Published online Aug 18, 2015. doi: 10.5312/wjo.v6.i7.559
Peer-review started: March 2, 2015
First decision: May 14, 2015
Revised: June 6, 2015
Accepted: June 18, 2015
Article in press: June 19, 2015
Published online: August 18, 2015
Processing time: 172 Days and 14.2 Hours
A case of florid reactive periostitis ossificans (RPO) arising in a long bone is presented. This is a rare bone proliferation with a pronounced periosteal reaction. Less than 100 cases have been described in the literature with far fewer outside the bones of the hand, feet, fingers, and toes. Although the etiology is unknown, a relationship to preceding trauma is suggested. The imaging and histologic features show an overlap with other bone lesions including bizarre parosteal osteochondromatous proliferation, subungual exostosis, and malignant surface tumors of bone and cartilage which include, periosteal and parosteal osteosarcoma. It is important to recognize the clinical presentation and diagnostic features of RPO as a benign entity so that it is not mistaken for a more aggressive neoplasm. We present a case of a right distal humeral lesion that on histopathological review revealed florid RPO. This diagnosis was not suspected on imaging studies, but was made on open biopsy of the mass. The patient remains disease free, years postoperatively. In addition to presenting this unique case report, we review the pertinent literature, and offer a differential diagnosis and treatment strategy for its management.
Core tip: Florid reactive periostitis ossificans (RPO) is a rare benign entity that is classically localized to the phalanges of the distal extremities. This lesion is often clinico-radiologically and histologically confused for malignant entities, like osteosarcoma and chondrosarcoma. We report a rare presentation of this lesion arising from the posterior aspect of the right elbow in a 38-year-old woman, diagnosed on biopsy. Recognizing the key similarities and differences between florid RPO, and other similar appearing disorders discussed in this paper, can prevent the pitfall of misdiagnosis and unnecessary aggressive surgery.
- Citation: Soni A, Weil A, Wei S, Jaffe KA, Siegal GP. Florid reactive periostitis ossificans of the humerus: Case report and differential diagnosis of periosteal lesions of long bones. World J Orthop 2015; 6(7): 559-563
- URL: https://www.wjgnet.com/2218-5836/full/v6/i7/559.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i7.559
Reactive or reparative lesions of bone, which historically have been related to trauma, include subungual exostosis, giant cell reparative granuloma, florid reactive periostitis, and bizarre parosteal osteochondromatous proliferation (BPOP)[1]. Spjut and Dorfman[2] first identified reactive periostitis in 1981 within small tubular bones (phalanges, metacarpals, metatarsals) of the hands and feet. Typically florid reactive periostitis occurs in adolescent or young adults and presents as a small area of painful swelling and erythema over the affected bone[3,4]. As noted, these tumors typically occur in the bones of the hands and feet, but they may also present in long bones of the axial skeleton, as in our case[3-5]; when they occur in the phalanges, they are clinically reassuring, because such lesions are more likely to be benign than malignant (21:1)[4,5]. Regardless, it is important to recognize them so that they are not misdiagnosed. In this case report, we present an unusual presentation of this lesion, discuss its clinical, radiologic, and histologic appearance, review the pertinent literature, and offer a differential diagnosis and treatment strategy for its management.
A 38-year-old woman presented with a 2-mo interval of throbbing pain in her right elbow, which was aggravated by bending and lifting. The first time the patient noticed pain was soon after completing a half marathon where she carried her phone in her right hand. On physical examination she was found to have moderate swelling in the posterior aspect of her elbow along with a mild effusion and significant tenderness in the posterior-lateral compartment.
