13,19,20,25,30] a similar complication was described with the same low incidence in the majority of the larger case series. A recurrence of an operated cyst is exceptional and only one case is described[13]. The appearance of a new SGC, contralateral, higher or lower, is more frequent and occurred in 15 cases[13,17,19,20,22,29,38]. No recurrences were observed in our case series.
In conclusion, spinal ganglion cysts are generally found in the lumbar spine. Over the past decades, a wide variety of terms used to describe them has generated confusion: For this reason, the authors decided to return to the ancient definition of “ganglion cyst”. Their origin into the spine seems to be attributable to inflammatory phenomena, involving the synovial membrane and caused by repeated joint microtraumas, promoted by facet hypermobility or clear instability. The treatment of choice is microsurgical cystectomy, which generally does not require fusion. The need for fusion must be carefully evaluated: Pre-operative spondylolisthesis or a wide bone joint demolition are the main indications for fusion procedures. The proposal morphologic classification of SGCs is the first that clarifies different localizations of these cysts and may be clinically useful for radiologists and surgeons, together with the definition of ganglion, to speak the same scientific language.
Ganglion cysts of the minor and major joints, especially at the level of the wrist and back of the hand, have been known since ancient times. These cysts have a high incidence. In the past century, similar cysts were also described as originated from lumbar zygapophyseal joints and occupying the spinal canal, most frequently in the lumbar spine and occasionally, in the cervical and thoracic spine. To define these spinal neoformations, many terms have been adopted in the literature, according to the site of development or to the supposed origin: Ganglion, juxtafacet, flavum, cyfmos and synovial.
The etiology of the cyst was related to inflammatory phenomena secondary to facet hypermobility, which would produce modifications of the articular synovial membrane leading to cyst formation. Microsurgical cystectomy is today the treatment of choice. Generally, microsurgical approach does not produce vertebral instability and arthrodesis is required only in case of a clear pre-operative instability.
Evaluating all etiological factors and all treatment options, the authors propose an original morphological classification of lumbar ganglion cysts, based on their relation with the other anatomical structures. Lastly, in order to clarify the confusing terminology that describes these particular cysts, the authors suggest “spinal ganglion cyst” (SGC) as definitive term to be applied in clinical practice.
The proposal morphologic classification of SGCs is the first that clarifies different localizations of these cysts and may be clinically useful for radiologists and surgeons, together with the definition of ganglion, to speak the same scientific language.
The authors present a case series and a proposed standardized language for lumbar ganglion cysts. The paper is generally well-written and easy to read.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Italy
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Petersen SMB S- Editor: Kong JX L- Editor: A E- Editor: Lu YJ
| 1. | Burke FD, Melikyan EY, Bradley MJ, Dias JJ. Primary care referral protocol for wrist ganglia. Postgrad Med J. 2003;79:329-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Carp L, Stout AP. Branchial Anomalies And Neoplasms: A Report Of Thirty-Two Cases With Follow-Up Results. Ann Surg. 1928;87:186-209. [PubMed] |
| 3. | Foesio A, De articulis. Magni hippocratis medicorum omnium facile principis, opera omnia quae extant in VIII sectiones ex Erotiani mente distributa. Francofurti, 1596: 840-841. |
| 4. | Song JK, Musleh W, Christie SD, Fessler RG. Cervical juxtafacet cysts: case report and literature review. Spine J. 2006;6:279-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Graham E, Lenke LG, Hannallah D, Lauryssen C. Myelopathy induced by a thoracic intraspinal synovial cyst: case report and review of the literature. Spine (Phila Pa 1976). 2001;26:E392-E394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Kao CC, Uihlein A, Bickel WH, Soule EH. Lumbar intraspinal extradural ganglion cyst. J Neurosurg. 1968;29:168-172. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 142] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 7. | Kao CC, Winkler SS, Turner JH. Synovial cyst of spinal facet. Case report. J Neurosurg. 1974;41:372-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 187] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 8. | Vernet O, Fankhauser H, Schnyder P, Déruaz JP. Cyst of the ligamentum flavum: report of six cases. Neurosurgery. 1991;29:277-283. [PubMed] |
| 9. | Christophis P, Asamoto S, Kuchelmeister K, Schachenmayr W. “Juxtafacet cysts”, a misleading name for cystic formations of mobile spine (CYFMOS). Eur Spine J. 2007;16:1499-1505. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Sypert GW, Leech RW, Harris AB. Posttraumatic lumbar epidural true synovial cyst. Case report. J Neurosurg. 1973;39:246-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Freidberg SR, Fellows T, Thomas CB, Mancall AC. Experience with symptomatic spinal epidural cysts. Neurosurgery. 1994;34:989-993; discussion 993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 56] [Article Influence: 1.8] [Reference Citation Analysis (1)] |
| 12. | Howington JU, Connolly ES, Voorhies RM. Intraspinal synovial cysts: 10-year experience at the Ochsner Clinic. J Neurosurg. 1999;91:193-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 66] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 13. | Sabo RA, Tracy PT, Weinger JM. A series of 60 juxtafacet cysts: clinical presentation, the role of spinal instability, and treatment. J Neurosurg. 1996;85:560-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 132] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Yarde WL, Arnold PM, Kepes JJ, O’Boynick PL, Wilkinson SB, Batnitzky S. Synovial cysts of the lumbar spine: diagnosis, surgical management, and pathogenesis. Report of eight cases. Surg Neurol. 1995;43:459-464; discussion 465. [PubMed] |
