Published online Sep 18, 2016. doi: 10.5312/wjo.v7.i9.618
Peer-review started: March 29, 2016
First decision: May 17, 2016
Revised: May 29, 2016
Accepted: July 11, 2016
Article in press: July 13, 2016
Published online: September 18, 2016
Processing time: 167 Days and 1.2 Hours
Compartment syndrome is a rare complication of total knee replacement (TKR) surgery that needs prompt diagnosis and treatment as it may be associated with high morbidity and mortality. We have found very few reports in the literature describing compartment syndrome after TKRs and therefore, present a relevant case which occurred in the immediate postoperative phase and was treated with fasciotomy and subsequent operations to close the soft tissue defects.
Core tip: A case report and literature review of compartment syndrome following total knee replacement surgery is presented. Predisposing factors supported by literature are detailed and compared to findings from this case report emphasizing on early intervention to prevent subsequent complications.
- Citation: Shaath M, Sukeik M, Mortada S, Masterson S. Compartment syndrome following total knee replacement: A case report and literature review. World J Orthop 2016; 7(9): 618-622
- URL: https://www.wjgnet.com/2218-5836/full/v7/i9/618.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i9.618
Compartment syndrome is a serious condition that occurs due to elevation of interstitial pressure in closed fascial compartments resulting in microvascular compromise, myoneuronal function impairment and soft tissue necrosis. Fractures, crush injuries, vascular injuries, prolonged tourniquet application, anticoagulation and deep-vein thrombosis have all been associated with compartment syndrome[1], with fractures and soft tissue injuries accounting for approximately 80% of all cases. Pain out of proportion and pain on passive stretching of the affected compartment have been described as the most reliable clinical indicators of compartment syndrome. These symptoms alongside palor, pulselessness, paraesthesia and paralysis are characteristic for compartment syndrome. Paraesthesia and paralysis arise as a result of significant compartmental ischaemia, after which a full recovery becomes unlikely[1].
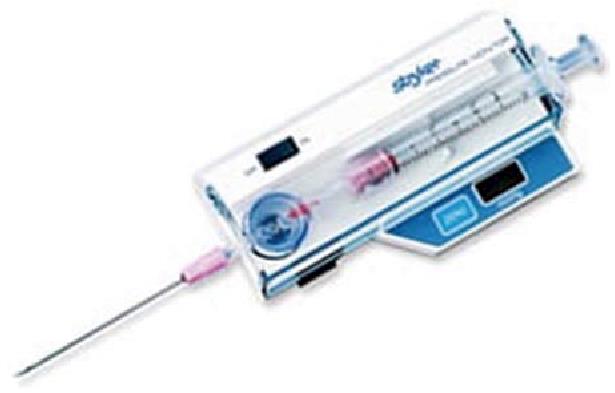
The increase in intracompartmental pressures can be measured using the Wick catheter technique[2] or a handheld manometer. A manometer device attached to a needle is inserted into each compartment to provide a pressure reading. A normal compartmental pressure reflects the capillary pressure of 0 to 8 mmHg. When measured, an intracompartmental pressure of 30 mmHg and delta (differential) pressure of 30 mmHg or less are used as an indication for fasciotomy[3].
Despite the relative scarcity in the incidence of compartment syndrome following total knee replacement (TKR), it remains an important complication which may potentially be limb as well as life threatening.
We hereby, present a case of a compartment syndrome which occurred following TKR surgery and discuss the potential factors which may have contributed to its development.
