Published online Aug 18, 2016. doi: 10.5312/wjo.v7.i8.513
Peer-review started: January 24, 2016
First decision: March 24, 2016
Revised: April 4, 2016
Accepted: June 14, 2016
Article in press: June 16, 2016
Published online: August 18, 2016
Processing time: 207 Days and 18.3 Hours
To ascertain the effectiveness of slacklining as a supplementary therapy for elderly stroke patients who are functionally non-progressing. This case study involved an 18-mo prospective observation of the management of an 87-year-old female stroke-patient of the left hemisphere with reduced balance, reduced lower limb muscular activation, hypertonia, and concurrent postural deficits. This entailed the initial acute care phase through to discharge to home and 18-mo final status in her original independent living setting. The introduction of slacklining as an adjunct therapy was made 12 mo post incident. Slacklining involves balance retention on a tightened band where external environmental changes cause a whole-body dynamic response to retain equilibrium. It is a complex neuromechanical task enabling individualized self-developed response strategies to be learned and adapted. This facilitates the innate process of balance retention, lower-limb and core muscle activation, and stable posture through a combination of learned motor skills and neurological system down regulation. Individuals adopt and follow established sequential motor learning stages where the acquired balance skills are achieved in a challenging composite-chain activity. Slacklining could be considered an adjunct therapy for lower limb stroke rehabilitation where function is compromised due to decreased muscle recruitment, decreased postural control and compromised balance. Initial inpatient rehabilitation involved one-month acute-care, one-month rehabilitation, and one-month transitional care prior to home discharge. A further six months of intensive outpatient rehabilitation was provided with five hourly sessions per week including:supervised and self-managed hydrotherapy, plus one individual and two group falls’ prevention sessions. These were supported by daily home exercises. At 12 mo post incident, recovery plateaued, then regressed following three falls. Rehabilitation was subsequently modified with the hydrotherapy retained and the group sessions replaced with an additional individual session supplemented with slacklining. The slacklining followed stages one and two of a standardized five-stage protocol. Self-reported functional progression resumed with improvement by 14 mo which further increased and was sustained 18 mo (Students’t test P < 0.05). Slacklining’s external stimulations activate global-body responses through innate balance, optimal postural and potentially down-regulated reflex control. Incorporated into stroke rehabilitation programs, slacklining can provide measurable functional gains.
Core tip: Slacklining may supplement stroke rehabilitation where lower limb function is compromised. This case study considers an 87-year-old female with reduced balance, reduced lower limb activation, and hypertonia. Rehabilitation from acute care to home discharge and subsequent six-month intensive outpatient therapy showed progression then plateaued at nine months. Three falls resulted in regression and rehabilitation was modified by supplementing slacklining. Functional progression improved by 14 mo and was sustained at 18 mo. Slacklining’s external stimulations activate global-body responses through innate balance, optimal postural response and potentially down-regulated reflex control that can provide quantifiable functional gains. Further prospective cohort studies are required.
- Citation: Gabel CP, Rando N, Melloh M. Slacklining and stroke: A rehabilitation case study considering balance and lower limb weakness. World J Orthop 2016; 7(8): 513-518
- URL: https://www.wjgnet.com/2218-5836/full/v7/i8/513.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i8.513
Stroke survivors are often required to adapt to a restricted lifestyle with reduced activities of daily living (ADL). They also have increased dependence on continuous external support to survive[1]. Thirty-five per-cent of Australians who experienced a stroke had a resulting disability, with 64% needing assistance with health care, 58% with mobility and 47% with self-care[2]. Furthermore, this neurologic pathology significantly impacts the ADL of individuals through impaired postural control. Following stroke, some patients have delayed and disrupted equilibrium reactions[3], exaggerated postural sway in both sagittal and frontal planes[4], reduced weight-bearing on the paretic limb during functional tasks[5,6] and an increased risk of falling[7,8].
