Published online Oct 18, 2016. doi: 10.5312/wjo.v7.i10.687
Peer-review started: May 27, 2016
First decision: July 6, 2016
Revised: July 27, 2016
Accepted: August 6, 2016
Article in press: August 8, 2016
Published online: October 18, 2016
Processing time: 138 Days and 22.5 Hours
To compare the outcomes of displaced distal radius fractures treated with volar locking plates and with immediate postoperative mobilisation with the outcomes of these fractures treated with modalities that necessitate 6 wk wrist immobilisation.
A prospective, randomised controlled single-centre trial was conducted with 56 patients who had a displaced radius fracture were randomised to treatment either with a volar locking plate (n = 29), or another treatment modality (n = 27; cast immobilisation with or without wires or external fixator). Outcomes were measured at 12 wk. Functional outcome scores measured were the Patient-Rated Wrist Evaluation (PRWE) Score; Disabilities of the Arm, Shoulder and Hand and activities of daily living (ADLs). Clinical outcomes were wrist range of motion and grip strength. Radiographic parameters were volar inclination and ulnar variance.
Patients in the volar locking plate group had significantly better PRWE scores, ADL scores, grip strength and range of extension at three months compared with the control group. All radiological parameters were significantly better in the volar locking plate group at 3 mo.
The present study suggests that volar locking plates produced significantly better functional and clinical outcomes at 3 mo compared with other treatment modalities. Anatomical reduction was significantly more likely to be preserved in the plating group. Level of evidence: II.
Core tip: The present study suggests that the treatment of distal radius fractures with volar locking distal radius plates and immediate postoperative mobilisation produces better functional, radiological and clinical outcomes at three months compared with other treatment modalities which necessitate six weeks immobilisation post fracture. Short term outcomes are very important in our view, as early mobility potentially means earlier return to activities of daily life and return to work for younger patients and remaining functionally independent for the elderly. Future studies should focus on cost savings gained by earlier return to activities of daily living.
- Citation: Drobetz H, Koval L, Weninger P, Luscombe R, Jeffries P, Ehrendorfer S, Heal C. Volar locking distal radius plates show better short-term results than other treatment options: A prospective randomised controlled trial. World J Orthop 2016; 7(10): 687-694
- URL: https://www.wjgnet.com/2218-5836/full/v7/i10/687.htm
- DOI: https://dx.doi.org/10.5312/wjo.v7.i10.687
Distal radius fractures are the most common type of fracture of the human skeleton, with about ten percent of the population sustaining a fracture at some point in their life[1-3]. Despite the lack of clear evidence, the treatment of distal radius fractures with volar locking distal radius plates (VLDRPs) has become increasingly popular in the last decade[4-8]. The driving force behind the development of VLDRPs was dissatisfaction with the results of conventional treatment modalities. Volar locking plates are expensive[9-11], but they are the only modality that allows distal radius fracture treatment without postoperative immobilisation. All other treatments necessitate between four and eight weeks of wrist immobilisation. Several studies show that these theoretical advantages of VLDRP seem to be equalized after twelve to 24 mo[12-22]. The data on short-term benefits are still unclear, because patients treated with VLDRP still often have their wrists immobilised postoperatively, rather than being allowed to use as tolerated[12-22]. There are only a few studies that specifically allow immediate postoperative mobilisation[23,24], however they did not report on short-term outcomes. The aim of our study was to evaluate short-term results of distal radius fracture treatment with VLDRP and with immediate postoperative wrist mobilisation as tolerated compared to treatment modalities with six weeks immobilisation (closed reduction and casting; Kirschner (K-) wires and casting; external fixation).
We carried out a randomised controlled single-centre trial involving patients presenting with distal radial fractures. The study was approved by the Queensland Health ethics committee (approval No. EC00407) and was registered with Clinical Trials.gov (NCT00809861; DCDRS00407).
The study was conducted at a regional general hospital in Mackay, Queensland, Australia, between June 2009 and December 2013.
