Published online Dec 18, 2016. doi: 10.5312/wjo.v7.i12.793
Peer-review started: June 29, 2016
First decision: August 5, 2016
Revised: September 15, 2016
Accepted: October 5, 2016
Article in press: October 7, 2016
Published online: December 18, 2016
Processing time: 163 Days and 6 Hours
Metatarsal fractures are one of the most common injuries of the foot. There has been conflicting literature on management of fifth metatarsal fractures due to inconsistency with respect to classification of these fractures. This article provides a thorough review of fifth metatarsal fractures with examination of relevant literature to describe the management of fifth metatarsal fractures especially the proximal fracture. A description of nonoperative and operative management for fifth metatarsal fractures according to anatomical region is provided.
Core tip: Nondisplaced fifth metatarsal fractures can be treated nonoperatively depending on fracture location and patient factors. When nonoperative management is utilized improved early functional scores are associated with less rigid immobilization and a shorter period of nonweightbearing. Neck and shaft fractures with greater than ten degrees plantar angulation or three millimeters of displacement in any plane where closed reduction is insufficient require operative management. Operative intervention is recommended for base of the fifth metatarsal avulsion fractures (zone one) with more than three millimeters of displacement. Acute and delayed union zone two fractures may be managed nonoperatively but operative management with an intramedullary screw should be considered in athletes. Zone three (diaphyseal stress fractures) fractures that are Torg type I and type II should be managed with intramedullary screw fixation in the athlete. In the non-athlete these fractures may be managed nonoperatively however prolonged immobilization is often required and a nonunion may still result. Symptomatic nonunions of zone two and zone three fractures should be managed operatively.
- Citation: Bowes J, Buckley R. Fifth metatarsal fractures and current treatment. World J Orthop 2016; 7(12): 793-800
- URL: https://www.wjgnet.com/2218-5836/full/v7/i12/793.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i12.793
Metatarsal fractures are frequently encountered injuries of the foot[1]. Approximately five to six percent of fractures encountered in the primary care setting are metatarsal fractures[2]. In adults, metatarsal fractures peak in the second to fifth decades of life. The most frequent fracture seen is the fifth metatarsal, accounting for 68% of metatarsal fractures[2]. Proximal fifth metatarsal fractures are divided into three zones[3-5]. Zone one, zone two, and zone three fractures account for 93%, four percent and three percent of proximal fifth metatarsal fractures, respectively[6]. There is some evidence–based literature to help make decisions with these fracture types, which will be described in this review.
The first to describe a fracture of the proximal fifth metatarsal was Sir Robert Jones[7-9]. He described a fracture in the proximal three quarter segment of the shaft distal to the styloid[7-9]. The Jones fracture as described by Sir Robert Jones was later defined by Stewart[10,11] as a transverse fracture at the junction of the diaphysis and metaphysis without extension into the fourth and fifth intermetatarsal articulation. Since then there has been a focus in the literature on fractures of the proximal fifth metatarsal due to the propensity for poor healing of some fractures in this region. The blood supply to the proximal fifth metatarsal is important in understanding troublesome fracture healing in this area. The blood supply of the fifth metatarsal was investigated in a cadaver model by Smith et al[12]. They found that the blood supply arises from three possible sources; the nutrient artery, the metaphyseal perforators, and the periosteal arteries. A watershed area exists between the supply of the nutrient artery and the metaphyseal perforators which corresponds to the area of poor fracture healing in the clinical setting[12]. A classification system created by Torg et al[13] is based on healing potential. This classification simplifies proximal fifth metatarsal fractures as either involving the tuberosity or the proximal diaphysis distal to the tuberosity, the latter group being called the Jones fracture[13,14]. Under this system the Jones fracture is divided into three types based on the radiological appearance of the fracture[13]. Type I (acute) fractures are characterized by a narrow fracture line and an absence of intramedullary sclerosis[13,15,16]. The features of acute fractures in this classification are no history of previous fracture, although previous pain or discomfort may be present[13]. Torg type I fractures are presumed to be acute fractures at a site of pre-existing stress concentration on the lateral cortex that becomes acutely disabling when they extend across the entire diaphysis[13]. Type II (delayed union) are distinguished by having a previous injury or fracture with radiographic features of a widened fracture line and evidence of intramedullary sclerosis (Figure 1)[13,15,16]. Type III (nonunion) are characterized by complete obliteration of the medullary canal by sclerotic bone with a history of repetitive trauma and recurrent symptoms (Figure 2)[13,15,16]. Although the term Jones fracture was applied to the fractures in this classification, based on Torg’s description these fractures are more consistent with stress fractures. As a result, proximal fifth metatarsal fractures were re-classified to avoid the confusing term of Jones fractures. Proximal fifth metatarsal fractures can be classified into three zones as described by Lawrence et al[3] and Dameron[4,5]. Tuberosity avulsion fractures represent zone one (Figure 3)[3-5]. Zone two (Jones fracture) is described as a fracture at the metaphysis-diaphyseal junction. Zone three or diaphyseal stress fractures include the proximal 1.5 cm of the diaphysis[3,4,5,9,17]. This classification is straightforward however, it must be noted that their description of zone two is a slight mis-representation of the true Jones fracture as described by Stewart[11]. It is important to note that the Jones fracture in this classification system is an acute injury with no prodrome whereas zone three fractures have a variable prodome[3]. The distinction between Jones (zone two) and proximal diaphyseal stress fractures (zone three) is commonly confused in the literature which potentially obscures important differences in prognosis and treatment[3,4,10,15]. A systematic review done by Dean et al[14], looked at the classification of Jones fractures in 19 studies. They found that the majority of authors did not differentiate between fractures involving the fourth/fifth intermetatarsal articulation from more distal fractures. They concluded that the Jones fracture is generally applied to all fractures of the proximal fifth metatarsal distal to the tuberosity within 1.5 cm of this region. However, because this is not a universal definition it very difficult to recognize differences in outcomes between operative and nonoperative management of zone two and zone three fractures in the literature. It also indicates that in many cases the literature fails to differentiate the chronicity of zone two and zone three fractures[14].
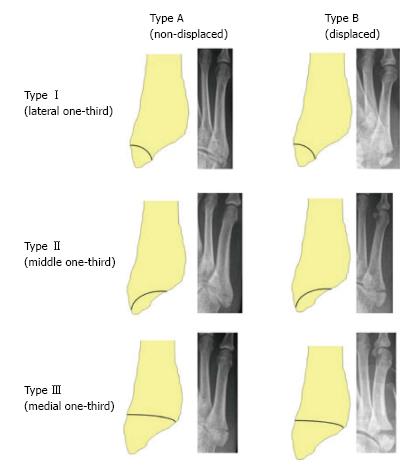
More recently, Mehlhorn et al[18] proposed another classification for base of fifth metatarsal fractures based on radiomorphometric analysis reflecting the risk for secondary displacement. In this classification the joint surface of the fifth metatarsal base is divided into three equal parts. Type I, type II, and type III fractures represent the lateral third, middle third, and medial third respectively (Figure 4). Adding to this classification they introduced an A type which represents no relevant displacement and a B type which denotes a fracture step off of greater or equal to two millimetres[18].
An injury to the fifth metatarsal presents with history of acute trauma or repetitive trauma to the forefoot[19]. Zone one fractures are typically avulsion type injuries. The mechanism of these fractures are an acute episode of forefoot supination with plantar flexion[3,19,20]. This results in pull from the lateral band of the plantar fascia and peroneus brevis[20]. Typically, the fracture pattern is transverse to slightly oblique. Occasionally, these fractures are comminuted, significantly displaced or disrupt the cuboid-base of fifth metatarsal joint[6]. Zone two fractures result from an acute episode[3-5]. The exact mechanism is not known but is thought to result from a large adduction force applied to the forefoot with the ankle plantar flexed[3,4,19]. Zone three fractures (diaphyseal stress fractures) typically results from a fatigue or stress mechanism[3]. Stress fractures of the proximal fifth metatarsal have been defined by DeLee et al[1] as a spontaneous fracture of normal bone that results from a summation of stresses any of which by itself would be harmless. Multiple factors contribute to the development of stress fractures including systemic factors, anatomic factors, and mechanical factors[1]. Although multiple factors contribute the exact mechanical mechanism is unclear. It is thought that either muscle creates a localized force that outweigh the stress-bearing capacity of bone or that when muscle fatigues excessive forces are transmitted to the surrounding bone[19].
Radiographic imaging for a suspected metatarsal fracture includes three standard radiographic views of the foot: Lateral, anteroposterior, and a 45 degree oblique. Acute stress fractures are typically not detected on the standard three views of the foot. It is suggested that repeated radiographs are made at 10 to 14 d after the initial onset of symptoms[9]. At this time a radiolucent reabsorption gap around the fracture confirms the diagnosis[9]. In the case of more complex midfoot trauma, a CT scan is recommended to rule out the Lisfranc fracture dislocation[9].
Management of fifth metatarsal fractures depends on the classification of the fracture, the nature of other injuries sustained, and patient demographics. Taking everything into consideration, along with patient activity level, treatment can be nonoperative or operative.
If there is more than three to four millimeters displacement or ten degrees of plantar angulation of neck or shaft fractures and closed reduction is not sufficient, operative intervention is recommended[10].
Avulsion fractures of the base of the fifth metatarsal that are displaced greater than three millimetres or comminuted should be reduced and operatively fixed[7]. Fracture reduction and fixation should be considered if the fracture fragment involves more than 30% of the cubometatarsal joint[10]. Mehlhorn et al[18] recommended (based on their radiomorphometric analysis) that fractures with larger than a two millimeter step off involving the joint surface be fixed with open reduction internal fixation given the risk for posttraumatic osteoarthritis. They found that fractures they classified as type IIIA (medial joint fracture) had a 45% risk of secondary displacement. Therefore, they recommend that for these fractures, open reduction and internal fixation be a consideration.
Displaced zone two fractures require operative management. Less consensus exists on acute nondisplaced Jones fractures (zone two). There are many studies that advocate for early intramedullary screw fixation for acute Jones fractures in the active population[21-24]. Porter et al[21] demonstrated that acute Jones fractures treated operatively resulted in quicker return to sport and clinical healing in competitive athletes. In this same study, athletes returned to sports at a mean of 7.5 wk (range 10 d to 12 wk). This time period is shorter than the average time to healing with nonoperative management. Mindrebo et al[22] described nine athletes that underwent early percutaneous intramedullary screw fixation and the patients were full weightbearing within seven to ten days. They found that on average the patients were able to return to full sport by 8.5 wk and all had radiographic union by an average of six weeks[22]. Literature published by Quill[23] reports that one in three nonoperatively treated Jones fractures re-fractured and therefore recommended early surgical management.
Another study by Mologne et al[24] compared nonoperative management with a nonweightbearing cast or early intramedullary screw fixation and weightbearing within 14 d. The operative treatment group demonstrated a reduced time to return to sport and faster clinical union by almost 50% compared to the nonoperative group[24]. The incidence of treatment failure in the cast treatment group was 44%. However, it should be noted that in this study a Jones fracture was defined as a type I Torg fracture and did not account for the difference between zone two and three fractures[24].
Zone two delayed unions are a relative indication for surgical intervention. While delayed unions may eventually heal the detrimental effects of prolonged immobilization and nonweightbearing is a reason to consider operative intervention[3].
Surgical intervention is typically recommended for type II and type III diaphyseal stress fractures, as seen in Figure 5[4,25]. Delayed unions may eventually heal by nonoperative means but often require prolonged immobilization and nonweightbearing which is a reason to consider operative management[3,25]. In highly active individuals with a type II diaphyseal stress fracture, operative management is recommended[3,10,25].
Additionally, when making decision between operative and nonoperative management of zone two and zone three fractures hindfoot varus should be excluded. Evidence of hindfoot varus is thought to be a predisposing factor for these fractures as well as re-fracture following fixation. In one study done by Raikin et al[26], 90% of patients with Jones fractures had evidence of hindfoot varus, whereas the incidence of hindfoot varus in the normal population is approximately 24%. In this study Jones fractures included acute and stress fractures of zone two and zone three. It can be concluded that patients presenting with zone two and zone three fractures and clinical hindfoot varus require correction of the varus to prevent re-fracture after operative or nonoperative management. Raikin et al[26] corrected hindfoot varus with a lateral heel wedge and forefoot post inserts which resulted in no re-fractures of operatively managed fractures.
There are a number of nonoperative treatment modalities used for metatarsal fractures. They vary by anatomical region, patient history and radiological findings but evidence based medicine has helped with this treatment type. Isolated nondisplaced shaft and neck fractures of the fifth metatarsal are treated nonoperatively[10,27]. A variety of nonoperative modalities include elastic dressing and a rigid shoe, short leg walking cast, posterior splint, or a hard plastic cast shoe with weightbearing as tolerated[26]. A study done by O’Malley et al[28] demonstrated that active individuals do well when treated nonoperatively. The study looked at 35 ballet dancers with distal shaft fractures treated nonoperatively and 31 of the patients returned to dance without limitations or pain[28].
Evidence based studies suggest that nondisplaced zone one fractures at the base of the fifth metatarsal are treated with protected weightbearing utilizing one of the many modalities varying from a short leg cast to elastic dressing and rigid shoe only as seen in Table 1[3,9,26,29-32]. The outcomes of nonoperative treatment for nondisplaced zone one fractures are good with low nonunion rates reported between 0.5% and 1%[33].
| Ref. | Treatment modality | Outcome |
| Shahid et al[29] | Airboot compared to below knee walking cast | Pain and function recovered quicker with airboot No difference in time to union between groups |
| Clapper et al[30] | Hard-soled shoe compared to below knee cast | No difference between clinical healing results |
| Gray et al[31] | Plastic slipper compared to tubi-grip support | Fractures treated with a plaster slipper resulted in significantly better pain and function at 2 wk At 6 and 12 wk the outcomes were similar for both treatment groups |
| Wiener et al[32] | Below knee casting compared to soft “Jones” dressings | The average time to union was 33 d vs 46 d respectively for soft dressings compared to rigid casting |
Acute zone two fractures are managed with nonweightbearing in a short leg cast for 6 to 8 wk. Torg type I diaphyseal stress fractures (zone three) are also managed the same however, prolonged immobilization up to twenty weeks may be required[3,10,13,31]. Despite prolonged immobilization zone three diaphyseal stress fractures may still go on to nonunion. Delayed unions of zone two and type II zone three fractures may eventually heal by nonoperative treatment but operative management is recommended in highly active patient populations[3,10,13,25]. Additionally, despite prolonged immobilization in zone three fractures it is not uncommon for a nonunion to occur[3].
There is a clear lack of randomized controlled trials comparing various nonoperative treatment modalities. As a result, the choice of nonoperative management should be based on the patient and the individual fracture type. A retrospective study done by Konkel et al[33], demonstrates the results obtained from nonoperative management of fifth metatarsal fractures. They found that the average time to bony union for tuberosity fractures, Jones, stress, segmental shaft, and oblique distal shaft/neck fractures was 3.7, 3.5, 4.8, 3.6 and 3.4 mo respectively. There was only one nonunion out of the 66 metatarsal fractures, which was a tuberosity fracture. There was delayed union in ten tuberosity fractures, two Jones fractures, two stress fractures and four oblique distal shaft/neck fractures. Overall they found that delayed union was seen in 27% of the patients with an overall union rate of 98.5%. The long-term satisfaction rate with nonoperative management was 100% in 40 patients with long-term follow-up[33].
One consideration is patients factors associated with less favourable outcomes. Female gender, diabetes mellitus and obesity are associated with adverse outcomes of metatarsal fractures[34]. One prospective cohort study showed that Torg type III fractures, displacement, and weight were significant independent predictors of poor outcomes at six weeks[35]. Additionally, this study showed that at 20 wk in addition to the above factors gender and diabetes were also significant independent predictors of poor outcome[35].
There are a variety of modalities for operative management of proximal fifth metatarsal fractures including percutaneous fixation with an intramedullary screw, corticocancellous bone graft, closed reduction and cross-pinning with Kirschner-wire (K-wire) fixation, or open reduction and internal fixation with minifragment plate and screws[3,4,9].
Zone one fractures that require operative fixation based on the indications specified in a previous section can be fixed using K-wires, tension band wiring, or small ASIF screws. If an avulsed fragment is too small for fixation excision may be required if chronic irritation results[3,4,19].
Percutaneous fixation with an intramedullary screw has become the preferred treatment choice for zone two and three fractures requiring operative fixation as specified in the indications for surgery section[3,15,19,24,25]. The advantage of this construct is that it is minimally invasive and compression across the fracture site can be obtained[1,36]. It also has been shown to have decreased healing time with accelerated mobilization[19,36]. DeLee et al[1] were the first to describe the use of percutaneous intramedullary screw fixation with a solid 4.5-mm malleolar screw for diaphyseal stress fractures in ten athletes. The study reported an average healing time of 7.5 wk and return to sport in an average of 8.5 wk with no postoperative complications or re-fractures[1,2,4]. It is important to note that this study was published prior to the introduction of the Torg et al[13] classification. Historically, the treatment of choice for symptomatic Torg type II and type III fractures as first described by Torg et al[13], in their study that introduced the Torg classification was cortico-cancellous bone graft. In this series 95% of patients treated with cortico-cancellous bone graft had healed radiographically and clinically at a mean of 12.3 wk[13]. Currently, the most accepted technique for nonunions is open curettage of the nonunion site followed by intramedullary screw placement[8].
Currently, there exists a variety of intramedullary screws a surgeon can select from for fixation of a proximal fifth metatarsal fracture. Solid and cannulated screws exist. The theoretical advantage of a cannulated screw is the precision and ease if screw placement over a guidewire[25,37]. However, a study done by Glasgow et al[38] reported the risk of re-fracture with cannulated screws. The study examined operative failure of three delayed unions, three nonunions, and five acute Jones fractures. A variety of intramedullary screws were used including: 4.0-mm cancellous, 4.5-mm malleolar, 4.5-mm cannulated screw, and a 6.5-mm cancellous screw. They concluded that intramedullary fixation with other than a 4.5-mm malleolar screw resulted in re-fracture and failure. In this same study two of the nonunions and all of the delayed unions treated with cortico-cancellous bone graft failed. They concluded failure was due to undersized cortico-cancellous grafts and incomplete reaming of the medullary canal. Additionally, early return to vigorous physical activity with the bone graft procedure and screw fixation was associated with re-fractures and delayed union[38]. It should be noted that that in this study the definition of Jones fracture included zone two and zone three fractures. On the contrary, a more recent study by Porter et al[21] described 100% union using a partially threaded cancellous 4.5 mm cannulated screw for fixation of acute zone two fractures in self-reported athletes with high satisfaction rates and no re-fractures[21].
Pietropaoli et al[37] compared the strength of 4.5-mm malleolar screws and 4.5-mm partially threaded cancellous cannulated screws in a simulated Jones fracture (zone two) cadaver model. The study reported no difference in the two screws from a biomechanical standpoint. They also found that the forces to cause displacement in both screws were much higher than the peak force experienced by the lateral aspect of the foot. Therefore, they concluded that early return to function after intramedullary screw fixation of these fractures should be considered[37].
Portland et al[25] demonstrated 100% union rate after immediate intramedullary fixation with 4.5-mm or 5.0-mm cannulated screws in acute Jones fractures (zone two) and Torg type I diaphyseal stress fractures, with an average time to union of 6.2 wk. Immediate intramedullary fixation of type II diaphyseal stress fractures resulted in 100% union and average time to union of 8.3 wk. They advocate for immediate intramedullary fixation of Jones fractures and acutely presenting Torg type I and II diaphyseal stress fractures[25].
A more recent study done by DeSandis et al[36] investigated screw sizing of zone two fractures using CT and radiographic analysis of fifth metatarsal morphology in 241 patients. The fifth metatarsal has a lateral curvature and a plantar bow and its shaft morphology is variable which makes choosing the correct screw challenging. They recommended using the largest diameter screw possible keeping in mind using a large diameter medullary screw in a narrow canal can result in diaphyseal fracture. The analysis found a range of canal widths between 2.2- and 5.9-mm and they concluded most canals can accommodate a 4.0- or 4.5-mm diameter screw. They recommend using AP radiographs for preoperative templating of screw diameter to ensure the screw is an adequate size for the patient. Screw length they concluded should be as short as possible with 16 mm of distal threads. Based on their imaging analysis screw length should rarely be larger than 50-mm and typically should be 40-mm or less to prevent fracture distraction that can result due to the natural plantar bow of the fifth metatarsal. Additionally, special attention should be paid to larger individuals which based on their analysis were found to have more bowing. In this population excessively long screws should be avoided to reduce the risk of medial cortex perforation which may lead to fracture distraction[36].
In some cases, tension band wiring may be favoured if there are small fragments that are not amenable to screw fixation[32]. Sarimo et al[39] treated 27 zone two fractures with tension band wiring with good results. Patients started weightbearing at three weeks and the mean time to union was 12.8 wk[36].
Postoperatively after fixation of proximal fifth metatarsal fractures the foot should be immobilized and kept nonweightbearing. The period of nonweightbearing is 1 to 2 wk with progressive weightbearing in a short-leg walking cast or aircast for four to six weeks[3,4,10,13,19,25]. A functional brace or foot orthoses may be worn if the patient is returning to strenuous competitive activity[19,26]. Following inlay cortico-cancellous bone grafting the patient should be immobilized and nonweightbearing for six weeks as specified by Torg et al[13].
The treatment of fifth metatarsal fractures is evolving and evidence-based medicine is directing care which can be nonoperative or operative. The choice of treatment varies by anatomical region, patient history and radiological findings. All nondisplaced fractures including stress fractures can be treated nonoperatively[3,9,10,19]. Fifth metatarsal neck and shaft fractures may be treated with a variety of nonoperative modalities and weightbearing as tolerated[19]. There is no definitive literature that describes the exact amount of translation and angulation that is acceptable for metatarsal neck and shaft fractures. The criteria cited is more than 10 degrees of plantar angulation or three to four millimeters of translation in any plane[19]. Displacement greater than this, should be corrected by open reduction if closed reduction fails[19]. The recommended treatment for nondisplaced zone one fractures is symptomatic care in a walking cast, air-boot, or compression wrap with protected weightbearing until discomfort subsides[3,19]. Based on the current literature, less rigid immobilization and shorter period of nonweightbearing can be associated with better early functional outcomes (Table 1). These fractures should be treated operatively if displaced more than three millimeters or if more than 30% of the cubometatarsal joint is involved. The treatment of zone two and zone three fractures is more complex because they are recognized for prolonged healing time and nonunion. Nonoperative treatment of zone two and zone three fractures includes immobilization and nonweightbearing for 6 to 8 wk or longer in the case of zone three stress fractures[3,9]. Torg type I diaphyseal stress fractures and acute zone two fractures are managed nonoperatively, however in the highly active population operative management should be considered due faster clinical healing and return to sport[3,4,21-24]. Zone two and zone three delayed unions may be managed operatively or nonoperatively[3,4]. Operative intervention is recommended in the active population[3]. Symptomatic zone two and zone three nonunions should be managed operatively[3,4].
Evidence based decisions are difficult in this anatomic area as there is a paucity of good randomized control trials comparing treatment options. In the studies that do exist zone two and zone three fractures are often confused. In addition to fracture classification inconsistencies there are also inconsistencies with respect to chronicity of fractures and differentiating between stress fractures and an acute traumatic mechanism[39]. Regardless, when making decisions on treatment, special attention should be paid to the athlete with operative and nonoperative approaches to treatment being outlined and the treatment modality should be based on the patient’s preference.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: Canada
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Erdil M, Vulcano E, Zheng N S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | DeLee JC, Evans JP, Julian J. Stress fracture of the fifth metatarsal. Am J Sports Med. 1983;11:349-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 255] [Cited by in RCA: 203] [Article Influence: 4.8] [Reference Citation Analysis (1)] |
| 2. | Petrisor BA, Ekrol I, Court-Brown C. The epidemiology of metatarsal fractures. Foot Ankle Int. 2006;27:172-174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 134] [Cited by in RCA: 114] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 3. | Lawrence SJ, Botte MJ. Jones’ fractures and related fractures of the proximal fifth metatarsal. Foot Ankle. 1993;14:358-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 294] [Cited by in RCA: 237] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 4. | Dameron TB. Fractures of the Proximal Fifth Metatarsal: Selecting the Best Treatment Option. J Am Acad Orthop Surg. 1995;3:110-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 129] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Dameron TB. Fractures and anatomical variations of the proximal portion of the fifth metatarsal. J Bone Joint Surg Am. 1975;57:788-792. [PubMed] |
| 6. | Thomas JL, Davis BC. Three-wire fixation technique for displaced fifth metatarsal base fractures. J Foot Ankle Surg. 2011;50:776-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Jones R. I. Fracture of the Base of the Fifth Metatarsal Bone by Indirect Violence. Ann Surg. 1902;35:697-700.2. [PubMed] |
| 8. | Armagan OE, Shereff MJ. Injuries to the toes and metatarsals. Orthop Clin North Am. 2001;32:1-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 9. | Rammelt S, Heineck J, Zwipp H. Metatarsal fractures. Injury. 2004;35 Suppl 2:SB77-SB86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 86] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 10. | Zwitser EW, Breederveld RS. Fractures of the fifth metatarsal; diagnosis and treatment. Injury. 2010;41:555-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 92] [Article Influence: 6.1] [Reference Citation Analysis (1)] |
| 11. | Stewart IM. Jones’s fracture: fracture of base of fifth metatarsal. Clin Orthop. 1960;16:190-198. [PubMed] |
| 12. | Smith JW, Arnoczky SP, Hersh A. The intraosseous blood supply of the fifth metatarsal: implications for proximal fracture healing. Foot Ankle. 1992;13:143-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 161] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 13. | Torg JS, Balduini FC, Zelko RR, Pavlov H, Peff TC, Das M. Fractures of the base of the fifth metatarsal distal to the tuberosity. Classification and guidelines for non-surgical and surgical management. J Bone Joint Surg Am. 1984;66:209-214. [PubMed] |
| 14. | Dean BJ, Kothari A, Uppal H, Kankate R. The jones fracture classification, management, outcome, and complications: a systematic review. Foot Ankle Spec. 2012;5:256-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 15. | Roche AJ, Calder JD. Treatment and return to sport following a Jones fracture of the fifth metatarsal: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2013;21:1307-1315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 92] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 16. | Lehman RC, Torg JS, Pavlov H, DeLee JC. Fractures of the base of the fifth metatarsal distal to the tuberosity: a review. Foot Ankle. 1987;7:245-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 76] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Zwipp H, Ranft T. [Malunited juvenile fractures in the foot region]. Orthopade. 1991;20:374-380. [PubMed] |
| 18. | Mehlhorn AT, Zwingmann J, Hirschmüller A, Südkamp NP, Schmal H. Radiographic classification for fractures of the fifth metatarsal base. Skeletal Radiol. 2014;43:467-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 19. | Fetzer GB, Wright RW. Metatarsal shaft fractures and fractures of the proximal fifth metatarsal. Clin Sports Med. 2006;25:139-150, x. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 47] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 20. | Chuckpaiwong B, Queen RM, Easley ME, Nunley JA. Distinguishing Jones and proximal diaphyseal fractures of the fifth metatarsal. Clin Orthop Relat Res. 2008;466:1966-1970. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 119] [Cited by in RCA: 102] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 21. | Porter DA, Duncan M, Meyer SJ. Fifth metatarsal Jones fracture fixation with a 4.5-mm cannulated stainless steel screw in the competitive and recreational athlete: a clinical and radiographic evaluation. Am J Sports Med. 2005;33:726-733. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 130] [Cited by in RCA: 103] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 22. | Mindrebo N, Shelbourne KD, Van Meter CD, Rettig AC. Outpatient percutaneous screw fixation of the acute Jones fracture. Am J Sports Med. 1993;21:720-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 68] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 23. | Quill GE. Fractures of the proximal fifth metatarsal. Orthop Clin North Am. 1995;26:353-361. [PubMed] |
| 24. | Mologne TS, Lundeen JM, Clapper MF, O’Brien TJ. Early screw fixation versus casting in the treatment of acute Jones fractures. Am J Sports Med. 2005;33:970-975. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 136] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 25. | Portland G, Kelikian A, Kodros S. Acute surgical management of Jones’ fractures. Foot Ankle Int. 2003;24:829-833. [PubMed] |
| 26. | Raikin SM, Slenker N, Ratigan B. The association of a varus hindfoot and fracture of the fifth metatarsal metaphyseal-diaphyseal junction: the Jones fracture. Am J Sports Med. 2008;36:1367-1372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 97] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 27. | Aynardi M, Pedowitz DI, Saffel H, Piper C, Raikin SM. Outcome of nonoperative management of displaced oblique spiral fractures of the fifth metatarsal shaft. Foot Ankle Int. 2013;34:1619-1623. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 28. | O’Malley MJ, Hamilton WG, Munyak J. Fractures of the distal shaft of the fifth metatarsal. “Dancer’s fracture”. Am J Sports Med. 1996;24:240-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 43] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 29. | Shahid MK, Punwar S, Boulind C, Bannister G. Aircast walking boot and below-knee walking cast for avulsion fractures of the base of the fifth metatarsal: a comparative cohort study. Foot Ankle Int. 2013;34:75-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 47] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 30. | Clapper MF, O’Brien TJ, Lyons PM. Fractures of the fifth metatarsal. Analysis of a fracture registry. Clin Orthop Relat Res. 1995;238-241. [PubMed] |
| 31. | Gray AC, Rooney BP, Ingram R. A prospective comparison of two treatment options for tuberosity fractures of the proximal fifth metatarsal. Foot (Edinb). 2008;18:156-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 32. | Wiener BD, Linder JF, Giattini JF. Treatment of fractures of the fifth metatarsal: a prospective study. Foot Ankle Int. 1997;18:267-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 85] [Article Influence: 3.0] [Reference Citation Analysis (1)] |
| 33. | Konkel KF, Menger AG, Retzlaff SA. Nonoperative treatment of fifth metatarsal fractures in an orthopaedic suburban private multispeciality practice. Foot Ankle Int. 2005;26:704-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 47] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 34. | Cakir H, Van Vliet-Koppert ST, Van Lieshout EM, De Vries MR, Van Der Elst M, Schepers T. Demographics and outcome of metatarsal fractures. Arch Orthop Trauma Surg. 2011;131:241-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 70] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 35. | Tahririan MA, Momeni A, Moayednia A, Yousefi E. Designing a prognostic scoring system for predicting the outcomes of proximal fifth metatarsal fractures at 20 weeks. Iran J Med Sci. 2015;40:104-109. [PubMed] |
| 36. | DeSandis B, Murphy C, Rosenbaum A, Levitsky M, O’Malley Q, Konin G, Drakos M. Multiplanar CT Analysis of Fifth Metatarsal Morphology: Implications for Operative Management of Zone II Fractures. Foot Ankle Int. 2016;37:528-536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 37. | Pietropaoli MP, Wnorowski DC, Werner FW, Fortino MD. Intramedullary screw fixation of Jones fractures: a biomechanical study. Foot Ankle Int. 1999;20:560-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 65] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 38. | Glasgow MT, Naranja RJ, Glasgow SG, Torg JS. Analysis of failed surgical management of fractures of the base of the fifth metatarsal distal to the tuberosity: the Jones fracture. Foot Ankle Int. 1996;17:449-457. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 113] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 39. | Sarimo J, Rantanen J, Orava S, Alanen J. Tension-band wiring for fractures of the fifth metatarsal located in the junction of the proximal metaphysis and diaphysis. Am J Sports Med. 2006;34:476-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 60] [Article Influence: 3.2] [Reference Citation Analysis (0)] |