Published online Mar 18, 2017. doi: 10.5312/wjo.v8.i3.271
Peer-review started: October 11, 2016
First decision: November 17, 2016
Revised: November 18, 2016
Accepted: December 16, 2016
Article in press: December 19, 2016
Published online: March 18, 2017
Processing time: 159 Days and 11.3 Hours
To evaluate the role of dynamic computed tomography (CT) scan imaging in diagnosing craniovertebral junction (CVJ) instability in patients with congenital CVJ malformations.
Patients with symptomatic congenital CVJ malformations who underwent posterior fossa decompression and had a preoperative dynamic CT scan in flexion and extended position were included in this study. Measurements of the following craniometrical parameters were taken in flexed and extended neck position: Atlanto-dental interval (ADI), distance of the odontoid tip to the Chamberlain’s line, and the clivus-canal angle (CCA). Assessment of the facet joints congruence was also performed in both positions. Comparison of the values obtained in flexion and extension were compared using a paired Student’s t-test.
A total of ten patients with a mean age of 37.9 years were included. In flexion imaging, the mean ADI was 1.76 mm, the mean CCA was 125.4° and the mean distance of the odontoid tip to the Chamberlain’s line was + 9.62 mm. In extension, the mean ADI was 1.46 mm (P = 0.29), the mean CCA was 142.2° (P < 0.01) and the mean distance of the odontoid tip to the Chamberlain’s line was + 7.11 mm (P < 0.05). Four patients (40%) had facetary subluxation demonstrated in dynamic imaging, two of them with mobile subluxation (both underwent CVJ fixation). The other two patients with a fixed subluxation were not initially fixed. One patient with atlantoaxial assimilation and C23 fusion without initial facet subluxation developed a latter CVJ instability diagnosed with a dynamic CT scan. Patients with basilar invagination had a lower CCA variation compared to the whole group.
Craniometrical parameters, as well as the visualization of the facets location, may change significantly according to the neck position. Dynamic imaging can provide additional useful information to the diagnosis of CVJ instability. Future studies addressing the relationship between craniometrical changes and neck position are necessary.
Core tip: This study shows the importance of the dynamic image in patients with congenital craniovertebral junction anomalies. A total of ten patients with a mean age of 37.9 years were included. We could demonstrate that 40% of the patients had facetary subluxation demonstrated in dynamic imaging and two of them required surgery for craniovertebral junction due to instability. This study reported the importance of routine dynamic imaging evaluation in patients with craniovertebral junction anomalies even without evidence of instability in static computed tomography scan or magnetic resonance imaging.
- Citation: da Silva OT, Ghizoni E, Tedeschi H, Joaquim AF. Role of dynamic computed tomography scans in patients with congenital craniovertebral junction malformations. World J Orthop 2017; 8(3): 271-277
- URL: https://www.wjgnet.com/2218-5836/full/v8/i3/271.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i3.271
Basilar invagination (BI) is a congenital craniovertebral junction (CVJ) malformation characterized by the ascension of the upper cervical spine into the skull base and can be associated with other bone anomalies, such as atlas assimilation, Klippel-Feil syndrome, condyle hypoplasia and atlanto-axial instability[1-4]. BI is generally diagnosed when the tip of the odontoid process is at least 5 mm above the Chamberlain’s line (a line traced from the posterior edge of the hard palate to the posterior margin of the foramen magnum)[5].
Surgical treatment of BI is well accepted in the setting of clinical symptoms[6,7]. Symptoms are usually caused by tonsillar herniation, brainstem/upper cervical spine compression and/or CVJ instability, which should be recognized by the surgeon before planning the surgical strategy[3,7,8].
Increased atlanto-dens interval, atlanto-axial dislocation (AAD), and the tip of the odontoid above the McRae’s line (a line drawn from the basion to the opistium), are clear signs of CVJ instability[8], therefore, in such cases, stabilization concomitant to neural structures decompression is generally recommended[8,9].
However, some patients may present symptoms of BI with a relative normal or near normal CVJ alignment[4]. For those patients, dynamic craniovertebral junction computed tomography (CT) scans with sagittal reconstructions can provide detailed information about the facet joints and CVJ alignment, as well as showing abnormal motion of the CVJ suggestive of instability.
