Published online Apr 18, 2017. doi: 10.5312/wjo.v8.i4.310
Peer-review started: April 6, 2016
First decision: May 17, 2016
Revised: February 7, 2017
Accepted: February 28, 2017
Article in press: March 2, 2017
Published online: April 18, 2017
Processing time: 379 Days and 15.1 Hours
To provide a “patient-normalized” parameter in the proximal forearm.
Sixty-three cadaveric upper extremities from thirty-five cadavers were studied. A muscle splitting approach was utilized to locate the posterior interosseous nerve (PIN) at the point where it emerges from beneath the supinator. The supinator was carefully incised to expose the midpoint length of the nerve as it passes into the forearm while preserving the associated fascial connections, thereby preserving the relationship of the nerve with the muscle. We measured the transepicondylar distance (TED), PIN distance in the forearm’s neutral rotation position, pronation position, supination position, and the nerve width. Two individuals performed measurements using a digital caliper with inter-observer and intra-observer blinding. The results were analyzed with the Wilcoxon-Mann-Whitney test for paired samples.
In pronation, the PIN was within two confidence intervals of 1.0 TED in 95% of cases (range 0.7-1.3 TED); in neutral, within two confidence intervals of 0.84 TED in 95% of cases (range 0.5-1.1 TED); in supination, within two confidence intervals of 0.72 TED in 95% of cases (range 0.5-0.9 TED). The mean PIN distance from the lateral epicondyle was 100% of TED in a pronated forearm, 84% in neutral, and 72% in supination. Predictive accuracy was highest in supination; in all cases the majority of specimens (90.47%-95.23%) are within 2 cm of the forearm position-specific percentage of TED. When comparing right to left sides for TEDs with the signed Wilcoxon-Mann-Whitney test for paired samples as well as a significance test (with normal distribution), the P-value was 0.0357 (significance - 0.05) indicating a significant difference between the two sides.
This “patient normalized” parameter localizes the PIN crossing a line drawn between the lateral epicondyle and the radial styloid. Accurate PIN localization will aid in diagnosis, injections, and surgical approaches.
Core tip: We present a “patient normalized” parameter that localizes posterior interosseous nerve (PIN) crossing point with a line interconnecting the lateral epicondyle and the radial styloid, with the “70-85-100” rule. The mean PIN distance from the lateral epicondyle was 100% of transepicondylar distance (TED) in a pronated forearm, 85% in neutral, and 70% in supination. Predictive accuracy was highest in supination; in all cases the majority of specimens (90.47%-95.23%) are within 2 cm of the forearm position-specific percentage of TED. Non-invasive accurate PIN localization will aid in diagnosis, injections, surgical approaches, and understanding neurological symptoms in the forearm.
- Citation: Kamineni S, Norgren CR, Davidson EM, Kamineni EP, Deane AS. Posterior interosseous nerve localization within the proximal forearm - a patient normalized parameter. World J Orthop 2017; 8(4): 310-316
- URL: https://www.wjgnet.com/2218-5836/full/v8/i4/310.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i4.310
The radial nerve’s localization has been the subject of much concern due to the potential for pathologic[1,2], traumatic[3,4], and iatrogenic[5-7] injuries. Radial nerve localization has been described relative to a distance from various bony landmarks: The acromion and lateral epicondyle[8] proximal to the elbow and the bicipital tuberosity distal to the elbow[9]. The deep radial nerve [posterior interosseous nerve (PIN)] has proven more difficult to localize distal to the elbow. Accurately localizing PIN in the proximal forearm is important when diagnosing nerve compression with physical examination, placing injections at the site of the nerve, accurately exposing the nerve during a surgical exposure[10], and reducing the incidence of iatrogenic nerve injury during surgical interventions[11-17]. Specifically, the surgical repair of open and closed injuries to the elbow/forearm, relief of entrapment neuropathies, and implantation of fixation devices for fracture stabilization all require intimate knowledge of PIN anatomy[8,10,13,17,18]. The general course of PIN has previously been described in detail in relation to muscular anatomy and by using absolute measurement from a bony landmark[8,9,11,14,16,19,20]. These descriptors serve a useful function for the general anatomic understanding of PIN location, but have their limitations. They are limited because muscular anatomy must be defined first, which limits its usefulness to surgical interventions with this capacity, such as open surgical dissection. Descriptors utilizing a specific measurement from a bony landmark can be difficult to use clinically due to body habitus or because the bony landmark is outside of the surgical field. An absolute measurement does not normalize for a particular individual and can lead to erroneous localization. This latter issue is based on the wide range of variability in body sizes. Thus, localization of PIN in the proximal forearm utilizing a patient-normalized parameter is advantageous when dealing with an individual person.
