Published online Dec 18, 2015. doi: 10.5312/wjo.v6.i11.983
Peer-review started: May 30, 2015
First decision: July 30, 2015
Revised: August 4, 2015
Accepted: September 29, 2015
Article in press: September 30, 2015
Published online: December 18, 2015
Processing time: 201 Days and 22.8 Hours
AIM: To describe initial results and experimental error measurement of a protocol analyzing Human posture through sagittal intersegmental moments.
METHODS: Postural analysis has been recently improved by development of three-dimensional radiographic imaging systems. However, in various situations such as global sagittal anterior malalignment interpretation of radiographs may not represent the real alignment of the subject. The aim of this study was to present initial results of a 3D biomechanical protocol. This protocol is obtained in a free standing position and characterizes postural balance by measurement of sagittal intersegmental net moments. After elaboration of a specific marker-set, 4 successive recordings were done on two volunteers by three different operators during three sessions in order to evaluate the experimental error measurement. A supplementary acquisition in a “radiographic” posture was also obtained. Once the data acquired, joint center, length, anatomical frame and the center of mass of each body segment was calculated and a mass affected. Sagittal net intersegmental moments were computed in an ascending manner from ground reaction forces at the ankles, knees, hips and the lumbo-sacral and thoraco-lumbar spinal junctions. Cervico-thoracic net intersegmental moment was calculated in a descending manner.
RESULTS: Based on average recordings, clinical interpretation of net intersegmental moments (in N.m) showed a dorsal flexion on the ankles (8.6 N.m), a flexion on the knees (7.5 N.m) and an extension on the hips (8.5 N.m). On the spinal junctions, it was flexion moments: 0.34 N.m on the cervico-thoracic; 6.7 N.m on the thoraco-lumbar and 0.65 N.m on the lumbo-sacral. Evaluation of experimental error measurement showed a small inter-trial error (intrinsic variability), with higher inter-session and inter-therapist errors but without important variation between them. For one volunteer the “radiographic” posture was associated to significant changes compared to the free standing position.
CONCLUSION: These initial results confirm the technical feasibility of the protocol. The low intrinsic error and the small differences between inter-session and inter-therapist errors seem to traduce postural variability over time, more than a failure of the protocol. Characterization of sagittal intersegmental net moments can have clinical applications such as evaluation of an unfused segment after a spinal arthrodesis.
Core tip: Postural evaluation is commonly performed using full-spine radiographs. However, a biomechanical approach using a dedicated protocol is possible in order to evaluate sagittal intersegmental net moments. Results from this study confirmed the technical feasibility of the protocol. Furthermore, these results revealed postural variability over time. Such evaluation may have various clinical applications such as evaluation of an unfused segment after a spinal arthrodesis.
- Citation: Blondel B, Viehweger E, Moal B, Tropiano P, Jouve JL, Lafage V, Dumas R, Fuentes S, Bollini G, Pomero V. Postural spinal balance defined by net intersegmental moments: Results of a biomechanical approach and experimental errors measurement. World J Orthop 2015; 6(11): 983-990
- URL: https://www.wjgnet.com/2218-5836/full/v6/i11/983.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i11.983
The clinical relevance of sagittal plane spino-pelvic parameters has continuously been demonstrated since their description by Duval-Beaupère et al[1] and Legaye et al[2] and multiple outcomes-related studies have reported correlations between sagittal radiographic parameters and Health Related Quality of Life scores pre or postoperatively[3-5]. These reports demonstrated that sagittal vertical axis (SVA, defined by the offset between the C7 plumb-line and the postero-superior corner of S1), Pelvic Tilt (PT, defined as the angle between a line drawn from the center of the femoral heads to the midpoint of the sacrum and the vertical), and more recently Pelvic Incidence minus Lumbar Lordosis (reflecting spino-pelvic harmony) are the 3 most important parameters due to their correlation with clinical outcomes for patients with spinal deformities[6,7]. With the exception of the pelvic incidence, those parameters are not fixed and are affected by the aging process of the spine where an increase of the thoracic kyphosis is usually associated with a pelvic retroversion (increased PT) and a loss of lumbar lordosis acting as compensatory mechanisms to maintain the head over the pelvis; then finally leading to a positive SVA[7]. This chain of correlation is also visible in patients with spinal deformities leading to a progressive anterior malalignment associated with an increased disability[6].
