Published online Dec 18, 2015. doi: 10.5312/wjo.v6.i11.954
Peer-review started: May 18, 2015
First decision: June 24, 2015
Revised: September 25, 2015
Accepted: October 23, 2015
Article in press: October 27, 2015
Published online: December 18, 2015
Processing time: 220 Days and 3.4 Hours
Fracture of the radial head is a common injury. Over the last decades, the radial head is increasingly recognized as an important stabilizer of the elbow. In order to maintain stability of the injured elbow, goals of treatment of radial head fractures have become more and more towards restoring function and stability of the elbow. As treatment strategies have changed over the years, with an increasing amount of literature on this subject, the purpose of this article was to provide an overview of current concepts of the management of radial head fractures.
Core tip: The radial head is one of the most debated subjects of the elbow. As treatment strategies have changed over the years, with an increasing amount of literature on this subject, the purpose of this article was to provide an overview of current concepts of the management of radial head fractures.
- Citation: Kodde IF, Kaas L, Flipsen M, Bekerom MPVD, Eygendaal D. Current concepts in the management of radial head fractures. World J Orthop 2015; 6(11): 954-960
- URL: https://www.wjgnet.com/2218-5836/full/v6/i11/954.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i11.954
Fractures of the radial head are the most common fractures in the elbow[1]. Although it has been 80 years since one of the first reports on radial head fractures was published in the New England Journal of Medicine; the radial head is still a topic for debate in the orthopedic and trauma literature[2]. Over the last decades, the radial head is increasingly recognized as an important stabilizer of the elbow[3,4]. In order to maintain stability of the injured elbow, the main goal in the treatment of radial head fractures is to restore the anatomy of the radial head and surrounding tissues. The purpose of this article was to discuss current aspects in the etiology and management of radial head fractures in adults.
Fractures of the radial head are common, with an estimated incidence of 2.5 to 2.8 per 10000 inhabitants per year. They account for approximately one-third of all elbow fractures. The mean age of patients that sustain a radial head fracture varies between 44 to 47.9 years[5-7]. Male-female ratios vary between 1:1, 2:3 and 3:2[1,6,8,9]. Female patients are significantly older compared to male patients (37-41 years vs 48-54 years)[6,7]. The peak incidence in men is between the age of 30 and 40 years and in women it is between 50 and 60 years[6]. Once the age rises above 50 years, the number of female patients with a radial head fracture is significantly larger than the number of male patients[6]. This typical distribution can be explained by a correlation with the presence of osteoporosis in female patients above the age of 50 years and higher energy trauma in young males[10].
The radial head is an important secondary stabilizer in valgus and external rotation. The issue of the individual contributions of the radial head and soft-tissue stabilizers of the elbow is very complex. Several biomechanical studies have been conducted to quantify elbow stability for simulated fractures, radial head excision, and radial head replacement, with and without the integrity of the collateral ligaments[3,11].
Radial head excision alters the kinematics and varus-valgus laxity of the elbow with intact ligaments and that stability is improved after radial head arthroplasty[11-13]. Also an increase in external rotation of the ulna with respect to the humerus during passive motion with the forearm in supination was observed after radial head excision when both ligaments were intact[12].
A significant decrease in elbow stability was noted if the radial head was excised in elbows with an associated disruption of the lateral collateral ligament (LCL). Elbow laxity was improved following radial head arthroplasty; however, these elbows were still unstable relative to those with intact ligaments[12]. These findings suggest that repair of the disrupted LCL complex is essential in order to restore elbow stability following open reduction and internal fixation (ORIF) of the radial head or radial head arthroplasty.
Pomianowski et al[14] reported that laxity was increased after radial head excision in elbows with disruption of the medial collateral ligament (MCL). Radial head arthroplasty restores valgus stability in elbows with disruption of the MCL to a state similar to that seen in elbows with a native radial head[14,15]. Other studies observed an improved but not normal stability after radial head arthroplasty with MCL insufficiency[12,16]. However, the amount of instability was very small, possibly because of the stabilizing effect of the biceps and brachialis.