Surgical landmarks traditionally used to localize PIN in the forearm (such as the bicipital tuberosity, articular surface of the posterior supinator head, and the entry and exit points of the supinator muscle) require invasive surgical exploration of the area for accurate use of the parameter[9,11,14,20,21]. The establishment of a non-invasive parameter using external anatomical landmarks would be beneficial by localizing PIN without invasive dissection and could potentially reduce the incidence of iatrogenic PIN injury.
We propose that the transepicondylar distance (TED) are, utilized as a body size descriptor and normalizing feature, can be used as a non-invasive parameter for PIN localization in the proximal forearm. In this study, we calculate PIN distance from the lateral humeral epicondyle as a percentage of TED and examine the predictive accuracy of this parameter in localizing PIN in three forearm positions: Pronation, supination, and neutral. We expect this information will be useful to guide surgical techniques in a more patient-specific manner, which may ultimately reduce surgical morbidities.
Approval was obtained from the Department of Anatomy in the College of Medicine at our University to collect morphometric data describing PIN position from cadavers. The procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation.
Skin was removed from 35 cadavers utilizing 63 upper extremities. A muscle splitting approach was utilized to locate PIN at the point where it emerges from beneath the supinator. The supinator was carefully incised to expose the midpoint length of the nerve as it passes into the forearm while preserving the associated fascial connections, thereby preserving the relationship of the nerve with the muscle.
TED: The medial and lateral epicondyles of the humerus were palpated to identify the maximum medial and lateral extensions of the humeral epicondyles. The distance between these points was measured using Mituyoto digital calipers. Maximum TED was measured on three separate occasions by two separate observers for a total of six measurements.
PIN distance: The distance between the lateral humeral epicondyle apex and the proximal and distal borders of PIN were recorded for each cadaver with the forearm in a pronated, supinated and neutral position along an interconnecting line between the lateral epicondyle and radial styloid tip (“epi-styloid line”). PIN position was measured by establishing the position of the lateral humeral epicondyle and then extending a length of inelastic string (0.5 mm diameter) from that point to the radial styloid process, following the surface contour of the forearm. Distances were recorded from the lateral epicondyle to the proximal intersection of PIN with the string and between the lateral epicondyle and the distal intersection of PIN with the guide string. Proximal and distal PIN positions were each measured on three separate occasions by two observers for a total of six proximal and six distal PIN measurements. PIN distance from the epicondyle was recorded as the distance from the epicondyle to the midpoint between the proximal and distal intersection of PIN with the guide string.
PIN width: The total difference between the proximal and distal intersection of PIN with the guide string.
Summary descriptive statistics (i.e., mean, standard deviation, range) were calculated for all individual PIN distance measurements and for all individual PIN distance measurements when calculated as a percentage of TED. We conducted the signed Wilcoxon-Mann-Whitney test for paired samples as well as a significance test (with normal distribution) for paired samples in order to compare difference between right and left sides of TED lengths, pronated position, supinated position, and neutral position. The distances of PIN from the lateral epicondyle, with respect to TED, were plotted with 95%CIs, using normal, long normal, Weibull, and Gamma distributions.
The mean TED for all elbows was 63.59 mm (range 53.0-80 mm). The mean left elbow TED was 62.92 mm (range 53-80 mm), and the mean right TED was 63.97 mm (range 54-77 mm). When comparing right to left sides for TEDs with the signed Wilcoxon-Mann-Whitney test for paired samples as well as a significance test (with normal distribution), the P-value was 0.0357 (significance - 0.05) indicating a significant difference between the two sides. However, when comparing the measurements by different observers, as a measure of inter-observer differences of measurements taken, all P-values were greater than 0.29 indicating no significance was detected.
