Published online Jan 18, 2015. doi: 10.5312/wjo.v6.i1.156
Peer-review started: December 26, 2013
First decision: February 13, 2014
Revised: August 10, 2014
Accepted: September 4, 2014
Article in press: September 10, 2014
Published online: January 18, 2015
Processing time: 391 Days and 4.8 Hours
AIM: To systematically review and analyze the overall impact and effectiveness of bony surgical procedures, the triangle tilt and humeral surgery in a comparative manner in permanent obstetric brachial plexus injury (OBPI) patients.
METHODS: We conducted a literature search and identified original full research articles of OBPI patients treated with a secondary bony surgery, particularly addressing the limitation of shoulder abduction and functions. Further, we analyzed and compared the efficacy and the surgical outcomes of 9 humeral surgery papers with 179 patients, and 4 of our secondary bony procedure, the triangle tilt surgical papers with 86 patients.
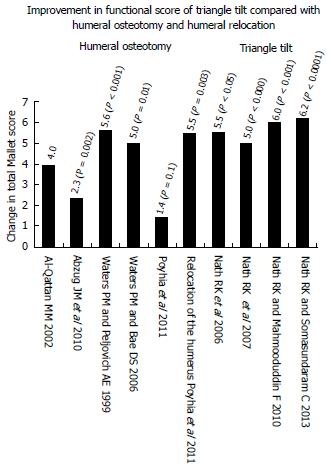
RESULTS: Seven hundred and thirty-one articles were identified, using the search term “brachial plexus” and obstetric or pediatric (246 articles) or neonatal (219 articles) or congenital (188 articles) or “birth palsy” (121 articles). Further, only a few articles were identified using the bony surgery search, osteotomy “brachial plexus” obstetric (35), “humeral osteotomy” and “brachial plexus” (17), and triangle tilt “brachial plexus” (14). Of all, 12 studies reporting pre- and post- operative or improvement in total Mallet functional score were included in this study. Among these, 9 studies reported the humeral surgery and 4 were triangle tilt surgery. We used modified total Mallet functional score in this analysis. Various studies with humeral surgery showed improvement of 1.4, 2.3, 5.0 and 5.6 total Mallet score, whereas the triangle tilt surgery showed improvement of 5.0, 5.5, 6.0 and 6.2.
CONCLUSION: The triangle tilt surgery improves on what was achieved by humeral osteotomy in the management of shoulder function in OBPI patients.
Core tip: We systematically reviewed, analyzed and compared the surgical outcomes of 9 humeral surgery papers with 179 permanent obstetric brachial plexus injury patients (OBPI), and 4 of our secondary bony procedure, the triangle tilt surgical papers with 86 OBPI patients. We used modified total Mallet functional score in this analysis. Studies with humeral surgery showed improvement of 1.4, 2.3, 5.0 and 5.6 total Mallet score, whereas the triangle tilt surgery showed improvement of 5.0, 5.5, 6.0 and 6.2. The triangle tilt surgery improves on what was achieved by humeral osteotomy in the management of shoulder function in OBPI patients.
- Citation: Nath RK, Somasundaram C. Triangle tilt and humeral surgery: Meta-analysis of efficacy and functional outcome. World J Orthop 2015; 6(1): 156-160
- URL: https://www.wjgnet.com/2218-5836/full/v6/i1/156.htm
- DOI: https://dx.doi.org/10.5312/wjo.v6.i1.156
Limitation to shoulder movement and function are the common secondary problems in permanent obstetric brachial plexus injury (OBPI) patients, as shoulder is the most frequently affected joint. If these infants do not receive early treatment, the chronic muscle imbalance leads to bone deformity and humeral head posterior subluxation.
To date, there has been no systematic evaluation of secondary bony surgical procedures that are involved in the treatment of shoulder function deficit in OBPI patients. Therefore, we attempted to systematically review and analyze the overall impact and effectiveness of bony surgical procedures, mainly the triangle tilt and humeral surgery in a comparative manner. The main goal of these secondary surgical procedures around the shoulder is to increase active abduction and external rotation in order to promote overall upper extremity functions.