| 15. | Landi A, Marotta N, Tarantino R, Ruggeri AG, Cappelletti M, Ramieri A, Domenicucci M, Delfini R. Microsurgical excision without fusion as a safe option for resection of synovial cyst of the lumbar spine: long-term follow-up in mono-institutional experience. Neurosurg Rev. 2012;35:245-253; discussion 253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 16. | Elmslie RC. Cyst of Synovial Membrane in the Region of the Internal Semilunar Cartilage. Proc R Soc Med. 1930;23:1586-1587. [PubMed] |
| 17. | Banning CS, Thorell WE, Leibrock LG. Patient outcome after resection of lumbar juxtafacet cysts. Spine (Phila Pa 1976). 2001;26:969-972. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 69] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 18. | Boviatsis EJ, Stavrinou LC, Kouyialis AT, Gavra MM, Stavrinou PC, Themistokleous M, Selviaridis P, Sakas DE. Spinal synovial cysts: pathogenesis, diagnosis and surgical treatment in a series of seven cases and literature review. Eur Spine J. 2008;17:831-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 122] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 19. | Epstein NE. Lumbar laminectomy for the resection of synovial cysts and coexisting lumbar spinal stenosis or degenerative spondylolisthesis: an outcome study. Spine (Phila Pa 1976). 2004;29:1049-1055; discussion 1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 49] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Métellus P, Fuentes S, Adetchessi T, Levrier O, Flores-Parra I, Talianu D, Dufour H, Bouvier C, Manera L, Grisoli F. Retrospective study of 77 patients harbouring lumbar synovial cysts: functional and neurological outcome. Acta Neurochir (Wien). 2006;148:47-54; discussion 54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 73] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 21. | Shah RV, Lutz GE. Lumbar intraspinal synovial cysts: conservative management and review of the world’s literature. Spine J. 2003;3:479-488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 92] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 22. | Trummer M, Flaschka G, Tillich M, Homann CN, Unger F, Eustacchio S. Diagnosis and surgical management of intraspinal synovial cysts: report of 19 cases. J Neurol Neurosurg Psychiatry. 2001;70:74-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 59] [Article Influence: 2.5] [Reference Citation Analysis (1)] |
| 23. | Psaila JV, Mansel RE. The surface ultrastructure of ganglia. J Bone Joint Surg Br. 1978;60-B:228-233. [PubMed] |
| 24. | Doyle AJ, Merrilees M. Synovial cysts of the lumbar facet joints in a symptomatic population: prevalence on magnetic resonance imaging. Spine (Phila Pa 1976). 2004;29:874-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 114] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 25. | Lyons MK, Atkinson JL, Wharen RE, Deen HG, Zimmerman RS, Lemens SM. Surgical evaluation and management of lumbar synovial cysts: the Mayo Clinic experience. J Neurosurg. 2000;93:53-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 80] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 26. | Choudhri HF, Perling LH. Diagnosis and management of juxtafacet cysts. Neurosurg Focus. 2006;20:E1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 27. | Khan AM, Girardi F. Spinal lumbar synovial cysts. Diagnosis and management challenge. Eur Spine J. 2006;15:1176-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 87] [Article Influence: 4.6] [Reference Citation Analysis (1)] |
| 28. | Miscusi M, Petrozza V, Polli FM, Forcato S, Rocca CD, Raco A. Symptomatic ganglion cyst of ligamentum flavum as a late complication of lumbar fixation. Neurol Neurochir Pol. 2012;46:82-86. [PubMed] |
| 29. | Khan AM, Synnot K, Cammisa FP, Girardi FP. Lumbar synovial cysts of the spine: an evaluation of surgical outcome. J Spinal Disord Tech. 2005;18:127-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 94] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 30. | Sandhu FA, Santiago P, Fessler RG, Palmer S. Minimally invasive surgical treatment of lumbar synovial cysts. Neurosurgery. 2004;54:107-111; discussion 111-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 75] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 31. | Salmon B, Martin D, Lenelle J, Stevenaert A. Juxtafacet cyst of the lumbar spine. Clinical, radiological and therapeutic aspects in 28 cases. Acta Neurochir (Wien). 2001;143:129-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 32. | Ramieri A, Domenicucci M, Seferi A, Paolini S, Petrozza V, Delfini R. Lumbar hemorrhagic synovial cysts: diagnosis, pathogenesis, and treatment. Report of 3 cases. Surg Neurol. 2006;65:385-390, discussion 390. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 34] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 33. | Arantes M, Silva RS, Romão H, Resende M, Moniz P, Honavar M, Costa M. Spontaneous hemorrhage in a lumbar ganglion cyst. Spine (Phila Pa 1976). 2008;33:E521-E524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 34. | Tatter SB, Cosgrove GR. Hemorrhage into a lumbar synovial cyst causing an acute cauda equina syndrome. Case report. J Neurosurg. 1994;81:449-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 66] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 35. | Keorochana G, Taghavi CE, Tzeng ST, Morishita Y, Yoo JH, Lee KB, Liao JC, Wang JC. Magnetic resonance imaging grading of interspinous ligament degeneration of the lumbar spine and its relation to aging, spinal degeneration, and segmental motion. J Neurosurg Spine. 2010;13:494-499. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 36. | Hsu KY, Zucherman JF, Shea WJ, Jeffrey RA. Lumbar intraspinal synovial and ganglion cysts (facet cysts). Ten-year experience in evaluation and treatment. Spine (Phila Pa 1976). 1995;20:80-89. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 205] [Cited by in RCA: 168] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 37. | Sehati N, Khoo LT, Holly LT. Treatment of lumbar synovial cysts using minimally invasive surgical techniques. Neurosurg Focus. 2006;20:E2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 30] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 38. | Pirotte B, Gabrovsky N, Massager N, Levivier M, David P, Brotchi J. Synovial cysts of the lumbar spine: surgery-related results and outcome. J Neurosurg. 2003;99:14-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 0.9] [Reference Citation Analysis (0)] |