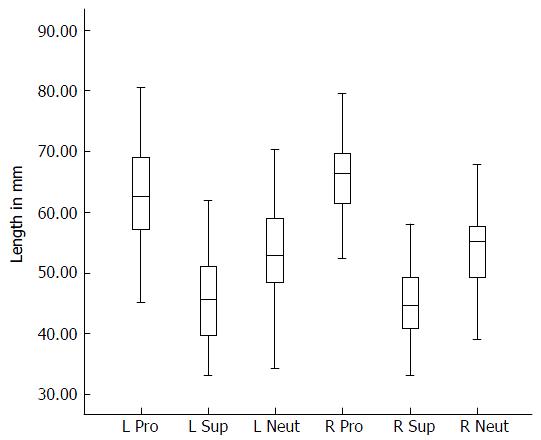
Mean radial nerve distances from the lateral epicondyle were greatest when the forearm was in a pronated position [63 mm (range 34.5-80.6 mm)] and least when the forearm was in a supinated position [45.7 mm (33-61.9 mm)]. Mean radial nerve distances when the forearm was in a neutral position [53.5 mm (34.3-70.6 mm)] was intermediate to the values reported for the pronated and supinated forearm (Figure 1).
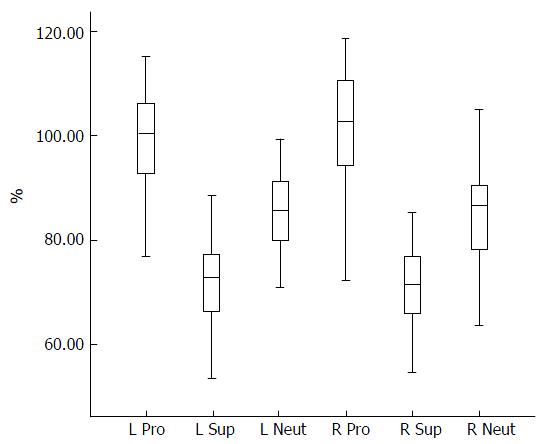
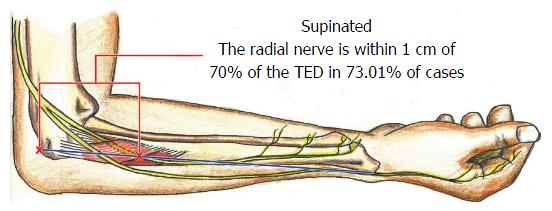
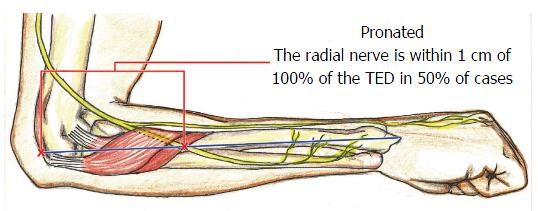
We calculated the location of PIN along the epi-styloid line as a percentage of TED for that same specimen. In neutral forearm rotation the radial nerve was located at 85% of TED [range 65% (4.1 cm) to 105% (6.6 cm) TED]. In supination it was located at 70% of TED [range 50% (3.15 cm) to 90% (5.7 cm) TED], and in pronation was 100% of TED [range 70% (4.4 cm) to 120% (7.6 cm) TED] (Figure 2).
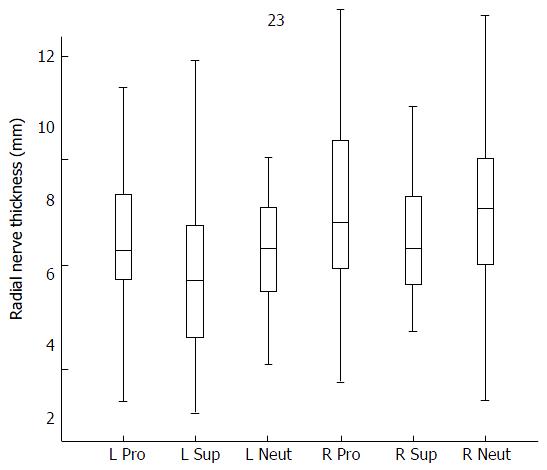
Radial nerve width (i.e., the distance between the proximal and distal intersection of the nerve with the guide string) was observed to vary across cadavers. Figure 3 represents boxplots of sample median, standard deviation and range for all forearm positions in both the left and right upper limb (Figure 3).
Mean PIN distance as a percentage of TED was greatest when the forearm is pronated (98.7%-101.4%) and least when the forearm was supinated (71.7%-72.6%). Mean PIN distance as a percentage of TED when the forearm was in a neutral position (84.4%-84.7%) were intermediate to the values reported for the pronated and supinated forearm.
