Peer-review started: July 27, 2016
First decision: September 6, 2016
Revised: September 17, 2016
Accepted: October 17, 2016
Article in press: October 18, 2016
Published online: January 18, 2017
Processing time: 172 Days and 9.9 Hours
To investigate the reliability and concurrent validity of the Baseline® Body Level/Scoliosis meter for adolescent idiopathic scoliosis postural assessment in three anatomical planes.
This is an observational reliability and concurrent validity study of adolescent referrals to the Orthopaedic department for scoliosis screening at Karolinska University Hospital, Stockholm, Sweden between March-May 2012. A total of 31 adolescents with idiopathic scoliosis (13.6 ± 0.6 years old) of mild-moderate curvatures (25°± 12°) were consecutively recruited. Measurement of cervical, thoracic and lumbar curvatures, pelvic and shoulder tilt, and axial thoracic rotation (ATR) were performed by two trained physiotherapists in one day. The intraclass correlation coefficient (ICC) was used to determine the inter-examiner reliability (ICC2,1) and the intra-rater reliability (ICC3,3) of the Baseline® Body Level/Scoliosis meter. Spearman’s correlation analyses were used to estimate concurrent validity between the Baseline® Body Level/Scoliosis meter and Gold Standard Cobb angles from radiographs and the Orthopaedic Systems Inc. Scoliometer.
There was excellent reliability between examiners for thoracic kyphosis (ICC2,1 = 0.94), ATR (ICC2,1 = 0.92) and lumbar lordosis (ICC2,1 = 0.79). There was adequate reliability between examiners for cervical lordosis (ICC2,1 = 0.51), however poor reliability for pelvic and shoulder tilt. Both devices were reproducible in the measurement of ATR when repeated by one examiner (ICC3,3 0.98-1.00). The device had a good correlation with the Scoliometer (rho = 0.78). When compared with Cobb angle from radiographs, there was a moderate correlation for ATR (rho = 0.627).
The Baseline® Body Level/Scoliosis meter provides reliable transverse and sagittal cervical, thoracic and lumbar measurements and valid transverse plan measurements of mild-moderate scoliosis deformity.
Core tip: The Baseline® Body Level/Scoliosis meter is inexpensive, easily administered and provides reliable transverse and sagittal cervical, thoracic and lumbar measurements as well as valid transverse plan measurements of mild-moderate scoliosis deformity.
- Citation: Prowse A, Aslaksen B, Kierkegaard M, Furness J, Gerdhem P, Abbott A. Reliability and concurrent validity of postural asymmetry measurement in adolescent idiopathic scoliosis. World J Orthop 2017; 8(1): 68-76
- URL: https://www.wjgnet.com/2218-5836/full/v8/i1/68.htm
- DOI: https://dx.doi.org/10.5312/wjo.v8.i1.68
Adolescent idiopathic scoliosis (AIS) is a three-dimensional (3D) structural deformation of the spine in otherwise normal adolescents during puberty[1]. AIS is characterized as: (1) a lateral spinal curvature in the frontal plane (Cobb angle > 10°); (2) a disturbance of spinal curvatures in the sagittal plane; and (3) an axial rotation of vertebrae in the transverse plane. In the majority of cases, spinal asymmetry is noted during primary health care screening[2], and the patients are referred to specialist orthopaedic clinics for assessment, longitudinal observation and treatment[3].
Methods for the clinical evaluation of trunk deformity that are reliable, valid, feasible and acceptable is of great importance for patients and clinicians to evaluate and monitor aspects of AIS[4]. Methods that are easy to administer and inexpensive could provide essential information replacing the need for repeated radiation from radiographs and also expensive surface topography equipment. An easy to administer and inexpensive test for scoliosis is measuring the axial thoracic rotation (ATR) using a Scoliometer[5]. The inter-observer and intra-observer reliability of Scoliometer assessments have in several studies ranged from very good to excellent, and the tool is reportedly useful as a screening device[6]. Further, the validity of the Scoliometer when correlated to the Gold Standard Cobb angle from radiographs has been found to be fair to very good[6,7]. A limitation with the Scoliometer ATR measurement and Cobb angle from radiographs is however that it only measures deformity in a single anatomical plane when scoliosis is a 3D deformity.
To obtain a better description of scoliosis related morphologic deformity in several anatomical planes and reduce the need of radiographic exposure, techniques such as 3D postural analysis systems have been developed[8]. However, these measurement systems are not accessible for most clinicians and require specialized training and complex data processing. Thus, a simpler, inexpensive 3D tool is needed to measure scoliosis morphology in a clinical setting. A thorough literature search[9] revealed no published research investigating the reliability and/or validity of simpler, inexpensive 3D tools. The Baseline® Body Level/Scoliosis meter is an inexpensive and easy to administer clinical tool that can be used to obtain quick measurements of scoliosis morphology in three anatomical planes.
