Published online Dec 18, 2012. doi: 10.5312/wjo.v3.i12.204
Revised: July 31, 2012
Accepted: December 6, 2012
Published online: December 18, 2012
Femoroacetabular impingement (FAI) is an increasingly recognized condition, which is believed to contribute to degenerative changes of the hip. This correlation has led to a great deal of interested in diagnosis and treatment of FAI. FAI can be divided into two groups: cam and pincer type impingement. FAI can lead to chondral and labral pathologies, that if left untreated, can progress rapidly to osteoarthritis. The diagnosis of FAI involves a detailed history, physical exam, and radiographs of the pelvis. Surgical treatment is indicated in anatomic variants known to cause FAI. The primary goal of surgical treatment is to increase joint clearance and decrease destructive forces being transmitted through the joint. Treatment has been evolving rapidly over the past decade and includes three primary techniques: open surgical dislocation, mini-open, and arthroscopic surgery. Open surgical dislocation is a technique for dislocating the femoral head from the acetabulum with a low risk of avascular necrosis in order to reshape the neck or acetabular rim to improve joint clearance. Mini-open treatment is performed using the distal portion of an anterior approach to the hip to visualize and to correct acetabular and femoral head and neck junction deformities. This does not involve frank dislocation. Recently, arthroscopic treatment has gained popularity. This however does have a steep learning curve and is best done by an experienced surgeon. Short- to mid-term results have shown relatively equal success with all techniques in patients with no or only mild evidence of degenerative changes. Additionally, all techniques have demonstrated low rates of complications.
- Citation: Wilson AS, Cui Q. Current concepts in management of femoroacetabular impingement. World J Orthop 2012; 3(12): 204-211
- URL: https://www.wjgnet.com/2218-5836/full/v3/i12/204.htm
- DOI: https://dx.doi.org/10.5312/wjo.v3.i12.204
Femoroacetabular impingement (FAI) is an anatomical condition that has recently been gaining recognition as potentially leading to future degenerative changes within the hip. FAI has recently been demonstrated to have an extremely high correlation for development of osteoarthritis. Some authors have suggested that FAI is likely the leading cause in what has previously been labeled “idiopathic” osteoarthritis of the hip[1-9].
FAI can be divided between two subgroups based on anatomic deformities: cam impingement or pincer impingement[2]. In cam impingement the anatomy of the proximal femur is abnormal, such as a nonspherical femoral head or decreased head-neck offset[2,6]. Pincer impingement is present when there is abnormal anatomy of the acetabulum such as acetabular rim overgrowth, acetabular retroversion, or coxa profunda[2]. Both of these conditions lead to abnormal, repetitive abutment of the acetabulum and the femoral neck[10,11].
Cam impingement leads to forceful contact of the abnormal femoral head and neck with the opposing joint surface during activity. This force is most noticeable during motions that place the hip in extremes of flexion[4]. The most frequent lesions both of labral tears and chondral injuries noted with cam impingement are located in the anterosuperior aspect of the joint[3,12,13].
In pincer impingement the abnormality is with the acetabulum. The predominant injury pattern seen in pincer impingement involves the labrum most often at the anterior aspect of the joint, the area of acetabular over-coverage[14,15]. The injury and inflammation to the labrum frequently leads to osteophyte formation, effectively worsening FAI by creating increased acetabular over-coverage[1-3]. This leads to contact with the femoral neck at even earlier points in the range of motion of the hip. The leveraging created by this contact between the femoral neck and acetabular rim can sometimes lead to articular cartilage injuries opposite the site of impingement. Frequently these injuries are smaller than those seen in cam impingement and less symptomatic[15].
The results of these anatomical variations leading to impingement are many. Those that contribute to osteoarthritis include: injury to the articular cartilage and labral tears. These injuries can then lead to progressive degeneration of the joint, ultimately resulting in pain and decreased motion through the hip joint. The insult to the joint caused by abutment of the femoral head or neck with the acetabular rim leads to decreased clearance for the joint, which in turn leads to worsening injury and a repetitive cycle that leads to degeneration of the joint[1-3,8,9]. The joint clearance is directly related the femoral head-neck offset as well as degree of acetabular coverage[4]. The forces that result from FAI can create very significant articular cartilage and labral injuries. This effect has been increasingly recognized over the past decade leading to increased research and development of novel techniques to treat both the cause of impingement as well as the resulting injuries in an attempt to slow the degenerative process[1,2,7,8,10].