Most of the work accomplished so far in this domain is based on plain radiograph. Despite recent advancements, there are limitations to biplanar radiographic acquisitions and significant differences have been reported between bi-dimensional and three-dimensional postural analyses[8,9]. Furthermore, while posture is a dynamic condition with constant reciprocal interactions in an effort to maintain the head over the pelvis, radiograph only represents a snapshot of posture and therefore can lead to misinterpretation of sagittal alignment[10,11]. This last point is especially important for patients with an anterior malalignment who will adopt an “artificial” posture during radiographic exam in order to “fit” into the cassette footprint. In the context, it appears evident that there is a need for new evaluation tools for postural analysis independent from radiographs.
The aim of this study is to report the experimental error measurement and the impact of the radiographic posture from a protocol characterizing the net inter-segmental moments which occurs at the center of musculo-skeletal joints during a free standing posture.
After informed consent, two healthy adult volunteers were recruited for this pilot study. Both volunteers had no previous history of back pain, any known spinal disorder or previous back surgery.
The protocol used for this study was based on a set of markers that could be used to calculate the center of mass of pre-defined segments, previously published[12] and summarized hereafter. Based on published reports[13-15], a set of 36 markers was used to divide the body in 10 segments (head, thorax, abdomen, pelvis, thighs, legs and feet): 4 markers were placed on the head, 8 on the thorax, 1 on the abdomen, 3 on the pelvis, 4 on each thigh, 4 on each leg and 3 on each foot. Among these 36 markers, the spine was described using 6 markers allowing a description of thoracic and lumbar curvatures (C7, T6, T8, T12, L3 and S1).
This set of markers was defined in order to be able to localize the centers of mass of each body segment using easily recognizable anatomical landmarks, then using anthropometric tables and the height/weight of the subject, a mass was attributed to each segment according to Dumas et al[13].
Once equipped, each volunteer was asked to adopt a free standing position (with horizontal gaze) without external constraint or support, with shoulders flexed at 30° and fingers tips on zygomatic processes (i.e., the “radiographic” posture). The location of the markers over time were recorded using a Vicon® (Vicon, Oxford, United Kingdom) optoelectronic system with 6 high resolution infrared cameras and a 100Hz sampling frequency.
Each foot was positioned over a forceplate (AMTI, United States) in order to collect the ground reaction force of the subject. The sagittal net intersegmental moments (ankles, knees, hips, hip-pelvis complex, lumbosacral junction, thoraco-lumbar junction and cervico-thoracic junction) were calculated in an ascending manner (i.e., going upward from the ground reaction forces) between each body segment previously identified except for the cervico-thoracic junction where the sagittal net intersegmental moment was calculated using a descending manner from the center of mass and mass of the head and neck.
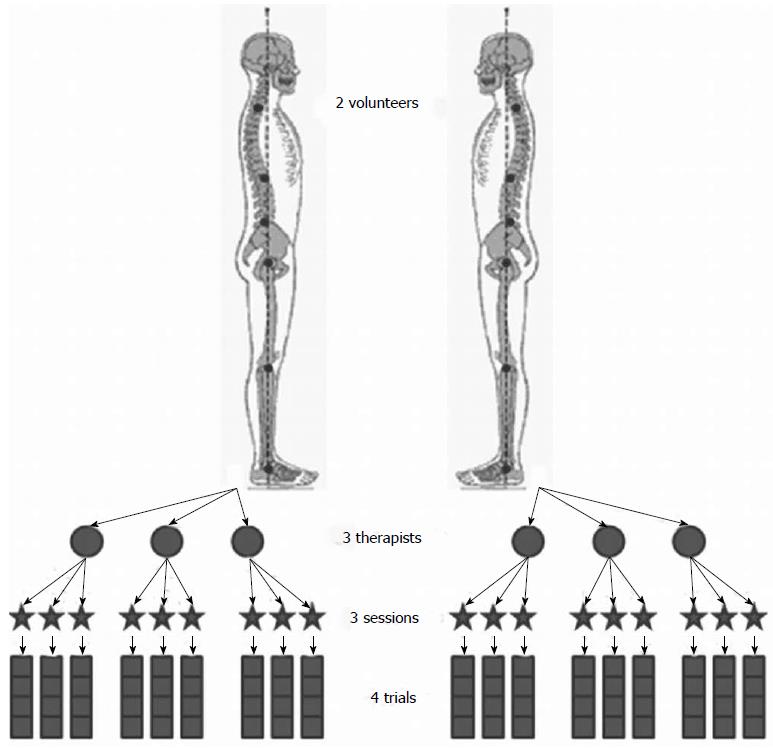
In order to estimate experimental errors of this protocol, measurements were repeated according to the experimental design described by Schwartz et al[16]. Postural data from the two volunteers were acquired by three trained therapists, during three different sessions with one week interval (Figure 1). During each session, the volunteer was asked to stand 4 times in a free standing position with each foot on a force platform (with a free walk between each trial), without modifications of the markers, and postural data were recorded during several seconds, then “radiographic” posture was recorded one time. Between each therapist evaluation, markers were all removed and the volunteer was equipped again.