The primary objective of this study was to investigate the inter-examiner reliability for the Baseline® Body Level/Scoliosis meter for the following parameters: Cervical, thoracic and lumbar curve in the sagittal plane; pelvic and shoulder tilt in the frontal plane as well as the inter-examiner and intra-examiner reliability for ATR in the transverse plane. A secondary objective was to investigate the concurrent validity of the Baseline® Body Level/Scoliosis meter compared to Orthopaedic Systems Inc. Scoliometer and Cobb angle from radiographs and discuss its clinical utility.
This is an observational reliability and concurrent validity study. All study participants, or their legal guardian, provided informed written consent prior to study enrolment. The study received ethical approval from the Swedish Research Council Regional Ethics Committee in Stockholm, Sweden (Dnr: 2012/172-31/4) and from Bond University Health Research Ethics Committee in 2014 (RO 1896). The study followed Guidelines for Reporting Reliability and Agreement Studies, which contains issues to be addressed when reliability and agreement studies are reported[10].
Recruitment was achieved through consecutive adolescent referrals to the Orthopaedic department for scoliosis screening at Karolinska University Hospital, Stockholm, Sweden between March-May 2012. Informed consent was obtained from individuals that fulfilled the inclusion criteria to participate in the study. Inclusion criteria included: (1) diagnosis of idiopathic scoliosis; and (2) males and females aged 9-17 years. Exclusion criteria included: (1) scoliosis with a possible non-idiopathic aetiology (patients were excluded from the study if the pathogenesis of the scoliosis was due to a neuromuscular, neurological, congenital malformation or trauma related comorbidity); or (2) inability to understand Swedish. Thirty-one patients participated in the study, 27 females and 4 males with a mean age of 13.6 years and mean Cobb angle of 25°. The number of participants was deemed adequate to establish a practically useful clinically important change[11]. Patient characteristics and demographics are presented in Table 1.
| Mean (± SD) | n (%) | |
| Age (yr) | 13.6 (0.6) | |
| Sex | ||
| Males | 4 (13) | |
| Females | 27 (87) | |
| Primary curve Cobbs angle (degrees) | 25 (12) | |
| Scoliosis type (Lenke classification) | ||
| Main thoracic (1AN) | 22 (71) | |
| Thoracolumbar/lumbar (5CN) | 9 (29) |
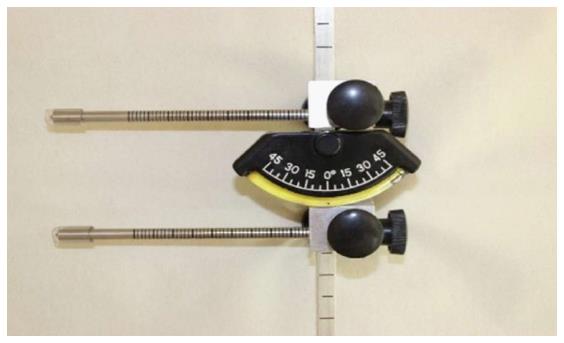
Two physiotherapists (10 and 15 years’ experience) performed examination of all participants with AIS, using two devices. To standardize their method of assessment the examiners trained in the use of the devices for 5 h before the outset of the study and had clinical experience in the application of the devices. The Baseline® Body Level/Scoliosis meter (Figure 1), developed by Orthopaedics Systems Incorporation®, is a fluid filled inclinometer in which an enclosed ball shows the ATR on a scale of 1 degree increments that range from 0-30 degrees. To improve the conformity of measurements, the recorded value is the one corresponding to the highest value entirely crossed by the enclosed ball. Measurements of cervical, thoracic, lumbar curvatures and pelvic and shoulder tilt, as well as ATR were performed with the Baseline® Body Level/Scoliosis meter. Measurements of ATR were also performed using the original Orthopaedics Systems Incorporation “Scoliometer”. In order to reduce the error associated with the measurement, both examiners used the same devices.
During the measurement, all subjects were barefoot and their back was exposed, which allowed palpation of the entire back. Trousers were lowered to the hip if there was difficulty in palpating the apex of the sacrum or L5. Measurements conducted by both raters were performed within 30 min and were executed in the same order. Examiners had no access to the results of the other measures to avoid recall of the previous values. A protocol that allowed as few manual changes as possible of the Baseline® Body Level/Scoliosis meter was chosen to obtain an efficient examination. The ATR measurements were repeated 3 times, as these measurements were associated with more sources of error. Other measurements were only executed once. Between each evaluation, the subject was instructed to leave the evaluation position to rest. The order of the therapist first taking measurements was randomized. Specific procedures regarding test positions, and device placement were performed according to the following protocol.
