Published online Jul 18, 2015. doi: 10.5312/wjo.v6.i6.491
Peer-review started: February 25, 2015
First decision: April 10, 2015
Revised: May 6, 2015
Accepted: May 16, 2015
Article in press: May 18, 2015
Published online: July 18, 2015
Processing time: 141 Days and 12.1 Hours
AIM: To determine an association between when the study was performed, the robustness of the study and the outcomes for insertional and non-insertional Achilles tendinopathy surgery.
METHODS: We performed a systematic review in accordance with the PRISMA guidelines to assess the methodology of studies investigating the outcome of surgery in chronic Achilles tendinopathy over the last 50 years to identify any trends that would account for the variable results. The Coleman Methodology Scores were correlated with the reported percentage success rates and with the publication year to determine any trends using Pearson’s correlation.
RESULTS: We identified 62 studies published between 1964 and 2014 reporting on a total of 2923 surgically treated Achilles tendinopathies. The average follow-up time was 40 mo (range 5-204 mo), and the mean reported success rate was 83.5% (range 36%-100%). The Coleman Methodology Scores were highly reproducible (r = 0.99, P < 0.01), with a mean of 40.1 (SD 18.9, range 2-79). We found a negative correlation between reported success rate and overall methodology scores (r = -0.40, P < 0.001), and a positive correlation between year of publication and overall methodology scores (r = 0.46, P < 0.001).
CONCLUSION: We conclude that although the success rate of surgery for chronic Acilles tendinopathy described in the literature has fallen over the last 50 years, this is probably due to a more rigorous methodology of the studies.
Core tip: Although the success rate of surgery for chronic Acilles tendinopathy described in the literature has fallen over the last 50 years, this is probably due to a more rigorous methodology of the studies. Future studies with more robust methodologies will hopefully address some of the unanswered questions in the surgical management of this difficult condition.
- Citation: Khan WS, Malvankar S, Bhamra JS, Pengas I. Analysing the outcome of surgery for chronic Achilles tendinopathy over the last 50 years. World J Orthop 2015; 6(6): 491-497
- URL: https://www.wjgnet.com/2218-5836/full/v6/i6/491.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i6.491
Overuse injuries of the Achilles tendon are becoming increasingly common. Its manifestation used to be more associated with male athletes[1], however the rise in the incidence of Achilles tendon disorders is considered to be due to more females participating in recreational and competitive sporting activities[1]. Even though injuries of the Achilles tendon are on the rise, little is known regarding the long-term outcome of their surgical management due to a lack of reliable outcome studies[2]. Subjectively there is evidence that the surgical outcomes reported in the literature are worse than those described historically[3].
In addition to the lack of reliable research on the management of insertional and non-insertional Achilles tendinopathy, there is also a poor understanding of its pathogenesis, and its aetiology is unknown[4]. Even though Achilles tendinopathy has been linked to overuse, one study found that 31% of 58 patients who had Achilles tendinopathy did not participate in vigorous activity[5]. Other suggested Achilles tendinopathy caused by a mixture of intrinsic and extrinsic factors such as poor vascularity, genetic make-up, quinolone antibiotics, change of training regime or a change of foot wear[5]. The term “tendinitis” is incorrect as Achilles tendinopathy is not an inflammatory reaction[6]. Puddu et al[7] stated that “tendinosis” is a better term as this describes the collagen degeneration that occurs in tendinopathy, however this can only be conclusively demonstrated after histopathological confirmation[7]. Puddu et al[7] also further classified Achilles tendon disease based on his histological findings into peritendinitis and tendinosis, that could coexist and also develop into each other[7]. We therefore advocate the use of the term “tendinopathy” as a generic descriptor of the clinical conditions in and around tendons arising from overuse, eliminating the need for histopathological confirmation[3].
The lack of understanding of this condition and the poor use of terminology leave many questions to be answered, regarding the management of Achilles tendinopathy[3]. It has been stated generally that conservative treatment is not successful for patients with chronic Achilles tendinopathy and that surgical intervention is needed for 25% of patients[4]. Research has showed that the historical short-term results of surgical treatment are frequently very good but these studies are generally unreliable and fail to record the long term outcome of surgical management[4].
We therefore performed a systematic review of the available published literature over the last 50 years to analyse the studies and identify any explanations for these observations.