Dynamic imaging (such as CT or magnetic resonance imaging in flexion and extension) is commonly used in traumatic spinal diseases, although the literature is relative scarce about its use in CVJ malformations[10]. Considering the potential benefits of dynamic CT scans in patients with CVJ without clear and evident instability, we proposed to evaluate our experience with this exam in our practice.
We performed a retrospective study of our database of patients with CVJ who underwent surgical treatment from 2010 to 2016 by the same surgeon (AFJ).
Symptomatic congenital CVJ malformation: Chiari Malformation (CM), characterized by tonsillar herniation through the foramen magnum or BI with or without CM who underwent posterior fossa decompression; age > 15 years old (younger patients have incomplete ossification of the region and were excluded)[11]; a complete sagittal CT scan of the CVJ in flexion and in extension (a head holder was used to flex the neck and a pad roll was placed below the shoulders for the extended position); non evident AAD or facet subluxation on static radiological exams.
Patients were followed by the same surgeon (AFJ). Neurologic status (pre and post-surgery as well as during the follow-up) was assessed using the Nürick scale (Table 1)[12,13]. Complications were described in details. Statistical analysis was performed using a paired Student’s t-test - considering statistical significance a P value < 0.05. Analysis was made using the software Stata/MP version 13.0 for Windows (StataCorp/LP®). This study was approved by our Institutional Review Board (CAAE: 49070915.9.0000.5404).
| 0 | Root involvement. No spinal cord disease |
| 1 | Signs spinal cord disease without restriction in walking |
| 2 | Difficulty in walking without impact on employment |
| 3 | Difficulty in walking with impact on employment |
| 4 | Walk only with aid or walker |
| 5 | Bedridden or chair bound |
The radiological data were assessed by two authors together (OTS and AFJ). The acquisition of images was performed in 64-row multidetector CT (Anquilion 64, Toshiba Medical Systems®). The images were reconstructed in 0.5 mm thick slices and analyzed in bone window settings, length 300 Hounsfield and width 2500 Hounsfield.
The measurements were performed in an imaging workstation and all images were downloaded in DICOM format and the measurements were performed using the PACS Aurora 2 (Pixeon Medical System, version: 1.9.2)®. The measurements were assessed in both positions (flexion and extension), in sagittal view, following the criteria adopted by the study of Batista et al[14], as it follows: Atlanto-dental interval (ADI): Measured from the posterior margin of the anterior arch of C1 to the anterior portion of odontoid; clivus-canal angle (CCA): The angle formed by a line drawn from the posterior line of the clivus and a line marked from the posterior margin of the body of C2; distance of the tip of the Odontoid to the Chamberlain line: The distance from the tip of the odontoid to the Chamberlain’s line. Presence or absence of facet joints subluxation of the occipital-lateral masses of the atlas and the atlanto-axial joints; diagnosis of clivus hypoplasia: Adopted when the clivus had less than 36.6 mm (less than 2σ of the mean of the normal population)[1].
Thirty patients with congenital CVJ malformations were operated from 2010 to 2016 by the senior author (AFJ) at our institution. A total of ten patients had complete dynamic exams and were included according our inclusion criteria. The mean age of our population was 37.9 years (ranging from 15- to 56-year-old). Five patients (50%) were male and five were female (50%). Table 2 summarizes the clinical data of the patients.