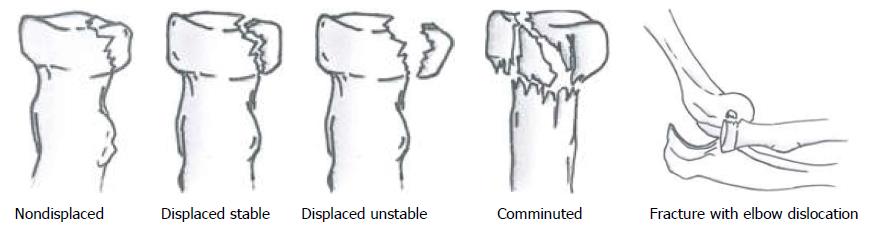
Mason[1] observed, back in 1954, the fracture patterns of the radial head in 100 patients and divided them in three groups. Mason Type I fractures (73%) of the radial head involved fractures without displacement, type II fractures (19%) were marginal sector fractures with displacement, and type III fractures (8%) were comminuted[17]. In 1962, Johnston[18] added fractures of the radial head that were associated with a dislocation of the elbow, as a type IV to the system. Subsequently, Broberg and Morrey[19] and Hotchkiss[20] further quantified the amount of dislocation for type II fractures. More recently, Rineer et al[21] suggested that the stability of the fracture can be determined based on the detail whether there was cortical contact between the fragments, or not. The various classifications are summarized in Table 1 and Figure 1. The interobserver agreement for diagnosing a 2 mm gap (κ = 0.55) or cortical contact (κ = 0.43) on standard radiographs was moderate[22]. Two- or three-dimensional computed tomography (CT) scans improved sensitivity for diagnosis in another study, though the interobserver agreement was still only moderate for most fracture characteristics[23]. Potential benefit of CT reconstructions is to determine the location of the fracture in the radial head (most commonly anterolateral quadrant with the forearm in neutral position), which may be associated with change on associated injuries and elbow instability[24,25].
| Description of classification according to various authors | |||||
| Type | Mason | Johnston | Hotchkiss | Broberg and Morrey | Rineer |
| I | Without displacement | Without displacement | < 2 mm dislocation | < 2 mm dislocation | |
| II | With displacement | With displacement | > 2 mm dislocation | > 2-3 mm dislocation and involves > 30% of radial head | Cortical contact between fragments |
| > stable | |||||
| No cortical contact between fragments | |||||
| > unstable | |||||
| III | Comminuted | Comminuted | Comminuted | Comminuted | |
| IV | - | Fracture associated with dislocation of the elbow | Fracture associated with dislocation of the elbow | ||
When treating patients with a fracture of the radial head, special attention has to be given to the detection and treatment of associated injuries of the injured extremity. van Riet et al[7] found an incidence of associated injures in 39% in a retrospective evaluation of 333 patients with a radial head fracture. Loss of cortical contact and comminution of the radial head fracture are strongly related to a high incidence of associated injuries[7,21]. Associated injuries as ligamentous injuries, or bone bruise of the capitellum can be found using magnetic resonance imaging (MRI) in 76% to 96% of the patients with a radial head fracture[26,27]. In 9 of 14 patients with a Mason type I radial head fracture Hausmann et al[28] found partial lesions of the interosseous membrane (IOM) with MRI. Seven of these patients reported pain in the region on the distal IOM[28]. On the other hand, McGinley et al[29] only found incomplete or complete tears of the IOM in 5 patients with a Mason type II or III radial head fracture, the IOM was intact in all 13 patients with a Mason type I fracture[29]. Overall, the clinical relevance of associated injuries found with MRI is likely to be limited[30].
Using MRI in 61% to 80% of the patients with a radial head fracture ligamentous injuries are seen; although these findings were not always clinically relevant[30]. Persistent symptoms after LCL injuries were seen in 11% of the patients with a radial head fracture, and in 1.5% of the patients with a MCL lesion. Lesions of both the MCL and LCL are found in 6%[7]. Ligamentous injuries of the elbow occur as the radial head fractures with the elbow in flexion and pronation with the hand fixed on the ground. As a result of the forced supination of the forearm the LCL ruptures when the body rotates internally on the elbow under axial compression. A posterolateral dislocation with or without rupture of the MCL can occur if rotational and axial forces continue. Also as a result of a valgus moment the MCL can rupture[31,32].
Posterolateral dislocation of the elbow accompanies 3% to 14% of radial head fractures and can occur after a fall on the (nearly) extended arm[6,7]. In the trauma mechanism as mentioned above, the coronoid process is forced under the trochlea of the humerus and can cause a shear fracture. The combination of an elbow dislocation, radial head fracture and coronoid fracture is called “the terrible triad of the elbow”. Severe elbow instability and many post-traumatic complications are associated with this terrible triad[33].
Ulnar fractures occur in 1.2% to 12% of the patients with a radial head fracture[6,7]. This includes the Monteggia lesion, which is a radial head dislocation in combination with a fracture of the distal one third of the ulna[34]. The trauma mechanism is a fall on the outstretched arm with the forearm in hyperpronation. A dislocation of the fractured radial head can also occur in complex proximal ulna fractures[35].
(Osteo) chondral lesions of the capitellum occur as the radial head is forced on the capitellum under the axial loading. In MRI studies injury to the capitellum is seen in 39% to 96% of the patients[26,27]. Capitellar fractures occur in 2%[7].
A rare associated injury of radial head fractures is a rupture of the IOM between radius and ulna and rupture of the triangular fibrocartilage complex. It is also known as an acute longitudinal radioulnar dissociation or Essex-Lopresti injury[36]. Neurovascular injuries can also occur. Neurologic injuries occur in 20% of elbow dislocations of which the ulnar and median nerve are most commonly affected[37]. Severe anterior displacement of the radial head can cause injury to the radial nerve. Posterior interosseous nerve injury has also been reported[38,39]. Brachial artery injury accompanies 0.3% to 1.7% of elbow dislocations[40].
In general, the treatment of Mason type I fractures is conservative with a pressure bandage and sling for support, and active mobilization as early as possible[41]. Aspiration of the intra-articular haematoma leads to a decrease in intra-articular pressure and pain[42]. Though there is no significant difference in pain between groups of patients in which the haematoma was aspirated compared to patients in whom aspiration was combined with bupivacaine injection in the elbow joint[43]. The natural course of Mason type I fractures is in general benign, however, in some studies persistent complaints have been reported in 20% of cases[44]. In several series, patients with the shortest period of immobilization had the best patient-reported outcome measure scores (PROMs) at follow-up[44,45]. Shulman et al[46] recently evaluated the follow-up of patients with a Mason type I fracture, and concluded that “orthopaedic surgeons are likely over treating patients with Mason-Johnson TypeI radial head fractures by recommending frequent radiographic follow-up without modifying treatment, leading to unnecessary patient visits, radiation exposure, and increased costs”.
There is currently no consensus on the treatment of patients with isolated, displaced, stable, partial articular fractures of the radial head. Surgical repair of radial head fractures became popular after the introduction of new techniques and implants for the fixation of small articular fracture fragments[47-52]. Later, enthusiasm grew with reports of good results on surgical treatment of these Mason type II fractures[49-51,53]. On the other hand, articles on the conservative treatment of Mason type II fractures also report favorable outcomes[54,55]. Lindenhovius et al[56] reported on the long-term outcome of ORIF for stable displaced partial articular fractures of the radial head with an average 22 years follow-up. Although the results were good, complications were seen in 44% of patients. Furthermore, they compared their results with the 19 years follow-up of the same type of fractures that were treated conservatively by Akesson et al[54] and concluded that ORIF is not superior in the long-term. These results are in accordance to a recent retrospective comparative study by Yoon et al[57], in which nonoperative management was compared to ORIF. They found no clinically significant difference in PROMs, ROM and strength between the groups[57]. However, more complications [failure of hardware and heterotopic ossifications (HO)] were seen following ORIF, and younger patients scored worse on PROMs. Helling et al[58] found no significant difference in outcome between ORIF with metal screws vs biodegradable polylactide pins for the treatment of displaced radial head fractures.
Kaas et al[59] performed a systematic review on the treatment of Mason type II fractures and concluded that, based on 9 included retrospective series, there was insufficient evidence to determine which treatment is superior[59]. Currently, the inclusion of patients for a multicenter randomized controlled trial is initiated to define whether stable partial articular displaced fractures of the radial head are best treated by ORIF or nonoperative management[60].
Although Mason[1] originally advised to perform a resection of the comminuted fractured radial head, numerous other surgical techniques have been described last decades. In cases of isolated comminuted radial head fractures, without associated instability of the elbow, resection of the radial head may lead to satisfactory results[61]. Replacement of the radial head by silicone implants was performed with the idea to restore elbow stability, but resulted in several implant-related problems and complications[62]. Subsequently, management by ORIF became more popular. Good results were reported after ORIF for stable radial head fractures[51]. However, Ring et al[63] established that ORIF for Mason type III fractures with more than three articular fragments was more likely to result in unsatisfactory outcomes compared to fractures with only 2 or 3 simple fragments[63]. These severely comminuted unstable fractures of the radial head are difficult to restore and are prone to result into hardware failure or nonunion. Moro et al[64] therefore advised to use metallic radial head prosthesis (RHP) if a stable internal fixation of the comminuted radial head cannot be achieved. A literature search revealed only one randomized study by Chen et al[65], which compared ORIF vs arthroplasty for comminuted unstable radial head fractures. After two years of follow-up patients in the replacement group had significantly better PROMs. Furthermore, more complications (limitation in motion, nonunion, malunion, HO, infection) were seen following ORIF (11/23) compared to arthroplasty (3/22). The authors concluded that replacement is more effective than ORIF in clinical practice. However, they justly noted that prosthesis have problems with ageing, loosening and wear, which are not seen in the short-term follow-up of that study. The main problem with of current RHP designs is that only short- to mid-term results are known. RHP may be classified according to the different materials used: (silicone, polyethylene, pyrocarbon, metal), into differences in modularity (monoblock vs modular), polarity (uni- or monopolar vs bipolar) or fixation method (cemented vs uncemented press fit vs intentional loose fit). Despite the growing amount of data, evolving surgical technique and improving implant design and rationale; prosthetic radial head replacement is far from what should be considered an established and routine procedure. It is currently unknown whether one fixation technique has superior outcomes over the others. The same question accounts for material and design of the implants. Future research should therefore compare the various types of RHP and obtain long-term results of the implants.
The treatment of complex elbow trauma is based on 2 principles[35]. The first principle is that elbow function should be maintained by restoring the ulnohumeral joint. Fractures of coronoid, olecranon or distal humerus should therefore be treated by osteosynthesis. The second principle is that elbow stability should be reestablished. As described above, the radial head is an important secondary stabilizer of the elbow, and radial head fractures are commonly concomitant to ligamentous injuries. Lesions of the LCL and MCL should therefore be repaired in most cases[35].
The radial head is important secondary stabilizer of the elbow, and fractures of the radial head (and its associated injuries) can result in pain, posttraumatic osteoarthritis and impaired elbow function. Management of radial head fractures should therefore be directed to achieve a stable and functional elbow joint (Table 2). Nondisplaced fractures should be treated by early active motion. The best treatment of stable partial articular fractures is currently unclear, and can be either conservatively by early motion, or ORIF and early motion. Comminuted unstable fractures that consist of 2 or 3 simple fragments can be treated by ORIF. However, if stable internal fixation is not obtained, or the fracture consists of more than 3 fragments, radial head arthroplasty results in better outcomes in the short-term. Long-term results of RHP are still unknown. In all cases of surgically treated radial head fractures it is of utmost importance to adequately assess and treat associated injuries of the coronoid, olecranon and ligaments.
| Mason type | Indication | Treatment options1 |
| I | All | Conservative with early motion |
| II | Stable | Conservative with early motion or ORIF |
| Unstable | Conservative with early motion or ORIF | |
| Block with rotation | ORIF | |
| III | 2-3 simple fragments | ORIF |
| > 3 unstable fragments | Arthroplasty | |
| IV | See above | See above |
P- Reviewer: Emara K, Fernandez-Fairen M, Ma DY, von Heideken J S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK
| 1. | Mason ML. Some observations on fractures of the head of the radius with a review of one hundred cases. Br J Surg. 1954;42:123-132. [PubMed] |
| 2. | Jones SG. Fractures of the Head and Neck of Radius - Separation of Upper Radial Epiphysis. New Engl J Med. 1935;212:914-917. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Morrey BF, An KN. Articular and ligamentous contributions to the stability of the elbow joint. Am J Sports Med. 1983;11:315-319. [PubMed] |
| 4. | Morrey BF, An KN. Stability of the elbow: osseous constraints. J Shoulder Elbow Surg. 2005;14:174S-178S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 146] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 5. | Duckworth AD, Clement ND, Jenkins PJ, Will EM, Court-Brown CM, McQueen MM. Socioeconomic deprivation predicts outcome following radial head and neck fractures. Injury. 2012;43:1102-1106. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Kaas L, van Riet RP, Vroemen JP, Eygendaal D. The epidemiology of radial head fractures. J Shoulder Elbow Surg. 2010;19:520-523. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 104] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 7. | van Riet RP, Morrey BF, O’Driscoll SW, Van Glabbeek F. Associated injuries complicating radial head fractures: a demographic study. Clin Orthop Relat Res. 2005;441:351-355. [PubMed] |
| 8. | Duckworth AD, Clement ND, Jenkins PJ, Aitken SA, Court-Brown CM, McQueen MM. The epidemiology of radial head and neck fractures. J Hand Surg Am. 2012;37:112-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 108] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 9. | Jackson JD, Steinmann SP. Radial head fractures. Hand Clin. 2007;23:185-193, vi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 31] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Kaas L, Sierevelt IN, Vroemen JP, van Dijk CN, Eygendaal D. Osteoporosis and radial head fractures in female patients: a case-control study. J Shoulder Elbow Surg. 2012;21:1555-1558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Morrey BF, Tanaka S, An KN. Valgus stability of the elbow. A definition of primary and secondary constraints. Clin Orthop Relat Res. 1991;187-195. [PubMed] |
| 12. | Beingessner DM, Dunning CE, Gordon KD, Johnson JA, King GJ. The effect of radial head excision and arthroplasty on elbow kinematics and stability. J Bone Joint Surg Am. 2004;86-A:1730-1739. [PubMed] |
| 13. | Jensen SL, Olsen BS, Søjbjerg JO. Elbow joint kinematics after excision of the radial head. J Shoulder Elbow Surg. 1999;8:238-241. [PubMed] |
| 14. | Pomianowski S, Morrey BF, Neale PG, Park MJ, O’Driscoll SW, An KN. Contribution of monoblock and bipolar radial head prostheses to valgus stability of the elbow. J Bone Joint Surg Am. 2001;83-A:1829-1834. [PubMed] |
| 15. | King GJ, Zarzour ZD, Rath DA, Dunning CE, Patterson SD, Johnson JA. Metallic radial head arthroplasty improves valgus stability of the elbow. Clin Orthop Relat Res. 1999;114-125. [PubMed] |
| 16. | Armstrong AD, Dunning CE, Faber KJ, Duck TR, Johnson JA, King GJ. Rehabilitation of the medial collateral ligament-deficient elbow: an in vitro biomechanical study. J Hand Surg Am. 2000;25:1051-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 65] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 17. | Kodde IF, Kaas L, van Es N, Mulder PG, van Dijk CN, Eygendaal D. The effect of trauma and patient related factors on radial head fractures and associated injuries in 440 patients. BMC Musculoskelet Disord. 2015;16:135. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Johnston GW. A follow-up of one hundred cases of fracture of the head of the radius with a review of the literature. Ulster Med J. 1962;31:51-56. [PubMed] |
| 19. | Broberg MA, Morrey BF. Results of treatment of fracture-dislocations of the elbow. Clin Orthop Relat Res. 1987;109-119. [PubMed] |
| 20. | Hotchkiss RN. Displaced Fractures of the Radial Head: Internal Fixation or Excision? J Am Acad Orthop Surg. 1997;5:1-10. [PubMed] |
| 21. | Rineer CA, Guitton TG, Ring D. Radial head fractures: loss of cortical contact is associated with concomitant fracture or dislocation. J Shoulder Elbow Surg. 2010;19:21-25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Bruinsma WE, Guitton T, Ring D. Radiographic loss of contact between radial head fracture fragments is moderately reliable. Clin Orthop Relat Res. 2014;472:2113-2119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Guitton TG, Brouwer K, Lindenhovius AL, Dyer G, Zurakowski D, Mudgal CS, Ring DC. Diagnostic accuracy of two-dimensional and three-dimensional imaging and modeling of radial head fractures. J Hand Microsurg. 2014;6:13-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | van Leeuwen DH, Guitton TG, Lambers K, Ring D. Quantitative measurement of radial head fracture location. J Shoulder Elbow Surg. 2012;21:1013-1017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 25. | Capo JT, Shamian B, Francisco R, Tan V, Preston JS, Uko L, Yoon RS, Liporace FA. Fracture pattern characteristics and associated injuries of high-energy, large fragment, partial articular radial head fractures: a preliminary imaging analysis. J Orthop Traumatol. 2015;16:125-131. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 26. | Itamura J, Roidis N, Mirzayan R, Vaishnav S, Learch T, Shean C. Radial head fractures: MRI evaluation of associated injuries. J Shoulder Elbow Surg. 2005;14:421-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 127] [Cited by in RCA: 105] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 27. | Kaas L, Turkenburg JL, van Riet RP, Vroemen JP, Eygendaal D. Magnetic resonance imaging findings in 46 elbows with a radial head fracture. Acta Orthop. 2010;81:373-376. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 49] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 28. | Hausmann JT, Vekszler G, Breitenseher M, Braunsteiner T, Vécsei V, Gäbler C. Mason type-I radial head fractures and interosseous membrane lesions--a prospective study. J Trauma. 2009;66:457-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 29. | McGinley JC, Gold G, Cheung E, Yao J. MRI detection of forearm soft tissue injuries with radial head fractures. Hand (N Y). 2014;9:87-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 30. | Kaas L, van Riet RP, Turkenburg JL, Vroemen JP, van Dijk CN, Eygendaal D. Magnetic resonance imaging in radial head fractures: most associated injuries are not clinically relevant. J Shoulder Elbow Surg. 2011;20:1282-1288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 30] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 31. | Amis AA, Miller JH. The mechanisms of elbow fractures: an investigation using impact tests in vitro. Injury. 1995;26:163-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 85] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 32. | Rosenblatt Y, Athwal GS, Faber KJ. Current recommendations for the treatment of radial head fractures. Orthop Clin North Am. 2008;39:173-85, vi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 64] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 33. | Ring D, Jupiter JB, Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am. 2002;84-A:547-551. [PubMed] |
| 34. | Somford MP, Wiegerinck JI, Hoornenborg D, van den Bekerom MP, Eygendaal D. Eponyms in elbow fracture surgery. J Shoulder Elbow Surg. 2015;24:369-375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 35. | Morrey BF. Current concepts in the management of complex elbow trauma. Surgeon. 2009;7:151-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 36. | Essex-Lopresti P. Fractures of the radial head with distal radio-ulnar dislocation; report of two cases. J Bone Joint Surg Br. 1951;33B:244-247. [PubMed] |
| 37. | Morrey BF. The elbow and its disorders. 4th ed. Philadelphia, PA: Saunders/Elsevier 2009; 1211. |
| 38. | Serrano KD, Rebella GS, Sansone JM, Kim MK. A rare case of posterior interosseous nerve palsy associated with radial head fracture. J Emerg Med. 2012;43:e115-e117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 39. | Sudhahar TA, Patel AD. A rare case of partial posterior interosseous nerve injury associated with radial head fracture. Injury. 2004;35:543-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 40. | Ayel JE, Bonnevialle N, Lafosse JM, Pidhorz L, Al Homsy M, Mansat P, Chaufour X, Rongieres M, Bonnevialle P. Acute elbow dislocation with arterial rupture. Analysis of nine cases. Orthop Traumatol Surg Res. 2009;95:343-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 41. | Mahmoud SS, Moideen AN, Kotwal R, Mohanty K. Management of Mason type 1 radial head fractures: a regional survey and a review of literature. Eur J Orthop Surg Traumatol. 2014;24:1133-1137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 42. | Ditsios KT, Stavridis SI, Christodoulou AG. The effect of haematoma aspiration on intra-articular pressure and pain relief following Mason I radial head fractures. Injury. 2011;42:362-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 43. | Chalidis BE, Papadopoulos PP, Sachinis NC, Dimitriou CG. Aspiration alone versus aspiration and bupivacaine injection in the treatment of undisplaced radial head fractures: a prospective randomized study. J Shoulder Elbow Surg. 2009;18:676-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 44. | Smits AJ, Giannakopoulos GF, Zuidema WP. Long-term results and treatment modalities of conservatively treated Broberg-Morrey type 1 radial head fractures. Injury. 2014;45:1564-1568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 45. | Paschos NK, Mitsionis GI, Vasiliadis HS, Georgoulis AD. Comparison of early mobilization protocols in radial head fractures. J Orthop Trauma. 2013;27:134-139. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 23] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 46. | Shulman BS, Lee JH, Liporace FA, Egol KA. Minimally displaced radial head/neck fractures (Mason type-I, OTA types 21A2.2 and 21B2.1): are we “over treating” our patients? J Orthop Trauma. 2015;29:e31-e35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 47. | Esser RD, Davis S, Taavao T. Fractures of the radial head treated by internal fixation: late results in 26 cases. J Orthop Trauma. 1995;9:318-323. [PubMed] |
| 48. | Geel CW, Palmer AK, Ruedi T, Leutenegger AF. Internal fixation of proximal radial head fractures. J Orthop Trauma. 1990;4:270-274. [PubMed] |
| 49. | Khalfayan EE, Culp RW, Alexander AH. Mason type II radial head fractures: operative versus nonoperative treatment. J Orthop Trauma. 1992;6:283-289. [PubMed] |
| 50. | King GJ, Evans DC, Kellam JF. Open reduction and internal fixation of radial head fractures. J Orthop Trauma. 1991;5:21-28. [PubMed] |
| 51. | Pearce MS, Gallannaugh SC. Mason type II radial head fractures fixed with Herbert bone screws. J R Soc Med. 1996;89:340P-344P. [PubMed] |
| 52. | Ring D. Open reduction and internal fixation of fractures of the radial head. Hand Clin. 2004;20:415-427, vi. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 43] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 53. | Akesson T, Herbertsson P, Josefsson PO, Hasserius R, Besjakov J, Karlsson MK. Displaced fractures of the neck of the radius in adults. An excellent long-term outcome. J Bone Joint Surg Br. 2006;88:642-644. [PubMed] |
| 54. | Akesson T, Herbertsson P, Josefsson PO, Hasserius R, Besjakov J, Karlsson MK. Primary nonoperative treatment of moderately displaced two-part fractures of the radial head. J Bone Joint Surg Am. 2006;88:1909-1914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 49] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 55. | Duckworth AD, Watson BS, Will EM, Petrisor BA, Walmsley PJ, Court-Brown CM, McQueen MM. Radial head and neck fractures: functional results and predictors of outcome. J Trauma. 2011;71:643-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 56. | Lindenhovius AL, Felsch Q, Ring D, Kloen P. The long-term outcome of open reduction and internal fixation of stable displaced isolated partial articular fractures of the radial head. J Trauma. 2009;67:143-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 57. | Yoon A, King GJ, Grewal R. Is ORIF superior to nonoperative treatment in isolated displaced partial articular fractures of the radial head? Clin Orthop Relat Res. 2014;472:2105-2112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 32] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 58. | Helling HJ, Prokop A, Schmid HU, Nagel M, Lilienthal J, Rehm KE. Biodegradable implants versus standard metal fixation for displaced radial head fractures. A prospective, randomized, multicenter study. J Shoulder Elbow Surg. 2006;15:479-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 22] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 59. | Kaas L, Struijs PA, Ring D, van Dijk CN, Eygendaal D. Treatment of Mason type II radial head fractures without associated fractures or elbow dislocation: a systematic review. J Hand Surg Am. 2012;37:1416-1421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 42] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 60. | Bruinsma W, Kodde I, de Muinck Keizer RJ, Kloen P, Lindenhovius AL, Vroemen JP, Haverlag R, van den Bekerom MP, Bolhuis HW, Bullens PH. A randomized controlled trial of nonoperative treatment versus open reduction and internal fixation for stable, displaced, partial articular fractures of the radial head: the RAMBO trial. BMC Musculoskelet Disord. 2014;15:147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 61. | Antuña SA, Sánchez-Márquez JM, Barco R. Long-term results of radial head resection following isolated radial head fractures in patients younger than forty years old. J Bone Joint Surg Am. 2010;92:558-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 100] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 62. | Vanderwilde RS, Morrey BF, Melberg MW, Vinh TN. Inflammatory arthritis after failure of silicone rubber replacement of the radial head. J Bone Joint Surg Br. 1994;76:78-81. [PubMed] |
| 63. | Ring D, Quintero J, Jupiter JB. Open reduction and internal fixation of fractures of the radial head. J Bone Joint Surg Am. 2002;84-A:1811-1815. [PubMed] |
| 64. | Moro JK, Werier J, MacDermid JC, Patterson SD, King GJ. Arthroplasty with a metal radial head for unreconstructible fractures of the radial head. J Bone Joint Surg Am. 2001;83-A:1201-1211. [PubMed] |
| 65. | Chen X, Wang SC, Cao LH, Yang GQ, Li M, Su JC. Comparison between radial head replacement and open reduction and internal fixation in clinical treatment of unstable, multi-fragmented radial head fractures. Int Orthop. 2011;35:1071-1076. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 84] [Article Influence: 6.0] [Reference Citation Analysis (0)] |