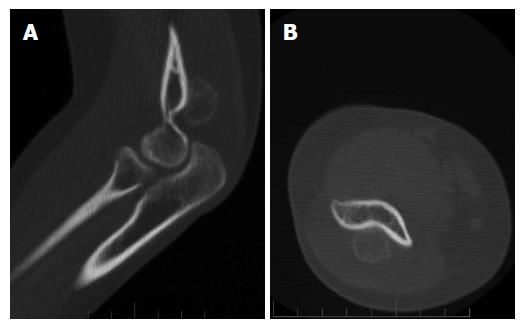
Conventional radiographs revealed an irregular mass posterior to the distal humerus just superior to the olecranon fossa (Figure 1). Magnetic resonance imaging showed extensive edema in the distal triceps muscle adjacent to the mass. A CT scan showed diffuse calcifications within the mass. No bony destruction was seen (Figure 2). At this point the differential diagnosis included atypical myositis ossificans or a neoplastic process. A repeat CT after 11 wk showed a 2.0 cm × 1.9 cm osseous excrescence arising from the posterior distal humeral metaphysis (Figure 3). The differential considerations broadened to include BPOP, a low-grade parosteal osteosarcoma, or less likely a periosteal chondroma. An open biopsy was performed through a posterior excision.
Operative findings revealed pallor of the anterior deep triceps and significant edema of the distal triceps. The specimen was removed piece-meal. The gross appearance was of loosely adherent tan-gray fibrous tissue. The distal portion of humerus showed focal necrosis and hemorrhage. Based on this appearance, an infectious etiology was considered and a fragment of the lesion was submitted for aerobic, anaerobic, mycobacterial, and fungal cultures. Histologic examination revealed mixed bland spindle cells adjacent to osteoblastic proliferation with reactive (woven) new bone formation (Figure 4). Zonation was seen suggestive of myositis ossificans (heterotopic ossification). Osteomyelitis was ruled out because of a lack of a significant inflammatory infiltrate. Osteosarcoma was ruled out because of lack of cellular atypia or tumor osteoid. There were no cytomorphologic features of a parosteal (low grade) osteosarcoma.
After surgery, her elbow motion improved from 30-degree flexion to full flexion and full forearm rotation over several weeks. The wrist and hand motion were judged to be normal with normal neuromuscular function. Neither recurrent heterotopic bone nor osteoblastic proliferation of the posterior humerus was seen radiographically. She was discharged home on a supportive Dynasplint with follow up on an outpatient basis.
Florid reactive periostitis is a benign bone lesion characterized by an aggressive periosteal reaction and soft-tissue inflammation[2,3]. This rare tumor has been identified by various names such as, pseudomalignant osseous tumor of the soft tissue, fasciitis ossificans, parosteal fasciitis and benign fibro-osseous pseudotumor[6]. For classification purposes this diagnosis is often grouped with either pseudomalignant osseous tumors of the soft tissue or myositis ossificans. Due to its mild course, it is generally managed by observation after initial biopsy, but rarely it can be locally aggressive and recurrent[7]. The imaging and histologic features of this benign bone lesion, show an overlap with other bone lesions including BPOP, subungual exostosis, osteomyelitis, myositis ossificans, and malignant surface tumors of bone and cartilage which include, conventional, periosteal and parosteal osteosarcoma.
Like florid reactive periostitis, BPOP (also known as Nora’s lesion) is also a rare entity that is grossly described as an exophytic outgrowth of the cortical surface of the phalanges of the hands and feet[6,8]. It is composed of a disorganized mixture of bone, cartilage, and fibrous tissue and the upper extremities are four times more affected than the lower extremities[8-10]. This lesion can present itself at any age, but individuals in their 20's and 30's are higher at risk[10-12]. It is sometimes mistaken for a malignant process due to its high rate of recurrence, proliferative nature, and atypical microscopic appearance[12]. However, unlike osteosarcoma, on imaging BPOP lacks cortical flaring and communication with the underlying medullary canal[12-15]. On histology, the exophytic bone mass has a characteristic dark blue tinctorial quality, especially at the interface with the cartilage. The intertrabecular spaces contain proliferating spindle cells that lack cytological atypia. The cartilaginous component is hypercellular and contains irregular groups of binucleated and “bizarre” chondrocytes. Although double-nucleated chondrocytes are common, hyperchromasia and cytological atypia are typically not present[13,16].