| No. | Gender | Nurick pre | Nurick post | Follow-up (mo) | Pathology | Clivus hypoplasia | Atlas assimilation | Treatment | Tonsillar herniation |
| 1 | 38 | 4 | 2 | 38 | BI + Chiari | Present | Absent | PFD + Duropls | 14.95 |
| 2 | 35 | 3 | 2 | 30 | BI + Chiari | Present | Absent | PFD + Duropls | 15.19 |
| 3 | 15 | 2 | 1 | 21 | BI + Chiari | Absent | Absent | PFD + Duropls + Tonsilec | 9.4 |
| 4 | 29 | 2 | 1 | 30 | Chiari I | Absent | Absent | PFD + Duropls | 11.45 |
| 5 | 20 | 2 | 2 | 6 | BI + Chiari | Present | Present | PFD + Duropls | 11 |
| 6 | 40 | 2 | 1 | 14 | BI + Chiari | Present | Present | PFD + Duropls | 5 |
| 7 | 48 | 4 | 3 | 28 | BI + Chiari | Absent | Present | PFD + Duropls + OCFix | 7 |
| 8 | 56 | 5 | 3 | 8 | BI + Chiari | Present | Present | PFD + Duropls + OCFix | N/A |
| 9 | 52 | 1 | 1 | 5 | Chiari I | Absent | Absent | PFD + Duropls | 9 |
| 10 | 46 | 3 | 3 | 1 | Chiari I | Absent | Absent | PFD + Duropls | 7.44 |
| M | 37.9 | 2.8 | 1.9 | 1654 | 10.04 |
All patients had some degree of tonsillar herniation (mean of 10.04 mm below the McRae line, ranging from 5 to 15.19 mm). Seven patients (70%) had also the diagnosis of BI (with the tip of the odontoid above at least 5 mm the Chamberlain’s line).
The mean pre-operative Nürick grade was 2.8 (ranging from 1 to 5). The mean post-operative Nürick grade was 1.9 (ranging from 1 to 3), after a mean follow-up of 18.1 mo (ranging from 1 to 38 mo).
Treatment consisted in posterior fossa decompression with removal of the posterior arch of C1 in all cases. In all cases, duroplasty was performed, but only two cases had also tonsillar resection due to the severity of the tonsillar herniation. Two patients underwent concomitant occipito-cervical fixation because they presented a mobile atlantoaxial subluxation on dynamic images, as explained below.
The main bone anomaly associated with BI was clivus hypoplasia. Five patients had clivus hypoplasia, four patients had atlas assimilation and two patients had a C2-C3 fusion (Table 3).
| Flexion position | Extension position | |||||||
| N | ADI | CCA | Facet dislocation | Chamberlain | ADI | CCA | Facet dislocation | Chamberlain |
| 1 | 1.5 | 92° | Absent | +22.86 | 1.25 | 131° | Absent | +19.43 |
| 2 | 1.72 | 134° | Absent | +6.6 | 1.72 | 155° | Absent | +4.76 |