Additionally, impaired dexterity in both the affected and unaffected lower extremities is a major reported problem post-stroke[9]. Activation failure in the affected lower limb can often be explained by weakness, which correlates strongly with reduced functional performance[7]. Furthermore, the presence of co-activation, muscle activation on both sides of the joint, is a common postural coordination strategy reported in those with neurologic deficits, including stroke[10]. Consequently, research is required for post-stroke rehabilitation strategies that focus strongly on improving the affected lower limb’s dexterity and postural control. One such novel technique not yet reported in the literature is slacklining as a supplementary therapy[11-14]. It is a complex neuromechanical task that involves balance retention on a tightened band where whole-body dynamics drive the response to external environmental changes[13,15]. This activity innately facilitates recruitment of muscles within the core[11,16] and the lower limb, particularly the quadriceps and gluteals[12]. Some studies have found that slacklining has transferable learning and skill acquisition including improved posture[14,17], static and dynamic balance[18-20], lower limb control[12,21,22], joint specific control[12,23,24], sporting performance[13,25] and probable neuroplastic changes[26,27]. Slacklining also stimulates the balance mechanism and functional control through individualized global body responses and learned movement patterns that are adaptations to external stimuli[15,17,22].
This paper presents a case study where slacklining was supplemented to an existing balance and functional control rehabilitation program.
An 87-year-old female who had sustained a non-specific cerebro-vascular accident within the left hemisphere affecting lower limb strength, balance control and hypertonia was monitored over an 18 mo period. Rehabilitation was progressed through five stages: (1) an initial one month of acute inpatient management; (2) one month inpatient rehabilitation at a specialized rehab centre; (3) one month of transitional care in a different inpatient facility to assist home skills for self-care and daily living; (4) home discharge with nine-month early care community support through nursing and carers; plus five times per week intensive outpatient rehabilitation involving hourly sessions of twice weekly occupational and physical therapy group falls prevention, an individual physical therapy session providing balance training, mobilization and massage with planning of additional home exercise, and two hydrotherapy sessions; and (5) management in the community for a further six months with modification of the outpatient sessions combined with the introduction of slacklining and a phase out of regular home care assistance. Slacklining, as part of the neurological rehabilitation program, was introduced and initially graduated over six weeks following the standardized protocol[12,13]. The sessions were initiated at three minutes and increased to seven and, finally, ten minutes in duration. They involved a step up onto the slackline, located over a grassy surface at a height of approximately 20 cm, with the patient provided balance support, initially from the front with both hands touching or holding the therapists hands and progressing to a hand support such as a wheeled frame or a walking stick (Figure 1). The adjunct or supplementary addition of slacklining to the standard rehabilitation program continued after the case study observation period finished at 18 mo. Sessions were twice weekly with minor progressions in the program difficulty levels based upon the individual’s adaptations, capacity and status (Figure 2).
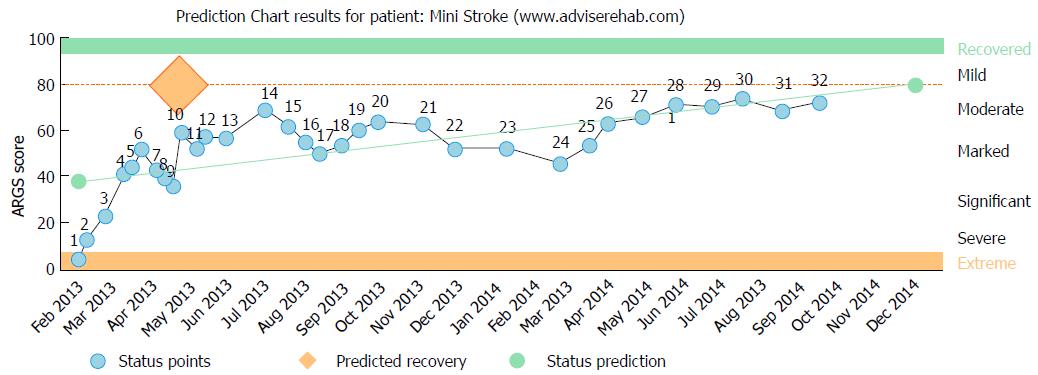
The status and the key points were recorded using computerized decision support software patient-reported outcome measurement[28] (Figure 1). Recovery plateaued at the six-month mark and there was subsequent regression following three falls at home over the subsequent six months despite the specific falls prevention program. At twelve-months the hydrotherapy continued and the group rehabilitation falls prevention program was ceased and replaced by a further individual rehabilitation session that was supplemented with slacklining (Figure 1). The slacklining was provided with the intention of specifically activating the quadriceps[12,22] and improving core muscle recruitment[14,19], postural position and awareness[14,17], and balance[18,21]. The slacklining followed stages one and two of a standardized five-stage, 20-step protocol[13]. This standard protocol was modified through the initial use of hand support that was progressively withdrawn. Initially a bilateral, two hand support position was provided, then progressed to a single hand, then one hand support to a fixed ground object, then a walking stick and finally free-standing and stepping up. At all times immediate close support was available for safety, feedback and confidence. Subsequently, functional status progression resumed with statistically significant improvement over the following six months (Students’ t test P < 0.05) (Figure 2).
