Published online Dec 18, 2017. doi: 10.5312/wjo.v8.i12.964
Peer-review started: September 22, 2017
First decision: November 7, 2017
Revised: November 13, 2017
Accepted: December 3, 2017
Article in press: December 3, 2017
Published online: December 18, 2017
Processing time: 87 Days and 18.1 Hours
Acute compartment syndrome (ACS) of the thigh following primary total hip arthroplasty (THA) is a highly uncommon complication and has not yet been reported before with regards to the anterior approach through the anterior supine interval. We present a case of a 69-year-old male patient with a history of stroke, who developed ACS of the thigh after elective THA while using therapeutic low molecular weight heparin as bridging for regular oral anticoagulation. ACS pathogenesis, diagnostic tools, treatment and relevant literature are discussed. The patient’s ACS was recognized in time and treated by operative decompression with fasciotomy of the anterior compartment. Follow-up did not show any neurological deficit or soft-tissue damage.
Core tip: Acute compartment syndrome of the thigh is an uncommon complication following total hip arthroplasty, which has not yet been reported after hip replacement by anterior approach through the anterior supine interval. Global increase in venous thromboembolism chemoprophylaxis may lead to an increase in incidence of postoperative bleeding and with this an increase in acute compartment syndrome of the thigh following primary total hip arthroplasty. Onset of severe pain of the upper leg postoperatively should warrant a high index of suspicion of this condition. Diagnostic tools such as ultrasound, computed tomography or intra-compartmental pressure measurements can be useful but should not lead to any delay of treatment.
- Citation: Hogerzeil DP, Muradin I, Zwitser EW, Jansen JA. Acute compartment syndrome of the thigh following hip replacement by anterior approach in a patient using oral anticoagulants. World J Orthop 2017; 8(12): 964-967
- URL: https://www.wjgnet.com/2218-5836/full/v8/i12/964.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i12.964
Acute compartment syndrome (ACS) is a known complication often following trauma such as fractures or crush injuries. However, ACS of the thigh is an uncommon complication, which has not been reported before after hip replacement by anterior approach through the anterior supine interval. Known causes for ACS of the thigh include femoral fractures, acetabular or proximal femur surgery, tourniquet application and extensive deep vein thrombosis[1-4]. With the current trend of more oral anticoagulants being used and perioperative bridging therapy using LMWH it is noted that postoperative bleeding and the hereby possibly inferred ACS may be on the rise.
A 69-year-old male, using oral anticoagulation medication (Fenprocoumon 3 mg) due to a history of stroke, underwent total hip replacement of the right hip using the anterior approach through the anterior supine interval, as treatment for his end stage osteoarthritis. Only uncemented materials were used. Following hospital protocol, the administration of oral anticoagulation (OAC) medication was discontinued 5 d before surgery and the patient was bridged using LWMH (Tinzaparin 18.000 IE, subcutaneously) as venous thromboembolism (VTE) chemoprophylaxis. Preoperatively the patients’ international normalized ratio was 1.3. Additionally, tranexamic acid, as part of hospital protocol regarding postoperative hemorrhage prophylaxis, was administered intraoperatively. THA was performed without any complications. However, total intraoperative blood loss was 600 cc, slightly higher than average. This was attributed to the patients’ regular use of anticoagulation medication and current bridging therapy. The night following the operation the patient complained of pain in the ipsilateral leg which was interpreted as postoperative pain for which additional opioids were prescribed. One day following surgery hemoglobin levels were 7.0 g/dL (Preoperative Hemoglobin levels were 9.4 g/dL). During the course of the day the patient needed additional opioids to perform routine exercises. However, during the evening the pain aggravated and additional opioids could not suppress the pain with progressing symptoms of swelling, hematoma and paresthesia of the right leg.
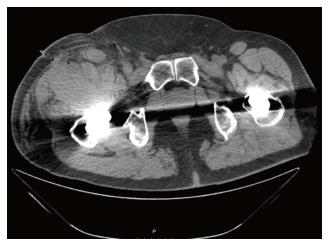
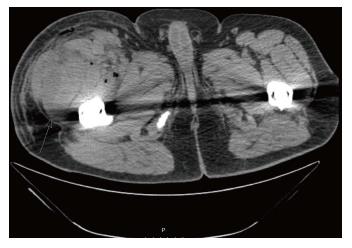
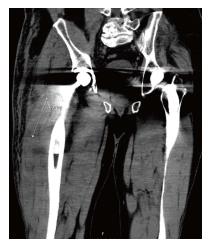
Ultrasound of the thigh was performed which showed an intramuscular hematoma of the anterior compartment of 8.3 cm by 3.5 cm (Figure 1). Additional computed tomography (CT-scan) was performed which confirmed the diagnosis and showed 2 hematomas of the anterior compartment (Figures 2-4). No intra-compartmental pressure measurements were performed as the diagnosis had already been confirmed and would only have delayed treatment. Delay of diagnosis in this case can be attributed to the fact that the patients’ need for additional opioids to perform routine exercises one day postoperatively is not an uncommon occurrence. Furthermore, the first postoperative Hemoglobin levels were slightly decreased (7.0 g/dL), however within acceptable postoperative range and thus warranted no further investigation at the time.
To prevent further expansion of the hematoma VTE prophylaxis was discontinued and an emergency fasciotomy through the anterior compartment of the thigh was performed. A large hematoma was evacuated, the surgical site was extensively irrigated with normal saline solution and tranexamic acid was administered topically in the wound. Cultures of the surgical site showed no infection. The following day postoperative hemoglobin levels were at 3.9 g/dL for which the patient received multiple 4 blood transfusions over the course of several days after which hemoglobin levels were normalized to 7.3 g/dL.