PIN distances recorded when the forearm was pronated, supinated, and in neutral rotation were used to predict PIN position relative to the lateral epicondyle. The mean distance between the lateral epicondyle and proximal intersection of PIN and guide string was used to establish predictive lengths for each of the three forearm positions. When the forearm was pronated the mean PIN distance was 100% of TED. In the supinated position the mean PIN distance was 70% of TED. When the arm is in a neutral position the mean posterior interosseous distance was approximately 85% of TED. These percentages were applied to the individual cadavers to establish a “Predictive Value” for PIN localization.
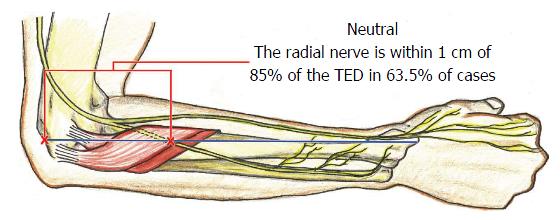
When the arm was pronated PIN was located within 1.5 cm of 1.0 × TED in 71.43% of the specimens and within 2 cm in 90.47% of specimens. The predictive accuracy was highest when the arm was supinated. PIN was identified within 1 cm of 0.7 × TED in 73.01% of cadavers, and within 1.5 cm in 85.7% of cadavers and within 2 cm in 95.23% of cadavers. When the forearm was in neutral rotation PIN was within 1 cm of 0.85 × TED in 63.5% of specimens, 1.5 cm in 84.12%, and within 2 cm in 93.7% of proximal forearms.
Our study introduces a non-invasive, patient-normalized parameter for localizing PIN in the proximal forearm within 2 cm of the predicted distance from the lateral humeral epicondyle with 90%-95% accuracy in three positions of forearm rotation. TED has previously been utilized to normalize radial nerve localization proximal to the elbow, to help prevent radial nerve injury when placing pins/screws[22], as has the bicipital tuberosity[9] distal to the elbow. We have demonstrated that the mean PIN distance relative to TED is approximately 85% in neutral (Figure 4), 70% when supinated (Figure 5), and 100% when pronated (Figure 6).
There are several potential limitations to consider when evaluating this “70-85-100” guideline. These issues include the use of cadavers, variable branching patterns, inter-individual differences, and the value of this parameter compared to using absolute values for localization of PIN.
Anatomical investigations often use cadavers for data collection, but some studies use formalin-embalmed cadavers while others use fresh specimens. While it is unclear how the embalming process would significantly alter anatomical relationships, Artico et al[8] postulated that differences in the distances of PIN to various landmarks in their study vs other literature can be explained by the use of either fresh cadaver specimens or formalin-embalmed cadavers. While fresh cadaver specimens likely preserve normal anatomy more accurately than embalmed ones, we believe the relatively large sample size of our study (n = 63) increases the power of our data such that the correlations we have found are true. However, future research with fresh cadaver specimens may be valuable in supporting or refuting our findings.
There were significant variations in the branching patterns of the deep PIN within the supinator muscle that made localization less precise even though care was taken during the dissection to preserve as much surrounding fascial tissue as possible with minimal disruption of anatomical relationships. This is reflected by the wide ranges of PIN widths (Figure 3) as determined by the distance from the lateral epicondyle to the proximal and distal edges of where the guide string crossed PIN. The inclusion of some, but not all, branches as part of the main PIN trunk led to some subjective interpretation of which branches were “too far” or “too small” to include. Variability in nerve sizes and branching patterns contributed to a wide range of widths which could affect the calculated mean distances of the “midpoint” of the nerve to the lateral epicondyle. A suggestion for future research would be to focus on the “safe zone” of where surgical incisions are less likely to damage PIN or any of its branches as opposed to direct PIN localization.
Intra-individual variation between right and left upper extremities is not well predicted by our “70-85-100” rule. Despite the fact that most people have similar right and left TED’s, this does not necessarily mean that their PINs have symmetric courses. Benham et al[23] found that there were significant intra-individual differences between the right and left limb in the distance from the lateral epicondyle to the bifurcation point of PIN into its superficial and deep branches. While this finding may have important clinical implications, it may not be relevant for deep PIN localization because their study uses a different point of measurement and our study found no significant difference between the right and left measurements in any of the three forearm positions. While intra-individual variation may exist at the bifurcation point of the superficial and deep PIN branches, it does not likely play a role in the localization of the deep PIN within the supinator muscle.