Cervical curve in centimetres: The subject was placed in standing position with feet together and asked to “stand straight”. The spinous process of C4 was palpated by palpating the process of C2, and then C3 to C4. Then the spinous process of C7 was palpated, the most prominent process in the cervical area, and was distinguished from C6 by bending the head backwards, causing C6 to move anteriorly. After localizing C4 and C7 the rods of the Scoliometer was placed over these spinous processes. The lower rod was unlocked until the gauge indicated 0. Then the rod was locked and the measurements were recorded in centimetres.
Thoracic curve in centimetres: The patient was placed in a standing position with feet together and asked to “stand straight”. The spinous process of C7 was palpated to place the upper rod. The bottom rod was placed at the spinous process of the vertebrae at the apex of the thoracic kyphosis. If there was a deviation of curvature in the frontal plane, the position of the gauge had to be held vertically and therefore the rod could be placed lateral to the spinous process. The lower rod was unlocked until the gauge indicated 0. Then the rod was locked and the measurements were recorded in centimetres.
Anteroposterior angulation L5 and Sacrum in centimetres: The patient was placed in standing position with feet together and asked to “stand straight”. The spinous process of L5 was palpated by placing the index fingers over the crest of the ilium and then palpating the spinous process at the same level, that usually is L4, and then the lower process should be L5. The next rod was placed over the most prominent tubercle of the sacral curvature. The lower rod was unlocked until the gauge indicated 0. Then the rod was locked and the measurements were recorded in centimetres.
ATR in degrees: The patient was placed in standing position with feet together and asked to “stand straight”, the trunk was anteriorly flexed and almost parallel to the ground, with relaxed arms, hanging perpendicular to the trunk and hands folded. The distance between the rods was set individually for each patient, and placed in the middle of both right and left thorax sides in relation to the spinal column posteriorly level with the apex of the curvature. Both of the rods were locked in the same length and placed over the most prominent point of the curvature. In this position the gauge reading showed the degree of the curvature. Two point five degrees or more was listed.
Pelvic tilt in degrees: The patient was placed in standing position with feet together and asked to “stand straight”. Both rods were loosened and placed firmly over each iliac crest and locked with the gauge in the middle. In this position the gauge reading showed the degree of the tilt with 2.5 degrees or more listed.
Shoulder tilt in degrees: The patient was sitting at a 43.5 cm high chair and asked to “sit straight”. The sitting position was chosen to avoid the influence of leg length difference. Both rods were loosened and placed firmly over each acromioclavicular articulation and locked with the gauge in the middle. To palpate the acromioclavicular joint (AC joint), find the “soft spot” at the back of the clavicle, anterior to that is the AC joint. In this position the gauge reading showed the degree of the tilt, anything equal to or greater than 2.5 degrees was listed.
ATR in degrees: The patient was placed in standing position with feet together and asked to “stand straight”, with trunk anteriorly flexed and parallel to the ground, with relaxed arms, hanging perpendicular to the trunk and hands folded. The value indicated by the metal sphere after placing the Scoliometer over the spinous process is used to indicate the value of axial trunk rotation. Examiners drew the Scoliometer along the spinous processes to discover the level with the highest reading and measured the axial trunk rotation with 1 degree or more listed.
Standing scoliosis posteroanterior radiographs were performed and measured by a radiologist, and double-checked by the physiotherapist. For the lateral image the feet are together and parallel to the screen. The right side of the body faces the radiation source. The patient was to hold his/her hands on a bar in front of the body and above the shoulders, so that the shoulders and elbows were at 90 degrees flexion. In this position the arms did not obscure the vertebral column. The hands were placed adjacent to one another. If the patient was wearing a brace, it was not to be worn the night prior to the scoliosis radiographs being taken. The Cobb angle was formed by the inclination of the upper end plate of the upper end vertebra and the inclination of the lower end plate of the lower end vertebra measured on posteroanterior view X-ray radiographs[12].
Two independent researchers completed statistical analysis of the data utilizing SPSS software Version 22. The statistics were additionally reviewed by three of the authors who have specific biostatistical competency for reliability and validity studies. Descriptive statistics including means, standard deviations and ranges (minimum and maximum) were calculated for both raters and tabulated as a summary of measurements and patient demographic data. The intraclass correlation coefficient (ICC) is nowadays the preferred retest correlation coefficient and was the method used to determine reliability[11]. A two-way random analysis of variance and ICC2,1 was used to determine inter-observer reliability in small groups with two test occasions. The intra-observer reliability was determined for ATR with a two way mixed analysis of variance and ICC3,3 using the average of three measurements. The ICC was interpreted with values of < 0.39 as poor, 0.40-0.74 as adequate, and > 0.75 as excellent, as these are considered the minimum standards for reliability coefficients sufficient for research purposes[13]. A 95%CI for the mean difference between the two test occasions was formed with the formula 95%CI = mean diff - 2.05 × standard deviation (SD) to determine if a true systematic difference existed between the two raters[11]. The mean difference between raters was calculated to evaluate changes in the mean between two test occasions[11]. To interpret absolute reliability the standard error of measurement (SEM) was calculated using the formula SEM = √WMS[11,14], where WMS is the mean square error term from the analysis of variance[11]. The smallest real difference (SRD and 95% SRD) was also calculated to determine the magnitude of change that would exceed the threshold of measurement error at the 95% confidence level[11]. The formula used was SRD = 1.96 × SEM ×√2. To calculate the 95% levels of agreement the formula mean difference - 2.05 × SD was applied, where n = 2.05 is a good approximation when the number of subjects is > 30[11]. The Spearman’s correlation coefficient was used to analyse the concurrent validity between measurements from the Scoliometer devices and Cobb angles from radiographs, as Spearman’s are not dependent on normality of test data. Correlation values smaller than 0.25 were considered poor, between 0.25 and 0.49 were low, between 0.50 and 0.69 were moderate, between 0.70 and 0.89 were good, and between 0.90 and 1.0 were excellent[15].
