Published online Oct 18, 2017. doi: 10.5312/wjo.v8.i10.809
Peer-review started: February 13, 2017
First decision: June 14, 2017
Revised: August 21, 2017
Accepted: September 3, 2017
Article in press: September 4, 2017
Published online: October 18, 2017
Processing time: 261 Days and 5.7 Hours
We report two cases where a proximal humeral locking plate was used for the fixation of an extremely distal, type III peri-prosthetic femoral fractures in relation to a total knee replacement (TKR). In each case there was concern regarding the fixation that could be achieved using the available anatomic distal femoral plates due to the size and bone quality of distal fragment. The design of the Proximal Humeral Internal Locking System (PHILOS) allows nine 3.5-mm locking screws to be placed over a small area in multiple directions. This allowed a greater number of fixation points to be achieved in the distal fragment. Clinical and radiological short-term follow-up (6-12 mo) has been satisfactory in both cases with no complications. We suggest the use of this implant for extremely distal femoral fractures arising in relation to the femoral component of a TKR.
Core tip: When dealing with periprosthetic fractures around a total knee replacement it is essential to consider the fracture site and configuration to allow selection of an implant that provides optimal fixation. When managing extremely distal femoral fractures a non-anatomic locking plate, such as Proximal Humeral Internal Locking System, may provide an option for fixation other than the available site-specific plates.
- Citation: Donnelly KJ, Tucker A, Ruiz A, Thompson NW. Managing extremely distal periprosthetic femoral supracondylar fractures of total knee replacements - a new PHILOS-ophy. World J Orthop 2017; 8(10): 809-813
- URL: https://www.wjgnet.com/2218-5836/full/v8/i10/809.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i10.809
Supracondylar periprosthetic femoral fractures around total knee replacement (TKR) are uncommon injuries with a reported prevalence in the literature of between 0.3% and 2.5%[1]. It is expected that these injuries will become more common as the population ages and an increasing number of TKRs are performed. Non-operative treatment of these fractures results in poorer outcomes and hence is reserved for minimally displaced fractures in low demand patients with significant co-morbidities[2,3].
A variety of operative treatment options exist, including retrograde femoral nailing, open reduction and internal fixation and revision arthroplasty. Perhaps the most challenging fracture patterns are the extremely distal peri-prosthetic femoral fractures. In these cases internal fixation or revision arthroplasty may be required as retrograde nailing may not be possible due to implant design or the inability to insert a locking screw in the distal fragment. Outcomes in treating these extreme distal fractures using femoral locking plates have been comparable with more proximal fractures treated in the same way[4]. One potential problem with anatomically designed distal femoral locking plates is the location and orientation of the screws, which may not allow adequate fixation in the distal fragment in these extremely distal peri-prosthetic femoral fractures.
Locking plates have been used successfully in proximal humeral fractures. The Proximal Humeral Internal Locking System (PHILOS) (DePuy Synthes, Switzerland) allows placement of 9 multi-directional locking screws over a small area. We discuss the use of the PHILOS in two elderly patients with very distal periprosthetic supracondylar fractures with satisfactory outcomes at short-term follow-up.
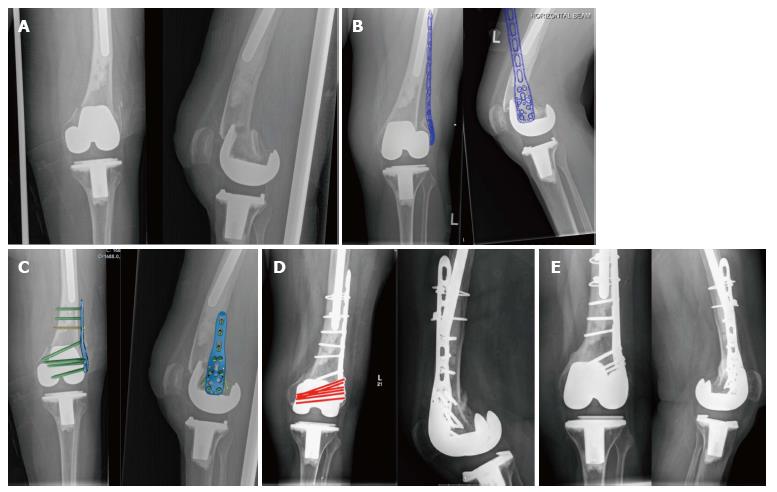
An 85-year-old female presented following a fall at home with pain and deformity around her left knee. She had undergone a left TKR four years previously. An ipsilateral long-stem revision total hip replacement was also noted. There was no other significant past medical history. She lived in sheltered accommodation and was independently mobile with the use of a single walking stick. Radiographs of her left femur revealed a very distal peri-prosthetic femoral fracture (Figure 1A).