This review was carried out following Institutional Review Board approval in accordance to PRISMA guidelines to analyse the quality of studies investigating the outcome of surgery for chronic Achilles tendinopathy from 1964-2014. The eligibility criterion for this systematic review was any study that investigated the surgical outcome for Achilles tendinopathy as its primary goal and that had its full text available in the English language. The eligibility criteria were not limiting as the aim of this study was to critically analyse the quality of the methodologies. A MEDLINE search covering the years 1964 to 2014 was performed. The search was first carried out on 10 September 2014 and the date last searched was 28 January 2015. Keywords used in the search were “Achilles tendon”, “tendinitis”, “tendon”, “surgery”, “postoperative complications”, “tendon injuries” and “tendinopathy”. All journals were considered and all relevant articles were retrieved. A hand search was also conducted and all relevant articles were also included in the study. The study selection process involved screening the study titles to check their relevance to Achilles tendinopathy, and then subsequently their abstracts were screened to check that the primary goal of each included study was investigating the surgical outcome of chronic Achilles tendinopathy. Studies that investigated the surgical outcome of Achilles tendon ruptures were excluded as even though these can develop as a result of chronic Achilles tendinopathy, this is not always the case and ruptures are Achilles tendinopathy, this is not always the case and ruptures are appropriately a separate medical condition in itself. The data collection involved examining all the studies for their reported surgical outcomes. We used the functional classification described by Nelen et al[8] (Table 1) to compare the outcome of the studies. We defined “success rate” as the sum of excellent and good outcomes expressed as a percentage of the total outcomes. A methods assessment for risk of bias in individual studies was carried out by using the criteria developed by Coleman et al[9] (Table 2) to blindly assess the methods of each article twice. Where previous Coleman Methodology Scores were available for studies in the literature, the scores were checked to ensure they corresponded. Each study was given a Coleman Methodology Score of between 0 and 100 after scoring for 10 criteria. The Coleman Methodology Scores were correlated with the reported percentage success rates and with the publication year to determine any trends using Pearson’s correlation (r). A statistical review of the study was performed by a biomedical statistician.
| Rating | Result |
| Excellent | No residual symptoms, sports performance unlimited |
| Good | Full return to the same sport as preoperatively; some stiffness after strenuous activities |
| Fair | Improvement with regard to the preoperative situation; still stiffness and aching relating to sports |
| Poor | No improvement at all |
| Section | Number or factor | Score |
| Part A - only one score to be given for each of the seven sections | ||
| Study size - number of tendons (N) (if multiple follow-up, multiply N by number of times subjects followed up) | > 60 | 10 |
| 41-60 | 7 | |
| 20-40 | 4 | |
| < 20, not stated | 0 | |
| Mean follow-up (mo) | > 24 | 5 |
| 12-24 | 2 | |
| < 12, not stated, or unclear | 0 | |
| Number of different surgical procedures included in each reported outcome. More than one surgical technique may be assessed but separate outcomes should be reported | One surgical procedure only | 10 |
| More than one surgical procedure, but > 90% of subjects undergoing the one procedure | 7 | |
| Not stated, unclear, or < 90% of subjects undergoing the one procedure | 0 | |
| Type of study | Randomized control trial | 15 |
| Prospective cohort study | 10 | |
| Retrospective cohort study | 0 | |
| Diagnostic certainty (use of preoperative ultrasound, MRI, or postoperative histopathology to confirm diagnosis) | In all | 5 |
| In > 80% | 3 | |
| In < 80%, not stated, or unclear | 0 | |
| Description of surgical procedure given | Adequate (technique stated and necessary details of that type of procedure given) | 5 |
| Fair (technique only stated without elaboration) | 3 | |
| Inadequate, not stated, or unclear | 0 | |
| Description of postoperative rehabilitation | Well described with > 80% of patients complying | 10 |
| Well described with 60%-80% of patients complying | 5 | |
| Protocol not reported or < 60%-80% of patients complying | 0 | |
| Part B - scores may be given for each option in each of the three sections if applicable | ||
| Outcome criteria (if outcome criteria is vague and does not specify subjects’ sporting capacity, score is automatically 0 for this section) | Outcome measures clearly defined | 2 |
| Timing of outcome assessment clearly stated (e.g., at best outcome after surgery or at follow-up) | 2 | |
| Use of outcome criteria that has reported good reliability | 3 | |
| Use of outcome with good sensitivity | 3 | |
| Procedure for assessing outcomes | Subjects recruited (results not taken from surgeons’ file) | 5 |
| Investigator independent of surgeon | 4 | |
| Written assessment | 3 | |
| Completion of assessment by subjects themselves with minimal investigator assistance | 3 | |
| Description of subject selection process | Selection criteria reported and unbiased | 5 |
| Recruitment rate reported: > 80% or < 80% | 5 | |
| Eligible subjects not included in the study satisfactorily accounted for or 100% recruitment | 5 | |
We identified 62[2,4-6,8,10-66] studies published between 1964 and 2014 reporting on a total of 2923 surgically treated Achilles tendinopathies. The average follow-up time was 40 mo (range 5-204 mo), and the mean reported success rate was 83.5% (range 36%-100%). The mean Coleman Methodology Scores for each of the 10 criteria for the included studies are summarised in Table 3.