Table 2 reports a descriptive summary of measurements taken by each of the raters.
| Examiner A | Examiner B | |||||||||||
| Mean | n | SD | Range | Min | Max | Mean | n | SD | Range | Min | Max | |
| Cervical lordosis (cm) | 2.5 | 31 | 0.8 | 3 | 1 | 4 | 3.0 | 31 | 0.8 | 4 | 2 | 6 |
| Thoracic kyphosis (cm) | 3.7 | 31 | 1.7 | 7 | 1.2 | 8.2 | 3.7 | 31 | 1.7 | 7.4 | 0.6 | 8 |
| Lumbar lordosis (cm) | 3.0 | 31 | 1.0 | 4.2 | 0.6 | 4.8 | 3.5 | 31 | 1.0 | 3.8 | 1.4 | 5.2 |
| Pelvic tilt (degrees) | 1.8 | 29 | 1.9 | 7.5 | 0 | 7.5 | 3.3 | 29 | 2.5 | 10 | 0 | 10 |
| Shoulder tilt (degrees) | 1.2 | 30 | 1.4 | 5 | 0 | 5 | 1.3 | 30 | 1.7 | 7.5 | -2.5 | 5 |
| ATR Scoliometer (degrees) | 10.2 | 31 | 6.1 | 27.5 | 0 | 27.5 | 10.5 | 31 | 6.1 | 27.5 | 0 | 27.5 |
| ATR Baseline Level/Scoliosis meter (degrees) | 10.9 | 31 | 5.8 | 24.5 | 3 | 27.5 | 10.3 | 31 | 5.6 | 23.8 | 0 | 23.8 |
Table 3 presents the inter-examiner reliability for the Baseline® Body Level/Scoliosis meter. In the measurement of thoracic kyphosis and ATR, there was excellent reliability between examiners with an ICC2,1 of 0.94 (95%CI: 0.87-0.97) and 0.92 (95%CI: 0.84-0.96) respectively. When taking into consideration excursions in the 95%CI, the method was adequate-to-excellent in the measurement of lumbar lordosis, with an ICC2,1 of 0.79 (95%CI: 0.47-0.91). Furthermore varying adequacy could be seen in the inter-observer reliability in the measurement of cervical lordosis (ICC2,1 = 0.51, 95%CI: 0.02-0.76), and poor inter-examiner reliability when used to measure secondary curves in the frontal plane; pelvic tilt (ICC2.1 = -0.41, 95%CI: -0.89-0.47) and shoulder tilt (ICC2,1 = -0.30, 95%CI: -1.86-0.39). When measurements from the Baseline® Body Level/Scoliosis meter were compared to measurements from the Scoliometer, which is the current Gold Standard to measure ATR, the reliability was similar, with an ICC2,1 of 0.92 (0.84-0.96), compared to the Scoliometer with an ICC2,1 of 0.94 (95%CI: 0.88-0.97).