Slacklining has an innate or automatic muscle recruitment action, particularly for the quadriceps and to a lesser degree the gluteals, calf and core[12,14]. These actions provide a positive focus for stroke patients with local muscle inhibition from the centrally derived deficits[12].
A further consideration is that the action of standing on a slackline requires muscular recruitment in a sequential and learned manner in order for the individual to remain upright and balanced[12,17]. This is a postural benefit for individuals with lower limb functional deficits of a central source that are acquired following stroke[29,30]. An additional benefit is that the Hoffman’s reflex (H-reflex)[12,31] can be affected through the pre-synaptic pathway[17] resulting in a learned activity that inhibits the reflex action from down regulation[32,33]. Such inhibition is advantageous as the H-reflex shows heightened sensitivity that may negatively affect the gait of stroke survivors[34,35]. However, it is considered to be a learned and temporary effect as withdrawal of the training stimulus results in reduction the training effect. Consequently, the effectiveness of the slacklining program as a rehabilitation therapy must be maintained through the ongoing practice of the activity[11,13,18].
This is of significance as the stroke patient has phase-related modulation of both the soleus H-reflex, that affects the ankle directly and less so the knee - regardless of joint stiffness[29]; and the quadriceps H-reflex primarily affecting the knee control[31]. Both of these actions are also partially disordered during hip movement due to modulated limb spasticity[34,35]. The anticipated beneficial consequence is that the action of slacklining may provide a positive effect through the action of pre-synaptic inhibition and down-regulation of the H-reflex[27] as well as supplement the quadriceps and soleus activation and control[12] in conjunction with balance, postural control, and an overall learning process[14,18,24]. This can assist the individual to adapt towards normalized balance and actively controlled positions[36]. The anticipation is that this specific action within the training phase will then overflow to normal daily activity[17,18] including the functional movements of walking and postural control. This in theory could subsequently improve the innate response action to perturbations and reduce the incidence of falls and in turn improve individual confidence while reducing health and socioeconomic costs[36].
It is widely accepted that the central nervous system of adult human beings has enormous potential for recovery and adaptability. The actions of slacklining can theoretically cause down-regulation of the muscle inhibitory action and the Hoffman reflex. This suppression of a spinal reflex may transfer the control of muscular activation from primary spinal to more supraspinal centers, which can be beneficial in terms of improved movement control[37,38]. Consequently, slacklining and its potential to influence cortical areas and the central nervous system of stroke patients is an area that needs investigation in this population group[34,35].
Slacklining may be a beneficial rehabilitation method that could be incorporated into the programs of stroke patients. The external stimuli activate global-body responses through innate balance and reflex modulations that provide quantifiable functional gains. In addition, the activity of slacklining provides an innate activation of the lower limb muscles, particularly the quadriceps, calf, gluteals and also the trunk core muscles in normal and lower limb injured individuals; consequently, it would seem likely to have a similar effect in stroke patients. Slacklining is a novel adjunct therapy that is challenging and rewarding where quantifiable exercise specific gains can be achieved and potentially transformed into daily functional status improvements in the areas of ADL, gait and balance. Further prospective studies are required to validate these initial findings and eventually to determine therapy frequency and progression rates.
An 87-year-old female stroke patient is discussed within the context of a novel method of rehabilitation through the use of slacklining to facilitate balance and function and to reduce and prevent falls.
Right lower limb weakness, mildly reduced sensation, reduced balance and general limb control with tonal changes and intermittent upper limb tonal alterations to a mild level.
Stroke affecting the right leg below the knee due to a left cerebral vascular accident (CVA).
A progressive graded rehabilitation over 18 mo from inpatients to transitional care and final home and community including a group falls reduction program. Progression to twice weekly physiotherapy outpatients with balance training, limb mobilization and massage and the addition of slacklining.
