Published online Nov 18, 2015. doi: 10.5312/wjo.v6.i10.821
Peer-review started: April 9, 2015
First decision: June 4, 2015
Revised: June 25, 2015
Accepted: July 29, 2015
Article in press: August 3, 2015
Published online: November 18, 2015
Processing time: 216 Days and 18.4 Hours
AIM: To introduce the navigation system of software and instruments designed specifically for revision total knee arthroplasty (TKA).
METHODS: We present an imageless navigation system for revision TKA, with optical point and tracker identification to assess kinematic and anatomical landmarks. The system automatically positions the cutting guides with a motorized cutting unit. The cutting unit is placed on the distal femur with a femoral clamp and acts as a rigid body and the base for all femoral cuts. The surgical technique for using the navigation system for revision TKA is based on the technique used in primary TKA. However, there are some important differences. The most notable are: (1) differences in estimation of the position of the primary implant relative to the bone and the mechanical axes; (2) the specific possibilities the revision navigation software offers in terms of optimal joint level positioning; and (3) the suggested “best fit” position, in which the clock position, stem position and offset, femoral component size, and mediolateral position of the femoral component are taken into account to find the optimal femoral component position. We assessed the surgical technique, and accompanying software procedural steps, of the system, identifying any advantages or disadvantages that they present.
RESULTS: The system aims to visualize critical steps of the procedure and is intended as a tool to support the surgeon in surgical decision-making. Combining a computer-assisted cutting device with navigation makes it possible to carry out precise cuts without pinning. Furthermore, the femoral clamp provides a stable fixation mechanism for the motorized cutting unit. A stable clamp is paramount in the presence of periarticular bony defects. The system allows the position of the primary implant relative to the bone and mechanical axes to be estimated, at which point any malalignments can be corrected. It also offers an optimal joint level position for implantation, and suggests a “best fit” position, in which the clock position, stem position and offset, femoral component size, and mediolateral position of the femoral component are considered. The surgeon can therefore make decisions intraoperatively to maximise alignment and, hence, outcomes. Based on the intraoperative findings of joint stability, the surgeon can modify the preoperative plan and switch from a constrained condylar system to a hinged version, or vice versa.
CONCLUSION: The system is flexible and easy to learn and allows improvements in workflow during TKA.
Core tip: The obscuring of bony landmarks by the previous implant, scar formation, the loss of bone stock and ligamentous insufficiency, make revision total knee arthroplasty very demanding. Current navigation systems do not typically allow reconstruction of the anatomic joint line, which is an important factor in implant survival, or compensation for the absence of classical landmarks. We present an imageless navigation system for revision total knee arthroplasty. The system automatically positions the cutting guides with a motorized cutting unit. We assessed the surgical technique, and accompanying software procedural steps, of the system, identifying any advantages or disadvantages that they present.
- Citation: Hoffart HE, Dinges H, Kolbeck S, Ritschl P, Hommel H. Novel computer-assisted method for revision arthroplasty of the knee. World J Orthop 2015; 6(10): 821-828
- URL: https://www.wjgnet.com/2218-5836/full/v6/i10/821.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i10.821
Primary total knee arthroplasty (TKA) is generally a successful procedure[1], but the lifespan of the prosthesis is finite[2]. Patients may require revision TKA due to mechanical wear, aseptic loosening, infection, instability, or malalignment, among other reasons[2,3]. Implant positioning is closely linked to outcome in primary and revision TKA, and the criteria for an acceptable result include restoration of physiological joint line position and correct implant component position in the sagittal, coronal and transverse planes[4]. Patients have been shown to have better functional outcomes when coronal alignment is within 3° of neutral alignment[5-9]. Proper rotational alignment is particularly important for successful flexion gap stability, and affects patellofemoral mechanics during knee flexion[10-13]. Rotational malalignment has been associated with postoperative pain in primary TKA[14,15].