| 3 | 1.18 | 115° | Right side - 4 mm | +9.95 | 1.18 | 127° | Right side - 4 mm | +10.86 |
| 4 | 1.75 | 141° | Absent | 0 | 1.75 | 155° | Absent | -3.7 |
| 5 | 0.5 | 120° | Absent | +20 | 0.6 | 125° | Absent | +19.3 |
| 6 | 3.27 | 130° | Absent | +12.28 | 3.12 | 140° | Absent | +12.11 |
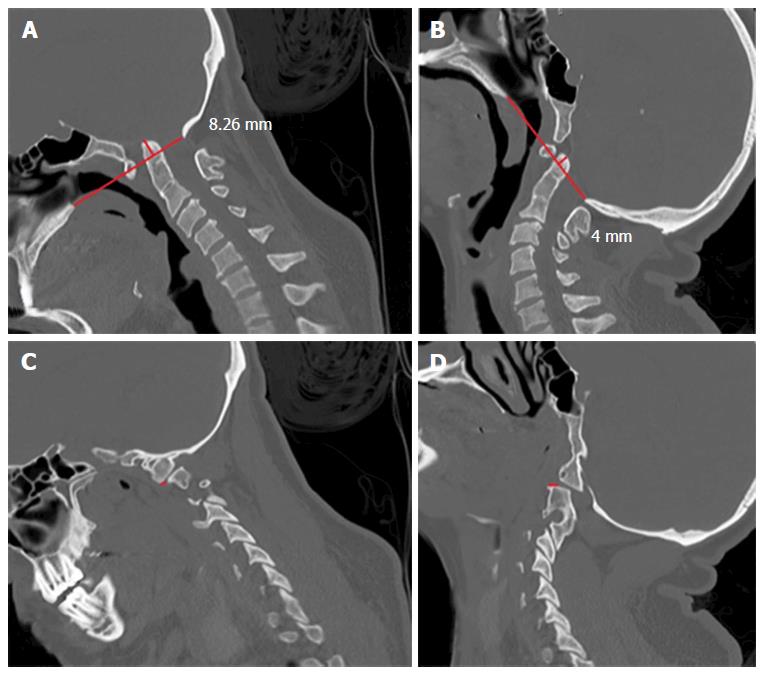
| 7 | 5.67 | 130° | Left side - 2 mm | +8.26 | 2.94 | 161° | Right side - 3 mm | +4 |
| 8 | 1 | 108° | Right side - 4 mm | N/A | 1 | 108° | Right side - 7 mm | N/A |
| 9 | 0.36 | 146° | Absent | +3.97 | 0.36 | 176° | Absent | -5 |
| 10 | 0.7 | 138° | Left site 3.7 mm | +2.67 | 0.7 | 144° | Left side 3.7 mm | +2.32 |
| M | 1.76 | 125.4° | +9.62 | 1.46 | 142.2° | +7.11 | ||
Flexion CT scan: The mean CCA was 125.4° (ranging from 92° to 146°), with a ADI of 1.76 mm (ranging from 0.36 to 5.67 mm) and a mean distance of the odontoid tip to the Chamberlain’s line of 9.62 mm above it (ranging from 0 to +22.86 mm). In the group with seven patients that also had the diagnosis of BI, the mean distance of the tip of the odontoid to the Chamberlain’s line was +13.32 mm (ranging from +6.6 to +22.86 mm) and the mean CCA was 118.4° (ranging from 92° to 134°). One patient surgically treated at a different institution had a previous posterior fossa decompression and the Chamberlain’s line was not accessed.
Extended CT scan: The mean CCA was 142.2° (ranging from 108° to 176°), with the mean ADI of 1.46 mm (ranging from 0.36 to 3.12 mm) and a mean distance from the tip of the odontoid to the Chamberlain’s line was 7.11 mm above it (ranging from less than -5 mm to up to 19.34 mm). In the six patients with BI, the mean distance from the odontoid tip to the Chamberlain’s line was 11.72 mm above it (ranging from 4 to 19.34 mm above it) and the mean CCA was 135.28° (ranging from 108° to 161°).
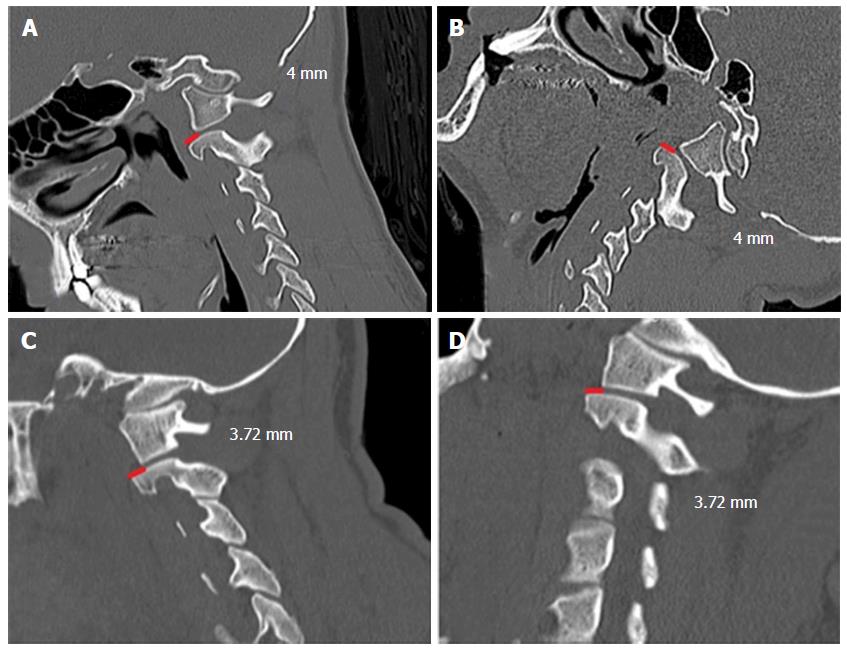
Four patients had some facet joints subluxation at the atlanto-axial region. Two of these patients underwent a cranio-cervical fixation due to their mobile subluxation: One patient had an increased facet subluxation in extension, from 4 to 7 mm, without changing the ADI distance and the other had an increased ADI in flexion, from 2.94 to 5.67 mm (Figure 1). The other two cases were treated initially without occipito-cervical fixation because their facet joints did not change on flexion and extension CT scan (Figure 2).