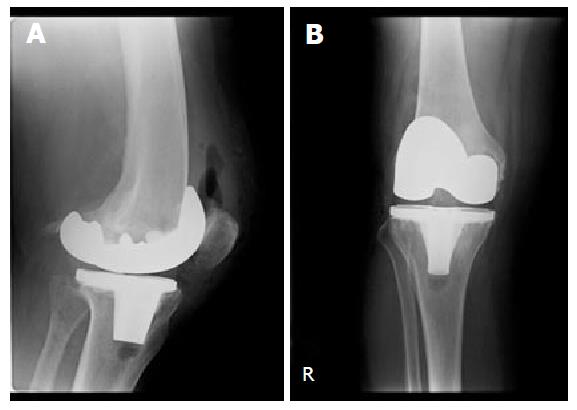
In May 2013, a 72-year-old white British lady with background of chronic obstructive pulmonary disease (COPD), hypertension, prior pulmonary embolism, oesophagitis and cataracts was admitted with a diagnosis of primary osteoarthritis for an elective right TKR. Her medications included spiriva18 mcg, uniphyllin 200 mg, ramipril 1.25 mg, folic acid 5 mg, amlodipine 10 mg, ipratropium 500 mcg, omeprazole 20 mg and salbutamol inhaler and she had no medication allergy. The patient occasionally also used home oxygen therapy for COPD exacerbations. Past surgical history included epistaxis needing cautery, duodenal ulcer surgery and gastroscopy. Family history was insignificant. She was a housewife and lived alone, a previously heavy smoker but stopped one year prior to her presentation and drank alcohol occasionally. Her clinical examination confirmed tenderness over the medial and lateral knee compartments as well as the retropatellar region with a range of movement from 0-120 degrees of flexion. There were no signs of neurological deficit or vascular compromise in the lower limbs. Radiographs taken pre-operatively showed tricompartmental osteoarthritis. Her ASA grading was 3[4]. The surgical procedure was performed as per the surgeon’s routine practice under a spinal/epidural anaesthetic. Patient had three doses of perioperative cefuroxime as per hospital antibiotic prophylaxis guidelines. After elevation of the limb, a pneumatic tourniquet around the upper part of the thigh was inflated to a pressure of 300 mmHg. A midline skin incision and medial parapatellar approach were utilised to expose the knee joint. Standard surgical techniques for intraoperative haemostasis were used. A cemented Columbus® TKR was implanted. After all components were cemented into place, a thorough washout with normal saline was performed and the wound was closed in layers. No surgical drain was used. The tourniquet was released after the application of dressings. Tourniquet time was 90 min. Forty mgs of clexane (enoxaparin) was given on the day of surgery with the plan to continue for 4 wk. The patient returned to the recovery unit where an anteroposterior and lateral X-rays of her right knee were performed as per departmental protocol (Figure 1). After an uneventful recovery, she was transferred to the ward to undergo rehabilitation. The following day she started complaining of pain in the right lower leg which by midday became excruciating and was exacerbated by any passive movement of the toes. The patient experienced tension across the entirety of the calf as well as paraesthesia. The distal pulses in the leg were palpable but weak. A clinical diagnosis of compartment syndrome of the leg was made based on these clinical findings and a Stryker Intra-Compartmental Pressure Monitor measured pressures of 26, 32 and 42 mmHg in the anterior, lateral and posterior compartments respectively (Figure 2).
Therefore she was taken immediately to the operating theatre and a decompression of all 4 compartments was performed using lateral and medial longitudinal incisions. Post fasciotomies the blood supply to the muscles which were deemed viable at the time of surgery was restored and pain was markedly relieved. The patient had to go back to theatre three times subsequently in order to completely close the wounds. The lateral incision was closed 3 d postoperatively while the medial incision was closed 3 wk later after a period of vacuum pump application.
The patient was followed up as an inpatient until complete closure of all wounds. On further examination, she was mobilizing fully weightbearing with no restrictions and achieved a range of movement from 0-95 degrees of flexion. At 12 mo follow-up appointment, the patient maintained her good functional outcome with no neurovascular deficit in the right lower limb and hence got discharged. However, in December 2014, she died from respiratory failure secondary to lung cancer. Reviewing her case notes did not show any deterioration of her knee prior to her death.