Successful revision TKA relies upon achieving the same results as a primary TKA[16,17]. Nevertheless, revision TKA is an even more demanding procedure than primary TKA due to previous implants hiding commonly used anatomical landmarks, scar formation, the loss of bone stock, and the frequent presence of osteolytic lesions, severe osteoporosis, lack of anatomical bony landmarks and ligamentous insufficiency that are often seen after the removal of the failed prosthesis[4,18-20]. A further complicating factor is that the patient’s bone may provide insufficient stability for the resection guides, due to the underlying osteoporosis and the presence of bone defects. Ligamentous tissue may also be distended, destroyed or retracted as a result of bone degradation, surgical over-exposure, or fibrous scars from previous procedures[4].
In revision TKA, implants with an intramedullary stem are typically used. The angle between the surface of the femoral prosthesis and the femoral stem, which is given by the manufacturer, limits the possibility to align the femoral implant in the coronal plane. This can be a further restricting factor during surgery to achieve correct alignment.
It is therefore unsurprising that revision TKA is less successful at producing high quality outcomes than primary TKA[21]. Currently, 10-year survival following revision TKA is estimated at 74%[22], substantially less than the expected survival rate after primary TKA[23].
Stability in revision TKA is achieved through the balance of collateral ligaments, the peripheral capsule, tendons, and other elements[4], and cannot rely simply on the stabilisation mechanism of the implant[24]. Accurate soft tissue balancing, proper three-dimensional restoration of limb alignment and joint line height, correct alignment of the patella, and a functional extensor mechanism are all important factors to achieve a successful functional outcome and long-term implant survival[25-29].
An anatomic joint line must be restored at the time of revision surgery[4,27]. Due to the frequent absence of the classical landmarks, this objective may be difficult to achieve. It cannot be assumed that an appropriate joint line was established at the primary surgery. In fact, it may be that an inappropriate joint line may have contributed to the failure of the primary arthroplasty[27].
Standard navigation software can significantly improve the accuracy of prosthesis implantation[30]. However, the use of systems designed primarily for primary TKA may be of limited benefit in a revision setting[31]. Dedicated software potentially allows the specific aspects of revision TKA to be addressed. The software aims to assist the surgeon with three dimensional implant alignment, medio-lateral positioning and antero-posterior shift, offset of the femoral component, and joint line reconstruction[30].
Here, a recently introduced navigation system for revision TKA is presented. The revision navigation software and instruments aim to guide surgeons through revision TKA. They have been designed for use with a dedicated constrained condylar knee system, and with a rotating hinged revision system. In this paper, the system, the surgical technique, and the potential advantages and disadvantages of the system are discussed.
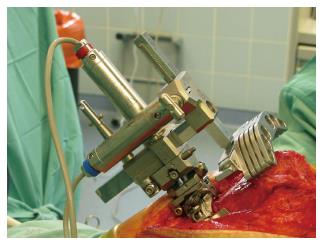
The navigation system for revision TKA (PiGalileo, Smith and Nephew Orthopeadics, Aarau, CH) is an imageless navigation system for revision TKA, with optical point and tracker identification to assess kinematic and anatomical landmarks. The system automatically positions the cutting guides with a motorized cutting unit. The cutting unit is placed on the distal femur with a femoral clamp and acts as a rigid body and the base for all femoral cuts (Figure 1).
The basic surgical technique for using the navigation system for revision TKA is based on the technique used in primary TKA described by Hoffart et al[32] and Matziolis et al[33]. While there are many similarities between the techniques used in primary and revision TKA, there are some important differences. The most notable are: (1) differences in estimation of the position of the primary implant relative to the bone and the mechanical axes; (2) the specific possibilities the revision navigation software offers in terms of optimal joint level positioning; and (3) the suggested “best fit” position, in which the clock position, stem position and offset, femoral component size, and mediolateral position of the femoral component are taken into account to find the optimal femoral component position.