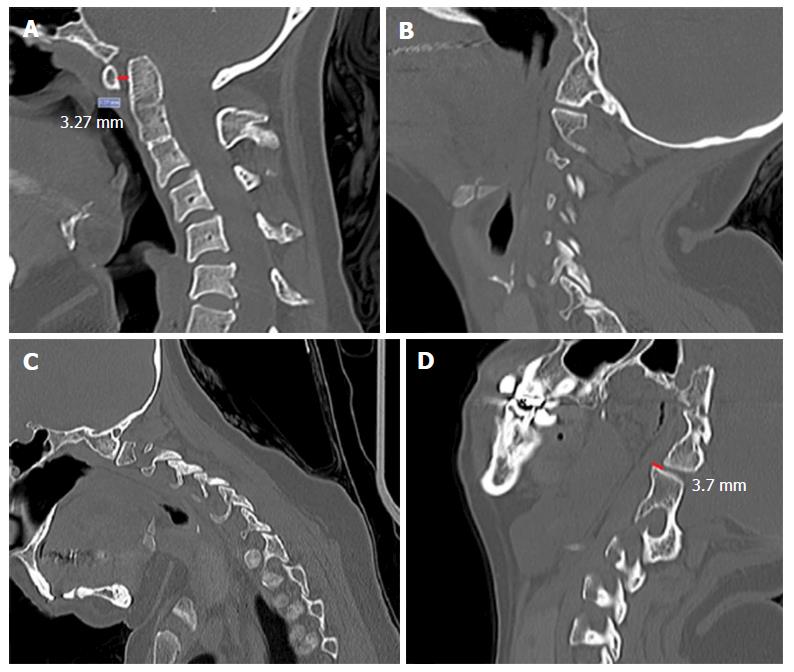
During the study follow-up, another patient who had BI and a congenital C2-C3 fusion developed latter cervical pain and dizziness when flexing the neck. A new dynamic CT scan was performed two years after posterior fossa decompression who had demonstrated a new atlanto-axial subluxation with dynamic change of 3.7 mm in the atlanto-axial right facet joint from flexion to extension. Additionally, this same patient also had an increased ADI varying from 1.51 mm in extension to 3.86 mm in flexion. We considered that she developed a postoperative instability and surgical fixation was proposed, but she refused it because she had a severe depression and familiar problems (Figure 3).
Comparing the differences of the measurements of the clivus canal angle and the distance of the tip of the odontoid to the Chamberlain’s line in flexion and extended position were statistically significant (P < 0.01 and 0.03, respectively), but for the ADI the difference was not observed (P = 0.29).
Panjabi et al[15] defined stability as the ability of the spine to maintain, under physiologic loads, the relationships between the vertebrae without resulting in pain, deformity or neurological compression. When specifically dealing with the mobile and complex CVJ, the criteria for instability are still debated[4]. According to the most recent studies, in patients with clear AAD, stabilization is mandatory. However, the indications for craniocervical fixation in patients with tonsillar herniation without AAD are controversial[2,6,8,16].
In congenital CVJ anomalies, instability may be secondary to bone hypoplasia, ligament and musculature laxity, and also by abnormal facet joints configuration that allows abnormal motion[16,17]. The instability may be not visualized in static radiological exams. In our series of ten patients, four had dynamic changes in the facet joints and one had late instability also well documented in flexion-extension CT scans, emphasizing the importance of adding this radiological modality in current investigation of congenital CVJ anomalies. Potential advantages of CT scans over plain radiographs include a better visualization of the facet joints and 3D reconstruction that allows better surgical planning and provides detailed anatomical visualization[18].
Additionally, in this study, we also analyzed the basic craniometry using dynamic CT. The mean CCA was 125.4° in flexion and 142.2° in extended position, with a mean difference of 16.8° (P < 0.01). This emphasizes the importance of proper positioning during occipito-cervical fusions. In the plain radiographs era, Smoker et al[19] had demonstrated that this angle changed about 30o from flexion to extension neck position, also reporting that normal range varied from 150° to 180°. Our limited variation from flexion to extension compared to the reported by Chandra et al[11] may be explained by the fact that some of our patients had clivus hypoplasia and atlas assimilation which may decrease CVJ motion when compared with normal subjects. Platybasia may lead to a lower CCA and CVJ kyphosis, with brainstem symptoms as well as compensatory subaxial hyperlordosis.