Finally, changes in spinal net intersegmental moments were calculated during a trunk flexion/extension for one volunteer.
Analysis of the acquired data was conducted on a one-second record sample, with the less body sway, in order to calculate mean and maximum net reaction moments in the sagittal plane at each joint center, with an evaluation of the intra-subject, the intra-observer (inter-session) and inter-observer (inter-therapist) variability according to Schwartz’s methodology[16]. Analysis between free standing and “radiographic” posture was done by comparison of mean spinal net moments for each volunteer and a significant difference was defined as a difference superior to the experimental error measure.
Results of estimated moments were interpreted using the convention as follows: Positives values were associated to extension moments on spinal junctions and knees, to dorsal flexion of the ankles and pelvic retroversion. Negatives values were associated to flexion moments on spinal junctions and knees, to plantar flexion of the ankles and pelvic anteversion.
The first volunteer was a 30-year-old male, 180 cm in height and 80 kg in weight. The second volunteer was a 26-year-old female, 158 cm in height and 52 kg in weight.
Results from analysis on the 2 volunteers revealed similar orientation of net sagittal moments on each joint (Table 1). Based on all the recordings acquired from the two volunteers, it was possible to estimate mean net intersegmental moments as follows: (1) A mean dorsal flexion moment of -10.4 N.m on the right ankle and -6.8 N.m on the left; (2) A mean moment of -7.15 N.m on the right knee and -7.95 N.m on the left; (3) A mean moment of 7.26 N.m on the right hip and 9.72 N.m on the left; and (4) On the spinal junctions: a mean moment of -0.65 N.m at the lumbosacral junction, -6.72 N.m at the thoracolumbar junction and -0.34 N.m at the cervicothoracic junction. Detailed results for each volunteer are summarized in Table 1.
| Cervical | Thoracic | Lumbar | Hip right | Hip left | Knee right | Knee left | Ankle right | Ankle left | ||
| Mean | Volunteer 1 | -0.65 | -9.23 | -0.45 | 10.73 | 14.62 | -6.7 | -5.81 | -13.04 | -7.52 |
| moments | Volunteer 2 | -0.03 | -4.2 | -0.86 | 3.79 | 4.82 | -7.59 | -10.09 | -7.76 | -6.08 |
| Max | Volunteer 1 | 0.71 | 10.76 | 7.71 | 11.35 | 15.2 | 7.6 | 7.59 | 14.06 | 8.59 |
| moments | Volunteer 2 | 0.43 | 5.92 | 3.91 | 4.27 | 5.08 | 8.12 | 10.44 | 8.5 | 6.49 |
According to the convention described in this protocol, the clinical interpretation of the net intersegmental moments applied on the different joints was: ankle dorsal flexion, knee flexion, hip extension (pelvic retroversion) and a flexion at the different spinal junctions. In other words, in order to maintain a free standing posture muscular system will have to generate an ankle plantar flexion, a knee extension, a pelvic anteversion and a spinal extension.
As per the methodology described by Schwartz, the following experimental errors were calculated: inter-trial errors (intrinsic error corresponding to the intra-subject variability), the inter-session errors (extrinsic error related to intra-observer variability) and the inter-therapist errors (extrinsic error related to inter-observer variability). Results from these analyses are summarized in Table 2.
| Cervical | Thoracic | Lumbar | Hip right | Hip left | Knee right | Knee left | Ankle right | Ankle left | |
| Inter-trial error | 0.26 | 1.36 | 1.08 | 1.66 | 1.71 | 1.55 | 1.5 | 2.14 | 2.03 |
| Inter-session error | 0.43 | 5.27 | 5.24 | 3.21 | 3.78 | 2.09 | 2.75 | 2.46 | 2.8 |
| Inter-therapist error | 0.48 | 6.68 | 6.64 | 4.09 | 4.5 | 4.22 | 4.07 | 2.6 | 2.86 |
In order to quantify the effect of an imposed posture, the net intersegmental moments at the spinal junctions during the “radiographic posture” were compared to the one obtained during the “free posture”. Change was considered significant only if the difference was greater than the intrinsic experimental error calculated for each junction. Results from these analyses did not showed significant differences for volunteer 2. Significant variations were observed on volunteer 1 mainly on the intra-subject measurement. Adopting a “radiographic” posture led to the following changes: an extension moment at the cervico-thoracic level, a decrease of the flexion moment at the thoraco-lumbar level and no significant change on the moment at the lumbo-sacral level. Results are summarized in Table 3.
| Cervical | Thoracic | Lumbar | ||
| Volunteer 1 | Mean Diff FSP vs RX (N/m) | 1.15 | 2.79 | 0.35 |
| Inter-trial significant diff | Yes | Yes | No | |
| Inter-session significant diff | Yes | No | No | |
| Inter-therapist significant diff | Yes | No | No | |
| Volunteer 2 | Mean Diff FSP vs RX (N/m) | 0.11 | 0.88 | 0.3 |
| Inter-trial significant diff | No | No | No | |
| Inter-session significant diff | No | No | No | |
| Inter-therapist significant diff | No | No | No | |
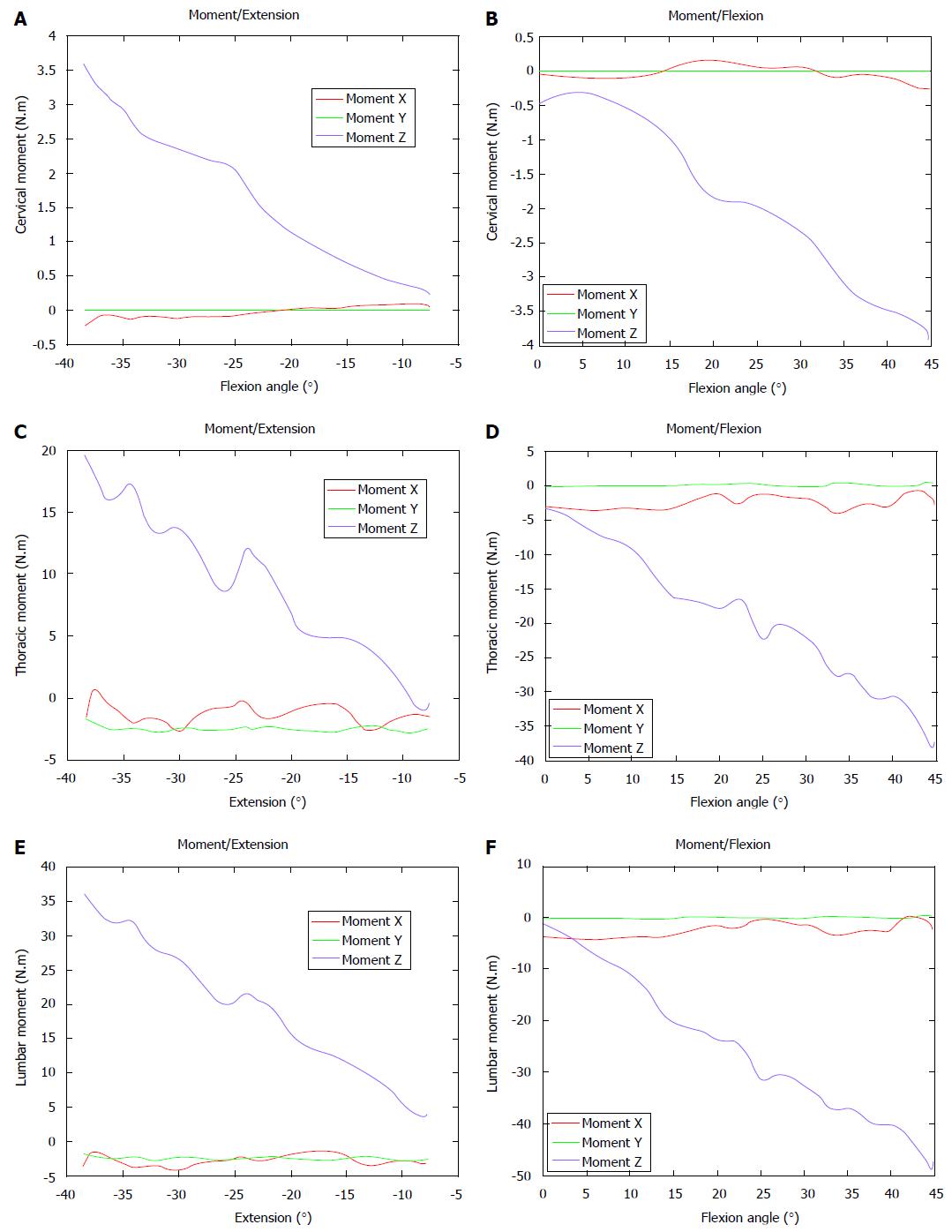
From the free standing position to an anterior flexion of the trunk at 45°, recordings demonstrated a progressively increased flexion moment (in absolute values) on the cervico-thoracic (> 3.5 N.m), the thoraco-lumbar (> 35 N.m) and the lumbo-sacral junctions (> 45 N.m).
During trunk extension (around 40°) recordings demonstrated changes towards extension moments on the cervico-thoracic (> 3.5 N.m), the thoraco-lumbar (> 18 N.m) and the lumbo-sacral junctions (> 35 N.m). These results are summarized in Figure 2.
