Published online Sep 18, 2015. doi: 10.5312/wjo.v6.i8.649
Peer-review started: February 26, 2015
First decision: May 13, 2015
Revised: June 16, 2015
Accepted: July 29, 2015
Article in press: August 3, 2015
Published online: September 18, 2015
Processing time: 205 Days and 8.6 Hours
AIM: To investigate the known incidences, treatment options, and related outcomes of periprosthetic tibia fractures after total knee arthroplasty (TKA).
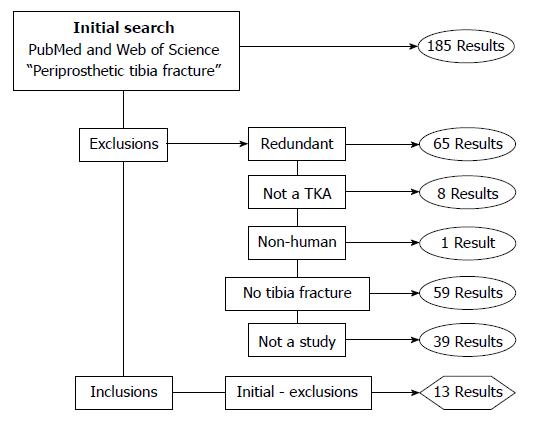
METHODS: A literature search was done to identify studies that fit the inclusion criteria. The database search yielded 185 results, which were further reduced by the exclusion criteria to 13 papers, totaling 157 patients that met these criteria. Incidence rates of the different types of periprosthetic tibia fractures were determined and their treatments were subsequently analyzed based on the fracture’s subclass, with patient outcomes being overall favorable.
RESULTS: Of the 144 documented patients, 54 (37.5%) had a subclass C fracture, which are frequently seen in revision arthroplasties or when using cement intraoperatively. The fractures of subclasses A and B occur postoperatively. There were 90 subclass A and B fractures with incidences of 18.75% and 43.75% respectively. When broken down by type, 62 (55.36%) were type 1, 24 (21.4%) were type 2, 24 (21.4%) were type 3, and 2 (1.8%) were type 4. Furthermore, from the studies that included origin of injury, the types were further classified as having non-traumatic or traumatic origins. Type 1 had 78% (40/51) non-traumatic origin and 22% (11/51) traumatic origin. Fifteen fractures were type 2, but 5 were falls and 1 through a motor vehicle accident, giving a trauma causation of 40% (6/15). Of the 24 type 3 fractures, 12 were falls and 2 vehicular accidents, leading to a trauma causation of 58% (14/24).
CONCLUSION: Type 1 fractures were the most common. Subclass A was treated with locking plates, B required a revision TKA, and C was treated intraoperatively or nonoperatively.
Core tip: A literature search of the PubMed and Web of Science databases was done to compile the known incidences and treatments of periprosthetic tibia fractures after total knee arthroplasties (TKA). Among the relatively uncommon periprosthetic tibia fracture, type 1 fractures were the most common among documented types. Subclass A fractures were treated with locking plates, subclass B fractures first required a revision TKA, and subclass C fractures were either treated intraoperatively when they occurred or were treated nonoperatively.
- Citation: Ebraheim NA, Ray JR, Wandtke ME, Buchanan GS, Sanford CG, Liu J. Systematic review of periprosthetic tibia fracture after total knee arthroplasties. World J Orthop 2015; 6(8): 649-654
- URL: https://www.wjgnet.com/2218-5836/full/v6/i8/649.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i8.649
As of 2010, there were approximately 500000 total knee arthroplastys (TKAs) being performed annually in the United States, with that number increasing each year[1]. After such a procedure, subsequent complications can no longer be treated with the same initial methodology that would be used for non-TKA patients, and so surgeons must approach each case with new treatments. One such complication is the occurrence of periprosthetic tibial fractures.
The incidence rate of periprosthetic tibial fractures after TKA is less than 1%[2], but with the increasing quantity of TKAs being performed each year, the absolute number of periprosthetic tibial fractures is also increasing[3]. However, due to its relatively scarce occurrence, very little research has been done on the subject. A meta-analysis of periprosthetic tibia fractures has not yet been done and so the purpose of this review is to compile the studies done on periprosthetic tibial fractures after TKA and analyze the procedures used for treatment. The focus will be on treatment method for the particular classification of fracture and the anatomical and functional outcome.