Another benign lesion that occurs in relation to the long bones (and shows overlapping radiologic and histologic findings with reactive periostitis) is myositis ossificans traumatica[17]. This lesion most commonly occurs in the muscles of the arms or in the quadriceps following covert or overt trauma[17]. On imaging, soft tissue calcifications are visible within 2–6 wk of the inciting incident. Peripheral ossification is the characteristic feature noted on CT[17,18]. This lesion is generally not biopsied as it rapidly resolves, but if clinical and imaging studies are inconclusive, an open biopsy may be indicated. There are three phases of myositis ossificans: acute (fibroblastic zone), subacute (osteoblastic zone), and late (calcified zone). Detection of this zonal phenomenon on histology is diagnostic of myositis ossificans[17,18].
Chronic osteomyelitis may also be in the differential diagnosis. This diagnosis is made radiologically by the presence of an osteolytic center with a ring of sclerosis on conventional imaging[19]. Additionally, a culture of the biopsy tissue is needed to support the diagnosis and identify the specific pathogen. Histology often only shows sclerotic bone with chronic inflammatory cells[20]. Due to its infectious etiology, treatment involves surgical debridement and prolonged antibiotic therapy.
Furthermore, subungual exostoses can also mimic florid reactive periostitis. These are bony projections that protrude from the dorsal aspect of the distal phalanx[21]. The reason it occurs on the dorsal aspect is thought due to the fact that the periosteum is relatively loose dorsally, but very tightly adherent on its volar aspect[22]. Due to its location, this lesion may lead to the destruction of the nail bed causing considerable pain or discomfort. There is a reproducible translocation [t(x; 6) (q13; q22)] associated with this diagnosis and thus, it may be considered a true neoplasm. Surgical excision is the mainstay of therapy.
Lastly, malignant osteoblastic tumors including parosteal, periosteal, and conventional osteosarcoma are considered in the differential diagnosis. These tumors are most prevalent in children and young adults[23,24]. They are localized at the end of long bones. Most often they affect the proximal end of the tibia or humerus, or the distal end of the femur. Of the three types, parosteal osteosarcoma has the best prognosis, followed by periosteal and then conventional. Periosteal osteosarcoma is the most uncommon among the three types[25]. This lesion most commonly appears in the diaphysis or metadiaphysis of the tibia and femur. Grossly, the tumor may form a cavity deep in the cortex with radiating striations that may break into the medullary cavity as the disease progresses. Histologically, there is a prominent cartilaginous component to this tumor with a small amount of osteoid production. Treatment depends on grade. Low-grade lesions may be treated with wide surgical excision alone, while higher-grade lesions may require chemotherapy in addition to surgery[25]. Parosteal osteosarcoma is the most frequently occurring osteosarcoma and thus it is crucial to diagnostically separate this entity from reactive periostitis. Seventy percent of the time, it arises in the metaphysis of the posterior aspect of the distal femur and less frequently involves the proximal tibia and humerus. It is composed of a dense osteoid component that extends from the outer cortex via a narrow zone[26,27]. Histologically, it exhibits an extensive boney matrix with a hypocellular stroma and mild to minimal fibroblastic cellular atypia. Radiologically, it takes the appearance of a firm, lobulated “cauliflower-like”, lesion encircling the bone. A thin radiolucent line delineating the tumor from the cortex, known as the “string sign”, is seen radiologically in 30% of cases. Treatment for parosteal osteosarcomas usually involves surgical resection without neoadjuvant chemotherapy, as these tumors are commonly low-grade in nature[26,27]. Conventional osteosarcoma can usually be easily separated from reactive periostitis. Histologically, these tumor cells are very pleomorphic with numerous atypical mitoses that are entrapped in the osteoid matrix. Complete radical surgical en bloc resection with chemotherapy is the treatment of choice for conventional osteosarcoma[25].