We also reported that the distance of the tip of the odontoid from the Chamberlain’s line varies from flexion (mean of +9.62 cm above the tip of the dens) to extension (mean of +7.11 above the tip of the dens) (P = 0.03), which may influence the incidence of the diagnosis of BI in patients with Chiari Malformation according to patients neck position when underwent a CT scan.
In the past, Goel et al[3,8] proposed that patients with BI without AAD required only foramen magnum decompression. In this study, we observed that some patients with tonsillar herniation but without AAD may have instability in about 20% of the cases. Additionally, these patients may develop CVJ instability after surgery (10% of the patients in the present study). Menezes et al[20] reported that patients with Chiari Malformation, atlas assimilation and concomitant congenital C2C3 fusion may develop atlanto-axial instability after posterior fossa decompression.
Another fact is that not only facet subluxation can be visualized with dynamic exams, but also changes in the ADI, similarly to upper cervical spine trauma or rheumatoid arthritis patients. In two of our patients, we observed an increasing ADI when changing the neck position, suggesting an occult insufficient transverse ligament that may potentially result in atlanto-axial instability, cervical pain and neurological deficits. In these patients, the mean ADI was 3.03 mm in extension to 4.47 mm in flexion, with an increase of about 47.5% after changing the position. However, the differences of the ADI in our series comparing flexion and extension were not significant (P = 0.29), probably because we excluded patients with evident AAD in static exams. The normal ADI obtained using CT scan in neutral position in a series of 100 patients without known CVJ anomalies varied from 0.5 to 1.7, using the exactly same methodology used in our study[14].
We also noted that some patients (patients 3 and 10) may have mild facet joints subluxation without dynamic changes. These patients were treated with foramen magnum decompression without fixation with an acceptable clinical outcome (both had improvement of their clinical symptoms).
Our study is limited by a small case series and limited follow-up. Additionally, we excluded many patients treated in our institution for congenital CVJ malformations because they did not have a complete preoperative dynamic exam. However, to our knowledge, we could clearly demonstrate the importance of dynamic CT scan evaluation in routine treatment of patients with symptomatic tonsillar herniation. Additionally, we reported that patients with mild subluxation without dynamics change may be considered for foramen magnum decompression alone. Dynamic CT was also useful for evaluating late postoperative instability.
In conclusion, we reported the utility of dynamic CT scans in the evaluation of the best treatment modality for patients with congenital CVJ anomalies. Significant changes were observed in the CCA and in the position of the odontoid in the cranial base. Prospective studies are necessary to evaluate the role of the radiological findings of dynamic CT scans on patients’ outcome.
Craniovertebral junction (CVJ) congenital malformations are challenging diseases. This study aims to identify which patient has signs of CVJ instability through a dynamic computed tomography scan.
Diagnostic of CJV instability in congenital disorders is still debated.
This article reported the importance of dynamic imaging evaluation of the CVJ in congenital malformation.
Decision making for surgical treatment of those patients that had CJV congenital malformations, such as Chiari I.
Atlanto-dental interval: Measured from the posterior margin of the anterior arch of C1 to the anterior portion of odontoid; clivus-canal angle: The angle formed by a line drawn from the posterior line of the clivus and a line marked from the posterior margin of the body of C2. Distance of the tip of the Odontoid to the Chamberlain line: The distance from the tip of the odontoid to the Chamberlain’s line. Presence or absence of facet joints subluxation of the occipital-lateral masses of the atlas and the atlanto-axial joints; diagnosis of clivus hypoplasia: Adopted when the clivus had less than 36.6 mm (less than 2σ of the mean of the normal population).