The study participants were recruited by two of the study authors (Herwig Drobetz and Lidia Koval). Consecutive patients presenting with distal radial fractures were invited to take part in the trial. The principle researcher was responsible for collecting data. Demographic information was collected for all patients, as well as clinical information regarding presence of osteoporosis, diabetes, or any other predetermined significant medical conditions. Fracture type was recorded. At the end of the recruitment period the principle and associate investigators re-examined hospital records to fill in any missing data.
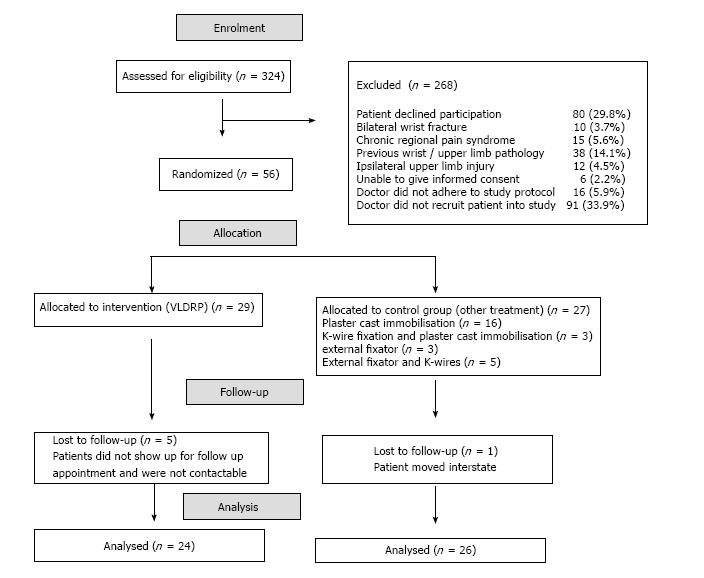
All patients over the age of 18 years presenting to the Emergency Department or Fracture clinic with a distal radial fracture were eligible to participate in the study. Patients who had bilateral wrist fractures, compound fractures, a concurrent ipsilateral upper limb injury, a past history of chronic pain syndrome or history of pathology of ipsilateral extremity (including ipsilateral wrist) or who were unable to give informed consent were excluded from the study. Patients were also not included if the treating doctors concluded that they could not adhere to the study protocol (Figure 1).
All operations were performed by three consultant surgeons (including the principal investigator) at the Mackay Base Hospital Department of Orthopaedic surgery. The following technique was used.
Intervention (VLDRP): The fracture was approached using a volar Henry approach, reduced under fluoroscopic guidance and stabilised with a volar locking distal radius plate. All plates used were Synthes® (Synthes GmbH, Solothurn, Switzerland) VLDRPs, although different models (fixed and variable locking plates with either single or multiple distal screw holes). No bone graft or other void fillers were used. Postoperatively, patients were allowed to immediately use their wrist as tolerated without splinting or any other form of immobilisation. Patients were usually discharged from the hospital the day after the operation and were referred to a physiotherapist. The patients were seen at 2, 6 and 12 wk postoperatively.
Control group (non-operative, K-wire fixation and external fixator): The patients in the control group received either: Closed reduction and casting (n = 16); closed reduction, K-wire fixation and casting (n = 3); or closed reduction and external fixation with (n = 5) or without (n = 3) additional K-wires (Figure 1). The same cohort of surgeons who performed the operations in the intervention group also treated the patients in the control group and were free to choose the control group treatment modality. All patients in the control group had their wrist immobilised for six weeks. K-wires and/or external fixators were removed at six weeks. The patients were seen weekly for cast checks/changes or pin checks. Patients were referred for physiotherapy after removal of the cast or external fixator. All patients were then seen again at 12 wk.
All patients gave written informed consent before enrolling in the study. After agreeing to participate, patients were randomised using computer generated random numbers and opaque sealed envelopes. The principle investigator enrolled patients and assigned participants to their groups. All participating patients received written instructions on post-operative care.