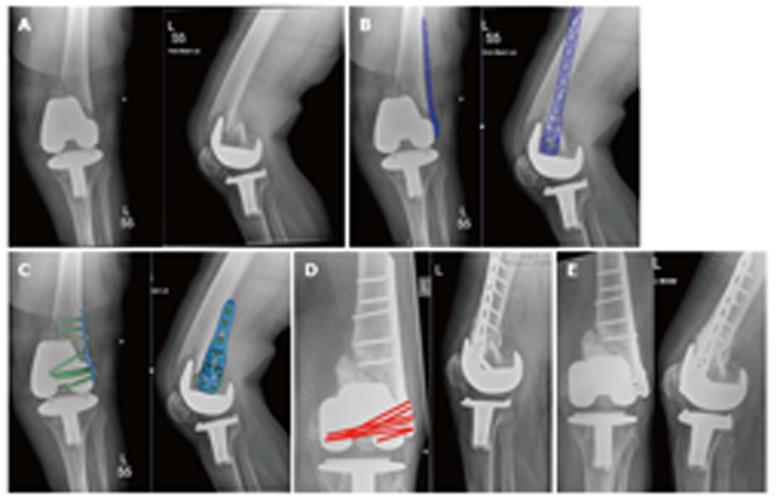
An 85-year-old female presented with pain and deformity around her left knee following a fall at home. She had undergone bilateral TKR’s 19 years previously. Significant medical comorbidities were noted which included atrial fibrillation and previous transient ischaemic attack, anticoagulation with warfarin, hypothyroid disease and polymyalgia rheumatica. She lived at home alone, with input from her family twice daily. She was independently mobile with the use of a rollator. Radiographs of her left femur revealed a very distal periprosthetic femoral fracture (Figure 2A).
Both senior authors reviewed each case and the injury radiographs. Pre-operative planning and templating was performed using the Northern Ireland Picture Archive and Communication System (Sectra AB, Sweden) (Figure 1B and Figure 2B). For both cases, surgery was performed under spinal anaesthesia and femoral nerve block. A single dose of 2 g IV Flucloxacillin and 160 mg IV Gentamicin were administered at induction of anaesthesia. A tourniquet was not used in either case. A direct lateral approach to the distal femur was performed in both cases. The fracture patterns extended very distally in each case and also narrow femoral shafts were noted. Taking these factors into consideration, a 6-hole PHILOS plate was used allowing optimal locking screw placement in the distal fragment and placement of the plate on the lateral aspect of the femur. Locking screws were placed in the distal fragment in both patients. To avoid a stress riser in Patient A the plate overlapped the distal aspect of the hip replacement stem by at least two cortical diameters. Three non-locking screws were inserted below the tip of the stem and two cables passed at the area of over-lap (Dall-Miles, Stryker, Switzerland). Patient B had five diaphyseal screws inserted.
Both patients had uneventful peri-operative periods and were discharged day 8 post-operatively to rehabilitation units for on-going physiotherapy and social care. Immobilisation was achieved using a locked cast brace and both patients were kept non-weightbearing for six weeks followed by a period of partial weight bearing with the brace unlocked. At 3 mo both patients were allowed to mobilise bearing full-weight on the injured side albeit with the use of a walking aid.
Patient A: At 6 mo follow-up, the patient was fully weight bearing with the use of one crutch, with a range of movement of 10-70 degrees. Radiographs demonstrated bridging callus on both the AP and lateral views (Figure 1D). At 19 mo, the range of movement had improved to 5-95 degrees and remained independently mobile. Radiographs confirmed radiological union (Figure 1E).
Patient B: At 5 mo follow-up position has been maintained. Callus is present posteriorly (Figure 2D). Range of movement 10-90 degrees. Has started progressive weightbearing. At 16 mo, range of movement was 5-90 degrees and the patient mobilised independently with the assistance of a walking frame. Radiographs confirmed radiological union (Figure 2E).
Fractures within 15 cm of the joint line or 5 cm of the proximal end of the femoral component of a TKR are considered peri-prosthetic femoral fractures. These fractures often occur in the setting of osteoporotic bone with rheumatoid arthritis, chronic steroid use and neurological disorders being established risk factors[1].