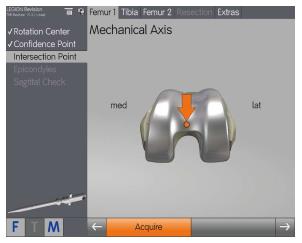
Once the computer-assisted saw guide unit and femoral clamp have been assembled and fixed flush to the ventral aspect of the distal femoral corticalis, the center of rotation of the hip is determined (Figure 2). This is performed through kinematic assessment of the lower extremity. The existing implant remains in situ at this point. The distal definition of the femoral mechanical axis is pinpointed by identifying the most dorsal part of the trochlea above the intercondylar notch on the implant or at the medial insertion point of the posterior cruciate ligament (Figure 3). Next, the medial and lateral epicondyles are identified.
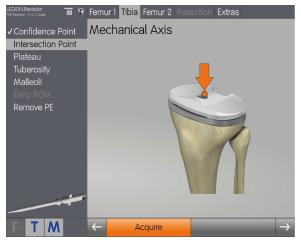
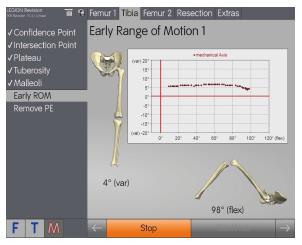
On the tibial implant, the intersection point of the mechanical axis on the old implant is measured, and the location of the medial and lateral deepest points of the existing tibial plateau identified. The direction of tuberosity, aligned parallel to the tibial plateau, is determined, and the position of the medial and lateral malleoli is identified. These latter measurements represent the distal definition of the tibial mechanical axis (Figure 4). The stability of the existing implantation is tested via the varus/valgus in extension/flexion to establish an early range of motion. This gives the surgeon an overview of the existing implant malalignment and stability of the knee, including the status of the ligaments. Consequently it offers the surgeon the opportunity to choose an alternative implant before any surgical steps with the original implants have been carried out. This early range of motion assessment is stored in a final report, thus giving evidence in case of any previous malalignment and instability (Figure 5).
The existing polyethylene is then removed to create space for the subsequent measurements. Next, further femoral landmarks are measured on the original implant and on the existing bone. The whiteside line and distal and posterior condyles of the original implant are measured. The condylar width is determined by identifying the medial and lateral edge of the medial condyle on the bone. The endpoint of the anterior shield of the implant on the anterolateral cortex is then pinpointed.
Next, the implants are removed, and the intramedullary canal is opened and reamed until a stable reaming can be achieved. The orientation of the last reamer is also measured to identify the anatomical axes. The motorized cutting unit is then placed and calibrated.
The surgeon now aligns the cuts and plans the implant position. The alignment of the mechanical axes can be performed by using either an anatomical axes orientation or a mechanical orientation, depending on the length of the chosen stem.
Before cutting, the position is checked and shifted, if necessary, in 0.5 mm steps distally or proximally to achieve minimal bone resection. Additionally the cutting block is raised or lowered closer to the bone to minimize saw blade twisting. The resection is performed through the 0 cut slot, or the -5, -10 or -15 cut slot if wedges are required.
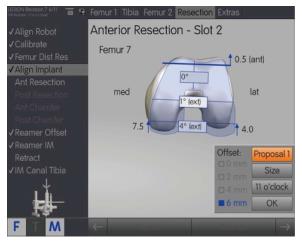
The system then presents a “best fit” position, which includes size, offset and position of the intramedullary stem, medio-lateral implant position, and clock position. The surgeon then assesses these parameters, including in rotation, and then performs the anterior resection. The motorized unit also allows anteroposterior adjustment in 0.5 mm increments.
Posterior and anterior chamfer resections are performed next, followed by the posterior chamfer cut and reaming of the intramedullary canal, with the guide moved to the correct mediolateral position beforehand. The cutting guide/block is then removed, before returning the motorized cutting unit to the zero position.
The tibial procedure is similar, with the intramedullary rod inserted through the intramedullary adaptor and into the tibial canal. The anatomical and mechanical axis is displayed on-screen for both varus/valgus and flexion/extension. This helps to determine the optimal varus/valgus alignment of the resection. The tibial resection is performed with the existing tibia cut block used for the revision implant. For proper alignment, resection height, varus/valgus and slope are checked. After implantation of the trial components, the range of motion can be measured to assess the stability of the joint and correct the polyethylene height, if necessary.
This navigation system for revision TKA consists of two elements: a bone referencing imageless navigation system and a computer-assisted cutting device. It has been designed to cope with a number of surgical issues that are specific for revision knee arthroplasty.
The system aims to visualize critical steps of the procedure and is intended as a tool to support the surgeon in surgical decision-making. Combining a computer-assisted cutting device with navigation makes it possible to carry out precise cuts without pinning. Furthermore, the femoral clamp provides a stable fixation mechanism for the motorized cutting unit. A stable clamp is paramount in the presence of periarticular bony defects.
As the position of the primary implant is measured first, the surgeon should correct for any malalignments, including rotational, that occurred with the primary implant. In standard revision TKA, the commonly used anatomical landmarks disappear once the implants have been removed, making correct placement of the prosthesis, especially in the presence of pre-existing malalignments, extremely challenging.
Based on the intraoperative findings of joint stability (status of joint capsule and ligaments), the surgeon can modify the preoperative plan and switch from a constrained condylar system to a hinged version, or vice versa.
Joint-level planning can be based on the old prosthesis or on a calculated algorithm based on the relationship between epicondylar distance to the medial and the lateral condyles developed by Romero et al[34].
In revision TKA, implants with an intramedullary stem are typically used. The angle between the surface of the femoral prosthesis and the stem generally measures 6° of valgus. Using such an implant will result in a perpendicular angle of the mechanical axis to the joint surface of the knee. The implant itself therefore has a restricted guidance and the surgeon has limited opportunities to change the alignment in the varus/valgus direction (In the tibia, the anatomical and mechanical axis typically coincide.). When using a short stem, the navigation software offers the possibility, alongside intramedullary and mechanical axis alignment, of an alignment “in between” the optimal anatomical and mechanical alignment, achieving an ideal implant position based on the given anatomical constraints of the individual patient.
As implant sizing and positioning is difficult to achieve in revision TKA, the navigation system calculates the optimal position of the femoral implant based on size, the anteroposterior and mediolateral dimensions, and the clock position of the offset. In addition, the software gives the optimal configuration for the chosen implant. Based on this algorithm, the best six options with regard to implant configuration (including clock position and offset), component size, position, and stem position, depending on the stem offset, are suggested to the surgeon (Figure 6).
The workflow of the surgery may be adapted to personal preferences or surgical requirements by rearranging individual functional sections or “blocks” of the surgical workflow, via drag and drop. Some changes are possible even during the procedure. However, the system also was designed to refuse modifications if a specific workflow is not possible for safety or technical reasons. This offers the opportunity for the surgeon to examine the consequences of each decision taken, and to assess different implant solutions, and, if ultimately, an intraoperative switch to another implant.
For these reasons, the authors believe the system is suitable to serve as a teaching tool for understanding revision TKA.
Revision TKA is frequently a highly complex and difficult procedure, as commonly used anatomical references are hidden by previous implants and disappear after the failed implants are removed. Some degree of bone loss is typically encountered in all cases during revision surgery, and may often be underestimated[35] Causes of bone loss include stress shielding, osteolysis, infection, mechanical bone loss generated from a loose implant, and iatrogenic loss during implant removal[36-42]. Additionally, decreased bone mineral density is observed[35], which compromises pin fixation and promotes fractures. The degree of bone loss is variable, ranging from situations in which the epicondyles remain in situ to massive bone loss where the traditional bony landmarks are no longer available. Consequently, exact positioning of the revision cutting devices is aggravated[43].
During revision surgery, osteoporosis and bony defects at the distal femur can lead to suboptimal positioning of the pins and, hence, the cutting blocks. In addition, inadequate rigid fixation of the cutting blocks to osteoporotic bone may cause oscillations of the sawblades that change the position of the cutting blocks. This may result in discordant cutting planes on the condylar back surfaces of the implant, thus jeopardizing implant bone contact and, potentially, implant longevity.
In contrast, the presented navigation system offers rigid fixation of the cutting blocks, as the motorized block is secured on the distal femur corticalis with a clamp. The construct remains stable even in the presence of bony defects. From our initial experience, the rigidity leads to precise cuts, with good contact between the bone cuts and the prosthesis. A disadvantage is that the femoral clamp needs some space in region of the suprapatellar pouch. Even if the brackets of the clamp are provided with spaces for fixation in the cortical bone, the clamp can compress the periosteum/soft tissue around the bone.
The additional fine adjustment of the distal and posterior cutting planes in 0.5-mm increments allows further adaptation of the flexion and extension gap. In the presence of distal and dorsal bone defects, it is paramount that the surgeon is able to resect as little bone as possible.
A known issue associated with conventional instrumentation in TKA revision is joint line proximalization. There is always distal femoral bone loss during revision surgery, and there is a tendency to undersize the femoral component. In addition, there is usually a relatively large flexion space after component removal compared to the extension space[25]. To compensate for this, the surgeon frequently fills the flexion space with a thicker inlay to balance the flexion and extension gaps. This, however, comes at the price of an elevated joint line.
It is also possible that the joint line was already elevated during primary surgery. In that case, radiographs of the primary TKA may not reflect the true anatomical position before primary TKA[34]. Thus, the restoration of the anatomical joint line in revision TKA is challenging, especially in the presence of preoperative deviations. The presented navigation system implements the findings of Romero et al[34], who described an algorithm to calculate the position of the joint line that can be used even in absence of classical landmarks. They used the linear correlation between epicondylar width and the perpendicular distance from the medial and lateral epicondyle of the joint-line tangent. Consequently, the joint line in revision TKA can be determined accurately and can be compared on-screen with the former joint line. Based on our initial experiences, we believe this feature will be helpful as further guidance to achieve an anatomic joint-line reconstruction.
Another consideration is that standard revision TKA surgery, and surgeries using navigation systems originally developed for primary TKA, rely on anatomical landmarks that are frequently no longer present. In such situations, anatomical references need to be taken from preoperative X-rays or be acquired from implant components that are to be removed[18]. This may result in suboptimal implant positioning and joint line restoration (as mentioned above)[4,30], and indicates that native anatomy should be taken into account. It has also been observed that primary navigation systems used in revision TKA lack the flexibility to cope with mismatches between stem alignment and the articular resection. In such instances, the implanted prosthesis may be forced in the direction of the diaphyseal axis[30].
The current system, however, identifies the anatomical and mechanical axes to achieve optimal implant alignment, to a feasible extent. This gives surgeons a range of options, depending on the implants to be used. For example, when using a long femoral stem, the system allows alignment from the endosteal cortex of the intramedullary canal, which is a reliable method of achieving satisfactory alignment in most, but not in all, revision TKAs[44]. In cases where satisfactory alignment cannot be obtained, the use of short femoral stems will be beneficial. The navigation systems for revision TKA allows the surgeon to compromise between neutral anatomical and mechanical alignment, which may be valuable in femoral alignment.
The navigation system we describe is based on a bone-referencing technique. Future enhancements with the possibility of ligament balancing are currently being developed. At present, our experience indicates that a good estimate of stability is obtained after three passes of early ROM with the system. The first reading is performed under application of a valgus stress, the second with varus stress and the third with a spontaneous ROM as a reference. As a result, the surgeon has a good indication of the stability of the joint and ligaments, and the required level of constraint from the implant (i.e., a hinged design or a constrained condylar design). The decision can then be made intraoperatively to go ahead with the planned implant or change the implant type. Overall, this is only the first attempt at including soft tissue balancing in the navigation algorithm and will be developed further.
For the surgeon experienced in revision TKA, the software is easy to use and, by providing a number of choices, ensures that they are in control of the procedure while being guided on a step-by-step basis. However, it should be seen as a tool to facilitate the execution of thorough preoperative planning, instead of replacing it. The system facilitates precise implementation of a thoroughly prepared preoperative plan, and allows the surgeon to intraoperatively adapt the preoperative plan if necessary, based on feedback and feed-forward provided by the system.