Sagittal spino-pelvic parameters have been reported as of primary importance in the management of spinal deformities due to their correlation with clinical and functional outcomes in preoperative and postoperative evaluations[6,7,17,18]. More recently, those findings were revisited in order to define guidelines in realignment objectives[19]. Given the constrain of a radiographic environment (i.e., arms positioning), several authors demonstrated that the “radiographic” posture could lead to postural modifications[10,11] and therefore to subsequent alignment misinterpretation, especially for patients with a marked sagittal anterior malalignment.
Our objective was to propose a new protocol focusing on the calculation of resulting intersegmental moments during a free standing posture (i.e., without constrain of the radiographic environment) and to evaluate the experimental error of the protocol.
Results from this study confirm the feasibility of the proposed protocol for postural analysis and provide preliminary values of the resulting net sagittal moments on various articulations during normal stance. In a free standing position, net flexion moments calculated at each spinal junction correspond to the impact of the body weight. Therefore, in order to stand in an upright position, these moments have to be compensated by the action of posterior muscles. Muscular role is crucial in order to maintain a satisfactory posture and Mahaudens et al[20], demonstrated, in an energy-cost analysis, the impact of poor muscle efficiency on gait for adolescent with idiopathic scoliosis (AIS). Previous studies have already analyzed spinal alignment and posture using gait analysis but, to our best knowledge, characterization of posture with net sagittal moments has never been reported yet. Chen et al[21] reported poor postural stability control in AIS patients, without modifications of gait patterns in comparison with normal subjects. More recently, Engsberg et al[22] and Lenke et al[23] analyzed posture and trunk range of motion in AIS patients, post-operatively; they found a reduced gait speed, an improved coronal balance, but unchanged sagittal balance and a reduced range of motion in fused and unfused spinal segments. Using the protocol described in this study could provide further steps in the comprehension of the net reaction moment which occurs below or above a fused segment or evaluate an adjacent level degeneration.
Measurement of the experimental error was done according to Schwartz et al[16], and as for these authors, in our protocol the inter-trial error was the smallest, with higher inter-session and inter-therapist errors. This increased measurement error can be considered in different ways: it can be related to a lack of reliability of the protocol or can reflect the postural variability. Results from trunk flexion/extension moments showing a linear relation between trunk flexion/extension and moments, as well as the small differences between errors from inter-session and inter-therapist measurements are more likely to reveal changes in posture. Furthermore, differences found between the free-standing posture and the “radiographic” posture provides an additional argument in favor of a postural variability rather than a protocol failure.
Results from the analysis comparing the free standing and the “radiographic” posture revealed differences superior to the intrinsic experimental error for the volunteer 1 and no significant changes were visible for the volunteer 2, underlining the variability of posture with time and among individual. Clinical expressions of these changes were associated with an extension of the upper part of the trunk when the volunteer adopted the “radiographic” posture. These results are in line with previous reports[10,11] where arms positioning could be associated to negative shift of the SVA. Furthermore, this test was conducted in volunteer without sagittal malalignment and these differences may be even much more noticeable in patients with loss of lumbar lordosis and increased thoracic kyphosis.
Results from this study confirm the technical feasibility of the protocol. Using this methodology, it was possible to evaluate net moments applied to spinal junctions. Measurements of experimental errors showed differences between inter-trial, inter-session and inter-therapist recordings traducing variability of posture. Differences were also noted between free standing and “radiographic” posture. Further steps will be needed in order to include a larger sample of volunteers for description of normative values and to determine sagittal parameters from this protocol that can be associated with conventional radiographic parameters. Future development of this protocol can help to evaluate various clinical situations such as adjacent level degeneration or modification of forces applied on unfused segment after spinal surgery.
In clinical practice, postural analysis is mainly based on radiographs. However, in various situations such as global sagittal anterior malalignment interpretation of radiographs may not represent the real alignment of the subject.
Biomechanical analysis can currently be applied to postural analysis. Such development will help to understand spinal disorders and impact of surgical procedures on posture.
Results from this study confirm the technical feasibility of the protocol. Using this methodology, it was possible to evaluate net moments applied to spinal junctions. Differences were also noted between free standing and “radiographic” posture. Future development of this protocol can help to evaluate various clinical situations such as adjacent level degeneration or modification of forces applied on unfused segment after spinal surgery.
Future development of this protocol can help to evaluate various clinical situations such as adjacent level degeneration or modification of forces applied on unfused segment after spinal surgery.
In this biomechanical study the authors describe the initial results and experimental error measurement of a protocol analyzing human posture through sagittal intersegmental moments. After elaboration of a specific marker-set, 4 successive recordings were done on two volunteers by three different operators during three sessions in order to evaluate the experimental error measurement. A supplementary acquisition in a “radiographic” posture was also obtained. And these authors concluded that the first results confirm the technical feasibility of the protocol while the characterization of sagittal intersegmental net moments can have clinical applications such as evaluation of an unfused segment after a spinal arthrodesis.
P- Reviewer: Korovessis P, Sun J S- Editor: Tian YL L- Editor: A E- Editor: Jiao XK
| 1. | Duval-Beaupère G, Schmidt C, Cosson P. A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng. 1992;20:451-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 584] [Cited by in RCA: 550] [Article Influence: 16.7] [Reference Citation Analysis (0)] |
| 2. | Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1206] [Cited by in RCA: 1189] [Article Influence: 44.0] [Reference Citation Analysis (0)] |
| 3. | Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976). 2005;30:682-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 868] [Cited by in RCA: 917] [Article Influence: 45.9] [Reference Citation Analysis (0)] |
| 4. | Rose PS, Bridwell KH, Lenke LG, Cronen GA, Mulconrey DS, Buchowski JM, Kim YJ. Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine (Phila Pa 1976). 2009;34:785-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 237] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 5. | Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976). 2009;34:1828-1833. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 518] [Cited by in RCA: 548] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 6. | Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005;30:2024-2029. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1286] [Cited by in RCA: 1350] [Article Influence: 67.5] [Reference Citation Analysis (0)] |
| 7. | Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976). 2009;34:E599-E606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 798] [Cited by in RCA: 829] [Article Influence: 51.8] [Reference Citation Analysis (0)] |
| 8. | Gangnet N, Dumas R, Pomero V, Mitulescu A, Skalli W, Vital JM. Three-dimensional spinal and pelvic alignment in an asymptomatic population. Spine (Phila Pa 1976). 2006;31:E507-E512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 39] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 9. | Gangnet N, Pomero V, Dumas R, Skalli W, Vital JM. Variability of the spine and pelvis location with respect to the gravity line: a three-dimensional stereoradiographic study using a force platform. Surg Radiol Anat. 2003;25:424-433. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 78] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Marks MC, Stanford CF, Mahar AT, Newton PO. Standing lateral radiographic positioning does not represent customary standing balance. Spine (Phila Pa 1976). 2003;28:1176-1182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 52] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Vedantam R, Lenke LG, Bridwell KH, Linville DL, Blanke K. The effect of variation in arm position on sagittal spinal alignment. Spine (Phila Pa 1976). 2000;25:2204-2209. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 83] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Blondel B, Pomero V, Moal B, Lafage V, Jouve JL, Tropiano P, Bollini G, Dumas R, Viehweger E. Sagittal spine posture assessment: feasibility of a protocol based on intersegmental moments. Orthop Traumatol Surg Res. 2012;98:109-113. [PubMed] |
| 13. | Dumas R, Chèze L, Verriest JP. Adjustments to McConville et al. and Young et al. body segment inertial parameters. J Biomech. 2007;40:543-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 334] [Cited by in RCA: 276] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 14. | Wu G, Siegler S, Allard P, Kirtley C, Leardini A, Rosenbaum D, Whittle M, D’Lima DD, Cristofolini L, Witte H. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion--part I: ankle, hip, and spine. International Society of Biomechanics. J Biomech. 2002;35:543-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2049] [Cited by in RCA: 2125] [Article Influence: 92.4] [Reference Citation Analysis (0)] |
| 15. | Wu G, van der Helm FC, Veeger HE, Makhsous M, Van Roy P, Anglin C, Nagels J, Karduna AR, McQuade K, Wang X. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion--Part II: shoulder, elbow, wrist and hand. J Biomech. 2005;38:981-992. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2387] [Cited by in RCA: 2527] [Article Influence: 126.4] [Reference Citation Analysis (0)] |
| 16. | Schwartz MH, Trost JP, Wervey RA. Measurement and management of errors in quantitative gait data. Gait Posture. 2004;20:196-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 271] [Cited by in RCA: 252] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 17. | Hyun SJ, Rhim SC. Clinical outcomes and complications after pedicle subtraction osteotomy for fixed sagittal imbalance patients: a long-term follow-up data. J Korean Neurosurg Soc. 2010;47:95-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 141] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 18. | Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Sagittal thoracic decompensation following long adult lumbar spinal instrumentation and fusion to L5 or S1: causes, prevalence, and risk factor analysis. Spine (Phila Pa 1976). 2006;31:2359-2366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 99] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 19. | Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 2010;35:2224-2231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 733] [Cited by in RCA: 819] [Article Influence: 54.6] [Reference Citation Analysis (0)] |
| 20. | Mahaudens P, Detrembleur C, Mousny M, Banse X. Gait in adolescent idiopathic scoliosis: energy cost analysis. Eur Spine J. 2009;18:1160-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 53] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 21. | Chen PQ, Wang JL, Tsuang YH, Liao TL, Huang PI, Hang YS. The postural stability control and gait pattern of idiopathic scoliosis adolescents. Clin Biomech (Bristol, Avon). 1998;13:S52-S58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 94] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 22. | Engsberg JR, Lenke LG, Reitenbach AK, Hollander KW, Bridwell KH, Blanke K. Prospective evaluation of trunk range of motion in adolescents with idiopathic scoliosis undergoing spinal fusion surgery. Spine (Phila Pa 1976). 2002;27:1346-1354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 70] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 23. | Lenke LG, Engsberg JR, Ross SA, Reitenbach A, Blanke K, Bridwell KH. Prospective dynamic functional evaluation of gait and spinal balance following spinal fusion in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2001;26:E330-E337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 64] [Article Influence: 2.7] [Reference Citation Analysis (0)] |