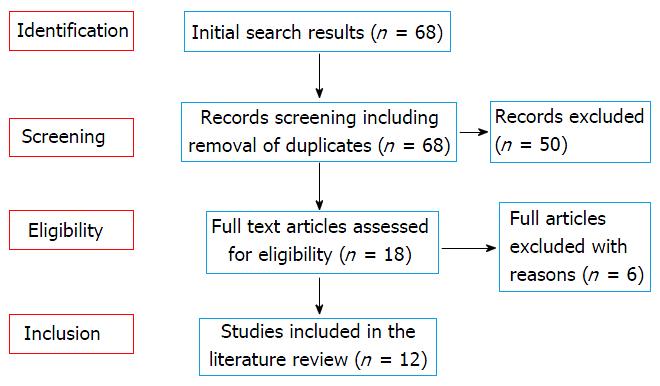
Owing to the rarity of this complication, a comprehensive literature review aiming to identify contributing factors was conducted. The exploded MeSH terms “total knee replacement” and “Compartment syndrome” were used to search MEDLINE and EMBASE databases for relevant articles in English. Two authors independently reviewed the titles and abstracts and when in doubt the full articles were retrieved and reviewed to reach consensus. Following this irrelevant studies were excluded. We included only cases where a unilateral primary TKR was performed to provide direct comparisons with the current case report. This yielded 12 studies which were relevant to our case report[3,5-15]. A PRISMA chart with the study selection process is outlined in Figure 3.
The literature review showed that compartment syndrome varies with regards to its onset and implications after TKR surgery. The time period from TKR to fasciotomy ranged from 14 to 192 h (Table 1). Such variation may be attributed to the masking effect of spinal/epidural anaesthesia. Eight out of 25 patients who underwent fasciotomies had no complications. However, 15 patients developed complications 8 of whom had permanent foot drop; one patient underwent an above and another patient below knee amputation. It is therefore important to intervene in a timely fashion and have a low threshold of performing a fasciotomy to prevent such serious complications. On the other hand, a recent review of 6 cases of compartment syndrome post TKR surgery showed overall high complication rates associated with treatment in this group of patients[3]. In particular, 2 patients developed periprosthetic infections one of whom ended up with an above knee amputation and 2 developed foot drops. As a result, authors suggested that surgeons need to maintain a relatively higher threshold for performing a fasciotomy following TKR in comparison to trauma patients who develop a compartment syndrome. However, it is worth mentioning that in this case series, all patients not only had a spinal anaesthetic but most of them also underwent vascular procedures prior to the fasciotomies. This may have adversely affected the result of the fasciotomies which were delayed in favour of such vascular interventions. In our case, had it not been for our low threshold for surgery and high index of suspicion, our patient may have developed complications. Therefore we disagree with the suggestion of delayed intervention in compartment syndrome developing after TKR surgery and support early treatment to avoid any complications.
| Age | Tourniquet pressure (mmHg) | Anticoagulation | Anaesthetic | Time to treatment (h) | Location | Fasciotomy | Complications | |
| Boonstra et al[5] | 62 | 350 | Yes | GA and Femoral block | 24 | Thigh | Yes | None |
| Haggis et al[6] | 69 | 350 | No | Epidural | 14 | Leg | Yes | Foot drop and equinus |
| 53 | N/A | No | Epidural | 38 | Thigh | Yes | Foot drop and equinus | |
| 65 | 300 | No | Spinal | 24 | Leg | Yes | None | |
| 48 | 350 | No | Epidural | 192 | Leg | Yes | Foot drop and numb sole | |
| 39 | 350 | Yes | Epidural | 20 | Leg | Yes | Foot drop and equinus/infected TKR | |
| 49 | 350 | No | Epidural | 51 | Leg | Yes | Foot drop | |
| 61 | 350 | Yes | Epidural | 38 | Leg | Yes | Below knee amputation | |
| Hailer et al[7] | 43 | 275 | Yes | Epidural | 50 | Leg | Yes | Pes equinus. Complete plegia of all muscle groups distal to the knee. Anesthesia of the sole of the foot |
| Kort et al[8] | 44 | 300 | N/R | Spinal + Epidural | 22 | Leg | Yes | Neurologic impairment and pain |
| Kumar et al[9] | 46 | N/R | No | Spinal + Epidural | 48 | Gluteal | Yes | None |
| 72 | N/R | Yes | Epidural | 47 | Gluteal | Yes | Trendelenburg gait | |
| Lareau et al[10] | 73 | N/R | N/R | GA and Femoral block | Approximately 36 | Thigh | Yes | None |
| Nadeem et al[11] | 71 | N/R | Yes | N/R | N/R | Thigh | Yes | None |
| Osteen et al[12] | 52 | N/R | N/R | Epidural | Approximately 48 | Gluteal | Yes | None |
| Pacheco et al[13] | 47 | N/R | N/R | Epidural | 44 | Gluteal | Yes | Gluteal discomfort |
| 71 | N/R | N/R | Epidural | Approximately 48 | Gluteal | Yes | Motor and sensory impairment distal to the knee | |
| Smith et al[14] | 66 | N/R | Yes | Epidural | N/R | Thigh | No | None |
| Tang et al[15] | 62 | 300 | N/R | Epidural | Approximately 48 | Leg | Yes | Calf numbness |