Stroke is due to a CVA affecting the cortical tissue and slacklining as a novel therapy involves balance retention on a tightened band where external environmental changes cause a whole-body dynamic response to retain equilibrium. As such slacklining is a complex neuromechanical task enabling individualized self-developed response strategies to be learned and adapted to facilitate balance, strength, control and functional improvement and/or stability.
This study offers a new frontier into the use of neural plasticity accessed through physical rehabilitation exercises to enhance and maintain balance and function. This is the first reported study with the use of this novel method of rehabilitation, ”slacklining”, in a clinical setting for stroke.
This paper proposes the activity ‘Slacklining’ as a rehabilitation supplement following stroke in the form of a case report and theoretical explanation. The manuscript is well written, and supported by references appropriately.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Australia
Peer-review report classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Anand A, Kwasnicki RM, Sakamoto A S- Editor: Qiu S L- Editor: A E- Editor: Wu HL
| 1. | Truelsen T, Begg S, Mathers C. The global burden of cerebrovascular disease Geneva, World Health Organisatin. Geneva: WHO 2006; 67. |
| 2. | Australian Institute of Health and Welfare (AIHW). Stroke and its management in Australia: an update. Canberra: AIHW 2013; 150. |
| 3. | Badke MB, Duncan PW. Patterns of rapid motor responses during postural adjustments when standing in healthy subjects and hemiplegic patients. Phys Ther. 1983;63:13-20. [PubMed] |
| 4. | Genthon N, Rougier P, Gissot AS, Froger J, Pélissier J, Pérennou D. Contribution of each lower limb to upright standing in stroke patients. Stroke. 2008;39:1793-1799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 148] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 5. | Engardt M, Olsson E. Body weight-bearing while rising and sitting down in patients with stroke. Scand J Rehabil Med. 1992;24:67-74. [PubMed] |
| 6. | Chou SW, Wong AM, Leong CP, Hong WS, Tang FT, Lin TH. Postural control during sit-to stand and gait in stroke patients. Am J Phys Med Rehabil. 2003;82:42-47. [PubMed] |
| 7. | Horstman AM, Beltman MJ, Gerrits KH, Koppe P, Janssen TW, Elich P, de Haan A. Intrinsic muscle strength and voluntary activation of both lower limbs and functional performance after stroke. Clin Physiol Funct Imaging. 2008;28:251-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 78] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 8. | Kerse N, Parag V, Feigin VL, McNaughton H, Hackett ML, Bennett DA, Anderson CS. Falls after stroke: results from the Auckland Regional Community Stroke (ARCOS) Study, 2002 to 2003. Stroke. 2008;39:1890-1893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 97] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 9. | Kiyama R, Fukudome K, Hiyoshi T, Umemoto A, Yoshimoto Y, Maeda T. The loss of dexterity in the bilateral lower extremities in patients with stroke. J Appl Biomech. 2011;27:122-129. [PubMed] |
| 10. | Lamontagne A, Richards CL, Malouin F. Coactivation during gait as an adaptive behavior after stroke. J Electromyogr Kinesiol. 2000;10:407-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 154] [Cited by in RCA: 146] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 11. | Gabel CP. Slacklining: A Novel Exercise to Enhance Quadriceps Recruitment, Core Strength and Balance Control. J Nov Physiother. 2014;4:4. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Gabel CP, Osborne J, Burkett B. The influence of ‘Slacklining’ on quadriceps rehabilitation, activation and intensity. J Sci Med Sport. 2015;18:62-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Gabel CP, Mendoza S. “Slacklining” - a self-generated, graded training program for lower limb rehabilitation. IJATT. 2013;18:14-19. |
| 14. | Pfusterschmied J, Buchecker M, Keller M, Wagner H, Taube W, Müller E. Supervised slackline training improves postural stability. Eur J Sports Sc. 2013;13:49-57. [RCA] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Paoletti P, Mahadevan L. Balancing on tightropes and slacklines. J R Soc Interface. 2012;9:2097-2108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Anlauff J, Cooperstock JR, Fung J. Augmented feedback for learning single-legged stance on a slackline. 2013;162-163. [DOI] [Full Text] |