| Methodology criteria (maximum score) | Mean | Range | |
| Score | SD | ||
| Part A | |||
| Study size (10) | 4.5 | 4.6 | 0-10 |
| Follow-up (10) | 3.3 | 2.4 | 0-5 |
| No. of procedures (10) | 6.6 | 5 | 0-10 |
| Type of study (15) | 3.4 | 5.4 | 0-10 |
| Diagnostic certainty (5) | 1.9 | 2.5 | 0-5 |
| Description of surgical technique (5) | 4.1 | 1.8 | 0-5 |
| Rehabilitation and compliance (10) | 4.8 | 5 | 0-10 |
| Part B | |||
| Outcome criteria (10) | 4.7 | 3.7 | 0-10 |
| Outcome assessment (15) | 5.2 | 4.5 | 0-12 |
| Selection process (15) | 4.6 | 6 | 0-15 |
| Methodology score (100) | 40.1 | 18.9 | 2-79 |
The methodology of each study was blindly assessed twice, and the Coleman Methodology Scores were highly reproducible (r = 0.99, P < 0.01), with a mean of 40.1 (SD 18.9, range 2-79). The Coleman Methodology Scores for the individual studies are shown in Table 4. The Table also includes data on year of publication, mean follow-up period, number of tendons and percentage success.
| Ref. | Year of study | Mean follow-up (mo) | N Tendons | % Success | Coleman Methodology Scores |
| Snook[10] | 1972 | 4 | 3 | ||
| Burry and Pool[11] | 1973 | 5 | 2 | ||
| Clancy et al[12] | 1976 | 5 | 5 | ||
| Denstad and Roaas[13] | 1979 | 58 | 46 | ||
| Gould and Korson[14] | 1980 | 12 | 8 | ||
| Kvist and Kvist[15] | 1980 | 201 | 97 | 35 | |
| Leach et al[16] | 1981 | 20 | 10 | ||
| Subotnick and Sisney[17] | 1986 | 42 | 15 | ||
| Saillant et al[18] | 1987 | 42 | 65 | 86 | 36 |
| Schepsis and Leach[19] | 1987 | 36 | 45 | 87 | 44 |
| Nelen et al[8] | 1989 | 143 | 67 | 41 | |
| Leppilahti et al[20] | 1991 | 150 | 86 | 12 | |
| Anderson et al[21] | 1992 | 52 | 48 | 94 | 27 |
| Clement et al[22] | 1992 | 69 | 14 | 13 | |
| Leach et al[23] | 1992 | 12 | 85 | 8 | |
| Leppilahti et al[24] | 1994 | 48 | 275 | 73 | 50 |
| Schepsis et al[25] | 1994 | 79 | 79 | 66 | |
| Aström and Rausing[26] | 1995 | 163 | 43 | ||
| Alfredson et al[6] | 1996 | 12 | 13 | 60 | |
| Johnston et al[27] | 1997 | 24 | 41 | 22 | |
| Maffulli et al[28] | 1997 | 22 | 52 | 71 | 70 |
| Morberg et al[29] | 1997 | 72 | 64 | 67 | 74 |
| Rolf and Movin[5] | 1997 | 25 | 60 | 75 | 69 |
| Alfredson et al[30] | 1998 | 12 | 11 | 59 | |
| Maffulli et al[31] | 1999 | 35 | 14 | 36 | 56 |