TED was measured after skin removal, which resulted in an over-estimation when assessing PIN in situ. However, our method provides a good estimation of PIN localization as the effect of skin thickness is likely negligible when using the parameter non-surgically (skin intact state).
Although our proposed localizing parameter is patient-normalized using TED, it may not be any more specific than using the absolute values provided by previous research. It is important to note that our “70-85-100” rule predicts the location of PIN within 1 cm in only 50% of cases when pronated, 63.5% when neutral, and 73.1% when supinated. Only when the range is increased to 2 cm does it include 90%-95% of cases, which is no more specific or accurate than the average values and ranges calculated from numerous specimens. For example, Strauch et al[11] found the average distance from the posterior interosseous tuberosity to PIN is 2.3 cm with a total range of only 1.4 cm (1.8 cm-3.2 cm). Witt et al[9] discovered the distance from the first branches of PIN to the articular surface of the posterior interosseous head are 6.0 cm ± 1 cm (range 4.0-8.4 cm). Thomas et al[14] reported that the bifurcation of PIN into its superficial and deep branches is 8.0 cm ± 1.9 cm distal to the lateral intermuscular septum and 3.6 cm ± 0.7 cm proximal to the leading edge of the supinator (Arcade of Froshe). While these studies use different landmarks, they all have ranges of < 2 cm when reporting absolute values for localizing PIN. Therefore, our patient-normalized parameter may be no more specific or individualized than absolute values for localizing PIN, but it still has the advantage of being non-invasive.
Our study has limitations that should be considered when utilizing it in the clinical setting. These were cadaveric specimens which may differ from patients in their musculoskeletal relationships as a consequence of the preservation procedure. The line connecting the lateral epicondyle and radial styloid was not a projected straight line, but a straight line following the contour of the forearm and may be influenced by the individual bulk of the forearm, which was not investigated in this study. Previous trauma or surgical procedures in the territory could influence this parameter.
We would like to thank the Department of Orthopaedics and Sports Medicine, the University of Kentucky College of Medicine, and the Department of Anatomy and Neurobiology for contributions in time and materials towards this project. We also thank Dr. Ruriko R for her help with with the statistics.
The authors describe a simple method, based on cadaveric data and corroborated in clinical practice, of locating the posterior interosseous nerve (PIN) in the proximal forearm. The location of the PIN can be simply summarized by the 70-85-100 rule. They have demonstrated that the location of the PIN from the lateral epicondyle, in terms of the patient’s transepicondylar distance (TED) is approximately 70%TED with forearm supination, 85%TED in neutral forearm rotation, and 100%TED when pronated. This will help clinicians to localize the PIN when dealing with a proximal forearm painful differential diagnosis, injections around the PIN for diagnostic and therapeutic purposes, and when surgically approaching the PIN for a decompressive operation.
The PIN is increasingly recognized as a differential diagnosis and a coexistent pathology in tennis elbow. The ability to locate the PIN accurately in relation to the patient’s own anatomy is a very important step towards an accurate diagnosis.
The significant innovation of the study is that they are able to locate the PIN by “normalizing” their measurement to the patient’s own anatomy. The authors’ normalizing parameter is the TED, which can easily be measured by the clinician.
The practical application of their study is that it accurately locates the PIN, it normalizes the location of this nerve to the patient’s own anatomy, helps in the diagnosis of lateral elbow and forearm pain, improves the localization of diagnostic and therapeutic injections around the PIN, and helps the surgeon decrease in the size of the incision when decompressing the PIN.
TED: The distance between the most prominent part of the medial and lateral epicondyle.