Diagnosis of FAI is critical in order to treat it early and prevent further injury to the chondral surface or labrum. Patients frequently present complaining of hip pain that is worsened with physical activity. Often the pain is exacerbated by activities that require the hip to assume a flexed position. These patients may also complain of difficulty with prolonged sitting due to pain and discomfort[8,10,16].
Physical exam often demonstrates lack of full flexion of the hip and decreased internal rotation with the hip in the flexed position. Pain can usually be reproduced by the impingement test, which is performed by attempting to place the hip in flexion, adduction, and internal rotation[13,16].
A standard anteroposterior radiograph of the pelvis should be obtained to assess the version of the acetabulum and the shape of the femoral head and neck. Additionally, a cross-table lateral of the affected hip should be obtained with the hip in 15 degrees of internal rotation. This view allows for better analysis of the sphericity of the femoral head as well as the femoral head-neck offset. MRI (specifically MR arthrography) can be used to evaluate for the presence of any articular surface or labral injuries[14,16].
All patients with symptomatic FAI should undergo a trial of nonoperative treatment prior to consideration of surgical treatment. Unfortunately, conservative measures are often unsuccessful or unrealistic with many patients as they are frequently younger, active patients. Conservative treatment generally entails restrictions of activities and motions that place the hip the offending, most often flexed, position. Nonsteroidal anti-inflammatory drugs may be used for inflammation and pain control, but ultimately have no effect on the disease process. Frequently, patients with FAI wish to return to their previous activity levels and therefore may be indicated for surgical treatment[8-10,14].
Indications for surgical management of FAI begin with the failure of conservative treatment measures. Additionally, the surgical patient should have signs and symptoms of FAI along with a radiographically definable anatomic variant known to result in impingement[14,17-20].
Contraindications for surgical treatment of FAI include advanced age, moderate (or worse) osteoarthritis of the hip, and morbid obesity. In these situations the surgeon should more likely perform total hip arthroplasty if surgical intervention is warranted. This discussion should take place with the patient[14,17-20].
The primary focus of surgical treatment of FAI should be to improve joint clearance, ultimately reducing destructive forces across the joint surfaces[17-20]. Appropriate preoperative planning should be done so that the most beneficial approach is used and the area of impingement is correctly identified and addressed. Multiple techniques for addressing FAI have been developed and each of their advantages and disadvantages have been the subject of much debate over the past decade.
An open surgical technique is the most established technique for FAI. Ganz et al[17] described a safe technique for open surgical dislocation in 2001. This technique involves surgical dislocation utilizing a trochanteric flip osteotomy. This technique provides relatively safe access to the hip joint with low risk of injury to the vascular supply of the femoral head. Many authors feel that this technique provides the surgeon with the most versatile approach to the hip, allowing sufficient access for osteochondroplasty of the acetabular rim or the femoral head-neck junction as well as labral repair[17-19,21-24].