| Vegari et al[3] | 81 | 350 | No | Spinal | 20 | Leg | Yes | Non-healing wounds |
| 74 | 325 | No | Spinal + Epidural | 24 | Leg | Yes | Skin/muscle necrosis | |
| 61 | 250 | Yes | Spinal + Epidural | 70 | Leg | Yes | Foot drop | |
| 56 | 300 | Yes | Spinal + Epidural | 17 | Leg | Yes | None | |
| 70 | 250 | Yes | Spinal | 18 | Leg | Yes | Above knee amputation | |
| 62 | 250 | Yes | Spinal | 26 | Leg | Yes | Foot drop | |
| Our case | 72 | 300 | Yes | Spinal + Epidural | 31 | Leg | Yes | None |
Compartment syndrome following TKR is an exceptionally rare complication, with only a small number of cases documented in the literature[3,5-15]. The commonest explanation is that a TKR involves the joint space without affecting the adjacent compartments[6,7,15]. However there have been sporadic cases of compartment syndrome following TKR affecting the gluteal, thigh and leg compartments. The recommended treatment is urgent fasciotomy with subsequent debridement and wound closure.
Numerous factors contributing to the development of compartment syndrome and the delay in diagnosing it have been suggested in the literature as follows.
Tourniquet pressure has been highlighted as a potential cause of raised intracompartmental pressure due to reperfusion following tourniquet release[8]. Haggis et al[6] suggested a correlation between higher tourniquet pressure and long term complications with the patient having the lowest tourniquet pressure suffering no long term complications. However when holistically considering all the cases described; a correlation between tourniquet pressure and severity of long term complications could not be established (Table 1).
Epidural anaesthesia has been discussed in several case reports. Two studies[7,15] described how a delay in the diagnosis of compartment syndrome due to the epidural masking pain, led to long term functional deficits. Two further studies[9,13] found that symptoms of gluteal compartment syndrome in four patients following TKR only appeared after withdrawal of the epidural. Hence, Hailer et al[7] suggested that epidural anaesthesia should be avoided after any lower limb orthopaedic surgery in order to allow for early detection of compartment syndrome.
Despite papers suggesting that thromboprophylaxis may predispose to compartment syndrome due to associated excessive bleeding, only half of the cases presented in the literature received anticoagulant medication[3,5-15].
Vegari et al[3] stated that vascular injury is the commonest cause of compartment syndrome following TKR. However, cases described in this review failed to determine any direct causal relationship.
Lareau et al[10] suggested overuse of the continuous passive movement machine as a cause of compartment syndrome. Continuous flexion and extension of the knee joint for a prolonged period may decrease the volume of the compartments thereby increasing intra-compartmental pressure. Another case of compartment syndrome of the thigh following TKR reported that compartmental pressures (measured using a continuous intracompartmental pressure monitor) would only increase on flexion of the knee joint[14]. Knee flexion exacerbated the pain whilst increasing the compartmental pressures which confirms that pain is a very reliable indicator of the severity of compartment syndrome.
In the case presented hereby, we believe that a combination of using a tourniquet and maybe thromboprophylaxis were contributive factors for developing compartment syndrome. However, the use of regional anaesthetic certainly added to the delay in presenting the symptoms as well.
This case report and review of the literature emphasizes the importance of having a high index of suspicion and low threshold of intervention for compartment syndrome occurring after TKRs.
A 72-year-old presented with excruciating right lower leg pain one day following an elective total knee replacement.
Pain on passive movement of the toes, tension across the entirety of the calf as well as paraesthesia. The distal pulses in the leg were palpable but weak.
Compartment syndrome vs simple postoperative swelling after total knee replacement (TKR) surgery.
Not relevant in this case report. However, the Stryker Intra-Compartmental Pressure Monitor was used to measure intracompartmental pressures of the anterior, lateral and posterior compartments.