| Paavola et al[32] | 2000 | 5 | 142 | 59 | |
| Wilcox et al[33] | 2000 | 14 | 20 | 32 | |
| Ohberg et al[34] | 2001 | 60 | 24 | 92 | 65 |
| Shalabi et al[35] | 2001 | 24 | 15 | 87 | 51 |
| Maquirriain et al[36] | 2002 | 16 | 7 | 37 | |
| Paavola et al[37] | 2002 | 7 | 42 | 46 | |
| Shalabi et al[38] | 2002 | 24 | 15 | 80 | 51 |
| Yodlowski et al[39] | 2002 | 39 | 41 | 39 | |
| Chiara Vulpiani et al[40] | 2003 | 156 | 86 | 88 | 35 |
| Den Hartog et al[41] | 2003 | 35 | 29 | 88 | 34 |
| Saxena[42] | 2003 | 56 | 37 | 100 | 17 |
| Martin et al[43] | 2005 | 41 | 44 | 52 | |
| Costa et al[44] | 2006 | 90 | 21 | 27 | |
| Johnson et al[45] | 2006 | 34 | 22 | 32 | |
| Maffulli et al[46] | 2006 | 37 | 93 | 81 | 74 |
| Wagner et al[47] | 2006 | 40 | 81 | 29 | |
| Alfredson et al[2] | 2007 | 6 | 20 | 61 | |
| Cottom et al[48] | 2008 | 27 | 62 | 95 | 37 |
| Hahn et al[49] | 2008 | 46 | 13 | 38 | |
| Maffulli et al[50] | 2008 | 40 | 86 | 73 | 79 |
| Vega et al[51] | 2008 | 24 | 8 | 100 | 51 |
| Bohu et al[52] | 2009 | 42 | 137 | 29 | |
| Thermann et al[53] | 2009 | 6 | 8 | 37 | |
| Will et al[54] | 2009 | 22 | 19 | 34 | |
| Duthon et al[55] | 2011 | 24 | 17 | 79 | 48 |
| van Sterkenburg et al[56] | 2011 | 12 | 3 | 100 | 44 |
| Maffulli et al[57] | 2011 | 36 | 30 | 85 | 54 |
| Sarimo et al[58] | 2011 | 30 | 24 | 100 | 42 |
| Oshri et al[59] | 2012 | 21 | 62 | 43 | |
| Kiewiet et al[60] | 2013 | 35 | 12 | 30 | |
| Maffulli et al[61] | 2013 | 204 | 39 | 77 | 42 |
| Maquirriain[62] | 2013 | 92 | 27 | 96 | 47 |
| Benazzo et al[63] | 2014 | 48 | 52 | 60 | |
| Tallerico et al[64] | 2014 | 14 | 11 | 28 | |
| Maffulli et al[65] | 2015 | 54 | 18 | 100 | 38 |
| Nawoczenski et al[66] | 2015 | 18 | 13 | 85 | 52 |
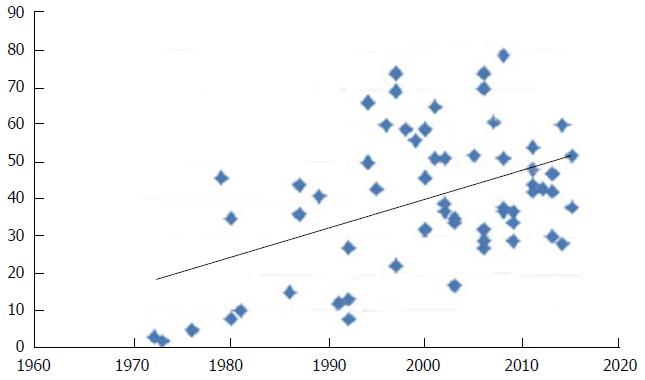
The Coleman Methodology Scores were correlated with the reported success rate and year of publication to determine any trends. For the 62 studies, the methodology score negatively correlated with the reported success rate (r = -0.40, P < 0.001) suggesting that studies with lower methodology scores reported higher success rates (Figure 1). The methodology score positively correlated with the year of publication (r = 0.46, P < 0.001) suggesting that methodology has improved over the past 50 years (Figure 2).