Very well designed and honest paper, worth publishing in the present form.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Brazil
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Anand A, Angoules A, Cui Q, Teli MGA S- Editor: Qiu S L- Editor: A E- Editor: Li D
| 1. | Joaquim AF. Basilar invagination. J Neurosurg Pediatr. 2012;10:355; author reply 355-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Shah A, Goel A. Clival dysgenesis associated with Chiari Type 1 malformation and syringomyelia. J Clin Neurosci. 2010;17:400-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 3. | Goel A. Basilar invagination, Chiari malformation, syringomyelia: a review. Neurol India. 2009;57:235-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 94] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 4. | Joaquim AF, Lawrence B, Daubs M, Brodke D, Tedeschi H, Vaccaro AR, Patel AA. Measuring the impact of the Thoracolumbar Injury Classification and Severity Score among 458 consecutively treated patients. J Spinal Cord Med. 2014;37:101-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Chamberlain WE. Basilar Impression (Platybasia): A Bizarre Developmental Anomaly of the Occipital Bone and Upper Cervical Spine with Striking and Misleading Neurologic Manifestations. Yale J Biol Med. 1939;11:487-496. [PubMed] |
| 6. | Goel A, Achawal S. The surgical treatment of Chiari malformation association with atlantoaxial dislocation. Br J Neurosurg. 1995;9:67-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 56] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Smith JS, Shaffrey CI, Abel MF, Menezes AH. Basilar invagination. Neurosurgery. 2010;66:39-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 116] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 8. | Goel A, Shah A, Rajan S. Vertical mobile and reducible atlantoaxial dislocation. Clinical article. J Neurosurg Spine. 2009;11:9-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 62] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 9. | Joaquim AF, Ghizoni E, Giacomini LA, Tedeschi H, Patel AA. Basilar invagination: Surgical results. J Craniovertebr Junction Spine. 2014;5:78-84. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Koller H, Resch H, Acosta F, Zenner J, Schwaiger R, Tauber M, Forstner R, Lederer S, Auffarth A, Hitzl W. Assessment of two measurement techniques of cervical spine and C1-C2 rotation in the outcome research of axis fractures: a morphometrical analysis using dynamic computed tomography scanning. Spine (Phila Pa 1976). 2010;35:286-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Chandra PS, Goyal N, Chauhan A, Ansari A, Sharma BS, Garg A. The severity of basilar invagination and atlantoaxial dislocation correlates with sagittal joint inclination, coronal joint inclination, and craniocervical tilt: a description of new indexes for the craniovertebral junction. Neurosurgery. 2014;10 Suppl 4:621-629; discussion 629-630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 12. | Nurick S. The natural history and the results of surgical treatment of the spinal cord disorder associated with cervical spondylosis. Brain. 1972;95:101-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 301] [Cited by in RCA: 275] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 13. | Nurick S. The pathogenesis of the spinal cord disorder associated with cervical spondylosis. Brain. 1972;95:87-100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 632] [Cited by in RCA: 610] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 14. | Batista UC, Joaquim AF, Fernandes YB, Mathias RN, Ghizoni E, Tedeschi H. Computed tomography evaluation of the normal craniocervical junction craniometry in 100 asymptomatic patients. Neurosurg Focus. 2015;38:E5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Panjabi MM, White AA. Basic biomechanics of the spine. Neurosurgery. 1980;7:76-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 166] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 16. | Fenoy AJ, Menezes AH, Fenoy KA. Craniocervical junction fusions in patients with hindbrain herniation and syringohydromyelia. J Neurosurg Spine. 2008;9:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 64] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 17. | Menezes AH. Craniovertebral junction database analysis: incidence, classification, presentation, and treatment algorithms. Childs Nerv Syst. 2008;24:1101-1108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 83] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 18. | Joaquim AF, Ghizoni E, Tedeschi H, Appenzeller S, Riew KD. Radiological evaluation of cervical spine involvement in rheumatoid arthritis. Neurosurg Focus. 2015;38:E4. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 58] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 19. | Smoker WR. Craniovertebral junction: normal anatomy, craniometry, and congenital anomalies. Radiographics. 1994;14:255-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 222] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 20. | Menezes AH, Vogel TW. Specific entities affecting the craniocervical region: syndromes affecting the craniocervical junction. Childs Nerv Syst. 2008;24:1155-1163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 33] [Article Influence: 1.9] [Reference Citation Analysis (0)] |