Directly after emergency fasciotomy the neurological deficit and the severe pain the patient had previously been experiencing, disappeared. Over the next few days mobilization was increased and at 6 d after emergency fasciotomy patient was discharged with low dose LMWH (Nadroparine 2850 IE, subcutaneously) as VTE prophylaxis. 11 d after emergency fasciotomy OAC therapy was resumed without any further complications.
At 8 and 12 wk follow-up, the patient did not have signs of any residual neurological deficit.
ACS is defined by increased pressure in a closed fascial space compromising the circulation to the nerves and muscles within the involved compartment[5]. ACS in the thigh is a rare complication following primary THA. This can be due to several reasons.
From an anatomical perspective, it could be explained by the large volume of soft tissue of the thigh, therefore requiring extravasation of a large volume of fluid to cause compression of local structures[3]. Aside from the large volume of the three compartments in the thigh, the fascia of the thigh seems to be more dilative compared to the fascia of the lower leg[6]. Furthermore, the compartments of the upper leg are partly open to the pelvis explaining the higher compensation space for increasing an intra-compartmental hematoma[7].
Literature shows cases with ACS both shortly after operation as well as several days following THA, the common denominator often being VTE prophylaxis[3,4,8]. It is our belief that in our patient, the increased intra-compartmental pressure was most likely caused by iatrogenic laceration to the branches of the circumflex femoral arteries aggravated by his regular use of anticoagulation medication and current bridging therapy. We noticed that the ACS progressively developed during the postoperative mobilization, which possibly severed the vessels during exercise. The classical sign of ACS, i.e. disproportionate pain, is difficult to judge in a patient after THA in which opiates are regularly required. However due to the alertness of the nurse staff and ward physician the diagnosis was confirmed shortly after the paresthesia developed, which prevented permanent neurological and vascular damage.
A 69-year-old male presented with severe pain, swelling, hematoma and paresthesia of the right leg following elective total hip replacement by anterior approach.
Severe pain, swelling and hematoma of the upper leg, as well as paresthesia of the lower leg.
Postoperative pain, postoperative dislocation of the hip, periprosthetic fracture, iatrogenic neurological damage.
Preoperative international normalized ratio was 1.3 and Hemoglobin level 9.4 g/dL, postoperative Hemoglobin levels were 7.0 g/dL and 3.9 g/dL.
Ultrasound of the thigh showed an intramuscular hematoma of the anterior compartment of 8.3 cm by 3.5 cm and computed tomography revealed two hematomas of the anterior compartment.
Cultures of the surgical site showed no infection.
Venous thromboembolism (VTE) prophylaxis was discontinued and an emergency fasciotomy through the anterior compartment of the thigh was performed during which a large hematoma was evacuated, the surgical site was extensively irrigated with normal saline solution and tranexamic acid was administered topically in the wound.
Acute compartment syndrome is a known complication often following trauma such as fractures or crush injuries. However, a highly uncommon presentation and localization of acute compartment syndrome is that of the thigh following total hip replacement by the anterior approach. The first symptoms of acute compartment syndrome of the thigh can easily be confused with other causes for postoperative pain, swelling, hematoma and paresthesia.
Acute compartment syndrome is defined by increased pressure in a closed fascial space compromising the circulation to the nerves and muscles within the involved compartment. VTE prophylaxis is a mechanical or pharmacologic method for prevention of venous thromboembolism.
Acute compartment syndrome of the thigh is a highly uncommon complication following total hip replacement by anterior approach and as such should and must be considered in case of postoperative onset of severe pain of the upper leg.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Netherlands
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Cui Q, Fenichel I S- Editor: Cui LJ L- Editor: A E- Editor: Lu YJ
| 1. | Kahan JS, McClellan RT, Burton DS. Acute bilateral compartment syndrome of the thigh induced by exercise. A case report. J Bone Joint Surg Am. 1994;76:1068-1071. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 39] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Rahm M, Probe R. Extensive deep venous thrombosis resulting in compartment syndrome of the thigh and leg. A case report. J Bone Joint Surg Am. 1994;76:1854-1857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 32] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Mar DD, MacDonald SJ, Bourne RB. Compartment syndrome of the right anterior thigh after primary total hip arthroplasty. Can J Surg. 2000;43:226-227 [PMID 10851420]. |
| 4. | Elsorafy KR, Jm Stone A, Nicol SG. Acute compartment syndrome of the thigh 10 days following an elective primary total hip replacement. Ortop Traumatol Rehabil. 2013;15:269-271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Lipson SJ, Mazur J. Anteroposterior spondyloschisis of the atlas revealed by computerized tomography scanning. A case report. J Bone Joint Surg Am. 1978;60:1104-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 404] [Cited by in RCA: 318] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 6. | Schwartz JT Jr, Brumback RJ, Lakatos R, Poka A, Bathon GH, Burgess AR. Acute compartment syndrome of the thigh. A spectrum of injury. J Bone Joint Surg Am. 1989;71:392-400. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 131] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | Burghardt RD, Siebenlist S, Döbele S, Lucke M, Stöckle U. Compartment syndrome of the thigh. A case report with delayed onset after stable pelvic ring fracture and chronic anticoagulation therapy. BMC Geriatr. 2010;10:51. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 8. | Nadeem RD, Clift BA, Martindale JP, Hadden WA, Ritchie IK. Acute compartment syndrome of the thigh after joint replacement with anticoagulation. J Bone Joint Surg Br. 1998;80:866-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.2] [Reference Citation Analysis (0)] |