Our review identified 62 studies investigating almost 3000 tendons followed up for almost 40 mo published over the last 50 years that looked at surgical outcome of Achilles tendinopathy. The studies included in our review reported a mean success rate of 84% (SD 14%). The studies had a mean Coleman Methodology Score of 40 (SD 19). Our results identified trends in Coleman Methodology Score with the year of publication and the success rate. It was interesting to note that as the Coleman Methodology Scores improve, the success rate of studies falls. This is likely to be due to the fact that more robust studies with a higher methodology score are more objective in assessing outcome and are associated with less bias. The Coleman Methodology Score is produced by assessing two parts and the more robust studies scored well in both of these. The first part scored higher for a robust high quality studies with a larger number of patients with diagnostic certainty, longer follow-ups, and describing only one surgical procedure. These studies described the surgical procedure and post-operative rehabilitation regime well. Studies that did not score well included retrospective studies with fewer patients, with poorer diagnostic certainty, shorter follow-up, and possibly describing more than one procedure. These factors although describe poor methodology, do lend them to a higher success rate. Retrospective short-term studies are associated with recall bias and are known to produce a higher success rate that randomised controlled trials with long-term follow-up. The second part scored higher for well-defined patient recruitment, valid outcome criteria and independent assessment. Studies that did not score well included poor reporting of patient recruitment, unreliable outcome measures and where there was greater investigator assistance in completing assessment. Again, these factors would contribute to a higher success rate. Over the past 50 years we have shown that the Coleman Methodology Scores has been increasing. There was a shift from retrospective to prospective studies. Over the last 50 years the number of journals and publications has increased, but this is associated with an increase in the quality of studies. Historically, most studies were retrospective studies reporting short-term follow-up for a small number of patients. More recent studies have included randomised controlled trials that recruit a large number of patients and report longer follow-ups. More recent studies are also more likely to confirm the diagnosis radiologically before instigating treatment, and describe the surgical procedure and post-operative rehabilitation regime well. We suggest future studies to continue to use a robust methodology. This should include multi-centre randomised controlled trials using a large number of patients with long-term follow-up where possible. It is important to have well-defined inclusion and exclusion criteria. These studies should have a uniform pre-operative, operative and post-operative rehabilitation course, with a greater degree of diagnostic certainty. They should be free from selection bias and results bias by describing the selection process and having a good follow-uprate. It is important to use a valid, reliable and responsive outcome measure that is free from bias. Blinding and independence of the investigator is useful. These studies are however associated with greater costs. We hope that poorer success rates that are associated with better methodology do not result in publication bias.
Insertional and non-insertional Achilles tendinopathy is a difficult problem to manage and surgery is performed when non-operative treatmentoptions fail.
Studies for insertional and non-insertional Achilles tendinopathy surgery describe a variable outcome in the literature. Future studies need to use a more robust methodology.
The authors performed a systematic review in accordance with the PRISMA guidelines to assess the methodology of studies investigating the outcome of surgery in chronic Achilles tendinopathy over the last 50 years to identify any trends that would account for the variable results. The Coleman Methodology Scores were correlated with the reported percentage success rates and with the publication year to determine any trends using Pearson’s correlation. The authors found a negative correlation between reported success rate and overall methodology scores (r = -0.40, P < 0.001), and a positive correlation between year of publication and overall methodology scores (r = 0.46, P < 0.001). The authors conclude that although the success rate of surgery for chronic Acilles tendinopathy described in the literature has fallen over the last 50 years, this is probably due to a more rigorous methodology of the studies.
Although the success rate of surgery for chronic Acilles tendinopathy described in the literature has fallen over the last 50 years, this is probably due to a more rigorous methodology of the studies. Future studies with more robust methodologies will hopefully address some of the unanswered questions in the surgical management of this difficult condition.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) is an evidence-based minimum set of items for reporting in systematic reviews and meta-analysis.
This work proposes an extensive review on Achilles tendinopathy over the last 50 years. There are merits in this study because it may give some cues for future researches and clinical application in Achilles tendinopathy. As such, the theme is of interest.