Fasciotomy with decompression of all four leg compartments, followed by wound closure.
Compartment syndrome following TKR is an exceptionally rare complication, with only a small number of cases documented in the literature. Factors potentially contributing to the development of compartment syndrome and the delay in its diagnosis include vascular injury, thromboprophylaxis, the use of a tourniquet and regional anaesthesia delaying the diagnosis.
Compartment syndrome is a serious condition that occurs due to elevation of interstitial pressure in closed fascial compartments resulting in microvascular compromise, myoneuronal function impairment and soft tissue necrosis.
Compartment syndrome following TKR is rare. However, a high index of suspicion and low threshold of intervention is necessary in order to avoid disastrous consequences.
The authors presented a case with compartment syndrome following TKR, which was a rare complication successfully treated by urgent fasciotomy. The manuscript is well written.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: United Kingdom
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Fenichel I, Ohishi T, Pastides PS, Zak L S- Editor: Ji FF L- Editor: A E- Editor: Li D
| 1. | Elliott KG, Johnstone AJ. Diagnosing acute compartment syndrome. J Bone Joint Surg Br. 2003;85:625-632. [PubMed] |
| 2. | Russell WL, Apyan PM, Burns RP. Utilization and wide clinical implementation using the wick catheter for compartment pressure measurement. Surg Gynecol Obstet. 1985;160:207-210. [PubMed] |
| 3. | Vegari DN, Rangavajjula AV, Diiorio TM, Parvizi J. Fasciotomy following total knee arthroplasty: beware of terrible outcome. J Arthroplasty. 2014;29:355-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Derrington MC, Smith G. A review of studies of anaesthetic risk, morbidity and mortality. Br J Anaesth. 1987;59:815-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 95] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 5. | Boonstra RH, Haverkamp D, Campo MM, van der Vis HM. Acute compartment syndrome of the thigh following total knee arthroplasty. Knee. 2012;19:151-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Haggis P, Yates P, Blakeway C, Fick D, Morgan DA, Holt M, Wood D. Compartment syndrome following total knee arthroplasty: a report of seven cases. J Bone Joint Surg Br. 2006;88:331-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 28] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 7. | Hailer NP, Adalberth G, Nilsson OS. Compartment syndrome of the calf following total knee arthroplasty--a case report of a highly unusual complication. Acta Orthop. 2007;78:293-295. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Kort NP, van Raay JJ, van Horn JR. Compartment syndrome and popliteal vascular injury complicating unicompartmental knee arthroplasty. J Arthroplasty. 2007;22:472-476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Kumar V, Saeed K, Panagopoulos A, Parker PJ. Gluteal compartment syndrome following joint arthroplasty under epidural anaesthesia: a report of 4 cases. J Orthop Surg (Hong Kong). 2007;15:113-117. [PubMed] |
| 10. | Lareau JM, Robbins CE, Talmo CT, Mehio AK, Puri L, Bono JV. Complications of femoral nerve blockade in total knee arthroplasty and strategies to reduce patient risk. J Arthroplasty. 2012;27:564-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Nadeem RD, Clift BA, Martindale JP, Hadden WA, Ritchie IK. Acute compartment syndrome of the thigh after joint replacement with anticoagulation. J Bone Joint Surg Br. 1998;80:866-868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Osteen KD, Haque SH. Bilateral gluteal compartment syndrome following right total knee revision: a case report. Ochsner J. 2012;12:141-144. [PubMed] |
| 13. | Pacheco RJ, Buckley S, Oxborrow NJ, Weeber AC, Allerton K. Gluteal compartment syndrome after total knee arthroplasty with epidural postoperative analgesia. J Bone Joint Surg Br. 2001;83:739-740. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Smith PN, Rampersaud R, Rorabeck CH. Incipient compartment syndrome of the thigh following total knee arthroplasty. J Arthroplasty. 1997;12:835-838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Tang WM, Chiu KY. Silent compartment syndrome complicating total knee arthroplasty: continuous epidural anesthesia masked the pain. J Arthroplasty. 2000;15:241-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 38] [Article Influence: 1.5] [Reference Citation Analysis (0)] |