| 17. | Keller M, Pfusterschmied J, Buchecker M, Müller E, Taube W. Improved postural control after slackline training is accompanied by reduced H-reflexes. Scand J Med Sci Sports. 2012;22:471-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 75] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 18. | Granacher U, Iten N, Roth R, Gollhofer A. Slackline training for balance and strength promotion. Int J Sports Med. 2010;31:717-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Mahaffey BJ. The Physiological Effects Of Slacklining On Balance And Core StrengthPhysical Education Teaching, University of Wisconsin-La Crosse. Crosse: University of Wisconsin-La Crosse 2009; 62. |
| 20. | Seeber G, Zalpour C. Auswirkungen des Slacklinings “auf die Gleichgewichtsfähigkeit von Senioren. Prävention und Gesundheitsförderung (German). 2012;7:30-35. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Pfusterschmied J, Lindinger S, Buchecker M, Stöggl T, Wagner H, Müller E. Effect of instability training equipment on lower limb kinematics and muscle activity. Sportverletz Sportschaden. 2013;27:28-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Pfusterschmied J, Stöggl T, Buchecker M, Lindinger S, Wagner H, Müller E. Effects of 4-week slackline training on lower limb joint motion and muscle activation. J Sci Med Sport. 2013;16:562-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Mayer C, Siems W. Patellaluxation100 Krankheitsbilder in der Physiotherapie. Berlin: Springer Berlin Heidelberg 2011; 146-157. [DOI] [Full Text] |
| 24. | Di Stasi S, Myer GD, Hewett TE. Neuromuscular training to target deficits associated with second anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2013;43:777-792, A1-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 121] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 25. | De Franceschi PA. Le slackline, un outil prophylactique au service des joueurs de badminton de haut niveau, France, 2012: 12. |
| 26. | Sibley KM, Salbach NM. Applying knowledge translation theory to physical therapy research and practice in balance and gait assessment: case report. Phys Ther. 2015;95:579-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 27. | Zehr EP. Considerations for use of the Hoffmann reflex in exercise studies. Eur J Appl Physiol. 2002;86:455-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 420] [Cited by in RCA: 425] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 28. | Advise Rehab Advise Rehabilitation, decision support software. Coolum Beach, Queensland: Advise rehabilitation Pty Ltd, 2013. |
| 29. | Harburn KL, Vandervoort AA, Helewa A, Goldsmith CH, Kertesz A, Teasell RW, Hill KM. A reflex technique to measure presynaptic inhibition in cerebral stroke. Electromyogr Clin Neurophysiol. 1995;35:149-163. [PubMed] |
| 30. | Yavuzer G, Eser F, Karakus D, Karaoglan B, Stam HJ. The effects of balance training on gait late after stroke: a randomized controlled trial. Clin Rehabil. 2006;20:960-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 124] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 31. | Hopkins JT, Wagie NC. Intrasession and intersession reliability of the quadriceps Hoffmann reflex. Electromyogr Clin Neurophysiol. 2003;43:85-89. [PubMed] |
| 32. | Van Boxtel A. Differential effects of low-frequency depression, vibration-induced inhibition, and posttetanic potentiation on H-reflexes and tendon jerks in the human soleus muscle. J Neurophysiol. 1986;55:551-568. [PubMed] |
| 33. | Schneider C, Lavoie BA, Capaday C. On the origin of the soleus H-reflex modulation pattern during human walking and its task-dependent differences. J Neurophysiol. 2000;83:2881-2890. [PubMed] |
| 34. | Tanabe S, Kamiya A, Muraoka Y, Masakado Y, Tomita Y. Disorder of phase-related modulation of soleus H-reflex during hip movement in stroke patients. Electromyogr Clin Neurophysiol. 2006;46:241-246. [PubMed] |
| 35. | Tanabe S, Muraoka Y, Kamiya A, Tomita Y, Masakado Y. Passive movement of hip and knee joints decreases the amplitude of soleus H-reflex in stroke patients. Electromyogr Clin Neurophysiol. 2004;44:365-370. [PubMed] |
| 36. | Hoffman J, Gabel P. Expanding Panjabi’s stability model to express movement: a theoretical model. Med Hypotheses. 2013;80:692-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 37. | Solopova IA, Kazennikov OV, Deniskina NB, Levik YS, Ivanenko YP. Postural instability enhances motor responses to transcranial magnetic stimulation in humans. Neurosci Lett. 2003;337:25-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 73] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 38. | Taube W, Gruber M, Gollhofer A. Spinal and supraspinal adaptations associated with balance training and their functional relevance. Acta Physiol (Oxf). 2008;193:101-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 204] [Cited by in RCA: 239] [Article Influence: 14.1] [Reference Citation Analysis (0)] |