P- Reviewer: Ju X, Wukich DK S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Kvist M. Achilles tendon injuries in athletes. Sports Med. 1994;18:173-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 326] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 2. | Alfredson H, Ohberg L, Zeisig E, Lorentzon R. Treatment of midportion Achilles tendinosis: similar clinical results with US and CD-guided surgery outside the tendon and sclerosing polidocanol injections. Knee Surg Sports Traumatol Arthrosc. 2007;15:1504-1509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Tallon C, Coleman BD, Khan KM, Maffulli N. Outcome of surgery for chronic Achilles tendinopathy. A critical review. Am J Sports Med. 2001;29:315-320. [PubMed] |
| 4. | Alfredson H, Lorentzon R. Chronic Achilles tendinosis: recommendations for treatment and prevention. Sports Med. 2000;29:135-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 246] [Cited by in RCA: 214] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 5. | Rolf C, Movin T. Etiology, histopathology, and outcome of surgery in achillodynia. Foot Ankle Int. 1997;18:565-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 178] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 6. | Alfredson H, Pietilä T, Lorentzon R. Chronic Achilles tendinitis and calf muscle strength. Am J Sports Med. 1996;24:829-833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Puddu G, Ippolito E, Postacchini F. A classification of Achilles tendon disease. Am J Sports Med. 1996;4:145-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 305] [Cited by in RCA: 232] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Nelen G, Martens M, Burssens A. Surgical treatment of chronic Achilles tendinitis. Am J Sports Med. 1996;17:754-759. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 108] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10:2-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 647] [Cited by in RCA: 767] [Article Influence: 30.7] [Reference Citation Analysis (0)] |
| 10. | Snook GA. Achilles tendon tenosynovitis in long-distance runners. Med Sci Sports. 1972;4:155-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Burry HC, Pool CJ. Central degeneration of the Achilles tendon. Rheumatol Rehabil. 1973;12:177-181. [RCA] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Clancy WG, Neidhart D, Brand RL. Achilles tendonitis in runners: a report of five cases. Am J Sports Med. 1976;4:46-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 94] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Denstad TF, Roaas A. Surgical treatment of partial Achilles tendon rupture. Am J Sports Med. 1979;7:15-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 34] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Gould N, Korson R. Stenosing tenosynovitis of the pseudosheath of the tendo Achilles. Foot Ankle. 1980;1:179-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Kvist H, Kvist M. The operative treatment of chronic calcaneal paratenonitis. J Bone Joint Surg Br. 1980;62:353-357. [PubMed] |
| 16. | Leach RE, James S, Wasilewski S. Achilles tendinitis. Am J Sports Med. 1981;9:93-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 72] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Subotnick SI, Sisney P. Treatment of Achilles tendinopathy in the athlete. J Am Podiatr Med Assoc. 1986;76:552-557. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 27] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 18. | Saillant G, Thoreux J, Benazet JP. The surgical treatment of Achilles tendinitis in athletes. French J Orthop Surg. 1987;1:368-372. |
| 19. | Schepsis AA, Leach RE. Surgical management of Achilles tendinitis. Am J Sports Med. 1987;15:308-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 173] [Cited by in RCA: 136] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 20. | Leppilahti J, Orava S, Karpakka J, Takala T. Overuse injuries of the Achilles tendon. Ann Chir Gynaecol. 1991;80:202-207. [PubMed] |
| 21. | Anderson DL, Taunton JE, Davidson RG. Surgical management of chronic Achilles tendinitis. Clin J Sport Med. 1992;2:38-42. [DOI] [Full Text] |
| 22. | Clement D, Taunton J, Davison R. Evaluation of performance of following Achilles tendon surgery in competitive runners. New Studies in Athletes. 1992;7:33-37. |
| 23. | Leach RE, Schepsis AA, Takai H. Long-term results of surgical management of Achilles tendinitis in runners. Clin Orthop Relat Res. 1992;208-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 17] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 24. | Leppilahti J, Karpakka J, Gorra A. Surgical treatment of overuse injuries to the Achilles tendon. Clin J Sport Med. 1994;4:100-107. [DOI] [Full Text] |
| 25. | Schepsis AA, Wagner C, Leach RE. Surgical management of Achilles tendon overuse injuries. A long-term follow-up study. Am J Sports Med. 1994;22:611-619. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 105] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 26. | Aström M, Rausing A. Chronic Achilles tendinopathy. A survey of surgical and histopathologic findings. Clin Orthop Relat Res. 1995;151-164. [PubMed] |
| 27. | Johnston E, Scranton P, Pfeffer GB. Chronic disorders of the Achilles tendon: results of conservative and surgical treatments. Foot Ankle Int. 1997;18:570-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 51] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 28. | Maffulli N, Testa V, Capasso G, Bifulco G, Binfield PM. Results of percutaneous longitudinal tenotomy for Achilles tendinopathy in middle- and long-distance runners. Am J Sports Med. 1997;25:835-840. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 112] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 29. | Morberg P, Jerre R, Swärd L, Karlsson J. Long-term results after surgical management of partial Achilles tendon ruptures. Scand J Med Sci Sports. 1997;7:299-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 30. | Alfredson H, Pietilä T, Ohberg L, Lorentzon R. Achilles tendinosis and calf muscle strength. The effect of short-term immobilization after surgical treatment. Am J Sports Med. 1998;26:166-171. [PubMed] |
| 31. | Maffulli N, Binfield PM, Moore D, King JB. Surgical decompression of chronic central core lesions of the Achilles tendon. Am J Sports Med. 1999;27:747-752. [PubMed] |
| 32. | Paavola M, Orava S, Leppilahti J, Kannus P, Järvinen M. Chronic Achilles tendon overuse injury: complications after surgical treatment. An analysis of 432 consecutive patients. Am J Sports Med. 2000;28:77-82. [PubMed] |
| 33. | Wilcox DK, Bohay DR, Anderson JG. Treatment of chronic achilles tendon disorders with flexor hallucis longus tendon transfer/augmentation. Foot Ankle Int. 2000;21:1004-1010. [PubMed] |
| 34. | Ohberg L, Lorentzon R, Alfredson H. Good clinical results but persisting side-to-side differences in calf muscle strength after surgical treatment of chronic Achilles tendinosis: a 5-year follow-up. Scand J Med Sci Sports. 2001;11:207-212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 35. | Shalabi A, Kristoffersen-Wiberg M, Aspelin P, Movin T. MR evaluation of chronic Achilles tendinosis. A longitudinal study of 15 patients preoperatively and two years postoperatively. Acta Radiol. 2001;42:269-276. [PubMed] |
| 36. | Maquirriain J, Ayerza M, Costa-Paz M, Muscolo DL. Endoscopic surgery in chronic achilles tendinopathies: A preliminary report. Arthroscopy. 2002;18:298-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 42] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 37. | Paavola M, Kannus P, Orava S, Pasanen M, Järvinen M. Surgical treatment for chronic Achilles tendinopathy: a prospective seven month follow up study. Br J Sports Med. 2002;36:178-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 65] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 38. | Shalabi A, Kristoffersen-Wiberg M, Papadogiannakis N, Aspelin P, Movin T. Dynamic contrast-enhanced mr imaging and histopathology in chronic achilles tendinosis. A longitudinal MR study of 15 patients. Acta Radiol. 2002;43:198-206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 39. | Yodlowski ML, Scheller AD, Minos L. Surgical treatment of Achilles tendinitis by decompression of the retrocalcaneal bursa and the superior calcaneal tuberosity. Am J Sports Med. 2002;30:318-321. [PubMed] |
| 40. | Chiara Vulpiani M, Guzzini M, Ferretti A. Operative treatment of chronic Achilles tendinopathy. Int Orthop. 2003;27:307-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 41. | Den Hartog BD. Flexor hallucis longus transfer for chronic Achilles tendonosis. Foot Ankle Int. 2003;24:233-237. [PubMed] |
| 42. | Saxena A. Results of chronic Achilles tendinopathy surgery on elite and nonelite track athletes. Foot Ankle Int. 2003;24:712-720. [PubMed] |
| 43. | Martin RL, Manning CM, Carcia CR, Conti SF. An outcome study of chronic Achilles tendinosis after excision of the Achilles tendon and flexor hallucis longus tendon transfer. Foot Ankle Int. 2005;26:691-697. [PubMed] |
| 44. | Costa ML, Donell ST, Tucker K. The long-term outcome of tendon lengthening for chronic Achilles tendon pain. Foot Ankle Int. 2006;27:672-676. [PubMed] |
| 45. | Johnson KW, Zalavras C, Thordarson DB. Surgical management of insertional calcific achilles tendinosis with a central tendon splitting approach. Foot Ankle Int. 2006;27:245-250. [PubMed] |
| 46. | Maffulli N, Testa V, Capasso G, Oliva F, Sullo A, Benazzo F, Regine R, King JB. Surgery for chronic Achilles tendinopathy yields worse results in nonathletic patients. Clin J Sport Med. 2006;16:123-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 53] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 47. | Wagner E, Gould JS, Kneidel M, Fleisig GS, Fowler R. Technique and results of Achilles tendon detachment and reconstruction for insertional Achilles tendinosis. Foot Ankle Int. 2006;27:677-684. [PubMed] |
| 48. | Cottom JM, Hyer CF, Berlet GC, Lee TH. Flexor hallucis tendon transfer with an interference screw for chronic Achilles tendinosis: a report of 62 cases. Foot Ankle Spec. 2008;1:280-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 37] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 49. | Hahn F, Meyer P, Maiwald C, Zanetti M, Vienne P. Treatment of chronic achilles tendinopathy and ruptures with flexor hallucis tendon transfer: clinical outcome and MRI findings. Foot Ankle Int. 2008;29:794-802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 102] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 50. | Maffulli N, Testa V, Capasso G, Oliva F, Panni AS, Longo UG, King JB. Surgery for chronic Achilles tendinopathy produces worse results in women. Disabil Rehabil. 2008;30:1714-1720. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 51. | Vega J, Cabestany JM, Golanó P, Pérez-Carro L. Endoscopic treatment for chronic Achilles tendinopathy. Foot Ankle Surg. 2008;14:204-210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 28] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 52. | Bohu Y, Lefèvre N, Bauer T, Laffenetre O, Herman S, Thaunat M, Cucurulo T, Franceschi JP, Cermolacce C, Rolland E. Surgical treatment of Achilles tendinopathies in athletes. Multicenter retrospective series of open surgery and endoscopic techniques. Orthop Traumatol Surg Res. 2009;95:S72-S77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 53. | Thermann H, Benetos IS, Panelli C, Gavriilidis I, Feil S. Endoscopic treatment of chronic mid-portion Achilles tendinopathy: novel technique with short-term results. Knee Surg Sports Traumatol Arthrosc. 2009;17:1264-1269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 34] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 54. | Will RE, Galey SM. Outcome of single incision flexor hallucis longus transfer for chronic achilles tendinopathy. Foot Ankle Int. 2009;30:315-317. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 31] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 55. | Duthon VB, Lübbeke A, Duc SR, Stern R, Assal M. Noninsertional Achilles tendinopathy treated with gastrocnemius lengthening. Foot Ankle Int. 2011;32:375-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 71] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 56. | van Sterkenburg MN, Kerkhoffs GM, van Dijk CN. Good outcome after stripping the plantaris tendon in patients with chronic mid-portion Achilles tendinopathy. Knee Surg Sports Traumatol Arthrosc. 2011;19:1362-1366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 57. | Maffulli N, Del Buono A, Testa V, Capasso G, Oliva F, Denaro V. Safety and outcome of surgical debridement of insertional Achilles tendinopathy using a transverse (Cincinnati) incision. J Bone Joint Surg Br. 2011;93:1503-1507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 58. | Sarimo J, Orava S. Fascial incision and adhesiolysis combined with radiofrequency microtenotomy in treatment of chronic midportion Achilles tendinopathy. Scand J Surg. 2011;100:125-128. [PubMed] |
| 59. | Oshri Y, Palmanovich E, Brin YS, Karpf R, Massarwe S, Kish B, Nyska M. Chronic insertional Achilles tendinopathy: surgical outcomes. Muscles Ligaments Tendons J. 2012;2:91-95. [PubMed] |
| 60. | Kiewiet NJ, Holthusen SM, Bohay DR, Anderson JG. Gastrocnemius recession for chronic noninsertional Achilles tendinopathy. Foot Ankle Int. 2013;34:481-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 61. | Maffulli N, Oliva F, Testa V, Capasso G, Del Buono A. Multiple percutaneous longitudinal tenotomies for chronic Achilles tendinopathy in runners: a long-term study. Am J Sports Med. 2013;41:2151-2157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 62. | Maquirriain J. Surgical treatment of chronic achilles tendinopathy: long-term results of the endoscopic technique. J Foot Ankle Surg. 2013;52:451-455. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 33] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 63. | Benazzo F, Zanon G, Klersy C, Marullo M. Open surgical treatment for chronic midportion Achilles tendinopathy: faster recovery with the soleus fibres transfer technique. Knee Surg Sports Traumatol Arthrosc. 2014;Sep 6; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 64. | Tallerico VK, Greenhagen RM, Lowery C. Isolated Gastrocnemius Recession for Treatment of Insertional Achilles Tendinopathy: A Pilot Study. Foot Ankle Spec. 2014;Nov 10; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 65. | Maffulli N, Del Buono A. Release of the medial head of the gastrocnemius for Achilles tendinopathy in sedentary patients: a retrospective study. Int Orthop. 2015;39:61-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 66. | Nawoczenski DA, Barske H, Tome J, Dawson LK, Zlotnicki JP, DiGiovanni BF. Isolated gastrocnemius recession for achilles tendinopathy: strength and functional outcomes. J Bone Joint Surg Am. 2015;97:99-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 40] [Article Influence: 4.0] [Reference Citation Analysis (0)] |