It can be appreciated from the above differentials that the diagnosis of florid reactive periostitis is often challenging. Therefore, a careful assessment of clinical history, radiology, and pathology are helpful in reaching an accurate diagnosis. Although rare, this entity should be considered in the differential diagnosis of any osteogenic growth in long bones. Being aware of the above differentials can assist in separating this benign entity from its malignant mimickers. Once the malignant and infectious imitators of this lesion are ruled out, treatment can be discussed. When presenting early, this process can be treated conservatively with rest and nonsteroidal anti-inflammatory medication. When presenting late, with an aggressive nature and/or with recurrence, wide local resection is considered treatment of choice.
A 38-year-old woman with no significant medical history presented with a 2-mo history of throbbing pain in her right elbow, which was aggravated by bending and lifting.
Moderate swelling in the posterior aspect of her elbow along with a mild effusion and significant tenderness in the posterior-lateral compartment.
Atypical myositis ossificans, bizarre parosteal osteochondromatous proliferation, low-grade parosteal osteosarcoma, periosteal chondroma or chondrosarcoma.
All labs were within normal limits.
CT showed a 2.0 cm × 1.9 cm osseous excrescence arising from the posterior distal humeral metaphysis.
Florid-reactive periostitis ossificans.
Complete surgical excision of lesion.
Reactive periostitis ossificans is a benign entity that classically present in the hands/feet, very rarely it has been reported in long bones with an etiology related to trauma. This entity is commonly confused for a neoplastic process due to its unusual location and can at times even histologically mimic sarcoma.
Benign parosteal osteochondromatous proliferations (BPOP) is a rare cartilaginous neoplasm that like reactive periostitis ossisficans (RPO) presents in the hands/feet. BPOP is known to be locally aggressive and requires extensive surgical resection.
This is entity is commonly confused for a neoplastic process due to its unusual location and can at times even histologically mimic sarcoma. Recognizing this as a diagnostic pitfall can prevent misdiagnosis and eliminate the need for aggressive surgical treatment.
The paper is well written.
P- Reviewer: Iwamoto J, Kim SJ S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK
| 1. | Ostrowski ML, Spjut HJ. Lesions of the bones of the hands and feet. Am J Surg Pathol. 1997;21:676-690. [PubMed] |
| 2. | Spjut HJ, Dorfman HD. Florid reactive periostitis of the tubular bones of the hands and feet. A benign lesion which may simulate osteosarcoma. Am J Surg Pathol. 1981;5:423-433. [PubMed] |
| 3. | Azorín D, López-Pino MA, González-Mediero I, Epeldegui T, López-Barea F. Long bone florid reactive periostitis ossificans: a case in the distal femur mimicking osteosarcoma. J Pediatr Orthop B. 2008;17:301-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Brien EW, Zahiri CA, Mirra JM. Florid reactive periostitis ossificans of the proximal aspect of the tibia: a lesion that must be distinguished from osteosarcoma. A case report. J Bone Joint Surg Am. 1999;81:1002-1007. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Gao Z, Wang J, Wang Z, Meng Q. Florid reactive periostitis of the metacarpal and phalanx: 2 case reports. J Hand Surg Am. 2013;38:2134-2137. [PubMed] |
| 6. | Porcel López MT, Fernández Gil MA, Campos de Orellana A, Quiles Galindo M. Florid reactive periostitis ossificans of the distal ulna. Orthopedics. 2008;31:286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Nance KV, Renner JB, Brashear HR, Siegal GP. Massive florid reactive periostitis. Pediatr Radiol. 1990;20:186-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Nora FE, Dahlin DC, Beabout JW. Bizarre parosteal osteochondromatous proliferations of the hands and feet. Am J Surg Pathol. 1983;7:245-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 197] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Torreggiani WC, Munk PL, Al-Ismail K, O’Connell JX, Nicolaou S, Lee MJ, Masri BA. MR imaging features of bizarre parosteal osteochondromatous proliferation of bone (Nora’s lesion). Eur J Radiol. 2001;40:224-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 51] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Abramovici L, Steiner GC. Bizarre parosteal osteochondromatous proliferation (Nora’s lesion): a retrospective study of 12 cases, 2 arising in long bones. Hum Pathol. 2002;33:1205-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 74] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 11. | Gursel E, Jarrahnejad P, Arneja JS, Malamet M, Akinfolarin J, Chang YJ. Nora’s lesion: Case report and literature review of a bizarre parosteal osteochondromatous proliferation of a small finger. Can J Plast Surg. 2008;16:232-235. [PubMed] |