| Measures | ICC2,1 | 95%CI for ICC | Mean difference | 95%CI for mean difference | SEM | SRD | 95% SRD |
| Cervical Lordosis (cm) | 0.51 | 0.02-0.76 | -0.53 | -0.84-0.21 | 0.82 | 2.28 | -2.81-1.76 |
| Thoracic Kyphosis (cm) | 0.94 | 0.87-0.97 | 0.013 | -0.29-0.31 | 1.66 | 4.60 | -4.47-4.47 |
| Lumbar Lordosis (cm) | 0.79 | 0.47-0.91 | -0.44 | -0.71-0.17 | 0.99 | 2.74 | -3.18-2.3 |
| ATR Scoliometer (degrees) | 0.94 | 0.88-0.97 | -0.35 | -1.39-0.70 | 6.07 | 16.81 | -17.16-16.47 |
| ATR Baseline Level/Scoliosis meter (degrees) | 0.92 | 0.84-0.96 | 0.60 | -0.51-1.72 | 5.67 | 15.72 | -15.12-16.33 |
| Shoulder tilt (degrees) | -0.30 | -1.86-0.39 | -0.17 | -1.05-0.71 | 1.56 | 4.33 | -4.49-4.49 |
| Pelvic tilt (degrees) | -0.41 | -0.89-0.47 | -1.47 | -0.267-0.26 | 2.32 | 6.42 | -7.89-4.96 |
Systematic error exists between raters in the mean measurements of lumbar lordosis and pelvic tilt when using the Baseline® Body Level/Scoliosis meter, as shown by the 95%CI for mean difference, suggesting non-random error exists. A large measurement error between examiners’ measurements exists for pelvic tilt (SEM = 2.3°) and shoulder tilt (SEM = 1.6°). The small 95% SRD between measurements taken by two separate examiners for thoracic kyphosis (-4.5-4.5) and ATR with Baseline® Body Level/Scoliosis meter (-15.1-16.3), and ATR measured with Scoliometer (-17.2-16.5), suggests these measurements are more sensitive and can be considered highly reliable.
Table 4 presents the intra-examiner reliability for the ATR measures. Excellent intra-examiner reliability was seen in ATR measured by the Baseline® Body Level/Scoliosis meter (Examiner A ICC3,3 = 1.00, Examiner B = 0.98) and by the Scoliometer (Examiner A ICC3,3 = 0.99, Examiner B = 0.98).
| Measures | Examiner | ICC3,3 | 95%CI for ICC | Mean difference | 95%CI for mean difference | SEM | SRD | 95% SRD | |
| ATR Scoliometer (degrees) | A | 0.99 | 0.99-1.00 | A1 | 0 | 0 | 1.35 | 3.74 | -3.74-3.74 |
| A2 | -0.24 | -3.00-3.05 | 1.35 | 3.75 | -4.00-3.51 | ||||
| A3 | -0.32 | 2.52-2.40 | 1.33 | 3.70 | -3.37-3.37 | ||||
| B | 0.98 | 0.97-1.00 | B1 | 0 | 0 | 1.39 | 3.90 | -3.87-3.87 | |
| B2 | -0.23 | -3.08-2.66 | 1.4 | 3.87 | -3.65-3.65 | ||||
| B3 | 0.34 | 2.63-3.34 | 1.47 | 4.07 | -3.73-4.41 | ||||
| ATR baseline level scoliosis meter (degrees) | A | 1.00 | 1.00-1.00 | A1 | 0 | 0 | 1.37 | 3.79 | -3.38-0.38 |
| A2 | -0.32 | -3.03-3.07 | 1.47 | 4.07 | -4.04-4.04 | ||||
| A3 | -0.05 | 2.97 | 1.48 | 4.09 | -4.14-4.14 | ||||
| B | 0.98 | 0.96-0.99 | B1 | 0 | 0 | 1.23 | 3.40 | -3.40-3.40 | |
| B2 | 0.52 | -2.24-2.54 | 1.35 | 3.75 | -2.88-3.91 | ||||
| B3 | 0.53 | 3.28-3.60 | 1.50 | 4.17 | -3.63-4.70 |
Table 5 presents the concurrent validity for the Baseline® Body Level/Scoliosis meter compared to the Scoliometer as well as Cobb angle as measured by radiographs. The correlation between measurements using the Baseline® Body Level/Scoliosis meter and measurements from the Scoliometer for ATR (degrees) was indicated by a Spearman’s rho of 0.78 indicating a good, statistically significant correlation between these measures. When ATR measured with the Scoliometer and Baseline® Body Level/Scoliosis meter were each compared to Cobb angle measured from radiographs, there was a moderately significant correlation of rho = 0.58 and rho = 0.63, respectively. When Cobb angles measured from radiographs were compared with thoracic kyphosis in the sagittal plane, there was a low correlation (rho = 0.32).
| Baseline Level/Scoliosis meter | Cobb angle (degrees) |
| Cervical lordosis (cm) | -0.22 |
| Thoracic kyphosis (cm) | -0.32 |
| Lumbar lordosis (cm) | -0.03 |
| ATR (degrees) | 0.63 |
| Pelvic tilt (degrees) | 0.13 |
| Shoulder tilt (degrees) | -0.00 |
| ATR Scoliometer (degrees) | 0.58 |
| Baseline Level/Scoliosis meter ATR (degrees) | 0.77 |
In line with the study’s objectives, the reliability and validity of the Baseline® Body Level/Scoliosis meter for measuring scoliosis morphology in three anatomical planes were studied. Results showed that the Baseline® Body Level/Scoliosis meter was as accurate as the Scoliometer when used repeatedly by the same examiner or by different examiners for the measurement of ATR in the transverse plane on patients with mild-moderate scoliosis. The Baseline® Body Level/Scoliosis meter had similar reliability in the measurement of ATR when compared to other high quality reliability studies assessing the Scoliometer[6,16,17] and smartphone applications such as the Scolioscreen with an acrylic sleeve[18].