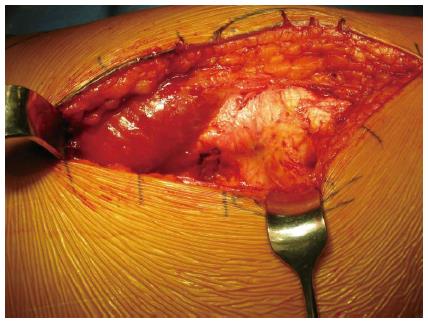
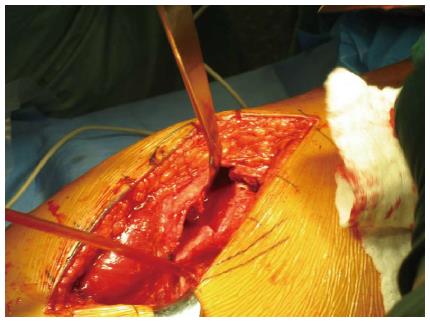
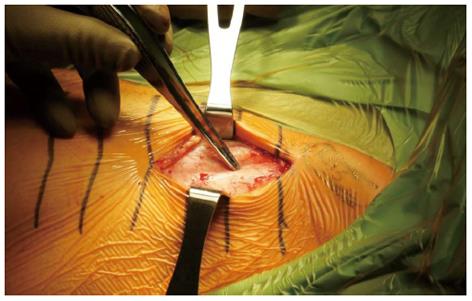
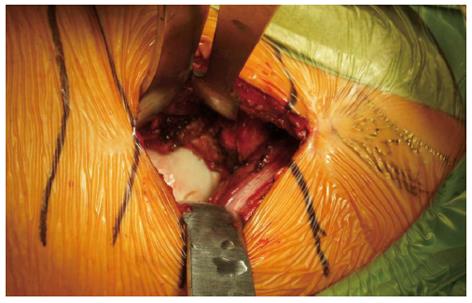
For an open surgical dislocation the patient should be placed in the lateral decubitus position such that the surgeon can use either a straight lateral approach or a posterolateral approach depending on surgeon preference[17,18,23]. Whichever approach is chosen it is extremely important to well visualize the greater trochanter prior to proceeding further with the operation (Figure 1). The posterior border of the greater trochanter must be well visualized, as it is the starting point for the trochanteric flip osteotomy with the medial circumflex artery in close proximity[21,22]. This portion of the operation is where the blood supply to the femoral head is at the greatest risk[21]. The trochanteric osteotomy is performed with the leg in internal rotation and care should be taken to leave the external rotators uninjured. The osteotomy begins at the posterior border of the greater trochanter and is carried anterior exiting superficial to the piriformis fossa and distal to the vastus ridge (Figure 2)[17,18,22,23]. Following osteotomy, muscle should be carefully dissected from the capsule. A Z-shaped capsulotomy is performed starting at the posterior acetabular rim then along the anterolateral femoral neck to the anteromedial femoral neck[17]. During this step, extreme care must be taken to avoid injury to any of the vasculature[17,22].
Once capsulotomy has been performed the hip should be assessed. The located hip should be taken through a full range of passive motion to most precisely locate the area of impingement. This step should always be performed prior to dislocation of the femoral head so that the surgeon may better visualize the area where osteochondroplasty must be performed in order to alleviate the impingement[17,23].
Moving the limb into flexion and external rotation then dislocates the femoral head. To completely dislocate the femoral head, the round ligament must be transected. This may need to be done if the lesions causing impingement are believed to be along the posterior femoral head or neck or the posterior acetabular rim[17,18].
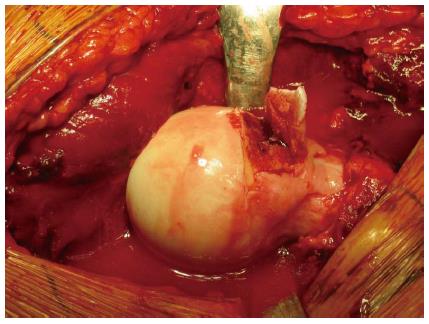
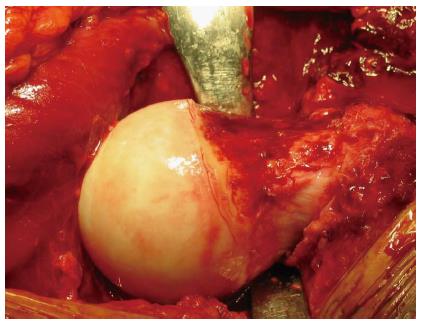
At this point, impingement caused by femoral head-neck junction can be corrected by performing osteochondroplasty (Figure 3). Along with identification of the site of impingement during range of motion of the hip, the area involved in FAI often has a distinct inflammatory appearance due to repetitive contact with the acetabulum. The femoral neck should be corrected to a normal contour using a curved osteotome to shave off slivers of the area of concern in a stepwise fashion taking care to avoid femoral neck vasculature (Figure 4)[1,17,18,23].