Su et al[1] suggested a classification system for these injuries based on fracture site and the available surgical options. Type I fractures are proximal to the femoral component. Type II fractures originate at the proximal aspect of the femoral component. These types were considered amenable to retrograde femoral nailing or fixation with a fixed angle device. In Type III fractures all parts of the fracture line is distal to the anterior flange of the femoral component. Revision arthroplasty is one possible treatment, especially in the presence of a loose femoral component. Fixation may also be possible if the distal fragment allows placement of screws. Each of the patients we have discussed had Type III fracture patterns.
A review performed by Ristevski et al[3] found favourable results with the use of retrograde intramedullary nailing and locked plating over conservatively managed fractures and those treated with conventional plating. However, in many cases the choice of fixation technique is influenced by factors such as the presence of a box in the femoral component to facilitate retrograde nailing[5], distal extent of the fracture, availability of existing bone stock and fix of the components. Good results have been reported with the use of site-specific locking plates[6-8], such as the Less Invasive Stabilization System (DePuy Synthes, Switzerland).
Biomechanically, locking plates create a fixed-angle single-beam construct[9]. This provides relative stability, allowing for secondary bone healing. Their use has been shown to possess superior resistance to rotational strain over both static and dynamically locked intramedullary nails -3.8° for locking plates, vs 14.2° and 15.7° for static and dynamic locking respectively[10]. Locking plate systems allow for even stress distribution along the implant length, and the plates function to convert shear forces into compressive forces at the screw bone interface[11].
The PHILOS has been used successfully in proximal humeral fractures where similar problems with osteoporotic bone and small fracture fragments can exist[12]. Again, it has been shown to resist torsional and bending forces more so than intramedullary nailing under cyclical loading, which is comparative to normal in vivo physiological functionality[13,14]. Periprosthetic fracture resulting in primary implant failure is rare complication, with rates quoted at 0.7%. The mechanical benefits of a PHILOS locking plate in managing this injury pattern make it an attractive implant option where longevity is required[15]. However, the PHILOS has not been studied for its use in lower limb fracture management.
A study by Stein et al[16] demonstrated that at any age, women have smaller femora, with less cortical bone and higher bone stresses than men. The PHILOS is narrower than many of the specific distal femoral locking plates and therefore may be a more appropriate fit for smaller females, such as the cases discussed. The major benefit we found of using the PHILOS was the design of the plate, which allowed the placement of a maximum of nine polyaxial divergent screws over a small area. This allowed us to maximise our fixation in the distal fragment.
In conclusion, we have shown that a PHILOS can be considered as a viable treatment option for very distal Type III fracture patterns with good short-term results in low demand patients. Each case highlights the need for careful consideration of the fracture configuration to allow the treating surgeon to select an appropriate means of fixation.
Two cases of 85-year-old females who both presented with pain and deformity of their lower limb following a fall at home.
Pain and deformity about the knee was apparent, with localised swelling and the inability to weight bear. Midline anterior scars in keeping with a previous knee arthroplasty were evident.
Periprosthetic fractures involving the distal femur or proximal tibia, fracture of femoral diaphysis.
All laboratory tests were within normal limits.
A periprosthetic fracture about the femoral component of a total knee arthroplasty was evident on plain film radiographs. No additional 3D imaging (i.e., computed tomography) was required.
A very distal periprosthetic femoral fracture.
Open reduction and internal fixation of the fracture using a PHILOS locking plate, using the ability to place polyaxial locking screws into the small distal fragment, thereby maximising construct stability.
Periprosthetic femoral fracture about a total knee arthroplasty are rare, and several methods for managing these are reported in the literature. This case is unique in that the distal fragment was too small to allow for a lateral LISS femoral plate, nor did the implants allow for a retrograde intramedullary device to be used.
PHILOS is an acronym for Proximal Humeral Internal Locking Osteo-Synthesis, and describes the locking screw nature of the internal implant.
The use of the PHILOS for this particular fracture configuration is novel. The authors have managed to use this in a rare, and challenging circumstance, with success both in terms of radiological union and restoration of mobility and function. Careful pre-operative planning, knowledge of available implants and appreciation of fracture configuration is crucial in managing the very distal femoral periprosthetic fracture about a total knee arthroplasty.
This is a nice paper. The idea for using PHILOS plate is very unique. This manuscript presents a novel technique for the management of periprosthetic supracondylar femoral fractures which deserves attention from the orthopaedic community in order to be fairly judged.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Angoules A, Fenichel I, Ohishi T, Papachristou GC S- Editor: Kong JX L- Editor: A E- Editor: Lu YJ
| 1. | Su ET, DeWal H, Di Cesare PE. Periprosthetic femoral fractures above total knee replacements. J Am Acad Orthop Surg. 2004;12:12-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 180] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 2. | McAlinden MG, Masri BA, Garbuz DS, Duncan CP. Periprosthetic Fractures About Total Knee Arthroplasty. In: Callaghan JJ, Rosenberg AG, Rubash HE, Simonian PT, Wickiewicz PT. The Adult Knee. |
| 3. | Ristevski B, Nauth A, Williams DS, Hall JA, Whelan DB, Bhandari M, Schemitsch EH. Systematic review of the treatment of periprosthetic distal femur fractures. J Orthop Trauma. 2014;28:307-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 82] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 4. | Streubel PN, Gardner MJ, Morshed S, Collinge CA, Gallagher B, Ricci WM. Are extreme distal periprosthetic supracondylar fractures of the femur too distal to fix using a lateral locked plate? J Bone Joint Surg Br. 2010;92:527-534. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 76] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 5. | Thompson SM, Lindisfarne EA, Bradley N, Solan M. Periprosthetic supracondylar femoral fractures above a total knee replacement: compatibility guide for fixation with a retrograde intramedullary nail. J Arthroplasty. 2014;29:1639-1641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Althausen PL, Lee MA, Finkemeier CG, Meehan JP, Rodrigo JJ. Operative stabilization of supracondylar femur fractures above total knee arthroplasty: a comparison of four treatment methods. J Arthroplasty. 2003;18:834-839. [PubMed] |
| 7. | Kääb MJ, Stöckle U, Schütz M, Stefansky J, Perka C, Haas NP. Stabilisation of periprosthetic fractures with angular stable internal fixation: a report of 13 cases. Arch Orthop Trauma Surg. 2006;126:105-110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 49] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Anakwe RE, Aitken SA, Khan LA. Osteoporotic periprosthetic fractures of the femur in elderly patients: outcome after fixation with the LISS plate. Injury. 2008;39:1191-1197. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Strauss EJ, Schwarzkopf R, Kummer F, Egol KA. The current status of locked plating: the good, the bad, and the ugly. J Orthop Trauma. 2008;22:479-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 109] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 10. | Citak M, Kendoff D, Gardner MJ, Oszwald M, O’Loughlin PF, Olivier LC, Krettek C, Hüfner T, Citak M. Rotational stability of femoral osteosynthesis in femoral fractures - navigated measurements. Technol Health Care. 2009;17:25-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Egol KA, Kubiak EN, Fulkerson E, Kummer FJ, Koval KJ. Biomechanics of locked plates and screws. J Orthop Trauma. 2004;18:488-493. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 505] [Cited by in RCA: 495] [Article Influence: 23.6] [Reference Citation Analysis (0)] |
| 12. | Erasmo R, Guerra G, Guerra L. Fractures and fracture-dislocations of the proximal humerus: A retrospective analysis of 82 cases treated with the Philos(®) locking plate. Injury. 2014;45 Suppl 6:S43-S48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Edwards SL, Wilson NA, Zhang LQ, Flores S, Merk BR. Two-part surgical neck fractures of the proximal part of the humerus. A biomechanical evaluation of two fixation techniques. J Bone Joint Surg Am. 2006;88:2258-2264. [PubMed] |
| 14. | Kralinger F, Gschwentner M, Wambacher M, Smekal V, Haid C. Proximal humeral fractures: what is semi-rigid? Biomechanical properties of semi-rigid implants, a biomechanical cadaver based evaluation. Arch Orthop Trauma Surg. 2008;128:205-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Thanasas C, Kontakis G, Angoules A, Limb D, Giannoudis P. Treatment of proximal humerus fractures with locking plates: a systematic review. J Shoulder Elbow Surg. 2009;18:837-844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 307] [Cited by in RCA: 265] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 16. | Stein MS, Thomas CD, Feik SA, Wark JD, Clement JG. Bone size and mechanics at the femoral diaphysis across age and sex. J Biomech. 1998;31:1101-1110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 46] [Article Influence: 1.7] [Reference Citation Analysis (0)] |