Based on our results for assessment of the sagittal plane, the Baseline® Body Level/Scoliosis meter can be recommended based on excellent reliability for use by trained examiners for measuring thoracic kyphosis and lumbar lordosis on patients with mild-moderate scoliosis. Furthermore, in the measurement of cervical lordosis on patients with mild-moderate scoliosis, the instrument showed adequate reliability but larger variability in measurements between examiners. Previous research suggests that increased cervical kyphosis is often a secondary coupling effect of increased thoracic kyphosis and coronal plan deformation and that despite this, global spine-pelvis alignment remains well-balanced[19]. This suggests that for the purpose of screening mild-moderate scoliosis, measurement of thoracic and lumbar sagittal curvature may be suffice, leaving cervical curvature measures redundant in many cases. However the utility of cervical curvature measurement suggests that in may be relevant for some mild-moderate cases and may be of more importance when screening moderate-severe scoliosis.
When compared to the reliability of 3D computerized systems, the Baseline® Body Level/Scoliosis meter had similar reliability for thoracic measures but was less reliable for measuring lordotic sagittal curvatures[20]. Potential challenges in the accuracy of palpation of anatomical landmarks have been noted in reliability studies to cause observer variations especially in the sagittal and frontal planes[7,21,22].
A low inter-examiner reliability was found between trained examiners when measuring frontal plane morphology in patients with mild-moderate scoliosis. The Baseline® Body Level/Scoliosis meter had similar reliability for shoulder and pelvic tilt measurements when compared to previous literature on aesthetic clinical tools, such as the Trunk Aesthetic Clinical Evaluation tool[21]. A potential source of the low reliability could be a low sensitivity for smaller measures in these frontal plane secondary measures of spinal curvature. For example, examiners in our study reported that when using the Baseline® Body Level/Scoliosis meter the fluid filled ball required 2.5 degrees of deformity in order for the ball to move. Therefore, the device was not sensitive for assessment of smaller secondary measures in the frontal plane for pelvic and shoulder tilt, and a digital recorder may be more precise. Based on our results, one can hypothesis that the Baseline® Body Level/Scoliosis meter may be reliable for larger secondary measures in the frontal plane for pelvic and shoulder tilt that are more common in moderate to severe cases of AIS. Future research should therefore assess the reliability and validity of the Baseline® Body Level/Scoliosis meter for patients with moderate to severe cases of AIS, with curvatures > 30-40 degrees to confirm this hypothesis.
In accordance with the secondary objectives of the study, measurements of ATR with the Baseline® Body Level/Scoliosis showed good correlation with measurements from the Scoliometer as well as the Gold Standard Cobb angles from radiographs. When examined in light of previous literature, the device had a similar correlation with Gold Standard Cobb angle from radiographs as the Scoliometer did[6,20], and better validity than 2D photography[23] and trunk surface examination[24] but lower validity than 3D computerized systems[20]. Therefore, the Baseline® Body Level/Scoliosis meter could be used for screening, and to monitor curve progression through measurement of ATR. However, ATR measures alone cannot replace Cobb angle measured from radiographs in the diagnosis of the condition, as it has been discussed in statistical literature that greater accuracy is required, with Spearman’s correlation of > 0.9, for a measure to be considered accurate for diagnosis[15]. Furthermore, it is important to note that when screened, not all adolescents have an ATR of the spine, despite changes in the sagittal and frontal planes. When the apex of the Cobb angle is higher up the thoracic region, less rotation is seen in the spine due to coupled movement[25].
Additional frontal and sagittal plane measurements provided by the Baseline® Body Level/Scoliosis meter may add important information regarding clinical signs of progression to inform treatment and diagnostic decisions. Cervical and thoracic sagittal curves and frontal plane measures in our study had however low correlation with Cobb angle, perhaps because a Cobb angle of 25° may not have been severe enough and considering we had a larger group of patients with thoracic curves who often have less disturbed lordosis in the cervical and lumbar spine[25].