Follow up was conducted at 12 wk and comprised patient reported (functional), clinical and radiological outcomes. Only the principle investigator performed the assessments.
Functional assessment: Two self-administered standard questionnaires were given to the study participants [Disabilities of the Arm Shoulder and Hand (DASH) Outcome Measure[25] and Patient Rated Wrist Evaluation (PRWE)][26] to measure disability at the three-month visit. Patients were assessed for their ability to perform activities of daily life (ADL) by being asked if they had resumed driving, and if employed if they had resumed working. They were further asked to grade their ability to perform ADLs into five categories (Group 1 = 100%; Group 2 = 75%-100%; Group 3 = 50%-75%; Group 4 = 25%- 50%; Group 5 = 0%-25%). Not being able to drive or work at the 3 mo mark immediately precluded patients from classification into group 1 or 2. The measurement of ADLs was considered to be a secondary outcome measurement.
Clinical assessment: The range of movement of the wrist was assessed with use of a standard goniometer. Wrist strength was measured with use of a dynamometer (Jamar Hydraulic Hand Dynamometer; Lafayette Instrument®, Lafayette, IN, United States). All clinical assessments were performed by the principle investigator (Herwig Drobetz) to reduce inter-observer variability.
Radiological assessment: Radiographs of the wrist taken pre-operatively, post reduction/postoperatively and at three months were assessed for study purposes. Volar tilt of the distal radius joint surface and anterior-posterior radial inclination were measured in degrees and ulnar variance as an indicator of radius shortening was measured in millimetres. Negative values for volar tilt represent dorsal tilt, and negative values for ulnar variance represent an ulna that is shorter than the radius. All radiological measurements were made by an independent assessor (Paula Jeffries) and validated by a radiologist. It was pre-determined that any inter-observer discrepancy of > 15% would trigger another review.
Sample size was calculated on the basis of the validated DASH scale, in which a 20-point difference is considered to be clinically significant. Group sample sizes of 21 and 21 achieve 82% power to detect a difference of 20.0 between the null hypothesis assuming that both group means are 40.0 and the alternative hypothesis that the mean of group 2 is 20.0 with estimated group standard deviations of 20.0 and 20.0 and with a significance level (alpha) of 0.025 using a two-sided two-sample t-test. Therefore 21 patients were required in the intervention and control groups. The sample size was set to a total of 46 patients to allow for drop out. The sample size calculation was based on the clinically significant difference for DASH in 2008 being considered to be 20.
All analysis was based on the intention-to-treat principal. Depending on the distribution, numerical data was described as mean value and SD or median value and inter-quartile range (IQR). Comparisons between intervention and control groups were conducted using bivariate statistical tests of the statistical programme SPSS (SPSS for Windows, version 22, SPSS Inc., Chicago, IL, United States). P-values less than 0.05 were considered to be statistically significant.
Of the total of 324 patients who presented with distal radial fractures during the study period from November 2009 to December 2013, 268 patients were excluded. Of the remaining 56 patients, 29 patients were randomised to the intervention (VLDRP) group, and 27 to the control (other treatments) group. A total of six patients were eventually lost to follow up because they failed to return for the 3-mo review. Follow up was completed in 50/56 (89%) randomised patients (Figure 1). Patients who completed the trial did not differ demographically, clinically or in terms of fracture severity from the group who were eligible for recruitment.
There were no significant differences between the intervention and the control groups at baseline (Table 1). Fracture types were comparable between groups.