To locate the publications used in this review, PubMed and Web of Science databases were searched for the key term “periprosthetic tibia fracture”. From the given results, studies were individually either included or excluded. Criteria for inclusion were the following: (1) Patient must have a fracture of the tibia; and (2) Patient must have undergone a TKA.
Multiple fractures and intraoperative fractures were included. Results that appeared in multiple searches, were not from a human, or were simply a documentation of treatment methods were excluded.
Preliminary data from these studies was organized into an excel spreadsheet for analysis. Important information included study dates, fracture classifications, number of patients, treatment methods, anatomical outcomes, functional outcomes, and any complications encountered during the process. This data was qualitatively and quantitatively analyzed for successful and unsuccessful patterns as well as novel techniques that require further attention.
The database searches yielded 185 results, which were then further reduced based on the inclusion and exclusion criteria from Section 2.65 of the results. Those studies that were eliminated included redundant studies, 8 results that focused on a unicompartmental arthroplasty, 1 result that was of a canine tibia, 59 results that did not actually have a tibia fracture, and 39 results that did not have any patient data. After the exclusion of these papers, only 13 papers were left that fit the inclusion criteria. This breakdown is graphically shown in Figure 1. The papers are shown in Table 1.
| Ref. | Number of patients | Fracture type | Treatment method |
| Agarwal et al[2] | 2 | Type 2 | Revision TKA and locking plate |
| Cipriano et al[4] | 16 | Subclass C | 13 were nonoperative and 3 were braced |
| Alden et al[5] | 18 | Subclass C | Observation |
| Thompson et al[6] | 7 | Not stated | Not stated |
| Jeong et al[7] | 1 | 3A | Reduction and revision of tibial stem component |
| Beharrie et al[8] | 1 | 3B | Revision TKA with long stemmed tibial component and bone grafting |
| Ruchholtz et al[9] | NA | NA | No patients, only offered treatment methods for various fracture classifications |
| Felix et al[10] | 102 | All types | Many different methods were used depending on the fracture type |
| Watanabe et al[11] | 1 | Not stated | Revision TKA with long stemmed tibial component |
| Cordeiro et al[12] | 1 | Not Stated | Revision TKA |
| Fonseca et al[13] | 1 | 1B | Revision TKA |
| Tabutin et al[14] | 6 | 3A | Intramedullary nailing |
| Banim et al[15] | 1 | 3C | Cables and plate, with reduction |
The majority of the papers used the Felix classification system to identify the fracture type associated with the periprosthetic tibia fracture. Simply, there are 4 fracture categories: type 1 are those that extend partially across the tibial plateau, type 2 fully cross the tibial plateau, type 3 are across the tibial shaft past the tibial stem of the prosthesis, and type 4 involve the tibial tuberosity. Each of these types can be further categorized into subclasses: (1) having a stable prosthesis; (2) having an unstable prosthesis; or (3) occurring intraoperatively[10]. This breakdown can be seen in Table 2.
| Type | Description | Subclass | Description |
| 1 | Partial tibial plateau | A | Stable prosthesis |
| 2 | Full tibial plateau | B | Unstable prosthesis |
| 3 | Distal tibial shaft | C | Intraoperatively |
| 4 | Tibial tuberosity |
Many of the studies did not provide a direct cause for the fractures, instead focusing on the fracture itself and the treatment used. However, a limited number of studies did include this information and, therefore, will be the only studies included here.
Of the 144 documented patients, 54 had a subclass C fracture. These fractures, by definition, occur intraoperatively. A variety of sources can cause subclass C fractures, but they are frequently seen in revision arthroplasties or when using cement.
The fractures of subclasses A and B occur postoperatively. There were 90 subclass A and B fractures. Fifty-one were type 1 and mainly occurred non-traumatically: 8 were through a fall and only 3 were caused by a more major traumatic event. This means only 22% (11/51) of type 1 fractures were caused through trauma. Fifteen fractures were type 2, but only 5 were through falls and 1 through a motor vehicle accident, giving a trauma causation of 40% (6/15). Of the 24 type 3 fractures, 12 occurred through falls and 2 through vehicular accidents, leading to a trauma causation of 58% (14/24).
As stated before, the incidence rate of periprosthetic tibia fractures is very low, and so diagnostic methods have yet to be standardized. Frequently, a periprosthetic tibia fracture can be clinically diagnosed using the same methods that would be utilized to diagnose a typical tibia fracture. In order to classify the fracture according to the Felix system, however, a radiological evaluation is required. This is important as treatment methods, to be described in section 4D, differ based upon the fracture classification.
From the studies, not every patient’s fracture was fully classified according to the Felix system - several only stated the type or the subclass. Taking this into account, the sum of the breakdown of the types will not add up to the total number of patients in the study. This data is shown in Table 3.
| Type | Incidents | Subclass | Incidents |
| 1 | 62 | A | 27 |
| 2 | 24 | B | 63 |
| 3 | 24 | C | 54 |
| 4 | 2 | ||
| Total | 112 | Total | 144 |
As for incidence rate, of the 144 categorized by subclass, 18.75% (27/144) were subclass A, 43.75% (63/144) were subclass B, and 37.5% (54/144) were subclass C. The large portion of subclass C fractures is misleading due to the fact that many of them did not require any treatment. The subclass B fractures, however, are important as these fractures typically require additional surgery and because they are the most prominent. When broken down by type, of the 112 classified, 55.36% (62/112) were type 1, 21.4% (24/112) were type 2, 21.4% (24/112) were type 3, and 1.8% (2/112) were type 4. A vast majority of the cases were type 1, which is the smallest of the possible fractures as it does not span the width of the bone. Type 2 and 3 fractures were equally prominent. Type 4 fractures, however, appear very rare and an analysis of them is hard to obtain with such a small sample size.
Treatment of the various fractures seemed to follow a pattern based on the subclass for the fracture. Patients with a subclass A fracture typically were treated as normal, that is, as one would be treated without a periprosthetic tibial fracture. This could encompass anything from weight bearing restrictions to nails, depending on the severity of the fracture. Of the 27 cases of subclass A fractures: 6 were treated with intramedullary nailing, all of which were type 3; 2 were treated with extension immobilization and screw fixation, both were type 4; and the rest were treated with either a cast or weight bearing restrictions. Furthermore, these fractures tended to heal as typical fractures and showed little complications.
Patients with subclass B fractures were initially treated in either one of two ways: either they had a revision TKA or they did not. Besides the revision TKA, the fracture itself was treated as normal. There were 63 subclass B fractures, of which only 28 did not immediately undergo revision TKA. For the 40 that underwent revision TKAs, the fractures healed without complications. For those that were simply treated without a revision TKA; however, complications arose in 23 and a revision TKA needed to be done later in order to resolve those issues. Another article did not provide numbers of patients diagnosed with subclass B fractures, but all of them were said to have undergone revision TKA[9]. From the data gathered, it seems that an unstable prosthesis requires a revision TKA before one can address the periprosthetic tibia fracture.
Subclass C fractures tended to be the least severe. Of the 54 type C fractures, none required additional surgery. Those that are noticed intraoperatively can be treated immediately, if necessary. Twelve of the fractures required additional attention during the surgery, while the others were treated nonoperatively. Of these 12, 9 were type 1C and were either fixed with screws or wires, 2 were type 2C and were fixed with bone grafting, lastly, 1 was type 3C, which required cables and a plate after reduction. There were 42 nonoperatively treated subclass C fractures that only required weight-bearing restrictions and, occasionally, casting. Of the 54 patients, only 1 had pain after treatment and 1 passed away before fully healing. The other 52 patients saw full recovery of their subclass C fracture. Overall, subclass C fractures required the least amount of attention.
TKAs alone have a low rate of failure, only 20% after 20 years[1], and so the incidence rate of periprosthetic tibia fractures seems to follow that same trend. Data was not gathered on the number of TKAs performed each year, but the small quantity of studies and case reports found on periprosthetic tibia fractures supports the notion that they are very uncommon. Furthermore, many of the more serious fractures, types 2 and 3, are much more common after a traumatic event. It seems as if the design of the prosthesis itself, as well as the procedure used to implant it, is not a major factor in the incidence of periprosthetic tibia fractures. The one obvious exception are subclass C fractures, which have basically no other causation factors.
Nonetheless, periprosthetic tibia fractures do occur and thus are a pertinent issue that needs addressing. Of the different types of periprosthetic tibial fractures, type 1 appeared the most often making up over half of the cases. Type 1 fractures also tended to be the least severe since these fractures do not span the width of the bone. Though not explicitly documented, these fractures can frequently be described as a collapse of the tibial head, where one side of the tibia caves under pressure. These collapses are infrequent in persons with a normal knee, and so their incidence in TKAs begs the question as to what causes these fractures to arise. Firstly, when undergoing a TKA, the removal of the original knee requires cutting of the bone. If too much of the bone is cut, the remaining bone is weaker and more susceptible to fractures. These most prominently result in type 1 fractures as they are closer to the tibial head and less severe. Furthermore, altering the surface of the tibia through cutting can affect the biomechanics of the knee where the tibia contacts the prosthesis. This change in the biomechanics of the joint can redirect the forces of the knee onto different parts of the tibia, which can result in fractures of those respective parts if they cannot support the new load.
In addition to the bone loss from a TKA, muscles are also cut or moved during the procedure. Since the knee initially does not have much muscle support, altering these muscles will have a larger impact on the performance of the knee. With less muscle support, there is more force being exerted from the knee onto the surrounding bone, which can cause the collapse fractures seen in type 1 periprosthetic tibia fractures. These pressure induced fractures are much more likely to cause type 1 fractures than type 2 or 3.
As noted before, type 2 and 3 fractures are seen less frequently than type 1 fractures, but are much more likely to be the result of a traumatic incident. This lends more support to the idea that the procedure or prosthesis has less of an effect on these fractures than they do in type 1. What makes these fractures notable is that they typically require more serious treatment than their non-TKA counterparts. By already having a TKA, the tibia is weaker, and so more cautious care must be given to the healing of these fractures. This is why reduction and internal fixation, using mainly locking plates and screws, was the most common form of treatment for these fractures.
Due to the variety of treatment methods for the different fracture types, it often becomes a difficult decision for the surgeon to decide on a treatment method. It has been shown that, in cases with a subclass B fracture, a revision TKA is required for full recovery over an extended period of time. However, in subclass A cases, the surgeon must decide whether to treat operatively or not. On one hand, nonoperative treatments are often preferred by the patient and are at less risk for other complications. However, operative treatments are often more direct and can reduce the complications that arise from the prolonged immobilization of nonoperative treatment[16]. In the end, there is not a standardized method to date and the decision is still a judgment call between the patient and surgeon.
Even 17 years after the study by Felix that established the classification system for periprosthetic tibia fractures, very little research has been done on the subject. Of the 13 studies used in this review, there were only 157 patients. Furthermore, of these 157, 102 were from the Felix study done at the Mayo clinic in Rochester, Minnesota. This limits the scope of this review to mostly that specific clinic. Of the remaining 52 patients, 34 came from 2 studies specifically on intraoperative fractures. This leaves only 18 patients from novel studies, many of which were case reports. While the data gathered in this review is still relevant, it is limited in scope by the scarcity of studies on the injury.
This systematic review showed, most importantly, that there is very little data on periprosthetic tibia fractures, but with the rise in occurrence of TKA, periprosthetic tibia fracture incidence will also rise. To this end, more studying needs to be done on the topic to standardize treatment methods so the patient can be given the best treatment.
In conclusion, periprosthetic tibia fractures are relatively uncommon. Type 1 fractures were the most common among documented types. Subclass A fractures were treated with locking plates, subclass B fractures first required a revision TKA, and subclass C fractures were either treated intraoperatively when they occurred or were treated nonoperatively.
Periprosthetic tibia fractures are relatively uncommon and there are no systemic reviews on this topic thus far. Since total knee arthroplasties are increasing, the incidence of periprosthetic tibia fractures will likely also be following the same trend.
Periprosthetic tibia fractures are not very common, however, total knee arthroplasties are. Since the incidence of these fractures is low after a total knee arthroplasty (TKA), the design and material used in the implants is being reflected as good. Additionally, there has yet to be an establishment of a standardized protocol for the periprosthetic tibia fracture after TKA.
The authors have summarized the available data on periprosthetic tibia fractures and have found that periprosthetic tibia fractures are relatively uncommon. Type 1 fractures were the most common among documented types. Subclass A fractures were treated with locking plates, subclass B fractures first required a revision TKA, and subclass C fractures were either treated intraoperatively when they occurred or were treated nonoperatively.