Rotation osteotomy of the humerus has been described by several authors to treat the internal rotation contracture of the shoulder in OBPI[1-15]. Eng et al[2] reported that later surgical treatment with rotational osteotomy of the humerus seems to improve cosmesis but not function. Recently, Al-Qattan[9] has also shown that this procedure mainly improves the cosmetic appearance of children with total brachial plexus birth palsy. In addition, Al-Qattan et al[8] also found surprisingly, a significant (P = 0.003) decrease in shoulder abduction on long-term follow-up of his OBPI patients (the mean shoulder abduction was 135º, 146º and 109º measured pre-, early post- and late postoperatively, respectively). This technique has been used as a preferred procedure in older OBPI children[1,11,12,14], and shown to improve shoulder function[1,12], yet was not demonstrated as effective[8,9,13] procedure comparatively[16-18].
Waters et al[12], Waters et al[1] showed improvement of 5.0, and 5.6 in total Mallet score after humeral osteotomy. The efficacy and functional outcomes of the triangle tilt and humeral surgery are listed in Tables 1 and 2.
| Name of thesurgery | Ref. | No. of patients (age at surgery) | Follow-up (yr) | Surgical outcomes |
| Internal/external rotational/derotational osteotomy of the humerus | Abzug et al[13] | 23 patients Mean age 10.1 | 2.2 | 13.8 ± 2.8, 16.1 ± 2.5 (P = 0.002), Mallet increased about 2.3 |
| Al-Qattan[7] | 15 patients mean age 6.5 | 3 | Mallet increased about 4.0 | |
| Al-Qattan et al[9] | 13 patients mean age 6 (4.5-9) | 2 | Improved the cosmetic appearance | |
| Al-Qattan[8] | 17 patients mean age 6 (range 8-14) Recalled back to the clinic at a mean of 10 yr (range 8-14) after surgery. Mean age of 16, (range 13-20) | 10 | Found surprisingly, a significant (P = 0.003) decrease in shoulder abduction on long-term follow-up (the mean shoulder abduction was 135º, 146º and 109º measured pre-, early post- and late postoperatively, respectively) | |
| Waters et al[1] | 16 patients mean age 8.4 | 3 | Mallet improved 9.5 to 15.1 (P < 0.001) | |
| Waters et al[12] | 27 patients mean age 7.6 range 2. 3-17 | 3.7 | Mallet improved13 to 18 (P = 0.01). External rotation achieved with osteotomy was 64° (range, 35° to 90°) | |
| Pöyhiä et al[15] | 5 patients | 3.8 | Mallet increased about 1.4 (P = 0.1) | |
| Kirkoset al[14] | 22 patients mean age 10.0 age range 5-12 | Vary, no mean | Increase in active abduction of the arm was 27 º (range, 0 to 60), and the average increase in the arc of rotation was 25 º (range, 5 to 85) | |
| Al-Zahrani[6] | 12 patients age range 0.5 to 6 | 3.5 (1-5) | Cosmetic and functional improvement. ER improved 32º (20-40), abduction improved about 61º (60-70). | |
| Relocation of the humerus | Pöyhiä et al[15] | 13 patients | 3.8 | Mallet increased about 5.5 (P = 0.003) |
| Triangle Tilt surgery | Nath et al[16] | 4 patients, mean age 10.2 (range 7.9-11.9) | < 1.0 | Mallet improved 12.8 to 18.3 (P < 0.05) |
| Nath et al[17] | 40 patients, mean age 6.5 (range 2.2-10.3) | 1.3 | Mallet improved 13.6 to 18.6 (P < 0.000) | |
| Nath et al[20] | 20 patients, mean age 5.0 (range 1.3-13) | 1.5 | Mallet improved about 6.0 (P < 0.001) | |
| Nath et al[18] | 22 patients, mean age 5.8 (range 2.1-11.8) | 5 | Mallet improved 14.1 to 20.3 extended long term follow-up (5 yr, P < 0.0001) |
| Surgery | Ref. | Total Mallet improved |
| Humeral osteotomy | Abzug et al[13] | 2.3 (P < 0.002) |
| Humeral osteotomy | Waters et al[1] | 5.6 (P < 0.001) |
| Humeral osteotomy | Waters et al[12] | 5.0 (P = 0.01) |
| Humeral osteotomy | Pöyhiä et al[15] | 1.4 (P = 0.1) |
| Relocation of the humerus | Pöyhiä et al[15] | 5.5 (P = 0.003) |
| Triangle tilt | Nath et al[16] | 5.5 (P < 0.05) |
| Triangle tilt | Nath et al[17] | 5.0 (P < 0.000) |
| Triangle tilt | Nath et al[20] | 6.0 (P < 0.001) |
| Triangle tilt | Nath et al[18] | 6.2 (P < 0.0001) |
The triangle Tilt is a novel osseous procedure, consists of osteotomy of the clavicle at the junction of the middle and outer thirds, osteotomy of the acromion at its junction with the spine of the scapula, ostectomy of the superomedial angle of the scapula and splinting of the limb in adduction, 5° of external rotation and full forearm supination.