Next the acetabular rim and labrum should be inspected. If the anterior acetabular rim is contributing to FAI, it should be resected. To perform resection osteoplasty of the acetabular rim, the labrum must be mobilized or resected. If the labrum appears significantly diseased, it should be resected, otherwise attempts to mobilize and preserve the labrum should be attempted in order to preserve normal function of the hip joint. Once again, osteochondroplasty should be done with a curved osteotome. The resection should be done in a stepwise fashion until the area of impingement is removed and the underlying articular cartilage appears healthy. At this time the healthy labrum can be reattached to the new acetabular rim (Figure 5)[3,17,18,25].
Once the femoral head and neck and the acetabulum have been addressed the dislocated femoral head may be reduced. Following reduction, the hip should once again be taken through a full range of motion paying special attention to those positions that were noted to cause impingement prior to dislocation. If adequate resection of the offending lesions has been performed the hip should be able to be taken through a full range of motion with no further impingement[17,18,23,25,26]. If the osteochondroplasty is deemed acceptable the capsule should be closed loosely. The trochanteric osteotomy may then be reduced and fixed with cortical screws. The remainder of the wound should be closed in a layered fashion appropriate for the chosen approach[17,18].
The mini-open technique for treatment of FAI is generally done as a combination of open and arthroscopic procedures. Currently only a few studies examining the use of a mini-open technique are reported in the literature[25-29].
For the mini-open technique the patient is positioned supine on an operating room table with traction available[25]. The hip is not formally dislocated in the mini-open approach. Lesions within the joint are inspected using an arthroscope[25,27]. Shaving of chondral lesion or labral lesions are done during this arthroscopic investigation[27].
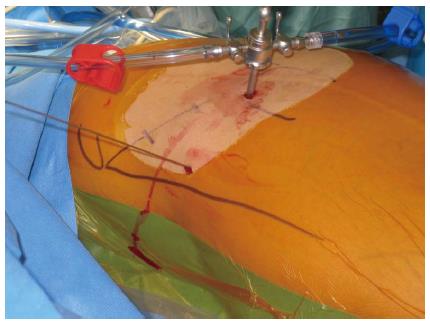
A partial anterior approach, the “Heuter Approach”, also called the “Short Smith-Pete” because it follows the interval of the Smith-Petersen distal to the anterior superior iliac spine, is used for access to the capsule and femoral neck (Figure 6). This can be accomplished with an incision ranging from 2 to 12 cm depending on the size of the patient This is done through the internervous plane between the femoral nerve (Sartorius, iliopsoas, and rectus femoris) and the superior gluteal nerve (gluteus minimus and medius and tensor fascia lata) (Figure 7)[27-29]. The capsulotomy is then performed using the same avascular location as that of the open surgical dislocation. This technique again allows easy identification of the lesion at the femoral head-neck junction (Figure 8). A high speed burr or an arthroscopic burr can be used for contouring of the femoral neck[27].
As with open dislocation, once all work has been completed the hip is fully ranged to assure complete resolution of the impingement. Following confirmation the capsule may be loosely closed and the remainder of the closure done in a layered fashion[27-29].
Some surgeons assert that FAI cannot be adequately treated using arthroscopy due to the limited view of the femoral neck and acetabulum. They also feel that lesions cannot be adequately accessed with the femoral head remaining located within the acetabulum. However, advocates of hip arthroscopy claim that due to the consistent location of most FAI lesions a 360-degree view of the femoral head, neck, and acetabulum is not necessary. Techniques believed to be useful for treatment of FAI using arthroscopy have been described in the literature[27,30-34].
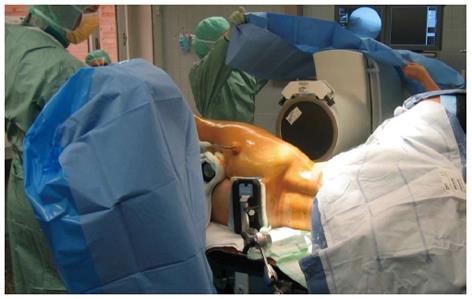
The patient should be placed either in the lateral position or supine based on surgeon’s preference. The operative leg should be placed in a traction device and fluoroscopy should be used to identify the areas of impingement (Figure 9). Fluoroscopy can also be used while placing the portals, which include anterior, anterolateral, and posterolateral portals[27,33,34].
The anterolateral portal is placed about 1 cm proximal and 1 cm anterior to the tip of the greater trochanter using fluoroscopy with the hip distracted. A 30-degree arthroscope is placed in the portal and the anterior portal is placed under direct visualization (Figure 10)[15,27,31]. The hip joint is then inspected and probed for articular cartilage damage as well as labral injuries. Both labral and chondral lesions can be debrided until stable tissue is reached[15,30,32,34]. Additionally, osteophytes can be removed with a burr. Some surgeons also advocate the use of microfracture techniques in areas where notable articular cartilage damage is seen[30,31].
Following the assessment of the articular surface, the arthroscope is placed in the anterolateral portal outside of the joint capsule. The capsule is dissected using instruments through the anterior portal. Once the capsule is well visualized an anterior capsulotomy is performed with minimal resection of the capsule. This allows for exposure of the femoral head-neck junction and manipulation of the instruments. Osteochondroplasty is then performed using a burr. Contour of the femoral neck should be checked using fluoroscopy throughout this portion of the procedure[27,30-32,34].
After all steps are completed the traction is removed from the leg and the hip is ranged while still being directly visualized using the arthroscope to check for any residual impingement[30,31,34].
Postoperatively the patient should be restricted to toe-touch weight bearing on the operative extremity for six to eight weeks. The patient should ambulate using crutches or a walker for assistance during this time to prevent falls. Physical therapy may be started immediately using passive range of motion for the first and second weeks postoperatively. At ten to fourteen days active motion may begin, however flexion should be limited 70 degrees for the first six to eight weeks. Early range of motion will help prevent the formation of adhesions[17-24].
Laude et al[28] report keeping patients with protected weight-bearing and use of crutches for five days. After 5 d the patients are allowed full weight bearing without crutches. At this time they are also encouraged to begin low impact active exercise, such as cycling. Patients are kept from high impact or contact sports for a total of six months postoperatively[25-29].
A recent review by Matsuda et al[25] found an overall result of surgical intervention for FAI with good to excellent results to be 65% to 95%. This was accompanied by an overall rate of complications of 0% to 20%.
Over the past decade numerous studies have helped define clear indications for surgical treatment of FAI. Thus far, surgical dislocation has demonstrated great success with most studies showing 65% to 95% of patients with good to excellent results in midterm follow-up[12,19,25,35]. Many studies have shown at least midterm benefit of halting or slowing of degenerative changes noted on follow-up radiographs of patients with Grade 0 or Grade 1 degenerative changes following surgical dislocation and removal of lesions, which had created FAI. Patients which Grade 2 or higher degeneration have shown less predictable results, although young patients with Grade 2 degenerative changes may be acceptable candidates for a trial of surgical dislocation[12].
Potential complications include trochanteric nonunion, heterotopic ossification, sciatic nerve palsy, osteonecrosis of the femoral head, femoral neck fracture. Osteonecrosis of the femoral head is rare with open surgical dislocation as the technique is designed to minimize risk to the blood supply to the femoral head. Additionally, risk of femoral neck fracture is minimized by limiting the depth of osteochondroplasty at the femoral head-neck junction to not greater than 30% of the diameter of the femoral neck[25,26].
Studies of open surgical dislocations have shown a rate of conversion to total hip arthroplasty of 0% to 30%, however the most recent studies with defined surgical indications show a lower rate of 0% to 5%[25].
A review of studies looking at mini-open treatment of FAI shows a reported success rate of 71% to 92%. Some researchers demonstrated an improvement in both the Harris hip score and UCLA activity score following mini-open treatment of FAI. Conversion to total hip arthroplasty was 0% to 11% and complications were seen in 0% to 17%. The literature suggests that there is a relatively high incidence of iatrogenic lateral femoral cutaneous nerve injury with the mini-open technique. There is limited data looking at mini-open treatment of FAI[25,27,29].
Some surgeons advocate hip arthroscopy when the lesion is localized and easily accessed with an arthroscope, especially those felt to be isolated labral tears. However many authors assert that labral tears do not occur without trauma or the presence of FAI. One study showed that less than 50% of patients treated with isolated arthroscopic labral debridement. Hip arthroscopy has also been noted to be associated with neuropraxia of many of the nerves near the hip joint due to the traction necessary for adequate visualization[5,25,27,32].
Other surgeons believed that adequate treatment of FAI might be achieved by arthroscopy. They advocate this technique as the claim patients are able to return to normal activities more quickly than with open surgical dislocation. Advocates also point toward series that demonstrate 75%-95% good to excellent outcomes at midterm follow-up for FAI treated arthroscopically. Series also show a conversion to total hip arthroplasty of 0% to 9%[25,32].
With the recently increased recognition of FAI and its possible contribution to early degenerative changes of the hip, the past decade has seen much study and advancement of various techniques to treat the pathologic anatomy of FAI. The techniques include open surgical dislocation, a mini-open technique with or without arthroscopy, and purely arthroscopic treatment.
Current literature with midterm follow-up shows similar success rates with all techniques. Additionally, all approaches have demonstrated similar conversions to total hip arthroplasty as well as similar rates of major complications. Open surgical dislocation showed a slightly higher rate of complications and reoperation, largely due to a 20% nonunion rate of the trochanteric flip osteotomy. Much more literature exists with respect to the arthroscopic approach to FAI. One important factor to note is surgeons with extensive experience with hip arthroscopy have performed all reported series of arthroscopic treatment of FAI. Hip arthroscopy is known to have a very steep learning curve. Therefore, the reliability of this technique likely depends heavily on the experience of the surgeon. The least studied technique is the mini-open technique.
The three techniques described in the literature of the past decade all have shown great success at treating FAI with significant improvement in symptoms. Midterm follow-up shows evidence supporting the slowing of degenerative changes in patients with minimal degeneration preoperatively. As the management of FAI continues to develop it is extremely important that a surgeon is comfortable with the technique chosen when surgical intervention is indicated.
Peer reviewers: Zoran Vukasinovic, Professor, Department of Pediatric Orthopaedics, Institute for Orthopaedic Surgery, “Banjica”28, Mihajla Avramovica, 11040 Belgrade, Serbia; Stefan Grote, MD, Department of Orthopaedic and Trauma Surgery, University of Munich, Nußbaumstr. 20, 80336 Munich, Germany
S- Editor Huang XZ L- Editor A E- Editor Zhang DN
| 1. | Baker-LePain JC, Lane NE. Relationship between joint shape and the development of osteoartritis. Curr Opin Rheumatol. 2010;22:538-543. [PubMed] |
| 2. | Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012-1018. [PubMed] |
| 3. | Ito K, Leunig M, Ganz R. Histopathologic features of the acetabular labrum in femoroacetabular impingement. Clin Orthop Relat Res. 2004;262-271. [PubMed] |
| 4. | Ito K, Minka MA, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171-176. [PubMed] |
| 5. | Kim KC, Hwang DS, Lee CH, Kwon ST. Influence of femoroacetabular impingement on results of hip arthroscopy in patients with early osteoarthritis. Clin Orthop Relat Res. 2007;456:128-132. [PubMed] |
| 6. | Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556-560. [PubMed] |
| 7. | Samora JB, Ng VY, Ellis TJ. Femoroacetabular impingement: a common cause of hip pain in young adults. Clin J Sport Med. 2011;21:51-56. [PubMed] |
| 8. | Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004;170-177. [PubMed] |
| 9. | Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747-1770. [PubMed] |
| 10. | Wisniewski SJ, Grogg B. Femoroacetabular impingement: an overlooked cause of hip pain. Am J Phys Med Rehabil. 2006;85:546-549. [PubMed] |
| 11. | Polkowski GG, Clohisy JC. Hip biomechanics. Sports Med Arthrosc. 2010;18:56-62. [PubMed] |
| 12. | Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;67-73. [PubMed] |
| 13. | Kubiak-Langer M, Tannast M, Murphy SB, Siebenrock KA, Langlotz F. Range of motion in anterior femoroacetabular impingement. Clin Orthop Relat Res. 2007;458:117-124. [PubMed] |
| 14. | Crawford JR, Villar RN. Current concepts in the management of femoroacetabular impingement. J Bone Joint Surg Br. 2005;87:1459-1462. [PubMed] |
| 15. | Larson CM. Arthroscopic management of pincer-type impingement. Sports Med Arthrosc. 2010;18:100-107. [PubMed] |
| 16. | Martin HD, Shears SA, Palmer IJ. Evaluation of the hip. Sports Med Arthrosc. 2010;18:63-75. [PubMed] |
| 17. | Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119-1124. [PubMed] |
| 18. | Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R, Leunig M. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;61-66. [PubMed] |
| 19. | Murphy S, Tannast M, Kim YJ, Buly R, Millis MB. Debridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004;178-181. [PubMed] |
| 20. | Vaughn ZD, Safran MR. Arthroscopic femoral osteoplasty/chielectomy for cam-type femoroacetabular impingement in the athlete. Sports Med Arthrosc. 2010;18:90-99. [PubMed] |
| 21. | Gautier E, Ganz K, Krügel N, Gill T, Ganz R. Anatomy of the medial femoral circumflex artery and its surgical implications. J Bone Joint Surg Br. 2000;82:679-683. [PubMed] |
| 22. | Nötzli HP, Siebenrock KA, Hempfing A, Ramseier LE, Ganz R. Perfusion of the femoral head during surgical dislocation of the hip. Monitoring by laser Doppler flowmetry. J Bone Joint Surg Br. 2002;84:300-304. [PubMed] |
| 23. | Anderson LA, Erickson JA, Severson EP, Peters CL. Sequelae of Perthes disease: treatment with surgical hip dislocation and relative femoral neck lengthening. J Pediatr Orthop. 2010;30:758-766. [PubMed] |
| 24. | Naal FD, Miozzari HH, Wyss TF, Nötzli HP. Surgical hip dislocation for the treatment of femoroacetabular impingement in high-level athletes. Am J Sports Med. 2011;39:544-550. [PubMed] |
| 25. | Matsuda DK, Carlisle JC, Arthurs SC, Wierks CH, Philippon MJ. Comparative systematic review of the open dislocation, mini-open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy. 2011;27:252-269. [PubMed] |
| 26. | Lamontagne M, Brisson N, Kennedy MJ, Beaulé PE. Preoperative and postoperative lower-extremity joint and pelvic kinematics during maximal squatting of patients with cam femoro-acetabular impingement. J Bone Joint Surg Am. 2011;93 Suppl 2:40-45. [PubMed] |
| 27. | Hartmann A, Günther KP. Arthroscopically assisted anterior decompression for femoroacetabular impingement: technique and early clinical results. Arch Orthop Trauma Surg. 2009;129:1001-1009. [PubMed] |
| 28. | Laude F, Sariali E, Nogier A. Femoroacetabular impingement treatment using arthroscopy and anterior approach. Clin Orthop Relat Res. 2009;467:747-752. [PubMed] |
| 29. | Ribas M, Ledesma R, Cardenas C, Marin-Peña O, Toro J, Caceres E. Clinical results after anterior mini-open approach for femoroacetabular impingement in early degenerative stage. Hip Int. 2010;20:36-42. [PubMed] |
| 30. | Baldwin K, Harrison R, Namdari S. Outcomes of Hip Arthroscopy for Treatment of Femoroacetabular Impingement: A Systematic Review. Current Orthop Practice. 2009;20:669-673. |
| 31. | Sampson TG. Arthroscopic treatment for chondral lesions of the hip. Clin Sports Med. 2011;30:331-348. [PubMed] |
| 32. | Yusaf MA, Hame SL. Arthroscopy of the hip. Curr Sports Med Rep. 2008;7:269-274. [PubMed] |
| 33. | Larson CM, Giveans MR. Arthroscopic management of femoroacetabular impingement: early outcomes measures. Arthroscopy. 2008;24:540-546. [PubMed] |
| 34. | Philippon MJ, Stubbs AJ, Schenker ML, Maxwell RB, Ganz R, Leunig M. Arthroscopic management of femoroacetabular impingement: osteoplasty technique and literature review. Am J Sports Med. 2007;35:1571-1580. [PubMed] |
| 35. | Nho SJ, Magennis EM, Singh CK, Kelly BT. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am J Sports Med. 2011;39 Suppl:14S-19S. [PubMed] |