This is a very well presented study.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Drosos GI, Matuszewski LS S- Editor: Ji FF L- Editor: A E- Editor: Li D
| 1. | Jou IM, Wang HN, Wang PH, Yong IS, Su WR. Compression of the radial nerve at the elbow by a ganglion: two case reports. J Med Case Rep. 2009;3:7258. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Nelson G. Radial nerve compression due to lipoma. J Vis Commun Med. 2007;30:191-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Chesser TJ, Leslie IJ. Radial nerve entrapment by the lateral intermuscular septum after trauma. J Orthop Trauma. 2000;14:65-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Banskota A, Volz RG. Traumatic laceration of the radial nerve following supracondylar fracture of the elbow. A case report. Clin Orthop Relat Res. 1984;150-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Haapaniemi T, Berggren M, Adolfsson L. Complete transection of the median and radial nerves during arthroscopic release of post-traumatic elbow contracture. Arthroscopy. 1999;15:784-787. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 103] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Caldwell JM, Kim HM, Levine WN. Radial nerve injury associated with application of a hinged elbow external fixator: a report of 2 cases. J Shoulder Elbow Surg. 2013;22:e12-e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Marcu DM, Balts J, McCarthy JJ, Kozin SH, Noonan KJ. Iatrogenic radial nerve injury with cannulated fixation of medial epicondyle fractures in the pediatric humerus: a report of 2 cases. J Pediatr Orthop. 2011;31:e13-e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Artico M, Telera S, Tiengo C, Stecco C, Macchi V, Porzionato A, Vigato E, Parenti A, De Caro R. Surgical anatomy of the radial nerve at the elbow. Surg Radiol Anat. 2009;31:101-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 25] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Witt JD, Kamineni S. The posterior interosseous nerve and the posterolateral approach to the proximal radius. J Bone Joint Surg Br. 1998;80:240-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Ducic I, Felder JM, Quadri HS. Common nerve decompressions of the upper extremity: reliable exposure using shorter incisions. Ann Plast Surg. 2012;68:606-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Strauch RJ, Rosenwasser MP, Glazer PA. Surgical exposure of the dorsal proximal third of the radius: how vulnerable is the posterior interosseous nerve? J Shoulder Elbow Surg. 1996;5:342-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Tabor OB, Bosse MJ, Sims SH, Kellam JF. Iatrogenic posterior interosseous nerve injury: is transosseous static locked nailing of the radius feasible? J Orthop Trauma. 1995;9:427-429. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Catalano LW, Zlotolow DA, Hitchcock PB, Shah SN, Barron OA. Surgical exposures of the radius and ulna. J Am Acad Orthop Surg. 2011;19:430-438. [PubMed] |
| 14. | Thomas SJ, Yakin DE, Parry BR, Lubahn JD. The anatomical relationship between the posterior interosseous nerve and the supinator muscle. J Hand Surg Am. 2000;25:936-941. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 67] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | Lindenhovius AL, Felsch Q, Ring D, Kloen P. The long-term outcome of open reduction and internal fixation of stable displaced isolated partial articular fractures of the radial head. J Trauma. 2009;67:143-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Heidari N, Kraus T, Weinberg AM, Weiglein AH, Grechenig W. The risk injury to the posterior interosseous nerve in standard approaches to the proximal radius: a cadaver study. Surg Radiol Anat. 2011;33:353-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Tornetta P, Hochwald N, Bono C, Grossman M. Anatomy of the posterior interosseous nerve in relation to fixation of the radial head. Clin Orthop Relat Res. 1997;215-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 38] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Clavert P, Lutz JC, Adam P, Wolfram-Gabel R, Liverneaux P, Kahn JL. Frohse’s arcade is not the exclusive compression site of the radial nerve in its tunnel. Orthop Traumatol Surg Res. 2009;95:114-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 19. | Diliberti T, Botte MJ, Abrams RA. Anatomical considerations regarding the posterior interosseous nerve during posterolateral approaches to the proximal part of the radius. J Bone Joint Surg Am. 2000;82:809-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 64] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 20. | Tubbs RS, Salter EG, Wellons JC, Blount JP, Oakes WJ. Superficial surgical landmarks for identifying the posterior interosseous nerve. J Neurosurg. 2006;104:796-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 21. | Prasartritha T, Liupolvanish P, Rojanakit A. A study of the posterior interosseous nerve (PIN) and the radial tunnel in 30 Thai cadavers. J Hand Surg Am. 1993;18:107-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 59] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Kamineni S, Ankem H, Patten DK. Anatomic relationship of the radial nerve to the elbow joint: clinical implications of safe pin placement. Clin Anat. 2009;22:684-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Benham A, Introwicz B, Waterfield J, Sim J, Derricott H, Mahon M. Intra-individual variations in the bifurcation of the radial nerve and the length of the posterior interosseous nerve. Man Ther. 2012;17:22-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |