Published online Jul 18, 2013. doi: 10.5312/wjo.v4.i3.130
Revised: April 15, 2013
Accepted: June 1, 2013
Published online: July 18, 2013
Processing time: 139 Days and 3.4 Hours
AIM: To define the optimum safe angle of use for an eccentrically aligned proximal interlocking screw (PIS) for intramedullary nailing (IMN).
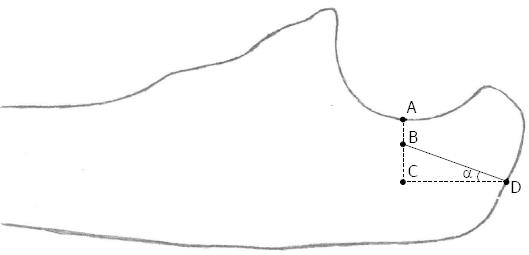
METHODS: Thirty-six dry cadaver ulnas were split into two equal pieces sagitally. The following points were identified for each ulna: the deepest point of the incisura olecrani (A), the point where perpendicular lines from A and the ideal IMN entry point (D) are intersected (C) and a point at 3.5 mm (2 mm safety distance from articular surface + 1.5 mm radius of PIS) posterior from point A (B). We calculated the angle of screws inserted from point D through to point B in relation to D-C and B-C. In addition, an eccentrically aligned screw was inserted at a standard 20° through the anterior cortex of the ulna in each bone and the articular surface was observed macroscopically for any damage.
RESULTS: The mean A-C distance was 9.6 mm (mean ± SD, 9.600 ± 0.763 mm), A-B distance was 3.5 mm, C-D distance was 12.500 mm (12.500 ± 1.371 mm) and the mean angle was 25.9° (25.9°± 2.0°). Lack of articular damage was confirmed macroscopically in all bones after the 20.0° eccentrically aligned screws were inserted. Intramedullary nail fixation systems have well known biological and biomechanical advantages for osteosynthesis. However, as well as these well-known advantages, IMN fixation of the ulna has some limitations. Some important limitations are related to the proximal interlocking of the ulna nail. The location of the PIS itself limits the indications for which intramedullary systems can be selected as an implant for the ulna. The new PIS design, where the PIS is aligned 20°eccentrically to the nail body, allows fixing of fractures even at the level of the olecranon without disturbing the joint. It also allows the eccentrically aligned screw to be inserted in any direction except through the proximal radio-ulnar joint. Taking into consideration our results, we now use a 20° eccentrically aligned PIS for all ulnas. In our results, the angle required to insert the PIS was less than 20° for only one bone. However, 0.7° difference corresponds to placement of the screw only 0.2 mm closer to the articular surface. As we assume 2.0 mm to be a safe distance, a placement of the screw 0.2 mm closer to the articular surface may not produce any clinical symptoms.
CONCLUSION: The new PIS may give us the opportunity to interlock IMN without articular damage and confirmation by fluoroscopy if the nail is manufactured with a PIS aligned at a 20.0° fixed angle in relation to the IMN.
Core tip: Limitations of intramedullary nailing (IMN) of the ulna, which make IMN a secondary choice, include problems experienced at the proximal interlocking screw (PIS). A new PIS system may solve most common problems with an eccentrically aligned screw. This new PIS system may be very advantageous if the fluoroscopy time, operation time and the need for additional incision in other systems is considered. However, the screw must be designed at a safe angle to have these advantages. According to our results, a 20.0° is the optimum angle of alignment for this screw.
- Citation: Küçükdurmaz F, Saglam N, Ağır İ, Sen C, Akpınar F. Olecranon anatomy: Use of a novel proximal interlocking screw for intramedullary nailing, a cadaver study. World J Orthop 2013; 4(3): 130-133
- URL: https://www.wjgnet.com/2218-5836/full/v4/i3/130.htm
- DOI: https://dx.doi.org/10.5312/wjo.v4.i3.130
Intramedullary nailing (IMN) of the forearm has gained much popularity but still has some technical limitations, especially in relation to IMN of the ulna[1,2]. The proximal interlocking screw (PIS) is one of the critical steps in IMN of the ulna. Location of the PIS limits the indications for which IMN of the ulna can be used with currently available IM systems. IM systems are useless in fractures where the olecranon is involved. In addition, IM systems may be insufficient in proximal ulna fractures and may require extra caution to avoid damage to the articular surface when placed around the olecranon[1,2]. Currently available IMN systems of the ulna have the same inherent problems as all IMN, requiring an extra incision for the interlocking screw and prolonged radiation exposure of the surgical team because of the use of fluoroscopy.
A newly developed PIS system[3] solves these problems with an eccentrically aligned PIS (Figure 1) which is inserted through a hole located at the proximal tip of the nail.
In this in vitro study, we aim to identify the optimum angle of the eccentrically aligned PIS to the IMN in relation to the olecranon articular surface.
Ulna bones of 36 dry bony cadavers were used. The proximal parts of the ulnas were split sagitally into two equal pieces. The deepest point of the incisura olecrani (A) was identified for each ulna. A horizantal line was drawn longitudinally at the middle of the medulla and a vertical line was drawn from point A perpendicular to this line. The point where these lines intersected (C) and the ideal IMN entry point (D) were also identified for each ulna. Then a point (B) was identified, located on the A-C line and 3.5 mm posterior to point A. 3.5 mm is the sum safe distance from the articular surface (2 mm) and the radius of PIS (1.5 mm) (Figure 2). Then, we calculated the angles of the screws when inserted from point D through to point B using the following formula: tanα = B-C/C-D (Figure 2).
In addition, taking into consideration the measured angles, a screw alligned eccentrically in relation to the IMN was inserted at a standard 20° through the anterior cortex of the ulna in each bone as a PIS and the articular surface was observed macroscopically for any damage.
The mean A-C distance was 9.600 mm (range 8.500-11.000 mm, SD = 0.763 mm). The mean A-B distance was 3.5 mm for each ulna. The mean C-D distance was 12.500 mm (range 10.000-14.600 mm, SD = 1.371 mm). The mean angle was 25.9° (range 19.3°-29.2°, SD = 2.0°) (Table 1). Lack of articular damage was observed macroscopically for each bone after the 20.0° eccentrically aligned screws were inserted.
| Ulna No. | A-C distance (mm) | C-D distance (mm) | Angle (°) |
| 1 | 9.7 | 11.2 | 24.9 |
| 2 | 9.4 | 13.8 | 23.1 |
| 3 | 9.0 | 12.0 | 24.6 |
| 4 | 8.5 | 14.3 | 19.3 |
| 5 | 8.9 | 13.4 | 21.9 |
| 6 | 11.0 | 14.6 | 27.2 |
| 7 | 10.1 | 13.6 | 25.9 |
| 8 | 10.4 | 12.4 | 29.1 |
| 9 | 11.0 | 13.4 | 29.2 |
| 10 | 11.0 | 14.6 | 27.2 |
| 11 | 9.0 | 11.7 | 25.2 |
| 12 | 8.7 | 10.6 | 26.1 |
| 13 | 10.2 | 14.0 | 25.6 |
| 14 | 10.5 | 13.2 | 27.9 |
| 15 | 9.3 | 12.9 | 24.2 |
| 16 | 9.8 | 12.4 | 26.9 |
| 17 | 10.0 | 14.5 | 24.1 |
| 18 | 9.5 | 12.8 | 25.1 |
| 19 | 9.5 | 12.7 | 25.3 |
| 20 | 8.8 | 10.7 | 26.3 |
| 21 | 10.1 | 13.5 | 26.0 |
| 22 | 11.0 | 14.5 | 27.3 |
| 23 | 9.0 | 10.7 | 27.2 |
| 24 | 9.6 | 12.1 | 26.7 |
| 25 | 9.9 | 12.5 | 27.1 |
| 26 | 8.7 | 11.3 | 24.7 |
| 27 | 8.9 | 10.2 | 27.9 |
| 28 | 10.8 | 13.6 | 28.2 |
| 29 | 9.0 | 11.0 | 26.6 |
| 30 | 9.0 | 10.6 | 27.4 |
| 31 | 8.9 | 10.1 | 28.1 |
| 32 | 8.6 | 12.5 | 22.2 |
| 33 | 9.3 | 12.7 | 24.5 |
| 34 | 10.1 | 13.1 | 26.7 |
| 35 | 9.8 | 12.4 | 26.9 |
| 36 | 8.7 | 10.0 | 27.4 |
| Total, mean ± SD (range) | 9.600 ± 0.763 (8.500-11.000) | 12.500 ± 1.371 (10.000-14.600) | 25.9 ± 2.0 (19.3-29.2) |
Intramedullary nail fixation systems have well known biological and biomechanical advantages for osteosynthesis. However, in addition to these well-known advantages, intramedullary nail fixation of the ulna has some limitations[1,2]. Some important limitations are related to the PI of the ulna nail. The location of the PIS itself limits the indications for which intramedullary systems can be selected as an implant for the ulna.
Intramedullary fixation systems are inadequate for fractures of the proximal ulna especially if the olecranon is involved. There is usually not enough bone stock to put a PIS into proximal fractures even if the fracture is slightly distal to the olecranon[4]. If the fracture is to the proximal part of the ulna or at the level of the olecranon, the screw should be inserted perpendicular or oblique to the articular surface[5-7]. This requires the selection of a PIS to avoid disturbing the joint, and this may not provide adequate stability. Moreover, there may be irritatation of the ulnar nerve if the PIS is aligned parallel to the articular surface of the olecranon[5]. Gehr and Friedl developed an intramedullary device for olecranon fractures, although this device cannot be used for segmental fractures, which also involve distal fractures, and they reported ulnar nerve irritation. The new PIS design allows the fixing of fractures even at the level of the olecranon without disturbing the joint when the PIS is aligned 20.0° eccentrically to the nail body. It also allows the eccentrically aligned screw to be inserted in any direction except through the proximal radio-ulnar joint.
Radiation exposure tends to be underestimated by surgeons[8,9]. Proximal interlocking always requires fluoroscopic confirmation. Currently available intramedullary nails for the ulna require quite long fluoroscopy time, even up to 150 min[7]. By contrast, with the new PIS system floroscopy usage is optional, provided preoperative measurements are done properly.
The PIS usually requires an additional incision[6,10,11]. In the new PIS system, the screw is inserted from the proximal tip of the nail. There is no need for an additional incision for PI other than the incision used for insertion of the IM nail, which means no additional soft tissue damage.
An eccentrically aligned PIS with a fixed angle may provide important advantages. The angle between the nail and screw has critical importance to the articular surface of the olecranon.
Taking into consideration our results, we use a 20° eccentrically aligned PIS for all ulnas by. In our results, the angle required to send the PIS was less than 20° (19.3°) for only one bone (No. 4). However, 0.7° difference corresponds to placement of screw only 0.2 mm closer to the articular surface. As we assume 2.0 mm to be a safe distance, a 0.2 mm closer placement of the screw to the articular surface may not produce any clinical symptoms. Moreover, as far as we know, there are no previous studies which have considered the safe distance between the screw and the articular surface of the olecranon. As a result, the lack of macroscopic articular surface damage in case 4, like all others, may be evidence of the safety of this system.
As a result, this new PIS system may be very advantageous if the fluoroscopy time, operation time and the need for additional incision compared to other systems is considered. However, the screw must be positioned at a safe angle to have these advantages. According to our results, a 20° is the optimum angle of alignment for the screw.
Intramedullary nail fixation systems have well known biological and biomechanical advantages for osteosynthesis. Limitations of intramedullary nailing (IMN) of the ulna, which makes IMN a secondary choice, includeproblems experienced at the proximal interlocking screw (PIS).
Location of the PIS limits the indications for use of IMN of the ulna in currently available intramedullary systems. A new PIS system may solve most common problems with an eccentrically aligned screw. The purpose of this in vitro study was to define the optimum safe angle of eccentrically aligned PIS for IMN.
İntramedullary systems may be insufficient in proximal ulna fractures and may require extra caution not to damage the articular surface when placed around the olecranon. Currently available IMN systems of the ulna have the same inherent problems as all IMN, requiring an extra incision for the interlocking screw and prolonged radiation exposure of the surgical team because of the use of fluoroscopy. The new PIS may give the authors the opportunity to interlock the IMN without articular damage and confirmation by fluoroscopy if the nail is manufactured with a PIS aligned at a 20° fixed angle in relation to the IMN.
The new PIS design allows fixing fractures even at the level of the olecranon without articular damage and confirmation of fluoroscopy.
Intramedullary nailing: A rod of metal, or other material for fixation of fragments of fractured bones, in this study for ulna fractures. Interlocking screw: A screw which passes through the IMN perpendicular to its long axis and prevents the nail to migrate or rotate within the bone.
This new PIS system may be very advantageous if the fluoroscopy time, operation time and the need for additional incision at other systems is considered. However, it must be designed at a safe angle to have these advantages. According to these results, 20° is the optimum angle of alignment for this screw.
P- Reviewers Erkan S, Kumar P S- Editor Gou SX L- Editor Hughes D E- Editor Ma S
| 1. | Hong G, Cong-Feng L, Hui-Peng S, Cun-Yi F, Bing-Fang Z. Treatment of diaphyseal forearm nonunions with interlocking intramedullary nails. Clin Orthop Relat Res. 2006;450:186-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Lee YH, Lee SK, Chung MS, Baek GH, Gong HS, Kim KH. Interlocking contoured intramedullary nail fixation for selected diaphyseal fractures of the forearm in adults. J Bone Joint Surg Am. 2008;90:1891-1898. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 3. | Akpinar F. New multifunctional locking intramedullary nailing system for ulna. Med J Umraniye. 2008;1:39-42. |
| 4. | Akpinar F, Aydinlioglu A, Tosun N, Tuncay I. Morphologic evaluation of the ulna. Acta Orthop Scand. 2003;74:415-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Gehr J, Friedl W. Intramedullary locking compression nail for the treatment of an olecranon fracture. Oper Orthop Traumatol. 2006;18:199-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 21] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Weckbach A, Blattert TR, Weisser Ch. Interlocking nailing of forearm fractures. Arch Orthop Trauma Surg. 2006;126:309-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Dalal S, Stanley D. Locked intramedullary nailing in the treatment of olecranon nonunion: a new method of treatment. J Shoulder Elbow Surg. 2004;13:366-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Hafez MA, Smith RM, Matthews SJ, Kalap G, Sherman KP. Radiation exposure to the hands of orthopaedic surgeons: are we underestimating the risk. Arch Orthop Trauma Surg. 2005;125:330-335. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 52] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Blattert TR, Fill UA, Kunz E, Panzer W, Weckbach A, Regulla DF. Skill dependence of radiation exposure for the orthopaedic surgeon during interlocking nailing of long-bone shaft fractures: a clinical study. Arch Orthop Trauma Surg. 2004;124:659-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 65] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 10. | Bansal H. Intramedullary fixation of forearm fractures with new locked nail. Indian J Orthop. 2011;45:410-416. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Visna P, Beitl E, Smídl Z, Kalvach J, Jaganjac E. Revision surgery in diaphyseal forearm fractures. Acta Chir Orthop Traumatol Cech. 2007;74:342-348. [PubMed] |