| Intervention group n = 24 | Control group n = 26 | |
| Patient characteristics | ||
| Mean age (SD) | 51.1 (16.0) | 52.5 (16.5) |
| Gender F (M) | 15 (9) | 13 (13) |
| % Osteoporosis | 43 | 47 |
| % Diabetes mellitus | 5 | 4 |
| % With medical condition1 | 25 | 29 |
| Dominant hand | 9 | 12 |
| Fracture classification | ||
| A2 | 0 | 2 |
| A3 | 4 | 7 |
| B2 | 3 | 3 |
| C1 | 7 | 6 |
| C2 | 8 | 7 |
| C3 | 2 | 1 |
The PRWE scores were significantly better in the VLDRP group than the control group at three months. The mean score in the VLDRP group was 21 compared to a mean score of 47 in the control group. This is also clinically significant as the minimum clinically important difference (MCID) is between 11 and 14 for the PRWE score[27,28]. ADLs were significantly better at three months in the VLDRP group. Twenty patients were able to drive or work at 3 mo (group 1 or 2) in the VLDRP group compared with 15 patients in the control group (Table 2). The DASH scores were also better but this did not reach statistical significance. Wrist extension was significantly better in the VLDRP group as well as grip strength.
| VLDRP groupn = 24 | Control groupn = 26 | P-value | |
| DASH (points) | 40 (12) | 50 (24) | 0.063 |
| PRWE (points) | 21 (20) | 47 (40) | 0.0071 |
| Grip strength (% of grip strength of uninjured limb) | |||
| 64 (29) | 42 (32) | 0.0121 | |
| Range of motion (in degrees) | |||
| Flexion | 60 (21) | 49 (22) | 0.072 |
| Extension | 65 (48) | 48 (27) | 0.0211 |
| Pronation | 70 (31) | 68 (26) | 0.805 |
| Supination | 82 (25) | 79 (24) | 0.677 |
| ADLs | |||
| Grade 1 | 19 | 10 | 0.0361 |
| Grade 2 | 1 | 5 | |
| Grade 3 | 4 | 7 | |
| Grade 4 | 0 | 2 | |
| Grade 5 | 0 | 2 |
At 3 mo, all radiological parameters were significantly better in the VLDRP group than in the control group (Table 3).
| VLDRP group n = 24 | Control groupn = 26 | P-value | |
| Injured wrist at presentation | |||
| Volar slope (degrees) | -17.2 (17.2) | -13.4(14.4) | 0.241 |
| Radial inclination (degrees) | 8.7 (7.6) | 14.2 (9.4) | 0.021 |
| Ulnar variance (mm) | 2.5 (2.2) | 2.3 (3.3) | 0.285 |
| Injured wrist post-reduction | |||
| Volar slope (degrees) | 4.7 (5.4) | 0.08(7.25) | 0.011 |
| Radial inclination (degrees) | 19.6 (4.5) | 18.69(4.52) | 0.45 |
| Ulnar variance (mm) | 0.1 (0.6) | 0.4 (1.4) | 0.146 |
| Injured wrist 3 mo | |||
| Volar slope (degrees) | 3.5 (4.6) | -5.4 (11.6) | 0.0011 |
| Radial inclination (degrees) | 19.3 (4.4) | 15.37 (7.0) | 0.0541 |
| Ulnar variance (mm) | 0.9 (1.3) | 2.1 (1.9) | 0.0111 |
In the VLDRP group we observed five complications in five patients at the three month follow up visit: Flexor tendon rupture, n = 1 (patient refused tendon reconstruction); carpal tunnel syndrome, n = 1 (patient underwent nerve release after 6 mo); Chronic Regional Pain Syndrome (CRPS), n = 1. Two patients did not like “having a plate inside my body” and the plates were subsequently removed 4 mo postoperatively. There were no intra-operative or immediate postoperative complications.
In the control group we observed seven complications in seven patients: Malunion, n = 2 (1 of which subsequently had a corrective osteotomy due to functional deficits); CRPS, n = 2; infected K-wires which had to be removed early, n = 3.
The results of our study suggest that clinical and radiological outcomes are superior in the VLDRP group when compared to treatment modalities that necessitate six weeks of wrist immobilisation at the 3-mo mark.
Currently there are no clear evidence based guidelines for the best treatment of distal radius fractures[28]. There have been many encouraging results with the use of VLDRPs[29-34] but other authors reported similar favourable results with other treatment modalities[13,16,21,22,35].
As mentioned in the introduction, many studies show that after one to two years the results of all treatment modalities are similar and there are no longer any significant differences. This fact is often used as an argument against the use of VLDRPs. We do not agree, as the short-term outcomes of treatments are important for patient quality of life and morbidity. Getting back to work 6 wk earlier or, for elderly patients, staying independent can make a significant difference. This might also have an economical impact, as the Medicare savings with earlier return to ADLs can potentially offset the costs for the more expensive treatment with VLDRPs.
Furthermore, it holds true for almost every fracture we treat that long-term outcomes are similar regardless of the treatment, but short-term outcomes are favourable for the more invasive treatment modalities. Tibial shaft fractures treated with intramedullary nails show excellent functional short-term results. After 12 to 24 mo, however, the results are not significantly different from treatment of these fractures with cast immobilisation or an external fixator, both of which are significantly cheaper options[36]. However, due to increased patient demands, the ability to mobilise early and the fact that the overall short-term benefits are significantly greater, intramedullary nailing of tibial shaft fractures has become the gold-standard treatment.
There are several limitations to our study. Various factors influence the outcomes of distal radius fractures and although information on as many variables as possible was recorded, it proved difficult to ensure that baseline data was comparable. For example, the prevalence of osteopenia or osteoporosis was not verified by a computer tomography or bone densitometry but we used information from the patient’s history or GP. Surgical training and technique of the surgeons involved is a potential confounder, which would be difficult to quantify and was not recorded. The study was not blinded, as the nature of surgical procedures, and related postoperative care cannot realistically be masked to patients and staff, and resulting scars preclude the blinding of a blinded independent outcome assessor.
DASH and PRWE, although validated questionnaires, are still subjective scores and especially the DASH has a lower specificity in reporting wrist problems[37,38]. The clinical measurements may be subject to inter and intra-observer variation, although one clinician completed all measurements to reduce inter-observer error. Radiological measurements may also be subject to intra and inter-observer error. Two observers including a radiologist checked all radiographs to reduce errors.
We asked the study participants to subjectively rate their ability to perform specific ADLs with their injured wrist, compare them to their uninjured wrist and then quantify them. We are aware that this is not a validated score but to our knowledge there is no validated wrist specific ADL score available yet[39]. The number of patients reporting full return to ADLs after twelve weeks in the VLDRP was, however, significantly higher than in the control group.
Another limitation is that the study had three different treatment types in the control arm. However, we felt it was unethical to use a single treatment modality as the control group for the purposes of the study, and we feel that this heterogeneous control group represents the “real-life” situation. Our main outcome measure was to see the effect of six weeks immobilization vs immediate mobilization.
There are some important strengths of this study. To our knowledge this is the first study that looked at immediate mobilisation vs immobilisation for the treatment of distal radius fractures. The study showed that distal radius fractures treated with VLDRP can be treated with immediate postoperative mobilisation without secondary loss of reduction. In a setting like Northern Queensland, where many patients live up to 600 km away from the hospital this constitutes an important factor as the number of follow up visits can potentially be significantly reduced. Treatment with plaster cast or external fixator necessitates more follow up visits and is generally more involved. While recent European studies[10,11] show significant cost savings with the use of K-wires over volar locking plates, this might be different in a regional Australian setting.
In conclusion, the evidence for using VLDRPs for the treatment of distal radius fractures is still a matter of debate and in addition to efficacy; costs and adverse effects should be taken into account. However, our study showed that in the short-term, the functional, clinical and radiological outcomes were superior in the VLDRP group in comparison to other treatment methods. We strongly believe we should concentrate on the early outcomes of distal radius fracture treatment with VLDRPs and not resign ourselves to the fact that “after time, they are all the same”. Therefore, the results of this study could encourage the judicial use of VLDRPs for the treatment of distal radius fractures. Future studies should focus on cost savings gained by earlier return to ADLs.
Despite the lack of clear evidence, the treatment of distal radius fractures with volar locking distal radius plates (VLDRPs) has become increasingly popular in the last decade VLDRPs are the only treatment which allows distal radius fracture fixation without the need for postoperative immobilisation. Several studies show that advantages of VLDRP seem to be equalized after 12 to 24 mo, but there are little data available on short-term benefits of VLDRPs when combined with early mobilisation.