This study can hopefully guide physicians on the periprosthetic tibia fracture and allow them to provide information to their patients. However, further investigation is still necessary.
Periprosthetic fractures are fractures that occur around implants associated with arthroplasty, particularly after TKA in the proximal tibia in this study.
This systematic review showed, most importantly, that there is very little data on periprosthetic fractures. This summarization of literature with regards to incidence and treatment can help physicians treat this situation and will improve patient outcomes.
P- Reviewer: Papachristou GC S- Editor: Tian YL L- Editor: A E- Editor: Jiao XK
| 1. | Minnesota Department of Health. Total knee replacement: Impact and recommenda-tion document 2010. [accessed 2010 Jun]. Available from: http://www.health.state.mn.us/healthreform/measurement/2010_TotalKneeReplacement.pdf. |
| 2. | Agarwal S, Sharma RK, Jain JK. Periprosthetic fractures after total knee arthroplasty. J Orthop Surg (Hong Kong). 2014;22:24-29. [PubMed] |
| 3. | Chimutengwende-Gordon M, Khan W, Johnstone D. Recent advances and developments in knee surgery: principles of periprosthetic knee fracture management. Open Orthop J. 2012;6:301-304. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Cipriano CA, Brown NM, Della Valle CJ, Moric M, Sporer SM. Intra-operative periprosthetic fractures associated with press fit stems in revision total knee arthroplasty: incidence, management, and outcomes. J Arthroplasty. 2013;28:1310-1313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Alden KJ, Duncan WH, Trousdale RT, Pagnano MW, Haidukewych GJ. Intraoperative fracture during primary total knee arthroplasty. Clin Orthop Relat Res. 2010;468:90-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 64] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 6. | Thompson NW, McAlinden MG, Breslin E, Crone MD, Kernohan WG, Beverland DE. Periprosthetic tibial fractures after cementless low contact stress total knee arthroplasty. J Arthroplasty. 2001;16:984-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Jeong GK, Pettrone SK, Liporace FA, Meere PA. “Floating total knee”: ipsilateral periprosthetic fractures of the distal femur and proximal tibia after total knee arthroplasty. J Arthroplasty. 2006;21:138-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Beharrie AW, Nelson CL. Impaction bone-grafting in the treatment of a periprosthetic fracture of the tibia: a case report. J Bone Joint Surg Am. 2003;85-A:703-707. [PubMed] |
| 9. | Ruchholtz S, Tomas J, Gebhard F, Larsen MS. Periprosthetic fractures around the knee-the best way of treatment. Eur Orthop Traumatol. 2013;4:93-102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Felix NA, Stuart MJ, Hanssen AD. Periprosthetic fractures of the tibia associated with total knee arthroplasty. Clin Orthop Relat Res. 1997;113-124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 122] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Watanabe T, Tomita T, Fujii M, Kaneko M, Sakaura H, Takeuchi E, Sugamoto K, Yoshikawa H. Periprosthetic fracture of the tibia associated with osteolysis caused by failure of rotating patella in low-contact-stress total knee arthroplasty. J Arthroplasty. 2002;17:1058-1062. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Cordeiro EN, Costa RC, Carazzato JG, Silva Jdos S. Periprosthetic fractures in patients with total knee arthroplasties. Clin Orthop Relat Res. 1990;182-189. [PubMed] |
| 13. | Fonseca F, Rebelo E, Completo A. Tibial periprosthetic fracture combined with tibial stem stress fracture from total knee arthroplasty. Revista Brasileira de Ortopedia. 2011;46:745-750. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Tabutin J, Cambas PM, Vogt F. [Tibial diaphysis fractures below a total knee prosthesis]. Rev Chir Orthop Reparatrice Appar Mot. 2007;93:389-394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Banim RH, Fletcher M, Warren P. Use of a Dall-Miles plate and cables for the fixation of a periprosthetic tibial fracture. J Arthroplasty. 2000;15:131-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Sarmah SS, Patel S, Reading G, El-Husseiny M, Douglas S, Haddad FS. Periprosthetic fractures around total knee arthroplasty. Ann R Coll Surg Engl. 2012;94:302-307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |