Revised: March 23, 2013
Accepted: April 10, 2013
Published online: April 18, 2013
Processing time: 52 Days and 0.7 Hours
In this article, we present a case of humeral biepicondylar fracture dislocation concomitant with ulnar nerve injury in a seventeen year-old male patient. Physical examination of our patient in the emergency room revealed a painful, edematous and deformed-looking left elbow joint. Hypoesthesia of the little finger was also diagnosed on the left hand. Radiological assessment ended up with a posterior fracture dislocation of the elbow joint accompanied by intra-articular loose bodies. Open reduction-Internal fixation of the fracture dislocation and ulnar nerve exploration were performed under general anesthesia at the same session as surgical treatment of our patient. Physical therapy and rehabilitation protocol was implemented at the end of two weeks post-operatively. Union of the fracture lines, as well as the olecranon osteotomy site, was achieved at the end of four months post-operatively. Ulnar nerve function was fully restored without any sensory or motor loss. Range of motion at the elbow joint was 20-120 degrees at the latest follow-up.
Core tip: Elbow joint posterior fracture-dislocations accompanied by neurovascular injuries are generally require surgical intervention. In this article, we present a case of humeral biepicondylar fracture dislocation concomitant with ulnar nerve injury in a seventeen year-old male patient. We obtained a successful clinical result by applying open reduction-internal fixation of the fracture dislocation and ulnar nerve repair at the same session as surgical treatment of this case. Although elbow fracture-dislocations with neurovascular complications are rarely seen, assessment of the neurovascular status in emergency room should always be a crucial part of physical examination which may affect the clinical result of the treatment.
- Citation: Konya MN, Aslan A, Sofu H, Yıldırım T. Biepicondylar fracture dislocation of the elbow joint concomitant with ulnar nerve injury. World J Orthop 2013; 4(2): 94-97
- URL: https://www.wjgnet.com/2218-5836/full/v4/i2/94.htm
- DOI: https://dx.doi.org/10.5312/wjo.v4.i2.94
Elbow joint is the second most common site of upper extremity dislocations in young adults[1]. Mechanism of injury in posterior elbow dislocation is generally described as falling on an outstretched hand[2]. Recent studies in the literature have shown that elbow joint is more likely to dislocate when it is in slightly abducted and flexed position. Posterior dislocation of the elbow joint occurs when compressive forces are directed on to the outstretched hand through the radius and ulna, along with the valgus stress at the elbow joint[3]. These biomechanical forces also contribute to associated fractures at the dislocated joint. Sport related injuries are the etiology in 10%-50% of all elbow dislocations. More than 90% of the cases are posterior dislocations. Isolated cases can be successfully treated with closed reduction; however, dislocations accompanied by fractures or neurovascular injuries are more prone to different complications and generally require surgical intervention[1-3].
In this article, we present a case of humeral biepicondylar fracture dislocation concomitant with ulnar nerve injury in a seventeen year-old male patient.
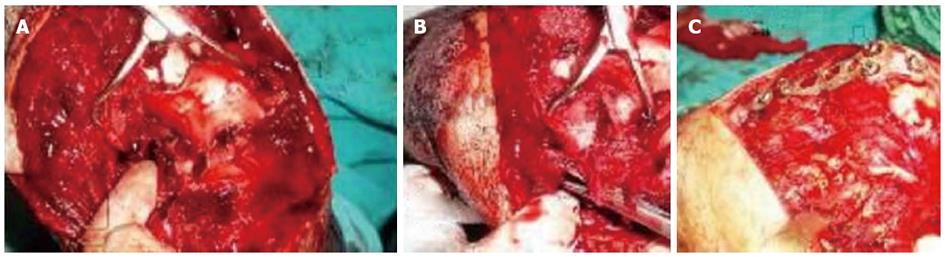
Seventeen year-old male patient was admitted to the emergency department after falling on to left arm. Physical examination of the patient in the emergency room revealed a painful, edematous and deformed-looking left elbow joint. Hypoesthesia of the little finger was also diagnosed on the left hand. Radiological assessment ended up with a posterior fracture dislocation of the elbow joint accompanied by intra-articular loose bodies (Figure 1). Closed reduction in the emergency room was failed and surgical treatment was planned for the patient. Under general anesthesia, the patient was admitted to the operation table in prone position. A pneumatic arm tourniquet was applied and then sterile dressing of the left upper extremity was set. Following a twenty centimeters long skin incision, ulnar nerve was explored and total disruption of the nerve was diagnosed (Figure 2).
V-shaped olecranon osteotomy was applied in order to achieve open anatomic reduction of the distal humeral joint surface as well as the removal of the loose bodies inside the joint. Lateral collateral ligament (LCL) was ruptured with avulsion fracture of the lateral epicondyle (Figure 2). Fixation of the lateral epicondyle together with the LCL was carried out by using a headless screw. A nerve stimulator was used to explore and find out the distal end of the ulnar nerve. Following release of the two ends, microsurgical repair with anterior transposition was applied for disrupted ulnar nerve. Medial collateral ligament (MCL) was also ruptured with avulsion fracture of the medial epicondyle. Fixation of the medial epicondyle together with the MCL was achieved by using a headless screw. Plate and screw fixation was chosen for olecranon osteotomy site (Figure 2).
Following wound closure, a posterior long arm splint was applied. Physical therapy and rehabilitation protocol was implemented at the end of two weeks post-operatively. Active and passive stretching exercises were put into practice following a 3-wk passive ROM rehabilitation program. Galvanic current electrotherapy nerve stimulation was also applied at the same time.
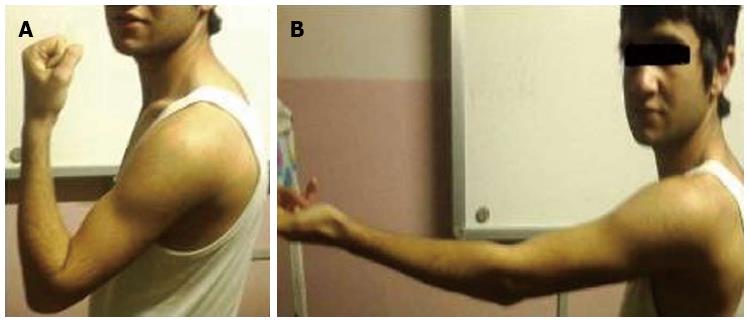
Union of the fracture lines, as well as the olecranon osteotomy site, was achieved at the end of forth months post-operatively and the plate was removed after one year (Figure 3). Ulnar nerve function was fully restored with minimally hypoesthesia and no motor loss. Finger co-ordination was fully recovered and the reduced grip strength was improved at the end of six months. Disability of the Arm-Shoulder-Hand (DASH) Score was used to evaluate healing status during the post-operative follow-up period. Quick DASH score was measured as 27.5 at the end of 1 year.
Range of motion at the elbow joint was between 20 to 120 degrees and there was not sensory or motor loss except slight hypoesthesia of the fourth and fifth fingers by the end of one year post-operatively (Figure 4).
Stability of the elbow joint is supplied by the primary and secondary stabilizers playing role in different stages of motion. Main primary stabilizer is the anatomical structure of the ulnohumeral joint. Coronoid process is especially the most important part of this anatomical structure. Secondary stabilizers are the radial head, joint capsule, and the origins of flexor and extensor tendons[4]. Fracture dislocation of the elbow joint is often accompanied by disruption of one or more bony stabilizers, and thus pathophysiology of the elbow fracture dislocation is complicated. Generally, the stability of the joint cannot be secured by closed reduction because of the impaired function of these bony fragments which are very small in size but play crucial role in the biomechanical stability[5].
Biepicondylar fracture dislocation of the elbow joint was reported by several authors in the literature[6-9]. Bono et al[10] presented a case of intraosseous median nerve entrapment following posterior elbow dislocation in a seven year-old child. Abu Jayyap et al[11] reported biepicondylar fracture dislocation with complete radial nerve transection. In another study, median nerve entrapment and ulnar nerve palsy following elbow fracture dislocation in a child was discussed[12]. Acute ulnar nerve entrapment following closed reduction of a posterior fracture dislocation of the elbow joint was also highlighted as a potential risk in the literature[13]. Our patient had biepicondylar fracture dislocation of the elbow concomitant with complete ulnar nerve disruption.
Twelve months clinical outcome of our case was evaluated by the use of DASH scale. This scale is a 30-item self-report questionnaire which was developed to evaluate the functional status and symptoms of the patients with musculoskeletal disorders of the upper extremity[14]. Validity and reliability of this questionnaire in Turkish were tested and used in different studies. The scale is scored between 0 to 100 points and the higher scores indicate a high level of disability[15]. DASH score of our case was measured as 27.5 at the end of one year.
In conclusion, we obtained a successful clinical result by applying open reduction-internal fixation of the fracture dislocation and ulnar nerve repair at the same session as surgical treatment of the case. As far as we could reach, we did not find any similar case reported in the literature. Although a few article can be considered close to our case report in the literature. We believe that although elbow dislocations with neurovascular complications are rarely seen, assessment of the neurovascular status in the emergency room should always be a crucial part of physical examination which may affect the clinical result of the treatment.
P- Reviewers Wang B, Liliang PC, Lykissas MG S- Editor Gou SX L- Editor A E- Editor Zhang DN
| 1. | Lattanza LL, Keese G. Elbow instability in children. Hand Clin. 2008;24:139-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Beyzadeoğlu T, Parmaksızoğlu F, Bekler H, Özyurt Y. Old unreduced medıal fracture - dıslocatıon of the elbow case report. Eklem Hastalı. k Cerrahisi. 2004;15:41-44. |
| 3. | McCabe MP, Savoie FH. Simple elbow dislocations: evaluation, management, and outcomes. Phys Sportsmed. 2012;40:62-71. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | O’Driscoll SW, Jupiter JB, King GJ, Hotchkiss RN, Morrey BF. The unstable elbow. Instr Course Lect. 2001;50:89-102. [PubMed] |
| 5. | Doornberg JN, van Duijn J, Ring D. Coronoid fracture height in terrible-triad injuries. J Hand Surg Am. 2006;31:794-797. [PubMed] |
| 6. | Gani NU, Rather AQ, Mir BA, Halwai MA, Wani MM. Humeral biepicondylar fracture dislocation in a child: A case report and review of the literature. Cases J. 2008;1:163. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Taylor GR, Gent E, Clarke NM. Biepicondylar fracture dislocation of a child’s elbow. Injury. 1997;28:71-72. [PubMed] |
| 8. | Meta M, Miller D. Paediatric biepicondylar elbow fracture dislocation - a case report. J Orthop Surg Res. 2010;5:75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Guner S, Guner SI, Ceylan MF, Gormeli G, Gormeli CA, Onder H. Biepicondylar fracture presenting with elbow dislocation: a case report. J Med Case Rep. 2012;6:265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Bono KT, Popp JE. Intraosseous median nerve entrapment following pediatric posterior elbow dislocation. Orthopedics. 2012;35:e592-e594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Abu-Jayyab Z, Abu-Zidan F, Marlovits S. Fracture dislocation of the lateral condyle and medial epicondyle of the humerus associated with complete radial nerve transection. J Pak Med Assoc. 2011;61:920-921. [PubMed] |
| 12. | Petratos DV, Stavropoulos NA, Morakis EA, Matsinos GS. Median nerve entrapment and ulnar nerve palsy following elbow dislocation in a child. J Surg Orthop Adv. 2012;21:157-161. [PubMed] |
| 13. | Reed MW, Reed DN. Acute ulnar nerve entrapment after closed reduction of a posterior fracture dislocation of the elbow: a case report. Pediatr Emerg Care. 2012;28:570-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med. 1996;29:602-608. [PubMed] |
| 15. | Düger T, Yakut E, Öksüz Ç, Yörükan S, Bilgütay BS, Ayhan Ç, Leblebicioğlu G, Kayıhan H, Kırdı N, Yakut Y. Reliability and validity of the Turkish version of the Disabilities of the Arm, Shoulder and Hand (DASH) Questionnaire. Fizyoter Rehabil. 2006;17:99-107. |