The treatment of distal radius fractures with VLDRPs has been an area of increased research interest in the last ten years. Recently, many authors have focused on the fact that outcomes when compared with non-operative treatment are similar after 12 to 24 mo. There have also been recent publications showing that volar plating is significantly more expensive when compared to other treatment modalities. There are, however only very limited data on return to work and function in the short term. Earlier return of function and ability to work, which is potentially possible with volar locking plates could mean significant overall cost savings when compared to other treatment options which necessitate 6 wk of immobilisation.
The study showed that VDRLP produced significantly better functional and clinical outcomes at 3 mo compared with other treatment modalities. The study also showed that VLDRP patients can perform activities of daily life significantly earlier than patients who need 6 wk of wrist immobilisation. The study is the only study to the knowledge which allowed immediate postoperative wrist mobilisation after plating with VLDRPs. This allows accurate determination of early functional results, which in our opinion are crucial. All other studies the authors looked at immobilised the wrist for 2 to 4 wk postoperatively.
Short term benefits are very important, as they translate into the ability for patients to return to work earlier, improve patient quality of life and might have overall cost savings when patients can return to work potentially 6 wk earlier than patients treated with casts or external fixators.
VLDRPs have been in clinical use since 1997. The difference to traditional plates is that the screws are connected to the plate in an angle stable fashion, mostly by a thread in the plate hole and in the screw head. This effectively creates a rake like construct. The stiffness of the construct and its ability to withstand deforming forces are therefore not dependant of the bone quality anymore, as opposed to traditional plates, which need friction between bone and plate to create sufficient construct stiffness. This allows treatment of fractures from the “biomechanically wrong” volar side of the wrist - easier approach and better soft tissue coverage of the implants. It also allows immediate postoperative mobilisation of the wrist, a unique feature of VLDRPs.
It is a random controlled study involving patients presenting with distal radial fractures. Based on better functional, clinical and radiological outcomes at short-term follow-up, the authors encourage the use of volar locking plates for the treatment of distal radius fractures. The study is well designed and the data is reliable.
Manuscript source: Invited manuscript
Specialty type: Orthopedics
Country of origin: Australia
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Ma DY, von Heideken J S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Graff S, Jupiter J. Fracture of the distal radius: classification of treatment and indications for external fixation. Injury. 1994;25 Suppl 4:S-D14-S-D25. [PubMed] |
| 2. | Jupiter JB. Fractures of the distal end of the radius. J Bone Joint Surg Am. 1991;73:461-469. [PubMed] |
| 3. | Tscherne H, Jähne J. [Current status of the treatment of distal radius fracture]. Unfallchirurg. 1990;93:157-164. [PubMed] |
| 4. | Chung KC, Shauver MJ, Birkmeyer JD. Trends in the United States in the treatment of distal radial fractures in the elderly. J Bone Joint Surg Am. 2009;91:1868-1873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 306] [Cited by in RCA: 349] [Article Influence: 21.8] [Reference Citation Analysis (0)] |
| 5. | Mattila VM, Huttunen TT, Sillanpää P, Niemi S, Pihlajamäki H, Kannus P. Significant change in the surgical treatment of distal radius fractures: a nationwide study between 1998 and 2008 in Finland. J Trauma. 2011;71:939-942; discussion 942-943. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 99] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 6. | Chen NC, Jupiter JB. Management of distal radial fractures. J Bone Joint Surg Am. 2007;89:2051-2062. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 96] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 7. | Tarallo L, Mugnai R, Zambianchi F, Adani R, Catani F. Volar plate fixation for the treatment of distal radius fractures: analysis of adverse events. J Orthop Trauma. 2013;27:740-745. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 56] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Mellstrand-Navarro C, Pettersson HJ, Tornqvist H, Ponzer S. The operative treatment of fractures of the distal radius is increasing: results from a nationwide Swedish study. Bone Joint J. 2014;96-B:963-969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 166] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 9. | Dzaja I, MacDermid JC, Roth J, Grewal R. Functional outcomes and cost estimation for extra-articular and simple intra-articular distal radius fractures treated with open reduction and internal fixation versus closed reduction and percutaneous Kirschner wire fixation. Can J Surg. 2013;56:378-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Karantana A, Scammell BE, Davis TR, Whynes DK. Cost-effectiveness of volar locking plate versus percutaneous fixation for distal radial fractures: Economic evaluation alongside a randomised clinical trial. Bone Joint J. 2015;97-B:1264-1270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Tubeuf S, Yu G, Achten J, Parsons NR, Rangan A, Lamb SE, Costa ML. Cost effectiveness of treatment with percutaneous Kirschner wires versus volar locking plate for adult patients with a dorsally displaced fracture of the distal radius: analysis from the DRAFFT trial. Bone Joint J. 2015;97-B:1082-1089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 12. | Wilcke MK, Abbaszadegan H, Adolphson PY. Wrist function recovers more rapidly after volar locked plating than after external fixation but the outcomes are similar after 1 year. Acta Orthop. 2011;82:76-81. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 83] [Cited by in RCA: 83] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 13. | Wei DH, Raizman NM, Bottino CJ, Jobin CM, Strauch RJ, Rosenwasser MP. Unstable distal radial fractures treated with external fixation, a radial column plate, or a volar plate. A prospective randomized trial. J Bone Joint Surg Am. 2009;91:1568-1577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 135] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 14. | Egol K, Walsh M, Tejwani N, McLaurin T, Wynn C, Paksima N. Bridging external fixation and supplementary Kirschner-wire fixation versus volar locked plating for unstable fractures of the distal radius: a randomised, prospective trial. J Bone Joint Surg Br. 2008;90:1214-1221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 120] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 15. | Wright TW, Horodyski M, Smith DW. Functional outcome of unstable distal radius fractures: ORIF with a volar fixed-angle tine plate versus external fixation. J Hand Surg Am. 2005;30:289-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 170] [Cited by in RCA: 144] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 16. | Rozental TD, Blazar PE, Franko OI, Chacko AT, Earp BE, Day CS. Functional outcomes for unstable distal radial fractures treated with open reduction and internal fixation or closed reduction and percutaneous fixation. A prospective randomized trial. J Bone Joint Surg Am. 2009;91:1837-1846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 198] [Cited by in RCA: 202] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 17. | Koshimune M, Kamano M, Takamatsu K, Ohashi H. A randomized comparison of locking and non-locking palmar plating for unstable Colles’ fractures in the elderly. J Hand Surg Br. 2005;30:499-503. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Chung KC, Squitieri L, Kim HM. Comparative outcomes study using the volar locking plating system for distal radius fractures in both young adults and adults older than 60 years. J Hand Surg Am. 2008;33:809-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 75] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 19. | Chung KC, Watt AJ, Kotsis SV, Margaliot Z, Haase SC, Kim HM. Treatment of unstable distal radial fractures with the volar locking plating system. J Bone Joint Surg Am. 2006;88:2687-2694. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 159] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 20. | Karantana A, Davis TR. Extra-articular fractures of the distal radius--a European view point. Hand Clin. 2012;28:145-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Costa ML, Achten J, Parsons NR, Rangan A, Griffin D, Tubeuf S, Lamb SE. Percutaneous fixation with Kirschner wires versus volar locking plate fixation in adults with dorsally displaced fracture of distal radius: randomised controlled trial. BMJ. 2014;349:g4807. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 133] [Cited by in RCA: 148] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 22. | Karantana A, Downing ND, Forward DP, Hatton M, Taylor AM, Scammell BE, Moran CG, Davis TR. Surgical treatment of distal radial fractures with a volar locking plate versus conventional percutaneous methods: a randomized controlled trial. J Bone Joint Surg Am. 2013;95:1737-1744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 116] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 23. | Shetty MS, Kumar MA, Kiran K, Kini AR. Locking distal radius plate--early results from India. J Trauma. 2011;71:1359-1363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Osada D, Kamei S, Masuzaki K, Takai M, Kameda M, Tamai K. Prospective study of distal radius fractures treated with a volar locking plate system. J Hand Surg Am. 2008;33:691-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 84] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 25. | Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29:602-608. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 26. | MacDermid JC, Turgeon T, Richards RS, Beadle M, Roth JH. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12:577-586. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 561] [Cited by in RCA: 656] [Article Influence: 24.3] [Reference Citation Analysis (0)] |
| 27. | Walenkamp MM, de Muinck Keizer RJ, Goslings JC, Vos LM, Rosenwasser MP, Schep NW. The Minimum Clinically Important Difference of the Patient-rated Wrist Evaluation Score for Patients With Distal Radius Fractures. Clin Orthop Relat Res. 2015;473:3235-3241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 132] [Cited by in RCA: 148] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 28. | Sorensen AA, Howard D, Tan WH, Ketchersid J, Calfee RP. Minimal clinically important differences of 3 patient-rated outcomes instruments. J Hand Surg Am. 2013;38:641-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 317] [Cited by in RCA: 349] [Article Influence: 29.1] [Reference Citation Analysis (0)] |
| 29. | Lichtman DM, Bindra RR, Boyer MI, Putnam MD, Ring D, Slutsky DJ, Taras JS, Watters WC, Goldberg MJ, Keith M. Treatment of distal radius fractures. J Am Acad Orthop Surg. 2010;18:180-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 198] [Article Influence: 13.2] [Reference Citation Analysis (1)] |
| 30. | Matschke S, Marent-Huber M, Audigé L, Wentzensen A. The surgical treatment of unstable distal radius fractures by angle stable implants: a multicenter prospective study. J Orthop Trauma. 2011;25:312-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 31. | Lattmann T, Meier C, Dietrich M, Forberger J, Platz A. Results of volar locking plate osteosynthesis for distal radial fractures. J Trauma. 2011;70:1510-1518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 32. | Jupiter JB, Marent-Huber M. Operative management of distal radial fractures with 2.4-millimeter locking plates. A multicenter prospective case series. J Bone Joint Surg Am. 2009;91:55-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 119] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 33. | Arora R, Lutz M, Fritz D, Zimmermann R, Oberladstätter J, Gabl M. Palmar locking plate for treatment of unstable dorsal dislocated distal radius fractures. Arch Orthop Trauma Surg. 2005;125:399-404. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 59] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 34. | Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg Am. 2004;29:96-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 359] [Cited by in RCA: 310] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 35. | Hull P, Baraza N, Gohil M, Whalley H, Mauffrey C, Brewster M, Costa ML. Volar locking plates versus K-wire fixation of dorsally displaced distal radius fractures--a functional outcome study. J Trauma. 2011;70:E125-E128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 36. | Sarmiento A. A functional below-the-knee brace for tibial fractures: a report on its use in one hundred and thirty-five cases. 1970. J Bone Joint Surg Am. 2007;89 Suppl 2 Pt.2:157-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 37. | Changulani M, Okonkwo U, Keswani T, Kalairajah Y. Outcome evaluation measures for wrist and hand: which one to choose? Int Orthop. 2008;32:1-6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 197] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 38. | Mellstrand Navarro C, Ponzer S, Törnkvist H, Ahrengart L, Bergström G. Measuring outcome after wrist injury: translation and validation of the Swedish version of the patient-rated wrist evaluation (PRWE-Swe). BMC Musculoskelet Disord. 2011;12:171. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 39. | Goldhahn J, Beaton D, Ladd A, Macdermid J, Hoang-Kim A. Recommendation for measuring clinical outcome in distal radius fractures: a core set of domains for standardized reporting in clinical practice and research. Arch Orthop Trauma Surg. 2014;134:197-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 76] [Article Influence: 6.9] [Reference Citation Analysis (0)] |