This study has its strengths and weaknesses one must consider when interpreting results. A methodological strength of the study was that two physiotherapists performed measurements in 3 anatomical planes for all subjects using the same Baseline® Body Level/Scoliosis meter with no knowledge of results between examiners. The therapists received 5 h training, and were considered proficient with application of the tool. Although there is no recommendation in the literature regarding the training time necessary, previous studies have trained up to 10 h of which the authors suggested contributed to the good to excellent reliability within the study[26]. The study method aimed to control potential variance in measures caused by fatigue from repeated measures by providing rest periods between measurements. Similarly the study method aimed to control variance due to patient flexibility, body mass index (BMI) or previous activity by re-testing within the same session. The methods lacked however intra-rater reliability measures for sagittal and frontal plan measures which could have provided more thorough information on reliability of the Baseline® Body Level/Scoliosis meter
With regards to sample representativeness it can be considered a strength that our patient sample is consecutively recruited, has a female to male 6.8:1 ratio and main thoracic (1AN) to thoracolumbar/lumbar (5CN) 2:1 curve type ratio representative of the current prevalence of AIS in the population for a mean curvature of 20°-30°[27]. A possible limitation however is our sample size was not powered for gender or curve type subgroup analysis[27]. The size of our recruited sample was however adequate to establish group level clinically important change values and the sample was well above the minimum suggested sample size of 15-20 patients for reliability studies with continuous data[11].
Despite the discussed strengths and weaknesses of the study, the benefits of the Baseline® Body Level/Scoliosis meter outweigh the use of the Scoliometer and Cobb angle for initial screening of mild-moderate scoliosis. This mainly due to it providing reliable, valid, feasible and acceptable measures in several anatomical planes aiding decision making regarding the need for radiographic exposure and potential interventions to prevent AIS progression and dysfunction.
Within the study the authors were able to investigate the manual anthropometric measurement of 3D curvatures in AIS with a device that is inexpensive, easily administered and applicable in a clinical setting. The Baseline® Body Level/Scoliosis meter has the ability to provide reliable and valid measurements of mild-moderate scoliosis deformity in transverse and sagittal planes for the cervical, thoracic and lumbar spine, useful for screening scoliosis morphology.
Adolescent idiopathic scoliosis (AIS) is a structural deformation of the spine in the frontal, sagittal and transverse plans. Methods for the clinical evaluation of trunk deformity in all 3 planes that are reliable, valid, feasible and acceptable are of great importance for the prospecive measurement of severity and assessing the need of interventions to prevent deformity progression and dysfunction. Currently repeated radiological exposure or non-radiological methods requiring expensive equipment, specialized training and complex data processing are available.
Current no published research has investigated the reliability and/or validity and discussed the feasibility and acceptability of simple, inexpensive clinical tools that assess trunk deformity in all 3 anatomical planes.
The Baseline® Body Level/Scoliosis meter is an inexpensive and easy to administer clinical tool that can be used to obtain quick measurements of scoliosis morphology in three anatomical planes. It provides reliable transverse and sagittal cervical, thoracic and lumbar measurements as well as valid transverse plane measurements of mild-moderate scoliosis deformity. Poor reliability in frontal plane measures is likely due to the Baseline® Body Level/Scoliosis meter not being sensitive in the first 0-2.5 degrees of pelvic and shoulder tilt which was common in mild-moderate AIS.
The Baseline® Body Level/Scoliosis meter is recommended for transverse and sagittal cervical, thoracic and lumbar measurements of mild-moderate scoliosis. It should be combined with a thorough history and physical assessment to aid decision making regarding the need for radiographs and interventions to prevent AIS progression and dysfunction. It is potentially reliable in measuring larger frontal plane deformity of pelvic and shoulder tilt which is more common in moderate-severe scoliosis but research is needed to confirm this.
AIS is a three-dimensional structural deformation of the spine in otherwise normal adolescents during puberty. Axial thoracic rotation and Cobbs angle are common single pain measures of scoliosis morphology. Reliability refers to the reproducibility of measurements. Validity describes the extent to which a measure accurately represents the concept it claims to measure.
This is a well performed study with sound statistics and clear reliability tests. This is a non-invasive method for the evaluation of frontal and sagittal curvatures in mild AIS individuals.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Sweden
Peer-review report classification
Grade A (Excellent): A, A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): E
P- Reviewer: Erkan S, Korovessis P, Singh K S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Hawes MC, O’brien JP. The transformation of spinal curvature into spinal deformity: pathological processes and implications for treatment. Scoliosis. 2006;1:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 72] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 2. | Sabirin J, Bakri R, Buang SN, Abdullah AT, Shapie A. School scoliosis screening programme-a systematic review. Med J Malaysia. 2010;65:261-267. [PubMed] |
| 3. | Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA. Adolescent idiopathic scoliosis. Lancet. 2008;371:1527-1537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 754] [Cited by in RCA: 902] [Article Influence: 53.1] [Reference Citation Analysis (0)] |
| 4. | Zaina F, Atanasio S, Negrini S. Clinical evaluation of scoliosis during growth: description and reliability. Stud Health Technol Inform. 2008;135:125-138. [PubMed] |
| 5. | Bunnell WP. An objective criterion for scoliosis screening. J Bone Joint Surg Am. 1984;66:1381-1387. [PubMed] |
| 6. | Coelho DM, Bonagamba GH, Oliveira AS. Scoliometer measurements of patients with idiopathic scoliosis. Braz J Phys Ther. 2013;17:179-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 7. | Korovessis PG, Stamatakis MV. Prediction of scoliotic cobb angle with the use of the scoliometer. Spine (Phila Pa 1976). 1996;21:1661-1666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 64] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Fortin C, Feldman DE, Cheriet F, Gravel D, Gauthier F, Labelle H. Reliability of a quantitative clinical posture assessment tool among persons with idiopathic scoliosis. Physiotherapy. 2012;98:64-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 50] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 9. | Prowse A, Pope R, Gerdhem P, Abbott A. Reliability and validity of inexpensive and easily administered anthropometric clinical evaluation methods of postural asymmetry measurement in adolescent idiopathic scoliosis: a systematic review. Eur Spine J. 2016;25:450-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Kottner J, Audigé L, Brorson S, Donner A, Gajewski BJ, Hróbjartsson A, Roberts C, Shoukri M, Streiner DL. Guidelines for Reporting Reliability and Agreement Studies (GRRAS) were proposed. J Clin Epidemiol. 2011;64:96-106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1020] [Cited by in RCA: 1373] [Article Influence: 91.5] [Reference Citation Analysis (0)] |
| 11. | Lexell JE, Downham DY. How to assess the reliability of measurements in rehabilitation. Am J Phys Med Rehabil. 2005;84:719-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 384] [Cited by in RCA: 458] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 12. | Cobb JR. The American Academy of Orthopedic Surgeons Instructional Course Lectures. Vol. 5. Ann Arbor, MI: Edwards 1948; . |
| 13. | Fleiss JL. The Design and Analysis of Clinical Experiments. New York: John Wiley Sons 1986; 1-432. |
| 14. | Hopkins WG. Measures of reliability in sports medicine and science. Sports Med. 2000;30:1-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2699] [Cited by in RCA: 2953] [Article Influence: 118.1] [Reference Citation Analysis (0)] |
| 15. | Munro BH, Visintainer MA. Statistical methods for health care research. Vol 1, 5th ed. Philadelphia: Lippincott Williams and Wilkins 2005; 1-494. |
| 16. | Bonagamba GH, Coelho DM, Oliveira AS. Inter and intra-rater reliability of the scoliometer. Rev Bras Fisioter. 2010;14:432-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Murrell GA, Coonrad RW, Moorman CT, Fitch RD. An assessment of the reliability of the Scoliometer. Spine (Phila Pa 1976). 1993;18:709-712. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 54] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 18. | Driscoll M, Fortier-Tougas C, Labelle H, Parent S, Mac-Thiong JM. Evaluation of an apparatus to be combined with a smartphone for the early detection of spinal deformities. Scoliosis. 2014;9:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Yu M, Silvestre C, Mouton T, Rachkidi R, Zeng L, Roussouly P. Analysis of the cervical spine sagittal alignment in young idiopathic scoliosis: a morphological classification of 120 cases. Eur Spine J. 2013;22:2372-2381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 20. | Somoskeöy S, Tunyogi-Csapó M, Bogyó C, Illés T. Accuracy and reliability of coronal and sagittal spinal curvature data based on patient-specific three-dimensional models created by the EOS 2D/3D imaging system. Spine J. 2012;12:1052-1059. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 80] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 21. | Zaina F, Negrini S, Atanasio S. TRACE (Trunk Aesthetic Clinical Evaluation), a routine clinical tool to evaluate aesthetics in scoliosis patients: development from the Aesthetic Index (AI) and repeatability. Scoliosis. 2009;4:3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 50] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 22. | Pearsall DJ, Reid JG, Hedden DM. Comparison of three noninvasive methods for measuring scoliosis. Phys Ther. 1992;72:648-657. [PubMed] |
| 23. | Fortin C, Feldman DE, Cheriet F, Labelle H. Validity of a quantitative clinical measurement tool of trunk posture in idiopathic scoliosis. Spine (Phila Pa 1976). 2010;35:E988-E994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 24. | Grosso C, Negrini S, Boniolo A, Negrini AA. The validity of clinical examination in adolescent spinal deformities. Stud Health Technol Inform. 2002;91:123-125. [PubMed] |
| 25. | Schlösser TP, Shah SA, Reichard SJ, Rogers K, Vincken KL, Castelein RM. Differences in early sagittal plane alignment between thoracic and lumbar adolescent idiopathic scoliosis. Spine J. 2014;14:282-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 55] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 26. | ROAF R. Rotation movements of the spine with special reference to scoliosis. J Bone Joint Surg Br. 1958;40-B:312-332. [PubMed] |
| 27. | Konieczny MR, Senyurt H, Krauspe R. Epidemiology of adolescent idiopathic scoliosis. J Child Orthop. 2013;7:3-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 459] [Cited by in RCA: 659] [Article Influence: 54.9] [Reference Citation Analysis (0)] |