| 12. | Bandiera S, Bacchini P, Bertoni F. Bizarre parosteal osteochondromatous proliferation of bone. Skeletal Radiol. 1998;27:154-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 36] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Meneses MF, Unni KK, Swee RG. Bizarre parosteal osteochondromatous proliferation of bone (Nora’s lesion). Am J Surg Pathol. 1993;17:691-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 161] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 14. | Smith NC, Ellis AM, McCarthy S, McNaught P. Bizarre parosteal osteochondromatous proliferation: a review of seven cases. Aust N Z J Surg. 1996;66:694-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Sundaram M, Wang L, Rotman M, Howard R, Saboeiro AP. Florid reactive periostitis and bizarre parosteal osteochondromatous proliferation: pre-biopsy imaging evolution, treatment and outcome. Skeletal Radiol. 2001;30:192-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 51] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | Michelsen H, Abramovici L, Steiner G, Posner MA. Bizarre parosteal osteochondromatous proliferation (Nora’s lesion) in the hand. J Hand Surg Am. 2004;29:520-525. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 60] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 17. | Sodl JF, Bassora R, Huffman GR, Keenan MA. Traumatic myositis ossificans as a result of college fraternity hazing. Clin Orthop Relat Res. 2008;466:225-230. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Chadha M, Agarwal A. Myositis ossificans traumatica of the hand. Can J Surg. 2007;50:E21-E22. [PubMed] |
| 19. | Kumar V, Abbas AK, Fausto N, Mitchell RN. Robbins Basic Pathology. 8th ed.. Saunders Elsevier. 2007;810-811. |
| 20. | Senneville E, Morant H, Descamps D, Dekeyser S, Beltrand E, Singer B, Caillaux M, Boulogne A, Legout L, Lemaire X. Needle puncture and transcutaneous bone biopsy cultures are inconsistent in patients with diabetes and suspected osteomyelitis of the foot. Clin Infect Dis. 2009;48:888-893. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 70] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 21. | Rapini RP, Bolognia JL, Jorizzo JL. Dermatology: 2-Volume Set. St. Louis: Mosby 2007; . |
| 22. | Suga H, Mukouda M. Subungual exostosis: a review of 16 cases focusing on postoperative deformity of the nail. Ann Plast Surg. 2005;55:272-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 23. | Klein MJ, Siegal GP. Osteosarcoma: anatomic and histologic variants. Am J Clin Pathol. 2006;125:555-581. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 275] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 24. | Yarmish G, Klein MJ, Landa J, Lefkowitz RA, Hwang S. Imaging characteristics of primary osteosarcoma: nonconventional subtypes. Radiographics. 2010;30:1653-1672. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 90] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 25. | Luetke A, Meyers PA, Lewis I, Juergens H. Osteosarcoma treatment - where do we stand? A state of the art review. Cancer Treat Rev. 2014;40:523-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 759] [Cited by in RCA: 945] [Article Influence: 78.8] [Reference Citation Analysis (0)] |
| 26. | Murphey MD, Jelinek JS, Temple HT, Flemming DJ, Gannon FH. Imaging of periosteal osteosarcoma: radiologic-pathologic comparison. Radiology. 2004;233:129-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 91] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 27. | Jelinek JS, Murphey MD, Kransdorf MJ, Shmookler BM, Malawer MM, Hur RC. Parosteal osteosarcoma: value of MR imaging and CT in the prediction of histologic grade. Radiology. 1996;201:837-842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 73] [Article Influence: 2.5] [Reference Citation Analysis (0)] |