Based on a complex measurement algorithm, the system visually and numerically presents six proposals of femoral implant configurations to the surgeon. These configurations contain details on implant size, offset and position of the intramedullary stem, medio-lateral implant position, and clock position that is adaptable by the surgeon, based on his experiences and preferences.
The system also allows the location of the primary implant to be documented at the time of revision, which may be beneficial in medico-legal situations.
The presented navigation system aims to further improve surgical strategy and accuracy over navigation systems designed solely for primary TKA. The system requires validation for accuracy and reproducibility in a variety of clinical settings, both in comparison with standard surgical approaches and with more traditional assisted navigation systems. The intraoperative advantages highlighted above must be carefully weighed against the expected increase in surgical time. Radiographic evidence from robust clinical studies will also be needed to prove that the current navigation system leads to improved implant alignment. Femoral component alignment in the coronal plane is largely determined by the stem component and the femoral diaphysis. For this reason, surgical navigation may not necessarily improve alignment in the coronal plane. The use of shorter stem components, as suggested in this paper, will offer additional possibilities to align the femoral component. In practice, this may be of marginal benefit, as this strategy is also at the disposal of the experienced surgeon who uses standard instrumentation. In addition, the additional flexibility of femoral component positioning must not be at the cost of implant fixation.
Once early results with this system for revision TKA will become available, it will doubtless present some limitations. For example, surgeons will be required to undergo training in order to be able to use the technology correctly and effectively, both in terms of accurate and careful data acquisition and use of the computer-assisted saw guide. Nevertheless, the system has been designed with this specifically in mind, with an in-depth of set of on-screen instructions and procedure guides. It is therefore anticipated that, for experienced surgeons, the learning curve will be no greater than in taking up a standard computer-assisted navigation system for primary TKA, and will assist surgeons in taking on more complex revision TKA procedures.
In summary, revision TKA is a demanding procedure, and current computer-assisted navigation systems typically do not allow surgeons to identify the pre-primary TKA anatomical and mechanical axes in order to arrive at the optimal revision implant position. The presented system for revision TKA is thought to offer surgeons a tool to improve workflows for total knee revision arthroplasty.
The authors are consultants for Smith and Nephew.
Revision total knee arthroplasty (TKA) is a demanding procedure due to previous implants hiding commonly used anatomical landmarks, scar formation, the loss of bone stock, and the frequent presence of osteolytic lesions, severe osteoporosis, lack of anatomical bony landmarks and ligamentous insufficiency that are often seen after the removal of the failed prosthesis. A recently introduced navigation system for revision TKA is presented. The revision navigation software and instruments aim to guide surgeons through revision TKA. In this paper, the system, the surgical technique, and the potential advantages and disadvantages of the system are discussed.
Revision TKA is less successful at producing high quality outcomes than primary TKA. Currently, 10-year survival following revision TKA is substantially less than the expected survival rate after primary TKA. Current computer-assisted navigation systems typically do not allow surgeons to identify the pre-primary TKA anatomical and mechanical axes in order to arrive at the optimal revision implant position.
The current system for revision TKA is thought to offer surgeons a tool to improve workflows for total knee revision arthroplasty. The current navigation system aims to further improve surgical strategy and accuracy over navigation systems designed solely for primary TKA.
The intraoperative advantages must be carefully weighed against the expected increase in surgical time. The system requires validation for accuracy and reproducibility in a variety of clinical settings, both in comparison with standard surgical approaches and with more traditional assisted navigation systems.
Computer-assisted revision arthroplasty described in the papers uses an imageless navigation system for revision TKA, with optical point and tracker identification to assess kinematic and anatomical landmarks. The system automatically positions the cutting guides with a motorized cutting unit.
Interesting topic, well written article.
P- Reviewer: Labek G, Mugnai R, SooHoo NF S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Higuera CA, Deirmengian C. The new technologies in knee arthroplasty. J Clin Rheumatol. 2012;18:345-348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Tay KS, Lo NN, Yeo SJ, Chia SL, Tay DK, Chin PL. Revision total knee arthroplasty: causes and outcomes. Ann Acad Med Singapore. 2013;42:178-183. [PubMed] |
| 3. | Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7-13. [PubMed] |
| 4. | de Ladoucette A. Computer-assisted revision of total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2009;17:1166-1171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, Faris GW, Davis KE. Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res. 2004;428:26-34. [PubMed] |
| 6. | Choong PF, Dowsey MM, Stoney JD. Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J Arthroplasty. 2009;24:560-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 313] [Cited by in RCA: 338] [Article Influence: 21.1] [Reference Citation Analysis (0)] |
| 7. | Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1991;73:709-714. [PubMed] |
| 8. | Rienmüller A, Guggi T, Gruber G, Preiss S, Drobny T. The effect of femoral component rotation on the five-year outcome of cemented mobile bearing total knee arthroplasty. Int Orthop. 2012;36:2067-2072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res. 1994;299:153-156. [PubMed] |
| 10. | Anouchi YS, Whiteside LA, Kaiser AD, Milliano MT. The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res. 1993;170-177. [PubMed] |
| 11. | Moreland JR. Mechanisms of failure in total knee arthroplasty. Clin Orthop Relat Res. 1988;226:49-64. [PubMed] |
| 12. | Poilvache PL, Insall JN, Scuderi GR, Font-Rodriguez DE. Rotational landmarks and sizing of the distal femur in total knee arthroplasty. Clin Orthop Relat Res. 1996;331:35-46. [PubMed] |
| 13. | Stiehl JB, Cherveny PM. Femoral rotational alignment using the tibial shaft axis in total knee arthroplasty. Clin Orthop Relat Res. 1996;331:47-55. [PubMed] |
| 14. | Bell SW, Young P, Drury C, Smith J, Anthony I, Jones B, Blyth M, McLean A. Component rotational alignment in unexplained painful primary total knee arthroplasty. Knee. 2014;21:272-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 146] [Article Influence: 13.3] [Reference Citation Analysis (0)] |
| 15. | Czurda T, Fennema P, Baumgartner M, Ritschl P. The association between component malalignment and post-operative pain following navigation-assisted total knee arthroplasty: results of a cohort/nested case-control study. Knee Surg Sports Traumatol Arthrosc. 2010;18:863-869. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 16. | Maculé-Beneyto F, Hernández-Vaquero D, Segur-Vilalta JM, Colomina-Rodríguez R, Hinarejos-Gomez P, García-Forcada I, Seral Garcia B. Navigation in total knee arthroplasty. A multicenter study. Int Orthop. 2006;30:536-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 43] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Rand JA, Ries MD, Landis GH, Rosenberg AG, Haas S. Intraoperative assessment in revision total knee arthroplasty. J Bone Joint Surg Am. 2003;85-A Suppl 1:S26-S37. [PubMed] |
| 18. | Marcacci M, Nofrini L, Iacono F, Di Martino A, Bignozzi S, Lo Presti M. A novel computer-assisted surgical technique for revision total knee arthroplasty. Comput Biol Med. 2007;37:1771-1779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Sierra RJ, Cooney WP, Pagnano MW, Trousdale RT, Rand JA. Reoperations after 3200 revision TKAs: rates, etiology, and lessons learned. Clin Orthop Relat Res. 2004;200-206. [PubMed] |
| 20. | Windsor RE, Scuderi GR, Moran MC, Insall JN. Mechanisms of failure of the femoral and tibial components in total knee arthroplasty. Clin Orthop Relat Res. 1989;15-19; discussion 19-20. [PubMed] |
| 21. | Saleh KJ, Rand JA, McQueen DA. Current status of revision total knee arthroplasty: how do we assess results? J Bone Joint Surg Am. 2003;85-A Suppl 1:S18-S20. [PubMed] |
| 22. | Sheng PY, Konttinen L, Lehto M, Ogino D, Jämsen E, Nevalainen J, Pajamäki J, Halonen P, Konttinen YT. Revision total knee arthroplasty: 1990 through 2002. A review of the Finnish arthroplasty registry. J Bone Joint Surg Am. 2006;88:1425-1430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 56] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 23. | Labek G, Thaler M, Janda W, Agreiter M, Stöckl B. Revision rates after total joint replacement: cumulative results from worldwide joint register datasets. J Bone Joint Surg Br. 2011;93:293-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 447] [Cited by in RCA: 389] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 24. | Whiteside LA. Ligament balancing in revision total knee arthroplasty. Clin Orthop Relat Res. 2004;178-185. [PubMed] |
| 25. | Bellemans J. Restoring the joint line in revision TKA: does it matter? Knee. 2004;11:3-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 62] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Bourne RB, Crawford HA. Principles of revision total knee arthroplasty. Orthop Clin North Am. 1998;29:331-337. [PubMed] |
| 27. | Hoeffel DP, Rubash HE. Revision total knee arthroplasty: current rationale and techniques for femoral component revision. Clin Orthop Relat Res. 2000;116-132. [PubMed] |
| 28. | Krackow KA. Revision total knee replacement ligament balancing for deformity. Clin Orthop Relat Res. 2002;152-157. [PubMed] |
| 29. | Laskin RS. Joint line position restoration during revision total knee replacement. Clin Orthop Relat Res. 2002;169-171. [PubMed] |
| 30. | Jenny JY, Diesinger Y. Navigated revision TKR: a comparative study with conventional instruments. Orthopedics. 2010;33:58-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Massin P, Boyer P, Pernin J, Jeanrot C. Navigated revision knee arthroplasty using a system designed for primary surgery. Comput Aided Surg. 2008;13:179-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 32. | Hoffart HE, Langenstein E, Vasak N. A prospective study comparing the functional outcome of computer-assisted and conventional total knee replacement. J Bone Joint Surg Br. 2012;94:194-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 52] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 33. | Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C. A prospective, randomized study of computer-assisted and conventional total knee arthroplasty. Three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am. 2007;89:236-243. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 307] [Cited by in RCA: 324] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 34. | Romero J, Seifert B, Reinhardt O, Ziegler O, Kessler O. A useful radiologic method for preoperative joint-line determination in revision total knee arthroplasty. Clin Orthop Relat Res. 2010;468:1279-1283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 35. | van Loon CJ, de Waal Malefijt MC, Buma P, Verdonschot N, Veth RP. Femoral bone loss in total knee arthroplasty. A review. Acta Orthop Belg. 1999;65:154-163. [PubMed] |
| 36. | Clarke HD, Scuderi GR. Revision total knee arthroplasty: planning, management, controversies, and surgical approaches. Instr Course Lect. 2001;50:359-365. [PubMed] |
| 37. | Completo A, Simões JA, Fonseca F. Revision total knee arthroplasty: the influence of femoral stems in load sharing and stability. Knee. 2009;16:275-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 40] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 38. | Fehring TK, Christie MJ, Lavernia C, Mason JB, McAuley JP, MacDonald SJ, Springer BD. Revision total knee arthroplasty: planning, management, and controversies. Instr Course Lect. 2008;57:341-363. [PubMed] |
| 39. | Gotterson PR, Nusem I, Pearcy MJ, Crawford RW. Metal debris from bony resection in knee arthroplasty--is it an issue? Acta Orthop. 2005;76:475-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 40. | Munjal S, Phillips MJ, Krackow KA. Revision total knee arthroplasty: planning, controversies, and management--infection. Instr Course Lect. 2001;50:367-377. [PubMed] |
| 41. | Sydney SE, Pickering SA, Bell CG, Crawford R. Reducing metal debris generation during total knee arthroplasty. Orthopedics. 2007;30:999-1000. [PubMed] |
| 42. | Tan GM, Lynne G, Sarbjit S. Osteolysis and wear debris after total knee arthroplasty presenting with extra-articular metallosis in the calf. J Arthroplasty. 2008;23:775-780. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 43. | Huten D. Femorotibial bone loss during revision total knee arthroplasty. Orthop Traumatol Surg Res. 2013;99:S22-S33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 49] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 44. | Ries MD. Endosteal referencing in revision total knee arthroplasty. J Arthroplasty. 1998;13:85-91. [PubMed] |