Humeral surgeries do not address the SHEAR deformity[19] and its central influence in the pathophysiology of the medial rotation contracture, and the shoulder deformity. In our experience, successful restoration of position and function in failed humeral osteotomy patients has followed from surgically addressing the SHEAR deformity. It may be inferred that the SHEAR correction, the triangle tilt surgery is a more specific operation because it addresses the root cause of the medial rotation.
We have shown improvement of 5.0, 5.5, 6.0 and 6.2 Mallet score following short and extended-long term (5 years) follow-up of triangle tilt surgery respectively in OBPI patients, age between 0.9 and 17 year[16-18]. Further, the triangle tilt surgery is a salvage procedure in failed humeral osteotomy patients[16,20].
We performed a search of the English language literature published up to December 2013 using mainly the Pubmed to identify full original research articles related to OBPI, using the following keywords “brachial plexus” and obstetric or pediatrics or neonatal or congenital or “birth palsy”. We conducted search for also keywords specific to bony surgeries addressing the shoulder deformities in OBPI: “humeral osteotomy”, “rotational/derotational osteotomy of the humerus”, “humeral relocation”, and “triangle tilt”. Databases such as Scopus and Google scholar were also referred. We do not find any of the articles not published in Pubmed appeared in Scopus. If any such articles appear in Scopus, mostly they are either non-English or with animal experiments. Of all the articles, we found 9 studies with humeral and 4 with triangle tilt surgery, reporting pre- and post- operative or change in total Mallet score (Table 3).
| Search term | Pubmed | Scopus |
| “Brachial plexus” obstetric | 731 | 620 |
| “Brachial plexus” pediatric | 246 | 176 |
| “Brachial plexus” neonatal | 219 | 226 |
| “Brachial plexus” congenital | 188 | 259 |
| “Brachial plexus”“birth palsy” | 121 | 115 |
| Bony Surgery search | ||
| Osteotomy “brachial plexus” obstetric | 35 | 34 |
| “Humeral osteotomy”“brachial plexus” | 17 | 23 |
| Osteotomy “brachial plexus”“birth palsy” | 11 | 13 |
| Osteotomy “brachial plexus” congenital | 8 | 14 |
| Osteotomy “brachial plexus” pediatric | 10 | 8 |
| Osteotomy “brachial plexus” neonatal | 0 | 3 |
| Triangle tilt “brachial plexus” | 14 | 8 |
Review articles, letter, technical and non-English language papers were excluded. Research articles using animal experiments and cadaver were also excluded. Articles reporting data from idiopathic or traumatic brachial plexus injuries in children were excluded as well (Table 4).
| Article parameters | Original full research paper with secondary bony surgical outcome of obstetric brachial plexus injury patients, English language publication, published till December 2013 in PubMed |
| Treatment options | Surgical-bony, humeral, triangle tilt |
| Patient age range | 9 mo-18 yr old |
| Functional outcome | Improvement in total Mallet score |
We included only articles using the triangle tilt and humeral surgery, reporting pre- and post- operative or change in total Mallet functional score in OBPI patients. 8 studies described the rotational osteotomy of the humerus with 166 patients, 1 described the relocation of the humerus with 13 patients, and 4 described triangle tilt surgery with 86 patients were included. Modified Mallet classification system was considered to assess the shoulder functions in this analysis (Table 1).
Seven hundred and thirty-one articles were identified, using the search term “brachial plexus” and obstetric or pediatric (246 articles) or neonatal (219 articles) or congenital (188 articles) or “birth palsy” (121 articles). Further, only a few articles were identified using the bony surgery search, osteotomy “brachial plexus” obstetric (35), “humeral osteotomy” and “brachial plexus” (17), and triangle tilt “brachial plexus” (14).
Of all, 12 studies reporting pre- and post- operative or improvement in total Mallet functional score were included in this study. Among these, 9 studies reported humeral surgery and 4 were triangle tilt surgery. We used modified total Mallet functional score in this analysis. Various studies with humeral surgery showed improvement of 1.4, 2.3, 5.0, and 5.6 total Mallet score, whereas the triangle tilt surgery showed improvement of 5.0, 5.5, 6.0 and 6.2 (Table 2 and Figure 1).
To our knowledge, this is the first attempt to review and analyze the surgical outcomes of the humeral and triangle tilt surgical procedures, that are involved in the management of shoulder function of OBPI patients. In examining restoration of shoulder function, the results of the meta-analysis suggest that the triangle tilt surgery improves on what was achieved by humeral osteotomy.
Limitation to shoulder movement and function are the common secondary problems in permanent obstetric brachial plexus injury (OBPI) patients, as shoulder is the most frequently affected joint. If these OBPI infants do not receive early treatment, the chronic muscle imbalance leads to bone deformity and humeral head posterior subluxation. To date, there has been no systematic evaluation of secondary bony surgical procedures that are involved in the treatment of shoulder function deficit in OBPI patients. Therefore, the authors attempted to systematically review and analyze the overall impact and effectiveness of bony surgical procedures, mainly the triangle tilt and humeral surgery in a comparative manner. The main goal of these secondary surgical procedures around the shoulder is to increase active abduction and external rotation in order to promote overall upper extremity functions.
The authors systematically reviewed, analyzed and compared the surgical outcomes of 9 humeral surgery papers with 179 permanent OBPI, and 4 of this secondary bony procedure, triangle tilt surgical papers with 86 OBPI patients. The authors used modified total Mallet functional score in this analysis. Studies with humeral surgery showed improvement of 1.4, 2.3, 5.0 and 5.6 total Mallet score, whereas triangle tilt surgery showed improvement of 5.0, 5.5, 6.0 and 6.2. The triangle tilt surgery improves on what was achieved by humeral osteotomy in the management of shoulder function in OBPI patients.
Triangle tilt surgery, a novel osseous surgical procedure developed by the lead author and surgeon, improves on what was achieved by humeral osteotomy in the management of shoulder function in OBPI patients. This is the first report comparing the secondary bony surgical procedures in OBPI patients.
The triangle tilt surgery showed significant improvement of shoulder functions when compared to humeral surgery in OBPI patients.
Meta-analysis, Triangle tilt surgery, humeral osteotomy, obstetric brachial plexus injury, Birth palsy, SHEAR deformity, Shoulder function, Mallet score. Triangle tilt surgery: This operative technique includes osteotomies of the clavicle, neck of the acromion and scapula in order to release the distal acromioclavicular triangle and allow it to reorient itself in a more neutral position into the glenoid.
This is a review concerning the beneficial effect of the triangle tilt surgery and humeral surgery in permanent OBPI patients from the literature. The review was comprehensive and should be published.
P- Reviewer: Canavese F, Pan HC, Schier R, Terzi R S- Editor: Song XX L- Editor: A E- Editor: Wu HL
| 1. | Waters PM, Peljovich AE. Shoulder reconstruction in patients with chronic brachial plexus birth palsy. A case control study. Clin Orthop Relat Res. 1999;144-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 57] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Eng GD, Koch B, Smokvina MD. Brachial plexus palsy in neonates and children. Arch Phys Med Rehabil. 1978;59:458-464. [PubMed] |
| 3. | Goddard NJ, Fixsen JA. Rotation osteotomy of the humerus for birth injuries of the brachial plexus. J Bone Joint Surg Br. 1984;66:257-259. [PubMed] |
| 4. | Dunkerton MC. Posterior dislocation of the shoulder associated with obstetric brachial plexus palsy. J Bone Joint Surg Br. 1989;71:764-766. [PubMed] |
| 5. | al Zahrani S. Modified rotational osteotomy of the humerus for Erb’s palsy. Int Orthop. 1993;17:202-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Al-Zahrani S. Combined Sever’s release of the shoulder and osteotomy of the humerus for Erb’s palsy. J Hand Surg Br. 1997;22:591-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Al-Qattan MM. Rotation osteotomy of the humerus for Erb’s palsy in children with humeral head deformity. J Hand Surg Am. 2002;27:479-483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 43] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Al-Qattan MM, Al-Husainan H, Al-Otaibi A, El-Sharkawy MS. Long-term results of low rotation humeral osteotomy in children with Erb’s obstetric brachial plexus palsy. J Hand Surg Eur Vol. 2009;34:486-492. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Al-Qattan MM. Total obstetric brachial plexus palsy in children with internal rotation contracture of the shoulder, flexion contracture of the elbow, and poor hand function: improving the cosmetic appearance of the limb with rotation osteotomy of the humerus. Ann Plast Surg. 2010;65:38-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Rühmann O, Gossé F, Schmolke S, Flamme C, Wirth CJ. Osteotomy of the humerus to improve external rotation in nine patients with brachial plexus palsy. Scand J Plast Reconstr Surg Hand Surg. 2002;36:349-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Soucacos PN, Vekris MD, Zoubos AB, Johnson EO. Secondary reanimation procedures in late obstetrical brachial plexus palsy patients. Microsurgery. 2006;26:343-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Waters PM, Bae DS. The effect of derotational humeral osteotomy on global shoulder function in brachial plexus birth palsy. J Bone Joint Surg Am. 2006;88:1035-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 55] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Abzug JM, Chafetz RS, Gaughan JP, Ashworth S, Kozin SH. Shoulder function after medial approach and derotational humeral osteotomy in patients with brachial plexus birth palsy. J Pediatr Orthop. 2010;30:469-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 69] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | Kirkos JM, Papadopoulos IA. Late treatment of brachial plexus palsy secondary to birth injuries: rotational osteotomy of the proximal part of the humerus. J Bone Joint Surg Am. 1998;80:1477-1483. [PubMed] |
| 15. | Pöyhiä T, Lamminen A, Peltonen J, Willamo P, Nietosvaara Y. Treatment of shoulder sequelae in brachial plexus birth injury. Acta Orthop. 2011;82:482-488. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Nath RK, Melcher SE, Paizi M. Surgical correction of unsuccessful derotational humeral osteotomy in obstetric brachial plexus palsy: evidence of the significance of scapular deformity in the pathophysiology of the medial rotation contracture. J Brachial Plex Peripher Nerve Inj. 2006;1:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | Nath RK, Lyons AB, Melcher SE, Paizi M. Surgical correction of the medial rotation contracture in obstetric brachial plexus palsy. J Bone Joint Surg Br. 2007;89:1638-1644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Nath RK, Somasundaram C. Extended long-term (5 years) outcomes of triangle tilt surgery in obstetric brachial plexus injury. Open Orthop J. 2013;7:94-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Nath RK, Paizi M. Scapular deformity in obstetric brachial plexus palsy: a new finding. Surg Radiol Anat. 2007;29:133-140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |